Abstract
A previously fit and well 76-year-old man, presented with distal lower limb sensory symptoms suggestive of peripheral sensory neuropathy, associated with positive anti-MAG antibodies (myelin associated glycoprotein) and IgM paraprotein. Bone marrow biopsy showed lymphoplasmocytoid lymphoma (Waldenstrom’s macroglobulinaemia, WM), consequently positive for MYD88 mutation. He subsequently developed medullary carcinoma of the thyroid, most likely secondary to WM. He underwent a successful total thyroidectomy and four treatment doses of rituximab, which proved beneficial. He is currently stable and under multidisciplinary monitoring. His sensory symptoms have improved following rituximab treatment and his WM is under control.
Keywords: thyroid disease, haematology (incl blood transfusion), monoclonal gammopathy of undetermined significance associated neuropathy, peripheral nerve disease, clinical neurophysiology
Background
This case highlights two key points: (1) that anti-MAG can be associated with abnormal paraprotein levels, which can lead to neuropathies and (2) that paraprotein neuropathies can be associated with Waldenstrom’s macroglobulinaemia (WM) and other blood neoplasms, which in turn, can be directly linked to ‘second’ cancers, such as thyroid medullary carcinoma. This case highlights the importance of having a high clinical suspicion for anti-MAG neuropathies and of thoroughly investigating for underlying neoplasms in such cases. It highlights the association between neurological, haematological and endocrine disorders and how we must keep an open mind about the possible links with other specialties when treating our patients.
Case presentation
A 76-year-old man, previously fit and well with no medical history nor regular medications, presented with a 4-month history of persistent numbness in both feet that had gradually spread to his ankles over the last month. Concurrently, his gait and balance started to deteriorate, most prominently when closing his eyes or when entering a dark room. The patient denied pain and upper limb involvement.
On examination, there was pallhypesthesia on the dorsal aspects of both feet with complete absence of vibration perception on the toes of the left foot. He had a positive Romberg test and abnormal tandem gait. There was no evidence of high-stepping gait. His strength was preserved in all four limbs. Both patellar reflexes were reduced and Achilles tendon reflexes were absent bilaterally. All upper limb reflexes were present and symmetrical. He was cognitively intact with no evidence of cerebellar nor cranial nerve dysfunction.
He was diagnosed with a sensory peripheral neuropathy and was sent for a nerve conduction studies and MRI of the spinal cord to exclude posterior column involvement. The latter was entirely normal and the former revealed a large fibre demyelinating sensory and motor polyneuropathy without conduction block; the distal lower limb sensory potentials were unobtainable and the distal motor latencies were prolonged (tables 1 and 2). Cerebrospinal fluid (CSF) analysis showed an elevated protein level of 1.8 g/L, but was otherwise normal, with a negative PCR.
Table 1.
Typical nerve conduction findings seen with axonal and demyelinating lesions
| Axonal | Demyelinating | |
| Sensory loss | Small or absent | Small or absent |
| Distal motor latency | Normal or slightly prolonged | Prolonged |
| CMAP (compound motor action potential) amplitude | Small | Normal |
| Conduction block/temporal dispersion | Not present | Present |
| Motor conduction velocity | Normal or slightly reduced | Notably reduced |
| F waves latency | Normal or slightly prolonged | Significantly prolonged |
Table 2.
Differences between axonal/anterior horn and peripheral neuropathies
| Evoked potentials: CMAP/SNAP | Nerve conduction velocity | |
| Axonal/anterior horn disorder | Small CMAP | Normal |
| Peripheral nerve disorder | Small CMAP+SNAP | Slow |
CMAP, compound motor action potential; SNAP, sensory nerve action potential.
Initial blood tests including Hb1Ac for diabetes and vitamin B12 and folate, were within normal limits. Protein electrophoresis (April 2019; see online supplemental table 1) was abnormal, showing an increased IgM (4.46 g/L), increased total paraprotein (6.9), increased gamma protein 1 (3.3 g/L) and increased B-2 paraprotein (3.6 g/L). This led to a diagnosis of IgM-MGUS (monoclonal gammopathy of uncertain significance) sensorimotor distal peripheral polyneuropathy. His white cell count, renal function and electrolytes were normal. A repeat protein electrophoresis (July 2019; see table 1) showed increased levels of IgM. Anti-MAG levels were very high at 135, 631 BTU.
bcr-2020-240242supp001.pdf (166.9KB, pdf)
Five months later (September 2019), his repeat white cell count, platelets, neutrophils, kidney and liver function were all within normal range and there was no evidence of lymphadenopathy nor of hepatosplenomegaly. CT of chest, abdomen and pelvis was normal. However, CT neck with contrast revealed a 13 mm right thyroid nodule with calcification. Calcitonin levels were very high, at 842 ng/L. Follow-up thyroid ultrasound showed U4 morphology and subsequent fine-needle aspirate (FNA) with core biopsy was suggestive of a medullary carcinoma. He underwent total thyroidectomy (December 2019) with a follow-up calcitonin level of 155 ng/L.
Due to the very high levels of anti-MAG, a bone marrow biopsy was done, with the aim of excluding an underlying plasma-cell dyscrasia. The aspirate morphology showed 4% plasma cells and 8% mature lymphocytes with occasional lymphoplasmocytoid forms; flow cytometry showed 2%–3% B-cells and 0.6% plasma cells both with a predominance of kappa chain detected. These findings were suggestive of a neoplastic B-cell/plasma disorder. The bone marrow trephine morphology showed 10% B-cells with 5% kappa light chain-predominant plasma cells. In conjunction with the flow cytometry, these findings were highly suggestive of a low-level bone marrow involvement by a low-grade B cell lymphoma. The differential diagnosis was a lymphoplasmocytoid lymphoma. Subsequent genetic testing revealed positive MYD88 mutation (c.794T>Cp. (Leu265Pro)) which was supportive of a lymphoplasmocytoid lymphoma (WM).
Following the bone marrow biopsy, he was diagnosed with IgM-paraprotein sensory polyneuropathy associated with positive anti-MAG and WM and was started treatment with rituximab in January 2020 (weekly dose for 4 weeks), with no side effects and improvement of his sensory symptoms. Follow-up protein electrophoresis (April and June 2020, see table 1) showed mild reduction in IgM levels (although still above upper limit) and elevated B2-paraprotein. The repeat anti-MAG levels came down to 89 451 BTU. He has remained stable and under surveillance ever since with no new clinical symptoms.
Differential diagnosis
The distal lower limb numbness was clinically suggestive of a length-dependent sensory neuropathy, which has a wide differential diagnosis. The nerve conduction study confirmed the clinical suspicion, showing a sensorimotor peripheral neuropathy affecting mainly the distal aspect of the lower limbs. After excluding common causes such as diabetes and vitamin B12 deficiency, he was investigated for less common conditions such as autoimmune, paraneoplastic and metabolic disorders. The protein electrophoresis was very helpful as it showed an abnormal IgM paraprotein, suggestive of an underlying plasma cell dyscrasia, which can cause peripheral neuropathies (both sensory, motor and sensorimotor). In fact, IgM gammopathy is more frequently associated with neuropathies than IgA or IgG gammopathies.
On the other hand, although the patient did not present with tremor—which is frequently associated with antibody-mediated peripheral neuropathies, especially anti-MAG. He was tested for anti-MAG levels as this antibody can be present in association with elevated paraprotein, especially in the context of an underlying idiopathic polyneuropathy of recent onset. We know that neuropathies can develop if the M-protein binds to peripheral nerve antigens, especially to MAG, which is a self-antigen.
The association between IgM monoclonal gammopathy and the very elevated anti-MAG levels were considered as the underlying cause of the sensorimotor neuropathy. That is when he was diagnosed with IgM paraprotein sensorimotor neuropathy associated with anti-MAG.
An elevated paraprotein in blood is suggestive of a haematological malignancy, hence, the referral to the haematologist, who carried out a bone marrow biopsy, which ultimately detected a lymphoplasmocytoid lymphoma. IgM MGUS and WM are usually associated with kappa light chain, which was consistent in this patient. WM tends to cause a length-dependent large-fibre sensory demyelinating or axonal neuropathy. This patient had a sensorimotor demyelinating polyneuropathy. When there are lambda light chains instead of kappa, there are two differential diagnosis: (1) light chain amyloidosis (AL) and (2) POEMS (polyneuropathy, organomegaly, endocrinopathy, protein M and skin changes).
WM carries a risk of causing a ‘second’ neoplastic disorder, most commonly, thyroid cancer. Therefore, it was important to exclude solid-tumours. The US and FNA of the thyroid demonstrated the existence of a medullary carcinoma, which was successfully treated with a complete thyroidectomy and post-operative levothyroxine.
Treatment
For sensory neuropathy, he received treatment with symptomatic management with gabapentin, with little improvement. Following the bone marrow biopsy, he was given rituximab (four weekly infusions of 375 mg/m2, throughout the month of January 2020) with good results. The medullary carcinoma of the thyroid was managed surgically, with total thyroidectomy and postoperative oral levothyroxine.
Previous studies have shown that IgM anti-MAG neuropathy usually responds poorly to most conventional immunomodulatory therapies.1 Dalakas et al2 published the results of using rituximab in these patients: (1) depletion of B cells lasting for more than 6–8 months and (2) there was a reduction in IgM by 34% and of anti-MAG in 50%. In the vast majority of cases, the clinical improvement is evident after roughly 3 months.
Outcome and follow-up
He has subsequently been referred for follow-up by neurology, haematology and endocrinology, likely on a 3–6 months basis, depending on his clinical status. He will continue to have routine bloods every 6 months to monitor paraprotein levels, anti-MAG levels, calcium, renal and liver function. He will have a repeat nerve conduction study to assess for any changes with regards to the previous assessment and to correlate those findings with his clinical presentation at the time.
Discussion
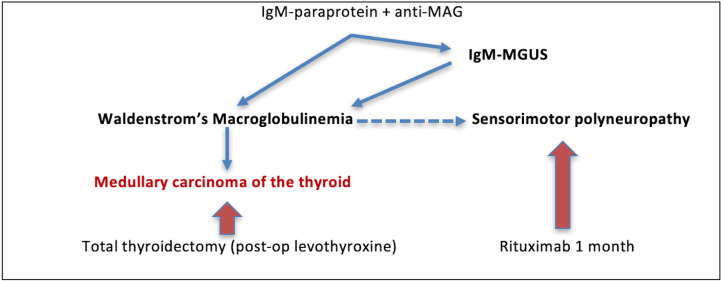
As described in figure 1, the main precipitating problems in this patient were the IgM paraprotein and the anti-MAG antibodies, which eventually, directly led to two other problems: (1) sensorimotor peripheral polyneuropathy and (2) WM. The latter then led to the development of the medullary carcinoma of the thyroid.
Figure 1.
Sequence of events leading to the sensorimotor polyneuropathy and to Waldenstrom’s macroglobulinaemia and medullary carcinoma. MGUS, monoclonal gammopathy of uncertain significance.
Roughly 60% of patients with IgM monoclonal gammopathy develop sensorimotor peripheral polyneuropathy3 4 (as compared with 30% in IgG and 10% in IgA).5 The M-protein has the potential of binding to specific antigens located on the surface of peripheral nerve,6 7 such as myelin associated glycoprotein (MAG), which acts as a self-antigen.8
Anti-MAG neuropathies are usually associated with tremor; however, this was not the case in this patient. The neuropathy can present in one of three options, previously described by Magy et al9: (1) sensory ataxic neuropathy (most common), (2) purely subjective (usually painful) neuropathy and (3) a sensorimotor neuropathy. Our patient presented with a combination of these subtypes: he had sensory ataxia with positive Romberg testing and also a nerve conduction study that revealed sensory and motor involvement, despite not having clinical weakness on examination. This case adds to the growing evidence that paraprotein/anti-MAG neuropathies are highly variable in their clinical presentation.
MGUS has the potential to evolve into: MGUS, multiple myeloma, WM, POEMS syndrome or AL. This patient evolved into WM.
Interestingly, neither the IgM was elevated that much nor was the haemoglobin reduced. Canepa10 reported a similar case of IgM-paraprotein demyelinating sensorimotor polyneuropathy who developed WM in the context of having IgM >20 g/L and erythrocyte sedimentation rate >40 mm/hour, which, according to Klein et al,11 were above the cut-off level of IgM (>1830 mg/dL or 18.3 g/L) and below that of haemoglobin (<126 g/L): values that represent a 71% sensitivity and an 88% specificity for predicting WM independent of nerve conduction studies. In our case, the IgM levels are only mildly elevated, between 4.46 and 3.2 g/L, nowhere near Klein’s suggested cut-off. The haemoglobin was also consistently within normal range. Nevertheless, he developed WM. This indicates that although Klein’s values are important, patients can still develop malignancies with values of IgM and haemoglobin below those cut-off points.
The bone marrow analysis was very helpful in reaching a conclusive diagnosis. The bone marrow trephine morphology showed 10% B-cells with 5% kappa light chain-predominant plasma cells and further genetic analysis revealed a positive MYD88 mutation (c.794T>Cp. (Leu265Pro)) which was supportive of a lymphoplasmocytoid lymphoma, WM.
WM, in turn, can cause other neoplastic disorders, that is, ‘secondary malignancies’ (SM). Varettoni et al12 described an increased risk of diffuse large B-cell lymphoma (DLBCL), myelodysplastic syndrome/acute myeloid leukaemia and brain cancer. From a cohort of 230 patients with WM, 32 developed SMs, of which only 1 had thyroid cancer (the subtype was not specified). Castillo et al13 in the largest population-based analysis evaluating the incidence of SMs in patients with WM versus general population, found an increased incidence of lung cancer, bladder, kidney and thyroid cancer, melanoma DLBCL and acute leukaemia. However, among these, the most common where lung, kidney and skin (melanoma). In this case we report medullary carcinoma of the thyroid associated with WM.
Interestingly, the WM and the medullary carcinoma where only discovered following investigations for a sensory polyneuropathy associated with an abnormal protein electrophoresis and positive anti-MAG, which highlights the importance of ruling out neoplastic disorders in such patients. Both neoplasms were detected and treated promptly, with good outcomes and good prognosis. This would not have been the case had the patient not been further investigated following the polyneuropathy diagnosis.
Patient’s perspective.
I was diagnosed with peripheral neuropathy/MGUS by a neurologist after suffering numbness in my toes. I was then referred to a haematologist, who carried out blood tests and a bone marrow biopsy and made me aware that they needed to check for a paraprotein (abnormal protein) in my blood and in may need to have chemotherapy treatment. The haematologist provided me with various sheets of information on the condition which I found very helpful; I also did some research to enable me to understand it, and deal with it in the best possible way.
The tests results did reveal I had a rare condition which would require chemotherapy in order to improve or slow the progression, so it was quite a shock. I was immediately introduced to a specialist nurse who would be looking after my care, and who explained procedures etc in great detail—which I found very reassuring. At a prearranged date I attended a review with the haematologist, to make sure everything was well and in place before my first chemotherapy session. I was then given an infusion of rituximab on a weekly basis for 4 weeks, which I did not find unpleasant or suffer any side effects whatsoever—after initially feeling great trepidation. The staff in the unit were exceptional with their professionalism, kindness and caring, nothing was too much trouble if I had any queries or worries.
My condition has slightly improved, I am experiencing a bit more flexibility, and I am doing the necessary foot exercises in order to maintain it, along with lots of walking. I am determined to be positive and get on with my life.
Learning points.
IgM paraprotein with or without anti-MAG can cause sensory, motor or sensorimotor neuropathy, which can be treated with rituximab,
Anti-MAG neuropathies are typically associated with tremor, however, this is not always present, such as in this case.
IgM paraprotein neuropathy with or without anti-MAG antibodies should be further investigated, looking for haematological neoplastic disorders, such as Waldenstrom’s macroglobulinaemia (WM).
Patients with WM are at risk of developing a ‘second’ cancer, which is most frequently a solid-tumour, mainly from the thyroid.
Footnotes
Contributors: CC designed, drafted the first manuscript and is the consultant responsible for the patient. YY revised and synthesised the final manuscript submitted for publishing. Figure 1 is an original image composed by CC. All authors have approved the final version.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Lunn MP, Nobile-Orazio E. Immunotherapy for IgM anti-myelin-associated glycoprotein paraprotein-associated peripheral neuropathies. Cochrane Database Syst Rev 2016;10:742–4. 10.1002/14651858.CD002827.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dalakas MC, Rakocevic G, Salajegheh M, et al. Placebo-controlled trial of rituximab in IgM anti-myelin-associated glycoprotein antibody demyelinating neuropathy. Ann Neurol 2009;65:286–93. 10.1002/ana.21577 [DOI] [PubMed] [Google Scholar]
- 3.Kelly JJ. Peripheral neuropathies associated with monoclonal gammopathies of undetermined significance. Rev Neurol Dis 2008;5:14–22. [PubMed] [Google Scholar]
- 4.Yeung KB, Thomas PK, King RH, et al. The clinical spectrum of peripheral neuropathies associated with benign monoclonal IgM, IgG and IgA paraproteinaemia. Comparative clinical, immunological and nerve biopsy findings. J Neurol 1991;238:383–91. 10.1007/BF00319857 [DOI] [PubMed] [Google Scholar]
- 5.Latov N, Hays AP, Sherman WH. Peripheral neuropathy and anti-MAG antibodies. Crit Rev Neurobiol 1988;3:301–32. [PubMed] [Google Scholar]
- 6.Ramchandren S, Lewis RA. An update on monoclonal gammopathy and neuropathy. Curr Neurol Neurosci Rep 2012;12:102–10. 10.1007/s11910-011-0237-4 [DOI] [PubMed] [Google Scholar]
- 7.Stork ACJ, Jacobs BC, Tio-Gillen AP, et al. Prevalence, specificity and functionality of anti-ganglioside antibodies in neuropathy associated with IgM monoclonal gammopathy. J Neuroimmunol 2014;268:89–94. 10.1016/j.jneuroim.2014.01.012 [DOI] [PubMed] [Google Scholar]
- 8.Braun PE, Frail DE, Latov N. Myelin-associated glycoprotein is the antigen for a monoclonal IgM in polyneuropathy. J Neurochem 1982;39:1261–5. 10.1111/j.1471-4159.1982.tb12563.x [DOI] [PubMed] [Google Scholar]
- 9.Magy L, Kaboré R, Mathis S, et al. Heterogeneity of polyneuropathy associated with anti-MAG antibodies. J Immunol Res 2015;2015:1–9. 10.1155/2015/450391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Canepa C. Waldenstrom-associated anti-MAG paraprotein polyneuropathy with neurogenic tremor. BMJ Case Rep 2019;12:e228376. 10.1136/bcr-2018-228376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Klein CJ, Moon J-S, Mauermann ML, et al. The neuropathies of Waldenström's macroglobulinemia (WM) and IgM-MGUS. Can J Neurol Sci 2011;38:289–95. 10.1017/S0317167100011483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Varettoni M, Tedeschi A, Arcaini L, et al. Risk of second cancers in Waldenström macroglobulinemia. Ann Oncol 2012;23:411–5. 10.1093/annonc/mdr119 [DOI] [PubMed] [Google Scholar]
- 13.Castillo J, Olszewski A, Hunter Z. Incidence of secondary malignancies among patients with Waldenstrom macroglobulinemia: an analysis of the SEER database. SEER Database 2015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bcr-2020-240242supp001.pdf (166.9KB, pdf)