Summary box.
Limited access to vaccines by African nations as Africa has been side-lined in the race to secure vaccines for COVID-19.
Uniform thinking and planning overlook distinct country realities that may imply different COVID-19 responses, including vaccination strategies, and that local stakeholders and communities have a central role in designing and implementing successful public health interventions.
The distribution of COVID-19 vaccines should be part of an integrated and broader strategy, both to curb COVID-19 and also to improve life and well-being of the target community.
The backdrop of Africa in the COVID-19 vaccine race highlights the urgency for Africans to invest in research to ensure that strategies are adapted to the Africa context and not just imported as the COVID-19 vaccine will be.
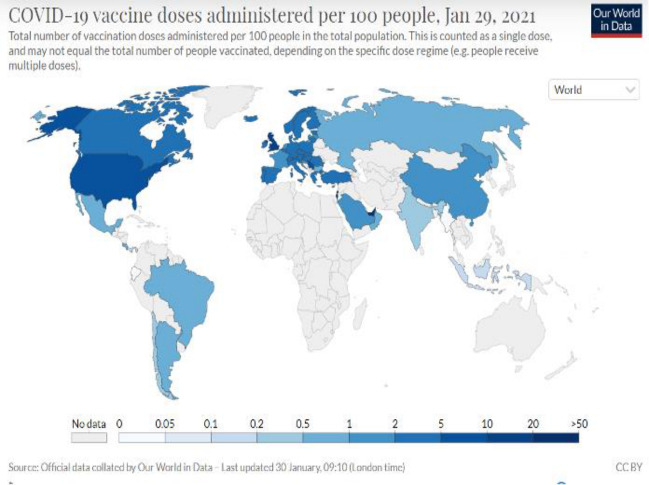
Despite pledges from world leaders for equitable access and fair allocation of COVID-19 vaccines globally, vaccine nationalism and hoarding, in particular by wealthy countries, have left Africa largely side-lined in the race to start vaccinating the most vulnerable and effectively curb the pandemic (figure 1). The African Union and Africa centre for disease control and prevention (CDC) recently announced that they were able to secure 670 million doses,1 yet delivery times are unclear. South Africa, by far the hardest hit country on the continent, just received a first shipment of a last-minute procured 1.5 million doses. Unfortunetely they had to give the Astra Zeneca doses because of the high proportion of new variants on which this vaccine is performing poorly.2
Figure 1.
Global distribution of COVID-19 vaccine doses administered (source: Coronavirus (COVID-19) Vaccinations—Statistics and Research—Our World in Data).
Nevertheless, the public discourse from health experts and politicians including in Africa continues to envision vaccination of two-thirds of the population in order to control COVID-19, as also outlined in a recent Lancet editorial.3 It assumes that the strategy of rushing towards mass-vaccination with the first available vaccines, as pursued by several wealthy countries, is both realistic and desirable everywhere. Such uniform thinking, including the focus on securing large numbers of doses, overlooks that distinct country realities may require different COVID-19 responses, including vaccination strategies, and that local stakeholders and communities have a central role in designing and implementing successful public health interventions.
While COVID-19 vaccines undoubtedly will have a critical role, they are no silver bullets. As we know from experience working in West and Central Africa, including responding to Ebola epidemics, there is a huge gap between having a vaccine authorised and deploying vaccination as an effective public health intervention. We already know that vaccine availability is constrained that different vaccines may have quite different profiles, and that the epidemic does not spread evenly, including with new variants arising. We must now design COVID-19 vaccination strategies that are fit-for-purpose to curb the pandemic in the local context and benefit the most vulnerable and exposed. As a first step, we are starting sero-surveillance studies in Côte d’Ivoire, Democratic Republic of Congo and Cameroon to better understand which populations are most affected and to guide our prevention and control efforts.
Beyond limited access, current vaccines also have significant constraints. In the race to develop a vaccine, the focus was on safety and efficacy in reducing symptomatic COVID-19, while deployability and impact on community transmission were not prioritised.4 As a result, the first available vaccines require stringent cold-chains, necessitate two doses and have limited shelf-lives which pose challenges for roll-out anywhere.5 More easy-to-use vaccines are now becoming available, but their efficacy is lower. It remains to be seen how the emergence and spread of new SARS-CoV-2 variants will impact the effectiveness of any of the vaccines. Without knowing moreover how long protection lasts, nor whether these vaccines break transmission, African countries with focal transmission may consider more targeted vaccination strategies with a chosen vaccine, instead of aiming at broad coverage, especially as COVID-19 recovery rates in certain West-African countries are as high as 95%.6 To this end, pragmatic implementation trials that compare different vaccines and vaccination strategies may be warranted, and potentially more effective.
At the same time, countries may wish to implement adapted testing algorithms to quickly identify infected persons and build targeted care, containment and/or vaccination strategies around them. For instance, in Cameroon, faced with a limited capacity of PCR-based testing, health authorities chose early on to evaluate and use rapid diagnostic tests that are better adapted to the Cameroonian environment, in particular for rural areas. To date, four out of 10 reported cases have been diagnosed by antigenic rapid tests.6
While it was possible, at considerable effort and cost, to deliver Ebola vaccines in West and Central Africa under cold chain using mobile −80°C freezers, it significantly complicated the roll-out in remote and rural areas. One of the major challenges beyond logistics was community engagement.7 For vaccines to be accepted by the communities, people need to understand and be convinced that they will benefit both individually and collectively, which is especially complicated when certain people are to receive priority access over others. Even in countries like France vaccine hesitancy and resistance is significant. Following the debate on Africans being ‘Guinea pigs’ for vaccine trials8 and the growing resistance against vaccines, especially HPV, we can expect challenges in how COVID-19 vaccines are received in Africa. Rather than racing towards massive deployment of vaccines as they become available, we must take the time to integrate communities in the response and ensure ownership of the implemented measures. Inappropriately, deployed vaccines could do more harm than good by jeopardising the already fragile acceptance of vaccination programmes.
Given the unprecedented amounts of funds being mobilised for responding to the pandemic, it is imperative to also consider which interventions besides COVID-19 vaccination can improve life and well-being of a given community and restore normal activities. Curbing COVID-19 cannot be a stand-alone goal, it must be one element within a broader health strategy and ideally bringing longer term improvements to people’s health and access to care. For instance, in many countries including Democratic republic of Congo (DRC), measles vaccination campaigns were interrupted because of COVID-19. It is estimated that over 117 million children globally may miss out on receiving life-saving measles vaccines.9 Similarly, COVID-19-related disruption of malaria control in Africa could almost double malaria mortality in 2020 and beyond.10 To avoid a reversal of two decades of progress, other community health measures such as measles vaccination and distribution of insecticide-treated mosquito nets could be implemented alongside COVID-19 vaccination. The massive resource mobilisation for COVID-19 vaccines could also be turned into an opportunity to start addressing other long-neglected health issues, for instance access to essential medicines including for tropical neglected and non-communicable diseases.11
Whether globally or in Africa, COVID-19 vaccines are but one pillar in a country’s response to the pandemic. To be successful, response strategies must be based on local needs, capacities, epidemiology and guided by community engagement. It must also take a broader look at improving health outcomes, not just focus on COVID-19. Appropriate vaccination will then complement other measures including testing and tracing, distancing, handwashing and masks to limit virus transmission and restore social and economic life. The challenges faced by African countries in acquiring COVID-19 vaccine highlight the urgency to invest in research to ensure that strategies are adapted to the Africa context and not just imported as the COVID-19 vaccine will be.
Footnotes
Handling editor: Seye Abimbola
Twitter: @yap.boum2
Contributors: YBII, AO, ET and CO have written the commentary.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; internally peer reviewed.
Data availability statement: There are no data in this work.
References
- 1.AfricaNews . African union secures additional 400 million vaccine doses. Available: https://www.africanews.com/2021/01/28/african-union-secures-additional-400-million-vaccine-doses//
- 2.BBC . Coronavirus: South Africa rolls out vaccination programme. Available: https://www.bbc.com/news/world-africa-55675806
- 3.The Lancet . An African plan to control COVID-19 is urgently needed. Lancet 2020;396:1777. 10.1016/S0140-6736(20)32580-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Torreele E. Business-as-usual will not deliver the Covid-19 vaccines we need. Development 2020;63:191–9. 10.1057/s41301-020-00261-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wallace-Wells D. America’s vaccine rollout is already a disaster. New York magazine, 2020. Available: https://nymag.com/intelligencer/article/americas-vaccine-rollout-disaster.html
- 6.COUSP . Rapport de situation COVID-19 au Cameroun N°61, 2020. [Google Scholar]
- 7.Osterholm M, Moore K, Ostrowsky J, et al. The Ebola vaccine team B: a model for promoting the rapid development of medical countermeasures for emerging infectious disease threats. Lancet Infect Dis 2016;16:e1–9. 10.1016/S1473-3099(15)00416-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reuters . 'We are not guinea pigs,' say South African anti-vaccine protesters, 2020. Available: https://www.reuters.com/article/uk-health-coronavirus-safrica-vaccine/we-are-not-guinea-pigs-say-south-african-anti-vaccine-protesters-idUKKBN2426SA
- 9.CDC . Statement by the measles & rubella initiative, 2020. Available: https://www.cdc.gov/globalhealth/measles/news/covid-impact-on-measles-vaccination.html
- 10.Weiss DJ, Bertozzi-Villa A, Rumisha SF, et al. Indirect effects of the COVID-19 pandemic on malaria intervention coverage, morbidity, and mortality in Africa: a geospatial modelling analysis. Lancet Infect Dis 2021;21:59–69. 10.1016/S1473-3099(20)30700-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Murphy A. Can we do for other essential medicines what we are doing for the Covid-19 vaccine? BMJ Glob Health 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]