Abstract
Purpose
In Germany, neonates undergo hip sonography examination using the Graf method during the routine U3 screening examination, performed by consultant physicians four to five weeks after birth, and are referred to specialized orthopaedic departments if there are any uncertainties. This study evaluated the quality of sonographic screening in the outpatient sector and the treatment requirements of referred children.
Methods
We performed a retrospective analysis of the patient data of 384 neonates collected in consultations performed between April 2016 and April 2019.
Results
In total, 74% (n = 284) of neonates presented a hip type Ia/b. Treatment (abduction brace or Fettweis cast) was required in 32% (n = 122) of cases. The treatment duration was significantly correlated with age at first presentation (Pearson’s r = 0.678; p = 0.001). The treatment duration for patients aged > 200 days old at first presentation was twice as long as those aged 100 days at first presentation. Patients with public health insurance require referral by a consultant. Developmental dysplasia of the hip as referral diagnosis could not be confirmed in control examination in 64% (n = 132) of cases. Of the public health insured children, 97% (n = 200) were referred through a consultant paediatrician.
Conclusion
We identified deficits in performing and interpreting the Graf method of ultrasound examination. A total of 64% of referred pathological hips turned out to be physiological configurations in our control examination. The future goal should be to increase anatomical knowledge of the newborn hip and ensure the correct use of Graf ultrasound method. Advanced training courses are recommended and necessary.
Level of evidence
IV
Keywords: developmental dysplasia of the hip, ultrasound, screening, neonates, quality control
Introduction
In Central Europe, developmental dysplasia of the hip (DDH) affects 2% to 4% of all births.1,2
Congenital hip dislocation has an incidence of 0.5% to 1% per 1000 births and female children seem to be more commonly affected.2,3 The aetiology of DDH is multifactorial and has not been fully elucidated. Multiple previously published studies postulate different endogenous and exogenous risk factors.4-6
In Germany the Graf method of ultrasound for screening of the neonatal hip has been performed during the U3-screening examination since 1996.7 The ‘U-screenings’ in Germany are developmental medical check-ups that begin shortly after birth and continue until 64 months of age. The U3- screening examination is performed four to five weeks after birth. This examination focuses especially on the examination of the hip joint8 and is considered the benchmark for early diagnosis of DDH in Germany.9,10 A standardized sonogram is obtained according to Graf’s checklist.11,12 The alpha-angle, which is the measurement of the bony roof of the acetabulum, and the beta-angle which measures the cartilaginous roof are measured according to three anatomically defined lines.11
There is consensus in the literature that early initial diagnosis with direct treatment during the first weeks of life significantly reduce long-term complications.7,13,14
During everyday care, we recognized an increase in the number of children referred to our special consultation hour for the pathological newborn hip, but the prescription of abduction braces and application of Fettweis casts did not seem to increase.
The goal of the current study was to evaluate the quality of referral diagnosis as an indicator of persisting lack of knowledge in how to correctly perform the Graf method of ultrasound in the ambulant care sector. We also investigated the necessity of treatment for the referred children. We performed a quantitative assessment of the target group.
Materials and methods
Our clinic is a supraregional reference centre for the treatment of DDH. A consultation hour specially for assessing developmental dysplasia of newborn hips has been established and is held weekly. A separate room with a higher ambient temperature is used for this purpose, equipped with a diaper changing table, examination table with a cradle and a probe guide system. We use the sonographic unit Sonoline G60S (Siemens, Erlangen, Germany) equipped with a 7.5-MgHz linear transducer (Fig. 1).
Fig. 1.
Examination table with cradle and probe guide system; sonographic unit Sonoline G60S (Siemens, Erlangen, Germany).
The sonographic and clinical findings are documented on standardized A4 format medical records which meet the legal requirements in Germany according to section 135, paragraph 2 in the German Criminal Code (§ 135 Abs. 2 SGB V).13
The medical history focuses on certain features of birth, including breech presentation, premature delivery, natural birth or caesarean section and oligohydramnios. The clinical examination focuses on limitation in hip abduction, leg-length discrepancy in 90° hip and knee flexion and presence of Ludloff’s sign. The feet of the newborn are examined for malformations.
The sonographic classification according to Graf is documented for each hip. The bony and cartilaginous form, shape of the lateral bony rim and alpha and beta angles are noted and classified according to Graf types. A treatment recommendation is finally noted. The medical record is given to the parents, while a copy is archived at our polyclinic.
A retrospective data analysis of the routinely gathered data from the medical records was performed, in addition to analysis of referral reports to our consultation hour for developmental dysplasia of the newborn hip was performed. A total of 702 medical records for 384 patients were evaluated for between 1 April 2016 and 30 April 2019. Sonographic examination and classification were exclusively performed by the head of department (C-DP) (German Society of Ultrasound in Medicine (DEGUM) Level III). Data analysis was performed anonymously.
The inclusion criteria were all children referred to our special consultation hour from 1 April 2016 until 30 April 2019.
We excluded patients who were examined sonographically by residents. We also excluded children which were presented consultatively to the gynaecological ward within the first few days postnatal for initial screening.
The key target parameters were the sonographic Graf classification, required treatment, treatment duration and referral diagnosis.
Statistical evaluation was performed using JASP version 0.8.6.0 (University of Amsterdam, Amsterdam, Netherlands). Descriptive statistics were generated, including number of cases, percentages and means. Linear correlation analysis was performed using Pearson’s correlation coefficient, with a p-value < 0.05 considered statistically significant.
Results
Study population
The gender distribution of referred newborns showed a female predominance of 73% (n = 280) compared with 27% (n = 104) male cases. The ratio of natural births (51%) to caesarean sections (49%) was approximately equal. Of newborns, 17% (n = 59) showed a breech position (total number = 348 due to language barrier) and 51% of our patients were born preterm. In all, 5% of cases showed oligohydramnios. A positive family history of DDH was confirmed in 37% (n = 141) of cases. The mean age at initial presentation was 58.36 days (sd 65.62, range: one day to 768 days). The female case group was older (mean age 58.33 days, sd 67,44, range: one day to 768 days) compared with the male case group (mean age 44.47 days, sd 57.47, range: one day to 276 days).
Clinical examination
In all, 5% (n = 19) of referred newborns presented a pathologically limited abduction. The left hip joint was affected twice as frequently as the right hip joint. In addition, 4% (n = 15) of hip joints were unstable, and a leg-length discrepancy was found in 1.7% (n = 6) of cases. A positive Ludloff sign was noticed in 3% (n = 11) of the examined newborns. In total, 5% (n = 19) of patients presented a foot anomaly.
Sonographic examination
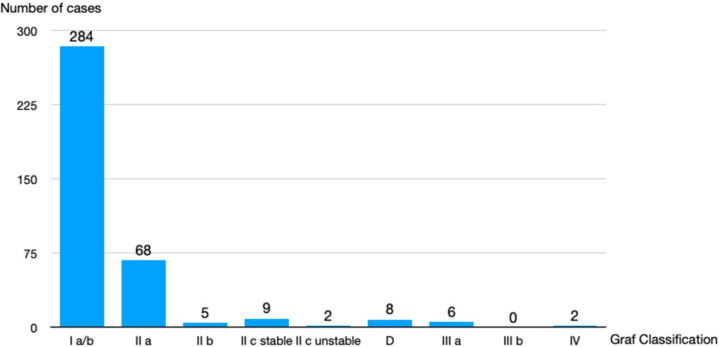
The majority (74%) of examined newborn hips (n = 284) were sonographically classified as type I a/b according to the Graf classification, with 17.7% (n = 68) presenting as type IIa. The remaining hips were classified in the following way: 1.3% type IIb (n = 5), 2.3% type IIc stable (n = 9), 0.5 % type c unstable (n = 2), 2% type d (n = 8), 1.5% type IIIa (n = 6), no type IIIb and 0.5% type IV (n = 2) (Fig. 2).
Fig. 2.
Hip types according to Graf classification.
Therapy
The majority (68%; n = 261) of referred newborns did not require treatment. Treatment with an abduction brace was required for 26% (n = 99) of newborns and an immobilization cast according to Fettweis was applied to 6% (n = 23) of newborns.
There was a statistically significant correlation between newborn age at initial diagnosis and duration of treatment (p = 0.001 and Pearson’s r = 0.678). The treatment duration for patients aged > 200 days at first presentation was twice as long as that for those children aged 100 days at first presentation. All newborns achieved a physiological hip type by the end of treatment (Fig. 3).
Fig. 3.
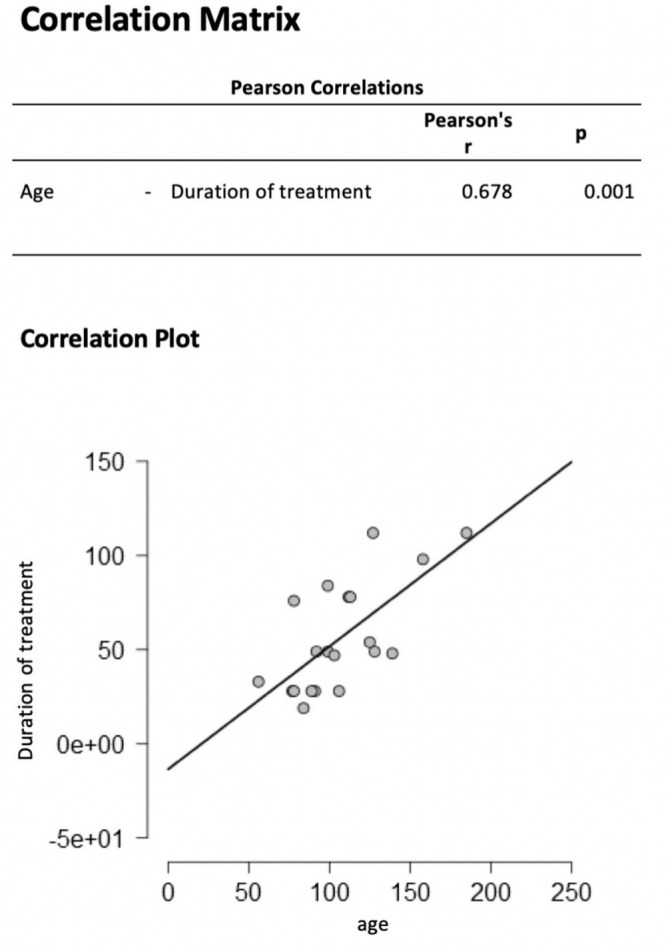
Correlation between age and duration of treatment.
Quality of referral diagnosis
In our study, 54% (n = 207) of newborns were insured with a public health insurance, while 46% (n = 177) patients had private health insurance. Of newborns covered by public insurance, 97% (n = 200) were referred to our consultation hour by a paediatrician consultant. Referral reports included the Graf classification or alpha and beta angles in 11% (n = 22) of cases.
For 64% (n = 132) of the newborns, although hips were classified as pathological by the referring consultant, our sonographic examination showed a physiological hip type according to Graf. Therefore, we could not confirm the initial referral diagnosis. Only 36% (n = 75) of referred newborn actually suffered from DDH.
Discussion
Our hypothesis was supported by our findings, as we observed a relatively poor quality of referral diagnostic accuracy. Of the referred newborns, 64% (n = 132) of hips that were classified as pathological by the referring consultant showed a physiological hip configuration in our sonographic control examination. Thus, presentation during our special consultation hour would not have been required. There are also consequences for parents, including high cost, long road trips and uncertainty about a possible malformation of their newborn.
Similar results regarding the deficits and doubt in knowledge and performance of the Graf method of ultrasound examination were recently published in the 2019 annual report by the National Association of Statutory Health Insurance Physicians.15 Furthermore, 32% of consultants failed initial approval in 2018 by the National Association of Statutory Health Insurance Physicians. The sample size of this previous study is comparable with ours (425 consultants).16
We were unable to identify any similar studies that evaluated the quality of referral diagnosis using the Graf method of ultrasound from the ambulant sector to a specialist clinic in Germany.
Incorrect or late diagnoses have severe consequences for the young patient, as growth and ossification potential decrease with age. Our study showed a statistically significant correlation between the age at initial presentation and the duration of treatment. The treatment duration for newborns aged up to 100 days was around 50 days. For newborns with a late initial presentation at 200 days, the treatment duration doubled up to 100 days. Similar results have been published by both Tschauner et al17 and Graf.11
Nowadays, patients are more willing to sue for compensation, so mistakes in performing the Graf method of ultrasound can quickly lead to high compensation claims.
The goal for the future should be increased quality of performance of Graf ultrasound examinations. Students should be introduced to this technique and resident doctors should receive further advanced training. Hospital staff should also be taught. In 2014, 24 university hospitals in Germany already offered special staff training.18
Consultant status is required to independently perform sonographic examination of the newborn hip. In order to receive consultant status as a trauma and orthopaedic surgeon, 50 sonographic examinations of the newborn hip have to be performed under the surveillance of an experienced consultant doctor. Paediatric specialist status requires 200 sonographic supervised sonographic examinations of the newborn hip.
Office-based physicians are supervised by the commission of care quality of the National Association of Statutory Health Insurance Physicians according to section 135, paragraph 2 in the German Criminal Code (§ 135 Abs. 2 SGB), where the first 12 newborn hip sonograms performed by the physician are submitted for evaluation. After initial approval, officed-based physicians are randomly tested after two years, then every five years thereafter.19
Quality management for sonographic examination of the hip at university hospitals is performed by internal commissions. In our clinic, the examiner has to perform at least 500 sonographic examinations of the respective body region, in order to validate the results recorded in our computer system.
Another option would be to establish national supraspecialized ultrasound centres, which would perform the sonographic screening of the newborn hip.
Consultants could be certified according to the quality standards of the DEGUM. Certification is given from Level I to III. In order to reach Level III, consultants have to perform 400 ultrasound examinations of the newborn hip, which ensures high quality standards. Level II and III consultants could perform the sonographic hip screening in supraspecialized ultrasound centres. Newborns with a pathological hip classification according to Graf could be referred to specialized treatment centres.
Our study has several limitations. Firstly, current research results vary with regard to the reproducibility of results obtained using Graf’s method of ultrasound. A study conducted by Orak et al20 found statistically significant differences between the sonographic results for experienced investigators, while Peterlein et al21 could not find any statistically significant difference even for investigators with very different levels of experience.
Our study is potentially biased as examinations were carried out by a single examiner (DEGUM Level III). Future studies should consider the opinion of multiple high-level examiners for even more reliable data and compare the diagnostic accuracy of multiple high experienced examiners.
Our study included a relatively small sample size over a three-year period. However, we consider the sample to be representative for the region. Future national multicentre studies with larger samples would give a better overview of the current quality of hip sonography examination. It would also help to distinguish whether the quality varies in certain areas of Germany.
Open access
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Compliance with ethical standards
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical statement
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Approval by the ethics commission was obtained on 19 March 2019.
Informed consent: Informed consent was obtained from all individual participants included in the study.
ICMJE Conflict of interest statement
None declared.
Author Contributions
FB: Data acquisition, Data analysis, Interpretation of data, Prepared manuscript for publication.
CG: Interpretation of data and its relation with previously published studies, Discussion.
SW: Interpretation of data and its relation with previously published studies.
C-DP: Study design, Data acquisition and interpretation, Prepared manuscript for publication
References
- 1. Roposch A, Liu LQ, Protopapa E. Variations in the use of diagnostic criteria for developmental dysplasia of the hip. Clin Orthop Relat Res 2013;471:1946-1954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rosendahl K, Markestad T, Lie RT. Developmental dysplasia of the hip: prevalence based on ultrasound diagnosis. Pediatr Radiol 1996;26:635-639. [DOI] [PubMed] [Google Scholar]
- 3. Ihme N, Altenhofen L, von Kries R, et al. Hip ultrasound screening in Germany. Results and comparison with other screening procedures. Orthopade 2008;37:541-549. [DOI] [PubMed] [Google Scholar]
- 4. Schmitz MR, Blumberg TJ, Nelson SE, Sees JP, Sankar WN. What’s new in pediatric hip? J Pediatr Orthop 2018;38:e300-e304. [DOI] [PubMed] [Google Scholar]
- 5. Swarup I, Penny CL, Dodwell ER. Developmental dysplasia of the hip: an update on diagnosis and management from birth to 6 months. Curr Opin Pediatr 2018;30:84-92. [DOI] [PubMed] [Google Scholar]
- 6. Mulpuri K, Schaeffer EK, Andrade J, et al. What risk factors and characteristics are associated with late-presenting dislocations of the hip in infants? Clin Orthop Relat Res 2016;474:1131-1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Nelitz M, Reichel H. Conservative treatment of hip maturation disorder. Orthopade 2008;37:550-555. [DOI] [PubMed] [Google Scholar]
- 8. Bundesausschuss Gemeinsamer. Your child’s medical records (November 2019). https://www.g-ba.de/service/versicherteninformationen/ (date last accessed 01 July 2020).
- 9. Tschauner C, Matthiessen HD, Graf R. Methodische Eckpunkte der Hüftsonografie nach GRAF. State of the art 2018. https://www.online-oup.de/media/article/2018/01/88ABD74E-DFA9-45DC-9B76-1B15E55C38D9/88ABD74EDFA945DC9B761B15E55C38D9_tschauner_1_original.pdf (date last accessed 08 December 2020).
- 10. Lauen J, Hofem R. Die Sonografie im Kindesalter. Orthopade 2006;35:596-599, 598-599. [DOI] [PubMed] [Google Scholar]
- 11. Graf R. Sonographie der Säuglinshüfte und therapeutische Konsequenzen. Stuttgart: Thieme, 2010. [Google Scholar]
- 12. O’Beirne JG, Chlapoutakis K, Alshryda , et al. International interdisciplinary consensus meeting on the evaluation of developmental dysplasia of the hip. Ultraschall in Med 2019;40:454-464. [DOI] [PubMed] [Google Scholar]
- 13. Lange A, Lange J, Thyrian R, et al. Incidence and duration of therapy of pathological hip findings in U2 and U3 examinations (SNiP study). Orthopade 2014;43:129-135. [DOI] [PubMed] [Google Scholar]
- 14. Roposch A, Liu LQ, Hefti F, Clarke NM, Wedge JH. Standardized diagnostic criteria for developmental dysplasia of the hip in early infancy. Clin Orthop Relat Res 2011;469:3451-3461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hessen Kassenärztliche Vereinigung. Durchführungsbestimmung zur Qualitätsprüfung der Ultraschalldiagnostik (01.10.2019). https://www.kvhessen.de/fileadmin/user_upload/kvhessen/Mitglieder/Qualitaet_Behandlung/GENEHMIGUNG_SONOGRAPHIE_Durchfuehrungsbestimmung_10102018.pdf (date last accessed 14 February 2020).
- 16. Qualitätsbericht Kassenärztliche-Bundesvereinigung. 2018. (January 2019). https://www.kbv.de/media/sp/KBV_Qualitaetsbericht_2018.pdf (date last accessed 11 June 2019).
- 17. Tschauner C, Klapsch W, Baumgartner A, Graf R. Maturation curve of the ultrasonographic alpha angle according to Graf’s untreated hip joint in the first year of life. Z Orthop Ihre Grenzgeb 1994;132:502-504. [DOI] [PubMed] [Google Scholar]
- 18. Peterlein C-D, Fuchs-Winkelmann S. Sonographie der Säuglingshüfte: aktueller Status an den deutschen Universitätskliniken. Orthopade 2014;43:136-142. [DOI] [PubMed] [Google Scholar]
- 19. Kassenärztliche-Bundesvereinigung. Vereinbarung von Qualitätsmaßnahmen nach § 135 Abs. 2 SGB V zur Ultraschalldiagnostik 8 (01.10.2019). https://www.kbv.de/media/sp/Ultraschallvereinbarung.pdf (date last accessed 11 June 2019). [Google Scholar]
- 20. Orak MM, Onay T, Çağırmaz T, et al. The reliability of ultrasonography in developmental dysplasia of the hip: how reliable is it in different hands? Indian J Orthop 2015;49:610-614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Peterlein CD, Schüttler KF, Lakemeier S, et al. Reproducibility of different screening classifications in ultrasonography of the newborn hip. BMC Pediatr 2010;10:98. [DOI] [PMC free article] [PubMed] [Google Scholar]