Abstract
Background:
Fractures of the metacarpals and phalanges account for more than half of all upper extremity fractures sustained by competitive athletes.
Purpose:
To determine which management strategy is best for expediting return to preinjury levels of competition in adult athletes with metacarpal and/or phalangeal fractures.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A methodology compliant with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) was used. A custom search strategy was designed and applied to MEDLINE and In-Process, Embase, EMCARE, and CINAHL.
Results:
Overall, 3135 records were identified, of which 8 met full inclusion criteria. All patients returned to preinjury levels of competition, at a mean of 30.6 days for phalangeal fractures and 21.9 days for metacarpal fractures. Meta-analysis demonstrated delayed return-to-sport time for operatively managed metacarpal fractures as compared with nonoperatively managed ones (28.5 vs 22.0 days). All studies were of fair or poor quality, and none were randomized.
Conclusion:
Optimal management strategies for athletes with metacarpal and phalangeal fractures remain equivocal. Injury, treatment, and sport-specific factors may confound results and preclude accurate estimation of optimal treatment strategies at present.
Keywords: hand, metacarpus, fractures, return to sport, athletic performance
Fractures of the metacarpals and phalanges account for 39.2% of all sports-related fractures1 and specifically for 54.8% of upper limb fractures sustained by competitive athletes.6 Injuries are frequently caused by direct blunt trauma and falling onto a clenched fist,12 with a high incidence in contact, ball-handling, and combat sports.25,26
In managing metacarpal and phalangeal fractures, care aims to support return to preinjury levels of competition in the shortest time possible. Expedited return to play may prevent deconditioning, stiffness, and muscle atrophy; maximize playing time during the competitive season; and allow training in the off-season.15
A variety of operative and nonoperative treatment strategies have been proposed to achieve anatomic restoration, fracture stability, and early rehabilitation in metacarpal and phalangeal fractures, all of which facilitate early return to play in athletes. Nonoperative management of closed simple metacarpal injuries has been traditionally favored,26 although open reduction and plate fixation provides fracture stability and may permit early active mobilization.10
Despite the relatively high incidence of metacarpal and phalangeal fractures in athletes, there is a lack of consensus regarding the optimal management strategy for return to play.16 The aim of this systematic review was to determine which management strategy is best for expediting return to preinjury levels of competition in adults participating in sports who have sustained closed fractures of the metacarpals and/or phalanges during sporting activity.
Methods
This systematic review was developed, conducted, and reported in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement,18 and the protocol was registered in PROSPERO (Prospective Register of Systematic Reviews; CRD42019152448).3
Eligibility Criteria
All randomized controlled trials, clinical trials, cohort studies, comparative studies, case series, and case reports were eligible for study inclusion. Review articles, meta-analyses, descriptions of operative technique that did not present original clinical data, and cadaveric and animal studies were excluded.
Participants
Included in this study were adults participating in amateur or professional sports with acute metacarpal and/or phalangeal fractures sustained during sporting activity (<6 weeks between injury and definitive management). Adults with metacarpal and/or phalangeal fractures sustained during nonsporting activities were excluded. Also excluded were patients with existing metacarpal and/or phalangeal nonunion or delayed union and patients with concurrent upper or lower extremity fractures.
Interventions and Comparators
All operative and nonoperative management strategies were eligible to be included as interventions, alongside any rehabilitation and hand therapy protocols implemented after initial definitive management. All treatments could also be comparators.
Outcomes
The primary outcome assessed was time to return to sport. For patients undergoing operative intervention, return-to-sport time was defined as the length of time from primary surgical intervention to recommencement of preinjury levels of sporting activity. For those undergoing nonoperative intervention, return-to-sport time was defined as the length of time from starting therapy to recommencement of preinjury levels of sporting activity.
Secondary outcomes assessed included rate of return to sport, rate of fracture union, time to union, overall hand function, and any complications. The rate of return to sport was defined as the proportion of athletes who returned to preinjury levels of competition after intervention. Rate of union was defined as the proportion of athletes who demonstrated radiological evidence of fracture union after intervention. Time to union was defined as the time taken to achieve radiologically proven fracture union. Hand function was quantified by objective functional measures and subjective patient-reported outcome measures, where recorded. Complications were defined as any adverse effects of interventions occurring within the first month after treatment.
Search Strategy
Search strategies were developed using index and free-text terms, in conjunction with a search strategist. The literature search was limited to human studies; full search strategies are available as supplemental material to this article. The searches were applied to MEDLINE and In Process (1946–December 2019), Embase (1974–December 2019), EMCARE (1995–December 2019), and CINAHL (1981–December 2019). The reference lists of articles were also hand-searched for relevant publications.
Study Selection
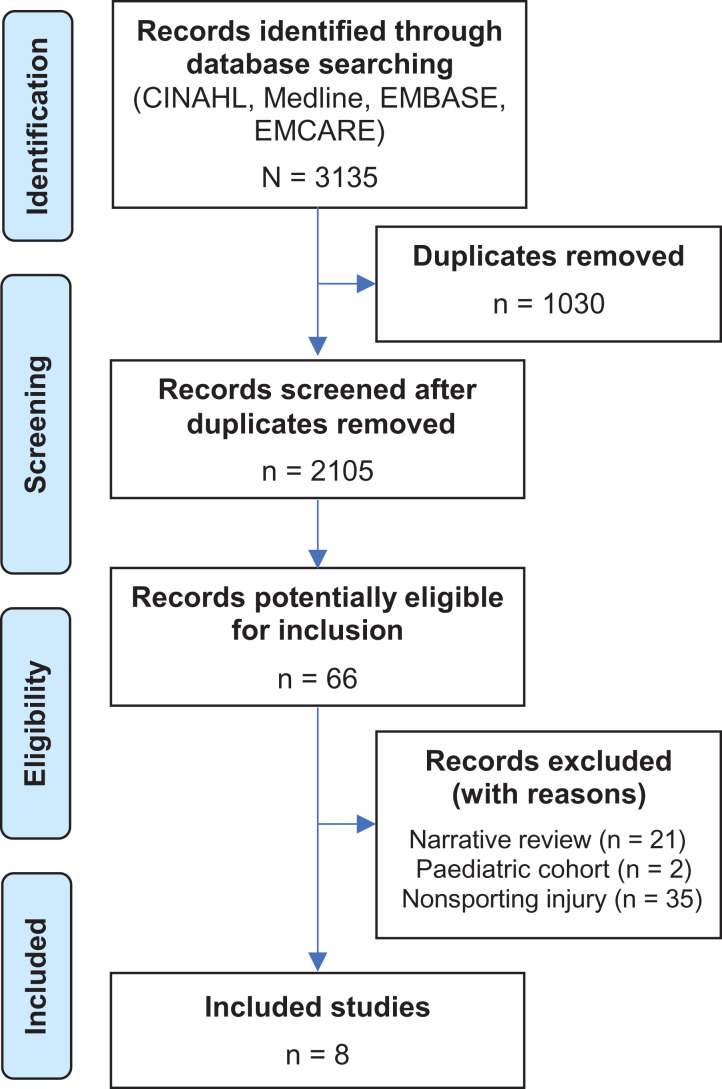
After pooling and removal of duplicate publications, 2 authors (L.G., A.S.) independently screened all abstracts against prespecified stepwise inclusion criteria. The study selection process is detailed in Figure 1.
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart of studies included in the review.
Data Extraction and Statistical Analysis
Relevant extracted data were demographics, type of fracture, fracture pattern, sport during which injury was sustained, rehabilitation protocol, return-to-sport time and rate, follow-up duration, rate of fracture union, time to union, hand function measure, patient-reported outcome measure, complications, and study quality. The US National Institutes of Health quality assessment tool for observational cohort and cross-sectional studies20 was employed to assess the quality of cohort studies. The GRADE (Grading of Recommendations Assessment, Development and Evaluation) tool was used to rate study quality by considering the risk of bias, publication bias, imprecision, inconsistency, indirectness, and magnitude of effect (where possible).14 GRADE ratings were assigned to reflect confidence in effect estimates. For studies in which patients underwent operative intervention, data were also extracted for fixation modality and time to surgery. Where possible, return-to-play times were pooled for injury type and treatment type, without head-to-head comparisons. As it was not anticipated that individual patient data would be available, the inverse variance method with random effects was used. All analyses were performed in R (Version 3.5.1; R Foundation) using the meta package (Version 4.11-0).
Results
Search Results
Collectively, 3135 records were identified through database searching, including 1185 from Embase, 575 from MEDLINE, 695 from EMCARE, and 696 from CINAHL. After duplicates were removed, 2105 records were screened, of which 8 met full inclusion criteria2,10,11,17,19,21,26,27 (Figure 1). Of the 58 excluded fully reviewed articles, 4 expert opinion articles related to the management of metacarpal/phalangeal fractures sustained in athletes were identified.4,5,13,24
Study Characteristics
All 8 studies were retrospective cohort studies based on an established definition7; there were no randomized controlled trials. Morse et al19 reported comparative data related to the operative and nonoperative management of metacarpal and phalangeal fractures sustained by professional basketball players. Table 1 shows the characteristics of the studies.
Table 1.
Characteristics of the Included Studiesa
| Lead Author (Year) | No. | Fracture Site | Sport | Competition Level | Return-to-Sport Rate, % | Follow-up, mo | Study Qualityb |
|---|---|---|---|---|---|---|---|
| Kodama17 (2014) | 20 | 8 metacarpal, 12 phalangeal | 6 rugby, 3 handball, 3 NFL, 3 baseball, 2 football, 1 volleyball, 1 equestrian, 1 combat | Unspecified | 100 | 27 | Fair |
| Etier10 (2015) | 20 | All metacarpal | 20 NFL players | 9 collegiate, 10 high school, 1 recreational | 100 | 3 | Fair |
| Yalizis27 (2017) | 16 | All metacarpal | 16 Australian rules football players | 16 professional | 100 | 56 | Fair |
| Morse19 (2017) | 59 | 26 metacarpal, 33 phalangeal | 59 basketball players | 59 professional | 100 | Unspecified | Fair |
| Toronto26 (1996) | 23 | All metacarpal | 12 NFL, 3 skiing, 3 combat, 4 baseball, 1 basketball, 1 running, 1 swimming | Unspecified | 100 | 17 | Poor |
| Bartels2 (2019) | 61 | 56 metacarpal, 5 phalangeal | 61 NFL players | 61 collegiate | Unspecified | Unspecified | Fair |
| Evans11 (1997) | 2 | All metacarpal | 2 rugby players | 2 professional | 100 | Unspecified | Poor |
| Rettig21 (1989) | 33 c | All metacarpal | 18 NFL, 8 basketball, 2 baseball, 2 sledding, 1 wrestling, 1 gymnastics, 1 combat | Unspecified | 100 | Unspecified | Fair |
aAll studies were retrospective cohort studies. NFL, National Football League.
bAccording to the National Institutes of Health quality assessment tool for observational cohort and cross-sectional studies.20
cThe original study included 56 patients: 21 were excluded in our analysis as they were aged <16 years, and a further 2 were excluded as return-to-sport time data were not reported.
Quality of Studies
All studies were of fair or poor quality according to the National Institutes of Health tool (see Table 1). A breakdown of the assessment results is shown in Appendix Table A1. None of the studies described attempts to measure and adjust for the effect of confounding variables. Studies provided varying descriptions of operative, nonoperative, and rehabilitation management strategies. Duration of follow-up was clearly documented in 4 studies and ranged from 3 to 56 months.
Demographics and Injury Details
The 8 studies reported data from 234 patients who sustained 184 metacarpal and 50 phalangeal fractures. Collectively, 97% of patients were male with a mean age of 21 years. Injuries were sustained across 15 sports: 49% of injuries from American football and 29% from basketball (collegiate and professional players) (Table 1). Kodama et al17 examined the anatomic site of phalangeal fractures and reported that the proximal phalanx was most commonly injured (8/12; 75%). Five studies indicated the anatomic site of metacarpal fractures10,17,19,21,26,27; the fourth metacarpal was most commonly injured (42/116; 36%).
Interventions and Rehabilitation
Studies included operative and nonoperative management strategies (Table 2). Patients who sustained phalangeal fractures and underwent operative intervention were treated with plate fixation (8/50; 16%), mini-screw fixation (4/50; 8%), or unspecified surgical fixation (13/50; 26%). Time from injury to surgery was not cited by any study. For patients with phalangeal fractures, 1 study19 indicated nonoperative management (20/50; 40%), and 1 study2 did not note any management strategy (5/50; 10%). Nonoperative management protocols were not published.
Table 2.
Interventions, Rehabilitation Protocols, and Reported Outcomes for the Included Studiesa
| Lead Author (Year) | Intervention | Time to Surgery, db | Rehabilitation Protocol | Return to Sport Time, Mean (Range), d | Complications | Reported Outcomes |
|---|---|---|---|---|---|---|
| Etier10 (2015) | Metacarpal: locking compression plate (n = 12), condylar plate (n = 1), metacarpal nail (n = 6), mini-screw (n = 1) | <2 (n = 8), 2-4 (n = 3), 14 (n = 1) | Protective equipment used for 21 d: padded glove (skilled position), padded cast (unskilled position) | All players: 16.9 (1-42). In-season: 5.5 (1-21) | None reported | All returned to preinjury level of competition |
| Kodama17 (2014) | Metacarpal: mini--low profile plate (n = 6), mini-screw (n = 2). Phalangeal: mini--low profile (n = 8), mini-screw (n = 4) | Unspecified | Week 1: active finger motion exercises with external immobilization. Week 2: light training with orthotic support (metacarpal fractures) and splinted to adjacent finger (phalangeal fractures). Week 3: full training without support or splint | All players: 28 (7-28). Metacarpal: 23 (7-28). Phalangeal: 25 (14-28) | Wound dehiscence (n = 2) | All patients achieved radiographic union at 3 mo. Mean TAM: 263° for metacarpal and phalangeal fractures (range, 240°-270°). 70% very satisfied, 30% satisfied with treatment |
| Yalizis27 (2017) | Metacarpal: locking compression plate (n = 16) | Mean, 1.65 d | Forearm-based immobilization splint for 3 d. Training resumed after splint removed | In-season: 13 (7-28). Off-season: 21 (14-35) | Mild to moderate discomfort along affected metacarpal (n = 2) | Two patients had significantly lower performance scores postoperatively. Mean QuickDASH score, 2.1 (range, 0-20.45). All patients achieved radiographic union within 6 wk |
| Morse19 (2017) | Metacarpal: undefined surgical fixation (n = 13), nonoperative (n = 13). Phalangeal: undefined surgical fixation (n = 13), nonoperative (n = 20) | Unspecified | Unspecified | Metacarpal: 42 (total), 57 (surgical), 26
(nonoperative) Phalangeal: 38 (total), 46 (surgical), 33 (nonoperative) |
None reported | Significantly longer return-to-sport time in surgically treated vs nonoperative metacarpal fractures (mean ± SD, 56.7 ± 26.3 vs 26.3 ± 12.1 d; P < .01) |
| Toronto26 (1996) | Metacarpal: modified functional casting technique (n = 23) | NA | Immobilization in functional cast with return to modified athletic activity as pain allowed | 28 (21-28) | None reported | 95% very satisfied, 5% satisfied with treatment |
| Bartels2 (2019) | Metacarpal: nonoperative (n = 42), undefined surgical fixation (n = 14). Phalangeal: unknown (n = 5) | Unspecified | Unspecified | Metacarpal: 12 (0-148) | None reported | Mean ± SD time loss for players who sustained metacarpal fractures: 12.3 ± 25.8 d |
| Evans11 (1997) | Metacarpal: locking compression plate (n = 2) | Unspecified | Unspecified | 28 d | None reported | All players returned to preinjury competition levels |
| Rettig21 (1989) | Metacarpal: nonoperative (n = 28), locking compression plate (n = 3), K-wire (n = 2) | Unspecified | Unspecified | 14 (0-56) | None reported | Evaluation of clinician-derived measures of function (range of motion, grip strength) and subjective patient assessment revealed no residual limitation |
aNA, not applicable; ORIF, open reduction and internal fixation; QuickDASH, Quick Disabilities of the Arm, Shoulder and Hand; TAM, total active motion.
bFor in-season injuries.
Patients who sustained metacarpal fractures and underwent operative intervention (78/184) were treated with plate fixation (40/78; 51%), mini-screw fixation (3/78; 4%), metacarpal nail fixation (6/78; 8%), external fixation with K-wires (2/78; 3%), and unspecified surgical fixation (27/78, 35%). One study cited the time from injury to surgery (mean, 1.65 days; range, 5 hours–3 days).27 Four studies indicated nonoperative management for patients with metacarpal fractures (106/184).2,19,21,26
One study reported nonoperative management strategies for closed metacarpal injuries. Toronto et al26 cited the use of a modified functional casting technique, which permitted active flexion and extension of the wrist with (1) concurrent immobilization using buddy taping to adjacent fingers for oblique metacarpal shaft fractures, (2) metacarpophalangeal immobilization for metacarpal neck fractures, and (3) immobilization at 30° of flexion for fractures of the first metacarpophalangeal joint. Athletes were permitted to engage in modified athletic activity, noncontact drills, and sport-specific conditioning as soon as symptoms permitted, with the use of a functional cast. All patients returned to full sport-specific activity by 4 weeks postinjury.
Rehabilitation protocols varied in the duration of immobilization and the use of protective equipment. Three studies reported the use of protective equipment on recommencement of sporting activity in the form of buddy taping and padded gloves/casts.10,17,27 Rehabilitation protocols favored early active motion, with digital flexion/extension exercises commenced immediately17 and 3 days27 postoperatively.
Outcome Measures
Collectively, 8 outcome measures were used across all studies, including return-to-sport rate (defined by all studies as return to preinjury level of competition), return-to-sport time, patient satisfaction scores, total active motion, time taken for osseous union, objective sporting performance metrics, Quick Disabilities of the Arm, Shoulder and Hand score, and complications. All studies used various combinations of outcome measurements at varying time points after injury (median follow-up, 22 months; range, 3-56 months).
Return-to-Play Time and Consequences
The return-to-sport rate for all studies was 100%. The pooled mean return-to-sport time for all phalangeal fractures was 30.6 days (95% CI, 17.5-43.9 days). The pooled mean return-to-sport time for all metacarpal fractures was 21.9 days (95% CI, 15-28.7 days). The pooled mean return-to-sport time for metacarpal and phalangeal fractures stratified by treatment type is outlined in Table 3. One study was excluded from the pooled meta-analysis, as it did not report the standard deviation for mean return-to-play time for treated metacarpal fractures.10 One study was excluded from the stratified meta-analysis, as it did not include mean estimates for return to play for operatively or nonoperatively treated metacarpal fractures.2
Table 3.
Modified GRADE Evidence Profile by Treatment Typea
| Treatment Type | No. of Studies | No. of Patients | Return-to-Play Time, Mean (95% CI), d | GRADE Ratingb |
|---|---|---|---|---|
| Metacarpal fractures | ||||
| Surgically treated | 5 | 44 | 28.5 (16.0-40.9) | Very low |
| Nonoperatively treated | 3 | 65 | 22.0 (11.5-32.3) | Very low |
| Phalangeal fractures | ||||
| Surgically treated | 2 | 45 | 35.1 (14.0-56.0) | Very low |
| Nonoperatively treated | 1 | 20 | NA | NA |
aGRADE, Grading of Recommendations Assessment, Development and Evaluation; NA, not applicable.
bGRADE Working Group grades of evidence: (1) high quality—further research is very unlikely to change the group’s confidence in the estimate of effect; (2) moderate quality—further research is likely to have an important impact on the group’s confidence in the estimate of effect and may change the estimate; (3) low quality—further research is very likely to have an important impact on the group’s confidence in the estimate of effect and is likely to change the estimate; (4) very low quality—the group is very uncertain about the estimate.
One comparative study demonstrated significantly longer return-to-sport time in surgically treated metacarpal fractures (mean ± SD, 56.7 ± 26.3 days; n = 13) as compared with nonoperatively managed metacarpal fractures (26.3 ± 12.1 days; n = 13; P < .01).19 Five studies reported radiographic union in all patients after intervention,10,17,22,26,27 and the remaining 3 studies did not include data related to fracture union.2,11,19
Complications after operative intervention included persistent discomfort at the surgical site after open reduction and internal fixation of metacarpal fractures (2/78) and wound dehiscence after surgically treated phalangeal fractures (2/30). One study cited no clinical or radiographic evidence of shortening, displacement, angulation, rotational deformity, or instability after nonoperatively managed metacarpal fractures,26 although limited inference can be drawn given the small cohort (N = 24) and poor study quality. Morse et al19 reported nonoperative management of phalangeal fractures, although data related to complications were not included.
Discussion
Decisions in treating athletes with metacarpal and phalangeal fractures are multifactorial. They require collaboration among athlete, surgeon, coaching staff, and training staff, and they often carry major financial implications. Fracture pattern, sport/position requirements, individual player considerations, surgical considerations, and various third-party considerations all have an impact on choice of management.
We are not aware of other studies that have systematically reviewed treatment and outcomes of common hand fractures in athletes. Despite the significance of professional sports today and the impact of such fractures on it, there are limited data available to inform management: only 8 studies of limited quality met the inclusion criteria for review. In these studies, nonoperative management strategies were more commonly reported in patients with metacarpal fractures, and operative management strategies were more commonly cited in patients with phalangeal fractures. Overall, all patients returned to preinjury levels of competition. It is possible that this result reflects the pressure to return to high performance for professional athletes. Indeed, return times appeared to be shorter for injuries sustained in season. However, there may also be publication bias, with a tendency to avoid publishing less desirable outcomes for a high-demand group such as adults participating in sports. It is also challenging to establish whether elite athletes can return to their premorbid level of performance, rather than to the same level of competition. These may well be different in many circumstances, and quantifying level of function and performance may be limited to the ceiling effects of many tools, such as patient-reported outcome measures, as high-level athletes may be functioning above the range of performance in the questionnaire. One study utilized “in game” statistics to provide a surrogate marker for functional performance after return from injury.27
Some findings from this review may be tempting to focus on, such as the apparently delayed return-to-sport time for operatively managed metacarpal fractures as compared with nonoperatively managed ones. While there were some data that suggested this, there are important issues to consider when drawing conclusions. All of the studies analyzed were methodologically limited, and none were randomized. As a result, important confounders may have affected the findings. The injury pattern may be a confounder, with worse injuries delaying return to sport and also requiring operative treatment. There is a risk of bias, with patients undergoing surgery likely to have more severe injuries as compared with their nonoperatively managed counterparts and with financial pressures perhaps influencing earlier return to professional sport for athletes treated nonoperatively. Thus, it would be inappropriate to advise that operative management delays return to sport. Instead, it would be more appropriate to advise sportspeople that fractures deemed to require operative management may lead to a delayed return to sport, but it is unclear whether this is due to the injury itself, the direct effects of intervention, the collateral effects of intervention (eg, a surgical wound that needs to heal), or a combination of all factors. Direct complications arising from fixation type must also be considered in the context of functional demands, with K-wires potentially having a greater propensity for displacement and bending as compared with internal fixation constructs. It is important to consider these factors when determining the clinical significance of a 6-day difference in return to sport between operatively and nonoperatively managed metacarpal fractures. Contextual, individual, and sport-specific factors must also be given consideration. A 6-day difference may have less clinical significance for an off-season injury sustained by a seasoned athlete in a noncontact sport, whereas the same difference may be career ending for an in-season injury sustained by a rookie athlete during a competitive series of games.
Nonoperative management may require longer periods of protective immobilization, which may be prohibitive to elite sportspeople, with operative intervention providing immediate fracture stability and enabling early active rehabilitation to minimize soft tissue atrophy and joint stiffness.27 Different treatment strategies may be desirable for those playing at different levels of performance.
Similarly, treatment strategy is dependent on the sport and position played. Drakos et al9 reported that 15.4% of all injuries sustained by basketball players are upper extremity injuries. Given the dependence on hand dexterity, upper limb injuries for basketball players can be devastating. Furthermore, nonoperative management using splints and buddy taping may compromise hand dexterity to the same or greater degree, resulting in equally poor athletic performance. This is in contrast to football, where compromised hand dexterity may not affect performance to the same degree. However, specific requirements vary within sports, with goalkeepers having much greater dependency on hand dexterity for optimal athletic performance. It is the surgeon’s role to act as an independent advocate for the athlete and provide impartial clinical advice. It is vital that the surgeon act impartially without coercion from the athlete, the club, or sponsors to maintain the athlete’s best interests.
The quality of studies reviewed was generally fair, although all had significant risk of confounding. The methodological quality of studies was demonstrably lower compared with similar systematic reviews,23 which may represent the potential sensitivity of publishing data describing elite sportspeople or a lack of academic investment in the management of such injuries, as supported by the limited number of identified studies and disproportionate representation of level 5 evidence identified.
Our results must be considered in view of the study limitations. Despite using a sensitive search strategy, it is possible that relevant studies were overlooked. Studies provided limited descriptions of return-to-sport rates and times. The use of return times and rates without comprehensively defined functional and competition-specific parameters predisposes to reporting and confirmation bias.8,23 Heterogeneity of cohorts with respect to sporting activity, competition level, rehabilitation protocols, and differential outcome measure reporting limited the applicability of study conclusions in the clinical setting. Furthermore, 97% of athletes were male; a large proportion of patients underwent unspecified surgical fixation; and postoperative rehabilitation strategies were not indicated, thereby limiting the generalizability of our findings.
Conclusion
Perhaps the most compelling conclusion from the current work is that all competitive athletes who sustained a metacarpal or phalangeal fracture returned to preinjury levels of competition after operative and nonoperative management. The current evidence base does not demonstrate a clear optimal management strategy for expediting safe return to play in athletes with metacarpal and phalangeal fractures. Evidence from individual studies tentatively supports early active mobilization for patients who undergo surgical intervention, with a graded return to sporting activity. Patients with injuries requiring surgical intervention may have a delayed return to sport. Improved reporting of the treatment, outcome, level of performance, and return to play through routine data collection or higher-quality studies may improve care for sportspeople and reduce adverse impacts on sports organizations and systems.
Supplemental Material
Supplemental Material, sj-pdf-1-ojs-10.1177_2325967120980013 for Return to Sport After Metacarpal and Phalangeal Fractures: A Systematic Review and Evidence Appraisal by Luke Geoghegan, Alexander Scarborough, Jeremy N. Rodrigues, Mike J. Hayton and Maxim D. Horwitz in Orthopaedic Journal of Sports Medicine
Acknowledgment
The authors thank Phillip Barlow for his expert help devising a comprehensive search strategy.
Appendix
Table A1.
Quality of Cohort Studies as Assessed With the NIH Quality Assessment Tool for Observational Cohort and Cross-sectional Studiesa
| Assessment Questionb | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study (Year) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | Overallc |
| Kodama17 (2014) | Y | Y | N | Y | N | Y | Y | CD | Y | NA | N | NR | Y | N | Fair |
| Etier10 (2015) | Y | Y | Y | Y | N | Y | Y | CD | Y | NA | Y | NR | Y | N | Fair |
| Yalizis27 (2017) | Y | Y | Y | Y | N | Y | Y | CD | Y | NA | N | NR | Y | N | Fair |
| Morse19 (2017) | Y | Y | Y | Y | N | Y | Y | CD | Y | NA | Y | NR | Y | N | Fair |
| Toronto26 (1996) | N | Y | NR | N | N | Y | Y | CD | Y | NA | N | NR | Y | N | Poor |
| Bartels2 (2019) | Y | Y | NR | Y | N | Y | Y | CD | Y | NA | N | NR | Y | N | Fair |
| Evans11 (1997) | N | N | NR | Y | N | N | Y | CD | Y | NA | N | NR | Y | N | Poor |
| Rettig21 (1989) | Y | N | Y | Y | N | Y | Y | CD | Y | NA | N | NR | Y | N | Fair |
aCD, cannot determine; N, no; NA, not applicable; NIH, National Institutes of Health; NR, not reported; Y, yes.
b1: Was the research question or objective in this paper clearly stated?
2: Was the study population clearly specified and defined?
3: Was the participation rate of eligible persons at least 50%?
4: Were all the participants selected or recruited from the same or similar populations (including the same time period)? Were inclusion and exclusion criteria for being in the study prespecified and applied uniformly to all participants?
5: Was a sample size justification, power description, or variance and effect estimates provided?
6: For the analyses in this paper, were the exposure(s) of interest measured prior to the outcome(s) being measured?
7: Was the time frame sufficient so that one could reasonably expect to see an association between exposure and outcome if it existed?
8: For exposures that can vary in amount or level, did the study examine different levels of the exposure as related to the outcome (eg, categories of exposure, or exposure measured as continuous variable)?
9: Were the exposure measures (independent variables) clearly defined, valid, reliable, and implemented consistently across all study participants?
10: Was the exposure(s) assessed more than once over time?
11: Were the outcome measures (dependent variables) clearly defined, valid, reliable, and implemented consistently across all study participants?
12: Were the outcome assessors blinded to the exposure status of participants?
13: Was loss to follow-up after baseline 20% or less?
14: Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure(s) and outcome(s)?
cOverall assessment of study quality was determined by appraisal of the internal validity based on the criteria listed above. Studies with a high risk of bias were deemed poor quality; studies with a moderate risk of bias, fair quality; and studies with a low risk of bias, good quality.
Footnotes
Final revision submitted July 20, 2020; accepted August 11, 2020.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Supplemental material for this article is available at http://journals.sagepub.com/doi/suppl/10.1177/2325967120980013.
References
- 1. Aitken S, Court-Brown CM. The epidemiology of sports-related fractures of the hand. Injury. 2008;39(12):1377–1383. [DOI] [PubMed] [Google Scholar]
- 2. Bartels D, Hevesi M, Wyles C, et al. Epidemiology of hand and wrist injuries in National Collegiate Athletic Association football players from 2009 to 2014: incidence and injury patterns. Orthop J Sports Med. 2019;7(4):2325967119835375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Booth A, Clarke M, Dooley G, et al. The nuts and bolts of PROSPERO: an international prospective register of systematic reviews. Syst Rev. 2012;1:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chen F, Kalainov DM. Phalanx fractures and dislocations in athletes. Curr Rev Musculoskelet Med. 2017;10:10–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cotterell IH, Richard MJ. Metacarpal and phalangeal fractures in athletes. Clin Sports Med. 2015;34(1):69–98. [DOI] [PubMed] [Google Scholar]
- 6. Court-Brown CM, Wood AM, Aitken S. The epidemiology of acute sports-related fractures in adults. Injury. 2008;39(12):1365–1372. [DOI] [PubMed] [Google Scholar]
- 7. Dekkers OM, Egger M, Altman DG, Vandenbroucke JP. Distinguishing case series from cohort studies. Ann Intern Med. 2012;156(1)(pt 1):37–40. [DOI] [PubMed] [Google Scholar]
- 8. Del Buono A, Smith R, Coco M, et al. Return to sports after ankle fractures: a systematic review. Br Med Bull. 2013;106:179–191. [DOI] [PubMed] [Google Scholar]
- 9. Drakos MC, Domb B, Starkey C, Callahan L, Allen AA. Injury in the National Basketball Association: a 17-year overview. Sports Health. 2010;2(4):284–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Etier BE, Scillia AJ, Tessier DD, et al. Return to play following metacarpal fractures in football players. Hand (N Y). 2015;10(4):762–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Evans NA, Evans RO. Playing with metal: fracture implants and contact sport. Br J Sports Med. 1997;31(4):319–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fufa DT, Goldfarb CA. Fractures of the thumb and finger metacarpals in athletes. Hand Clin. 2012;28(3):379–388. [DOI] [PubMed] [Google Scholar]
- 13. Gaston RG. Football commentary: phalangeal fractures—displaced/nondisplaced. Hand Clin. 2012;28(3):407–408. [DOI] [PubMed] [Google Scholar]
- 14. Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–394. [DOI] [PubMed] [Google Scholar]
- 15. Halim A, Weiss AP. Return to play after hand and wrist fractures. Clin Sports Med. 2016;35(4):597–608. [DOI] [PubMed] [Google Scholar]
- 16. Haughton D, Jordan D, Malahias M, Hindocha S, Khan W. Principles of hand fracture management. Open Orthop J. 2012;6:43–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kodama N, Takemura Y, Ueba H, Imai S, Matsusue Y. Operative treatment of metacarpal and phalangeal fractures in athletes: early return to play. J Orthop Sci. 2014;19(5):729–736. [DOI] [PubMed] [Google Scholar]
- 18. Moher D, Liberati A, Tetzlaff J, Altman DG; the PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Morse KW, Hearns KA, Carlson MG. Return to play after forearm and hand injuries in the National Basketball Association. Orthop J Sports Med. 2017;5(2):2325967117690002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. National Institutes of Health. Quality assessment tool for observational cohort and cross-sectional studies. Accessed November 20, 2020. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools.2020
- 21. Rettig AC, Ryan R, Shelbourne KD, et al. Metacarpal fractures in the athlete. Am J Sports Med. 1989;17(4):567–572. [DOI] [PubMed] [Google Scholar]
- 22. Rettig ME, Dassa GL, Raskin KB, Melone CP. Wrist fractures in the athlete: distal radius and carpal fractures. Clin Sports Med. 1998;17(3):469–489. [DOI] [PubMed] [Google Scholar]
- 23. Robertson GA, Wood AM. Return to sport following clavicle fractures: a systematic review. Br Med Bull. 2016;119(1):111–128. [DOI] [PubMed] [Google Scholar]
- 24. Singletary S, Freeland AE, Jarrett CA. Metacarpal fractures in athletes: treatment, rehabilitation, and safe early return to play. J Hand Ther. 2003;16(2):171–179. [DOI] [PubMed] [Google Scholar]
- 25. Swenson DM, Yard EE, Collins CL, Fields SK, Comstock RD. Epidemiology of US high school sports-related fractures, 2005-2009. Clin J Sport Med. 2010;20(4):293–299. [DOI] [PubMed] [Google Scholar]
- 26. Toronto R, Donovan P, Macintyre J. An alternative method of treatment for metacarpal fractures in athletes. Clin J Sport Med. 1996;6:4–8. [DOI] [PubMed] [Google Scholar]
- 27. Yalizis MA, Ek ETH, Anderson H, Couzens G, Hoy GA. Early unprotected return to contact sport after metacarpal fixation in professional athletes. Bone Joint J. 2017;99(10):1343–1347. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-pdf-1-ojs-10.1177_2325967120980013 for Return to Sport After Metacarpal and Phalangeal Fractures: A Systematic Review and Evidence Appraisal by Luke Geoghegan, Alexander Scarborough, Jeremy N. Rodrigues, Mike J. Hayton and Maxim D. Horwitz in Orthopaedic Journal of Sports Medicine