Editor,
A 65-year-old male non-smoker presented with a 2-month history of weight loss, fever and back pain. Bloods noted normocytic anaemia, elevated ESR (130mm/hr) and normal renal indices. To exclude malignancy, a CT chest, abdomen and pelvis was requested. This revealed a paravertebral mass extending from T6-T11 with significant uptake on subsequent CT-PET (Figure 1). CT guided biopsy was not possible due to the location of the mass. Endobronchial ultrasound guided biopsy of the mass was negative for malignancy, yet thisremained likely. Spinal referral was made for consideration of a biopsy/removal of the mass.
Figure 1.

CT-PET showing uptake in the prevertebral and bilateral paravertebral region, (SUV max 11.92), PET avid right hilar nodes (SUX max 6.7) with encasement of the descending aorta, associated with increased uptake.
The patient was readmitted with acute kidney injury (urea 16.5mmol/L, creatinine 123pmol/L, eGFR 51ml/min). Presuming pre-renal failure, intravenous fluids were given with no improvement. Renal tract ultrasound was normal. Urine dipstick demonstrated significant blood and protein. Vasculitis screen showed PR3 ANCA of >8.0 and cANCA 20, prompting a presumptive diagnosis of granulomatosis with polyangitis (GPA). On renal biopsy, focal segmental glomerulosclerosis, active crescents and C3 positivity on immunofluorescence confirmed the diagnosis (Figure 2). Patient was pulsed with methylprednisolone before commencing oral cyclophosphamide and prednisolone. At 4 month follow up the patient's renal function had normalised and repeat imaging showed complete resolution of the mass.
Figure 2.
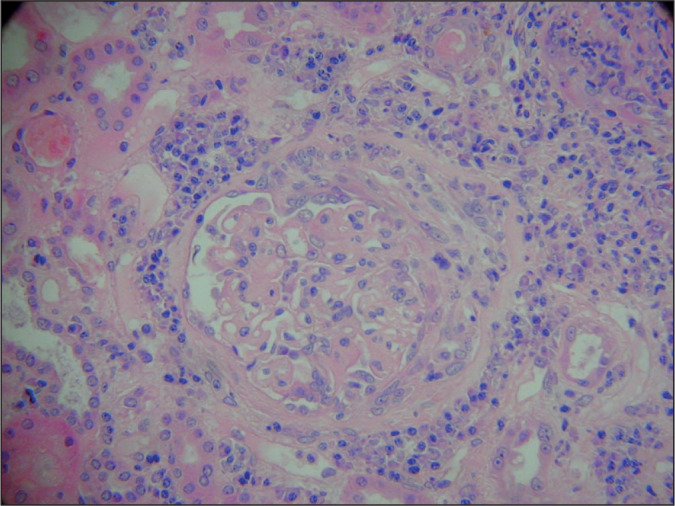
Histology showing rapidly progressive necrotising glomerulonephritis. In the image we can see crescents obliterating the glomerular space and fibrin deposits between proliferated cells. In the centre of the image compressed capillary loops are also seen. These findings are classic for Rapidly progressive glomerulonephritis.
GPA is a potentially lethal multisystem disorder of unknown aetiology which typically presents as a small-vessel vasculitis and necrotising granulomatous inflammation of the kidneys and respiratory tract. Anomalous manifestations exist with cutaneous, ocular, musculoskeletal, neurological and cardiac presentations previously described. GPA presenting as tumour like masses is less well documented. To date, GPA tumour like lesions have been noted in the orbits, nasal passages, lungs and right ventricle with a predilection for breast and renal masses.1-3 Notably, there appears a close temporal association between GPA and renal cell carcinomas yet the immunopathologic mechanism remains unclear.4 Within the literature there exists only one previous case of GPA presenting as a paraspinal mass with this patient exhibiting synchronous renal and paraspinal masses.5 To the authors knowledge, our case represents the only description of a solitary GPA paraspinal mass.
Those with suspected GPA require serum anti-neutrophil cytoplasmic antibody (ANCA) testing. Whilst not wholly pathognomonic, elevated cANCA and PR3 levels strongly support a diagnosis of GPA in patients with moderate/high probability scores. A negative ANCA does not exclude the diagnosis therefore ANCA testing is not advised for monitoring disease activity. Definitive diagnosis requires evidence of necrotising vasculitis on biopsy. Many biopsy sites exist however renal samples are considered superior.
As per the European Renal Association and European Vasculitis Society, management of GPA is in accordance with symptom severity at diagnosis. ‘Non organ threatening disease' requires treatment with methotrexate and glucocorticosteroids. Glucocorticoids with either cyclophosphamide or rituximab are recommended in “organ or life threatening disease” which includes tumour like lesions given their potential to compress surrounding structures. Plasma exchange is only required in the event of pulmonary haemorrhage or rapidly progressive renal failure. This case highlights the diagnostic difficulty surrounding GPA and its ability to present as tumour like masses. In such cases it is imperative to exclude malignancy, yet this may generate diagnostic delays. The authors therefore argue GPA should be considered in any patient with a mass and evidence of multi-system disease.
Patient consent was obtained for the publication of this case.
Footnotes
Conflicts of Interest: No conflicts of interest
UMJ is an open access publication of the Ulster Medical Society (http://www.ums.ac.uk).
REFERENCES
- 1.Rabahi MF, Coelho LB, Borges ED, Lemes MS, Castro WM, Carneiro SD. Lung pseudotumor as the initial presentation of Wegener's granulomatosis. J Bras Pneumol. 2009;35(4):392–5. doi: 10.1590/s1806-37132009000400015. [DOI] [PubMed] [Google Scholar]
- 2.Spanuchart I, Zungsontiporn N, O-charoen P, Changcharoen B, Bolger DT. Granulomatosis with polyangiitis: a case of nasal mass, necrotic lung, and normal kidneys. Hawaii J Med Public Health. 2015;74(9 Suppl 2):27–9. [PMC free article] [PubMed] [Google Scholar]
- 3.Kariv R, Sidi Y, Gur H. Systemic vasculitis presenting as a tumorlike lesion. Four case reports and an analysis of 79 reported cases. Medicine. 2000;79(6):349–59. doi: 10.1097/00005792-200011000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Tatsis E, Reinhold-Keller E, Steindorf K, Feller AC, Gross WL. Wegener's granulomatosis associated with renal cell carcinoma. Arthritis Rheum. 1999;42(4):751–6. doi: 10.1002/1529-0131(199904)42:4<751::AID-ANR19>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 5.Timlin H, Phillips M, Hackworth J, Geetha D. Renal and paraspinal mass in a patient with granulomatosis with polyangiitis: does biopsy of one mass reflect pathology in the other. J Rheumatol Arthritic Dis. 2017;2(2):1–2. [Google Scholar]


