Abstract
Rabies is a vaccine-preventable viral disease present in more than 150 countries around the world. Globally, almost 60,000 people die each year from rabies, of which more than 58% are in Asia and around 45% in South Asia with especially high incidence in India, Pakistan and Bangladesh. Vaccination coverage of both people and stray dogs is low in the region and in general people are not given enough protection and information about pre- and post-exposure prophylaxis. Engagement of multiple sectors and One Health collaboration including community education, awareness programmes and vaccination campaigns are critical to control and elimination of rabies.
Keywords: Transboundary diseases, Stray dogs, Post exposure prophylaxis, Vaccination
1. Introduction
South Asia comprises the countries of Afghanistan, Bangladesh, Bhutan, India, Maldives, Nepal, Pakistan and Sri Lanka. The region has a total area of 5,134,641 square km. The Human population of more than 1.8 billion occupies the land at a density of 362.3 people per square km. About one quarter of all people fall below the international poverty line. Although there are some enormous cities, 70% of people live in rural areas.
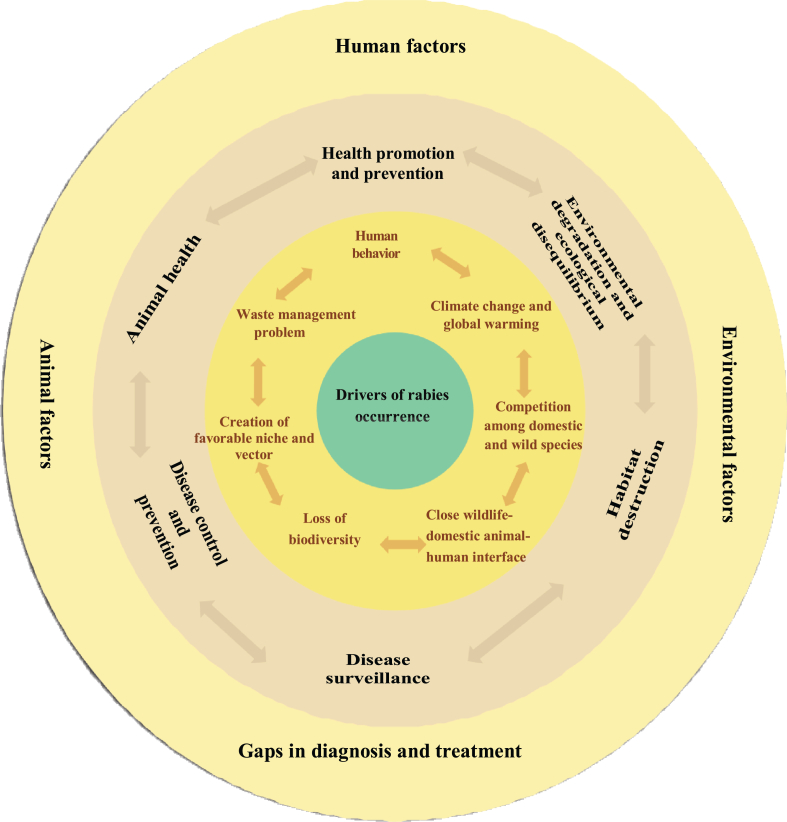
Human rabies is a fatal viral disease transmitted from bites by infected animals, predominantly domestic or street dogs. It can be controlled through mass vaccination of infected or potentially infected animals. The disease is entirely preventable through prompt administration to bite victims of post-exposure prophylaxis (PEP). Although rabies is vaccine preventable, several human, climatic and natural factors favour its spread in South Asia (Fig. 1).
Fig. 1.
Factors increasing risk of prevalence of rabies and its transmission (Information adapted and modified from Destoumieux-Garzón et al. 2018 [1] and Marban -Castro et al. 2020 [2]).
Rabies is notoriously under-reported because most deaths in low income countries (LMICs) occur at home so that the disease is often neglected. A study in Bangladesh find out that only one third of the patients were taken to hospital while rest of them died at home [3]. Vaccination of dogs is not widely practised and access to PEP is limited in low income countries. More focus on dog vaccination could eliminate the disease at source which would reduce the need for PEP and prevent the huge and largely unnecessary mortality in communities at risk [4,5].
Neglected infectious zoonotic diseases have a disproportionate effect on the health of marginalized poor people. More than 35,000 (58%) of the almost 60,000 people worldwide who die each year from rabies occur in Asia. Although no quantitative data are available, India, Pakistan and Bangladesh are known to have a high incidence [6]. It is estimated that South Asia carries 45% of the global burden of dog mediated human rabies [7]. All the countries of South Asia are rabies endemic except the Maldives which is free from rabies due to its isolated location in the Indian Ocean [8]. A joint call for action to eliminate rabies by 2030 was made in 2015 by the World Health Organization (WHO), the World Organization for Animal Health (OIE), the Food and Agriculture Organization (FAO), and the Global Alliance for Rabies Control (GARC) [9].
Most South Asian countries have large and predominantly unvaccinated dog populations both domestic and free-roaming. Poor sanitary conditions in rural and urban areas favour an increase in roaming dog populations. The risk of contracting rabies is high. The effects can disrupt human interaction in social security, development, trade, and tourism. The possibly exceptional economic and social consequences must be confronted in an effective and efficient manner, so as to grasp the profound impact of transmissible pathogens on human health and welfare [10].
South Asian countries already have some political and public support for elimination of rabies but levels vary across the region. Animal rabies control and management, access to vaccination for human rabies and better public awareness are keys to success. The “prevention at the source” approach through control by vaccination in the canid reservoir can provide cost-effective control [10]. It has been suggested that 70% or more of dogs should be vaccinated to prevent epidemics and to eliminate endemic rabies [11]. Although it would be difficult to achieve such a coverage under South Asian conditions, it is important to set realistic region-specific vaccination goals.
Animal welfare organizations and other charities conduct mass awareness campaigns and neutering and vaccination programmes in attempts to control rabies but most have a presence only in urban locations leaving rural areas at higher risk. In general, South Asian countries do not achieve coverage that is sufficient to reduce the incidence of rabies except in Bhutan and Bangladesh [12].
1.1. Strategies applied and constraints to rabies control in South Asian countries
Bhutan and Sri Lanka are nearest to achieving the goal of zero human deaths from by 2030 by the mass dog vaccination, better accessibility of PEP and efficient vaccine supply systems [13].
1.1.1. Afghanistan
Rabies is endemic and a major significant public health issue in Afghanistan. From 2017 to 2019, 29 human deaths, 1789 recorded dog bites and 36,959 animal rabies cases were reported [13,14]. The country has the highest estimated number of human rabies incidence in South Asia at 5.7 per 100,000 population [15]. A rabies control strategy developed by the Ministry of Agriculture, Irrigation and Livestock has yet to be implemented. The Ministry of Health has drafted the rabies guideline and Standard Operating Procedures [13]. Immunoglobins and antirabies vaccines are distributed to all provinces for PEP to humans. Until 2016 dogs were poisoned by strychnine in Kabul but the country has now started to adopt mass dog vaccination and neutering programmes [15]. Huge numbers of stray dogs, negative cultural attitudes towards dogs, lack of regular vaccination, limited human resources, inadequate technical capacity and Animal Birth Control (ABC) programmes and insufficient funds are the major constraints to rabies control.
1.1.2. Bangladesh
Bangladesh, with a dog population of about 1.7 million, ranked third in the world in terms of human impacts of rabies in 2010. The disease accounted for 2000–2500 human deaths [16] and 25,000 animal cases were reported every year [13]. Mass culling was the major control strategy for rabies in major cities until late 2011 [17]. The Obhoyaronno-Bangladesh Animal Welfare Foundation (OBAWF) then protested and requested a more humane way to control rabies be adopted. Killing of dogs was stopped in Dhaka in January 2012 [16]. Rabies is now a national priority and the problem is being approached through a multisectoral One Health (OH) approach with support from its development partners with the aim of eliminating rabies by 2020 [18]. A pilot project of Mass Dog Vaccination (MDV) was conducted in Cox's bazaar in 2011 and was later extended to all six entire districts and 65 district municipalities [19]. A strong political commitment and increased budget allocations (US$ 0 in 2010, US$ 7 million in 2011–2016 and US$ 33 million in 2017–2022) of successive five-year health sector plans were the key factors in the decrease in the annual incidence of rabies from over 2000 before 2010 to 1500 in 2012 and 200 in 2015 [13,19]. By 2019, Bangladesh had trained 1000 dog catchers/vaccinators and vaccinated more than 1.3 million dogs and planned to vaccinate around 1.6 million dogs by 2020 [19]. Three rounds of MDV in all districts, strengthening of laboratories and human resources, reporting and surveillance in both animals and humans and increased coverage of PEP are the key activities that are currently practiced to control rabies in Bangladesh. Large numbers of stray dogs, poor accessibility to quality vaccines and lack of appropriate diagnostic facilities at field level are the major constraints to the elimination of rabies in Bangladesh [13].
1.1.3. Bhutan
Rabies is endemic in Bhutan but the majority of reported outbreaks are near to the southern border with Assam and West Bengal of India [20]. From 2006 to 2016, 17 human deaths (0.23 per 10,000 population) were reported. No human rabies cases have been reported since although there were over 7000 dog bite cases (1026 bites per 100,000 people annually) [14,21]. Between 1996 and 2017, 442 dogs and 551 cattle died from rabies. Since 2018 the number of outbreaks has decreased to around 12 per year [13].
Poisoning and shooting (1970s and 1980s), translocation (1990s), impounding (early 2000s) and ad hoc sterilization (1970s-early 2000s) were practised to control dog populations and rabies but these failed due to poor animal welfare, high zoonotic prevalence and narrow coverage [14]. In 2009, the National Dog Population Management (NDPM) and Rabies Control Programme (RCP) with assistance from the Humane Society International, initiated the Catch-Neuter-Vaccinate-Release(CNVR) protocol [14]. Livestock Rules and Regulations 2017, Livestock Act of Bhutan 2001, National Rabies Prevention and Control Plan 2017, Human Rabies Management Guidelines 2014, Dog Population and Management Guidelines 2019, and the One Health Strategic Plan 2018–2023 are current policies and strategies for the containment of rabies [13,21]. Prevention and control strategies, such as mass dog vaccination, animal birth control, animal movement regulation via pre-travel checks and health certification, and regular rabies surveillance in both humans and animals are carried out [22]. The long open border, limited resources and competing priorities are key challenges to rabies control in Bhutan. Coordination and collaboration of Bhutan with Assam and West Bengal of India for active surveillance, mass dog vaccination and neutering programmes in the border area could decrease the rabies burden in the southern part of the country.
1.1.4. India
About 35% of all human deaths from rabies occur in India which also accounts 60% of rabies deaths in Asia [8,23]. Some 95% of rabies cases are dog mediated. It is estimated that there are about 60 million stray/free-ranging dogs in the country and more than one million people receive PEP each year [8,13,23]. Despite these figures, there is no coordinated and structured surveillance system for rabies which is not included in the list of regular surveillance diseases under the Integrated Disease Surveillance Project of the Indian Ministry of Health and Family Welfare [24]. This results in the underestimation of actual cases and deaths due to rabies. In the Eleventh 5-year plan (2007–2012), rabies control was mentioned for the first time in the form of pilot projects and 8.65 crore rupees (then 2.1 million US dollars) was allocated. Animal Birth Control, rabies control in animals, and vaccination of stray dogs were to be the responsibility of the Animal Welfare Board of India [25]. The National Rabies Control Programme of the Twelfth 5-year plan (2012–2017), administered by the National Centre for Disease Control and the Animal Welfare Board, aimed to halve human deaths by 2017 but there is no evidence that this target was achieved [23]. Control of human rabies is included in the National Rural Health Mission for which around 6.13 million US dollars was allocated in 2018 but then reduced to around 3.51 million US dollars in 2019 and 2020 [23].
The Assistance to States for Control of Animal Diseases (ASCAD) and the Scheme for Birth Control and Immunization of Stray Dogs of the Animal Welfare Board, the Prevention and Control of Infectious and Contagious Diseases in the Animals Act, 2009, and the Laboratory Diagnosis Facilities (One CDDL, 5 RDDL and 256 State laboratories) execute various rabies control and prevention programmes [13]. Tamil Nadu State of India was the first one to establish a multisectoral, coordinated One Health committee to control rabies [25]. In Goa State more than 10,000 dogs are vaccinated by door-to-door (DD) and catch-vaccinate-release (CVR) programs annually with coverage of 70% [26,27]. In Goa vaccination by DD and CVR and an awareness campaign reduced dog rabies from 78 in 2017 to 4 in 2019 and human cases from 17 in 2014 to 0 in 2018–2019 [27]. Goa received a score of 3.5 out of 5.0 by CDC suggesting that rabies in Goa is near to elimination [27]. Not being a notifiable disease, absence of a national rabies control programme, a focus by Ministry of Health only on PEP, absence of nationwide dog vaccination and an unsystematic reporting system are the major blocks to control and elimination of rabies in India.
1.1.5. Nepal
Reports indicate that up to 32 humans and 300–500 animals die every year in Nepal due to rabies although because of underreporting actual cases are probably higher [8,28]. Between 20,000 and 40,000 animal bites were reported between 2013/2014 and 2017/2018 and up to 150 people attend Sukraraj Tropical and Infectious Disease Hospital in Kathmandu to receive PEP [8].
Various national, international and governmental organizations are involved in rabies control and elimination in Nepal. The National Zoonoses and Food Hygiene Research Center (NZFHRC) has contributed to rabies control by vaccinating dogs since the 1980s and vaccinated over 18,000 dogs and cats between 2000 and 2007 [29]. Since its establishment in 2008 the Alliance Group for Rabies Control in Nepal has vaccinated more than 10,000 household and stray dogs [13]. In 2019, the Epidemiology and Disease Control Division (EDCD) of the Ministry of Health and Population was given the mandate for the containment of rabies in the country [30]. “National guidelines for rabies prophylaxis in Nepal 2019” directs health workers to achieve ‘zero human death by 2030’ [12]. In January 2020, Government of Nepal passed a “One Health Strategy 2020” to work on zoonoses and antimicrobial resistance [28].
Nepal allocated around 1 million US dollars to buy anti-rabies vaccinations in 2018/19 [8]. In the Stepwise Approach for Rabies Elimination (SARE) assessment, Nepal is between 0 and 1 and under this scenario it will take 12–13 years to stamp out the disease [28]. Weak intersectoral coordination among different stakeholders, poor governance structure and cross border issues are the major bottlenecks in control of rabies in Nepal.
1.1.6. Pakistan
Rabies, a priority zoonotic disease in Pakistan in 2017, is reported to kill 2000–5000 humans every year. Pakistan is currently at stage 1.5 on its way to stage 2 according to the SARE assessment conducted in 2017 [31]. Strategies that have been applied in the national capital, Islamabad, to control rabies including online reporting of dog bites, registration and control of dogs by implementation of the Punjab Local Government Act 2013 and responding to rabies outbreaks by Provincial Disease Surveillance and Response Units (PDSRUs) [13] although rabies control programmes are confined to the capital and some other cities. Inadequate epidemiological surveillance and information, lack of multisectoral collaboration, unsettled national policies and lack of adequate resources are existing challenges to the control of rabies in Pakistan.
1.1.7. Srilanka
Rabies is endemic in Sri Lanka and is notifiable in both animals and humans. Human deaths due to rabies decreased from 370 in 1970 to 19 in 2014 with current estimates of 20–30 human deaths per year [8,32].
Mass dog vaccination, ABC surgeries, proper garbage disposal and training of personnel are the principal activities in Sri Lanka for rabies control. Neutering of over 150,000 female dogs and vaccination of 150,000 stray dogs and 1.35 million domestic dogs per year are key activities [14]. The Rabies Ordinance and the National Plan for Rabies Control and Prevention are the policies for the control of rabies [13]. Both the animal health and public health sectors are involved in the dog rabies vaccination programme. Rapid change in dog population dynamics, lack of collaborative rabies surveillance networks, and lack of a strategy to control stray dogs are the major hindrances to control rabies in Sri Lanka [14].
2. Summary of national activities
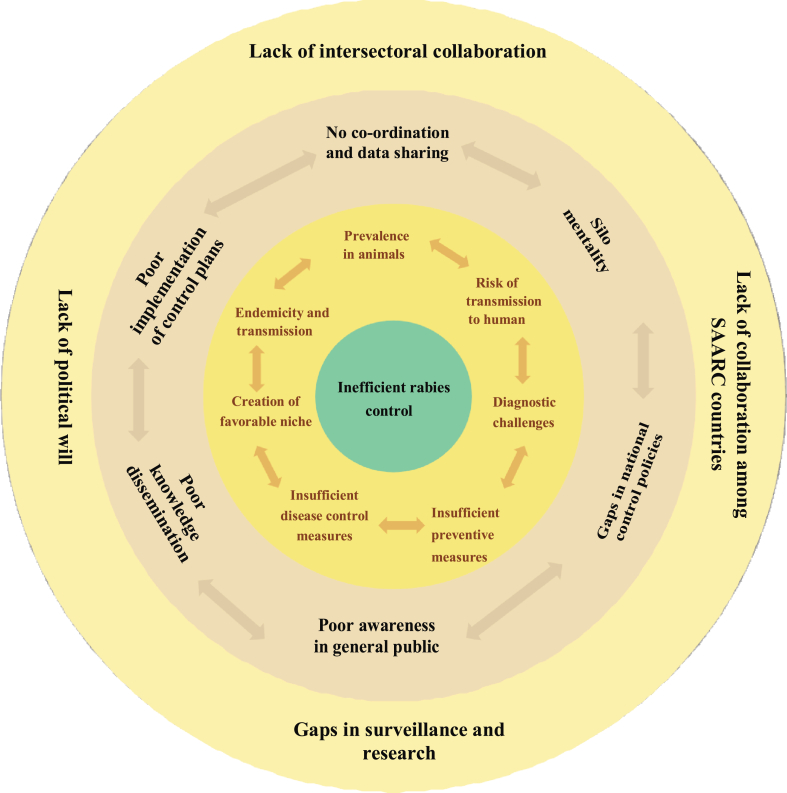
All South Asian countries attempt to control or eliminate rabies. Millions of dollars have been invested, various guidelines and strategies have been adopted but most targets have yet to be achieved. Various organizations work in various ways but something is lacking in the strategy of most SAARC countries. This lack covers regulation, coordination, collaboration, division of work, and communication among stakeholders related to animal health and human health (Fig. 2). This gap can be fulfilled by implementing a One Health approach.
Fig. 2.
Factors behind inefficient Rabies control programs in SAARC nations.
3. The One Health approach
The One Health (OH) approach is growing but could not progress towards institutionalization in much of South Asia in spite of funding and advice from the international community [33]. The principal reasons are limited political support, an inappropriate legal framework, a dearth of technical expertise, budgetary constraints, limited data sharing mechanisms and lack of coordination among the various components that should be promoting and implementing OH activities [34,35]. Nepal is a good example of the problems of OH [36]. India has similar problems to those of Nepal whereas Bangladesh has an ambitious health policy at national level and a separate framework for infectious disease control under an organized OH approach [37].
Three of the region's biggest countries – India, Pakistan and Bangladesh – are among the world's top five rabies endemic countries [5]. The OH approach has been found helpful in controlling zoonoses and has been practised effectively in some countries over several years [36]. Bhutan, Sri Lanka and Bangladesh have successfully reduced deaths from rabies over time using the OH approach.
Human population increase, urbanization, invasion of farmland and forested areas have resulted in closer and more constant contact between people and wildlife [38]. Exchange of pathogens, including rabies, occurs at the interface between humans and animals [38]. The true extent of human mortality from rabies is unknown because of massive under-reporting, the disease has been accorded priority for the OH approach in South Asia. A multi-sectoral OH approach would facilitate the promotion of actions for all sectors but would impose only one cost (mass dog vaccination costs are borne by the animal health sector but provide important benefits to public health) [38]. The World Health Organization (WHO), the Food and Agriculture Organization (FAO) and the South Asian Association for Regional Co-operation (SAARC)) independently help to strengthen the OH approach for rabies prevention in the region. A regional comprehensive integrated rabies control programme has been established with funding from the WHO's South East Asian Regional Office [38]. FAO's Regional Support Unit for SAARC incorporates OH components where possible. The One Health Alliance of South Asia (OHASA) network, involving wildlife, livestock and human health scientists and policymakers from Bangladesh, India, Nepal and Pakistan aims to develop trans-boundary and interdisciplinary approaches to the prevention and control of zoonotic disease outbreaks [38,39]. The main animal and human health concerns have been identified as zoonotic influenza, canine mediated human rabies and antimicrobial resistance [40]. Each problem has an impact or effect on animal, human and environmental health in some cases and is most likely to be overcome by working in collaboration or providing information to multiple sectors. A Regional Capacity Building project under Eco-Health (OHASA) addresses training of trainers, holds health days for public awareness and mass vaccination of dogs.
Eradication of rabies in several Asian [12] and some European [41] countries using a collaborative OH approach is an excellent example for South Asian countries. The initiatives of welfare and other charitable organizations are important in creating increased awareness of pre- and post-exposure prophylaxis. Control measures known to be effective could lead to the elimination of rabies in the medium term. Such a situation would result in improved human health, lower healthcare costs and increased livelihood benefits.
Progress has been made in institutionalizing OH in some South Asian countries but there is a need for further behavioural, attitudinal and institutional transformation to enhance OH. Training in and the implementation of integrated zoonotic control policies that are sustainable are also required. Deficiencies in the institutionalization of the OH approach include a lack of relevant scientific information and collaboration in the development and implementation of integrated zoonotic disease management policies as well as the continuing need to support trans-disciplinary OH research and politically based policy-relevant capacity building programmes [35].
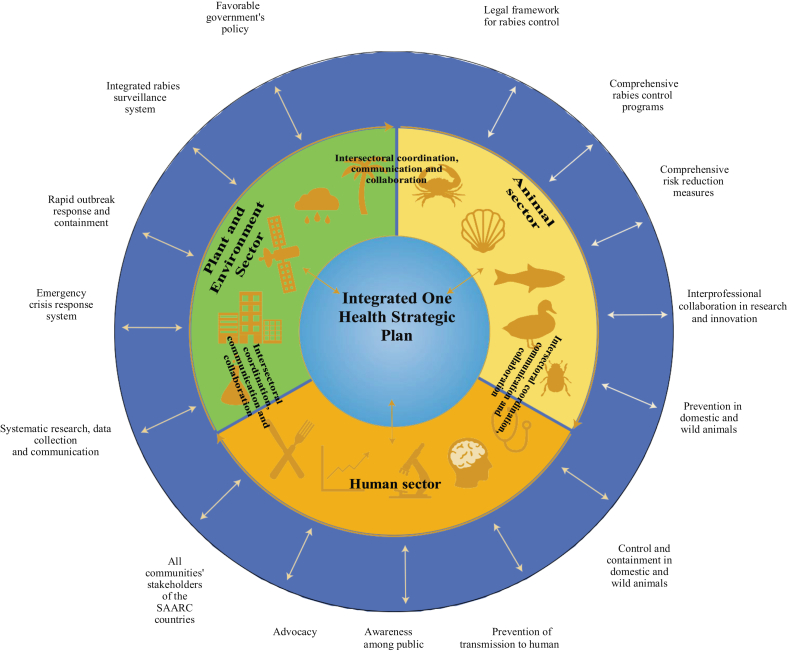
The number of people bitten by dogs is increasing in much of the region Asia. Control has been ineffective due to a general lack of awareness for pre-exposure and post-exposure prophylaxis. Low vaccine efficacy due to a failure to follow the proper cold chain procedures and possibly poor vaccine quality are further problems. Rabies is incurable but is preventable. Active participation and collaboration with and among farmers, animal health workers, veterinary professionals, medical professionals, politicians and a range of other stakeholders in an OH approach is required. Achieving this type of action is compounded in the South Asian region due to diverse cultures and traditions and to political instability [42]. The Model framework to promote intersectoral collaboration is presented in the Fig. 3.
Fig. 3.
Model framework for coordinated One Health approach to control rabies in South Asia (Skeleton of the figure adapted from https://doi.org/10.1038/s43016-020-0127-5 with permission from corresponding author of the paper).
4. Actions required for the control and elimination of rabies in South Asia
4.1. Co-ordination and data sharing among human, animal, plant and environmental health sectors
Poor data and sample sharing is a major hindrance to OH but is very important for the control of zoonotic diseases. Most South Asian countries lack relevant and formal mechanisms for coordination and collaboration across the human health, animal health, agriculture and environment sectors. Different ministries and departments have separate working frameworks and budgets. Collection and management of the primary data involving multisectoral effort and constructing local, regional, national and international databases would provide a clearer image of the scenario and burden of the disease which could then further assist in the implementation of control strategies. Systematic data collection and compilation involving dog population surveys, number of suspected and confirmed dog and human rabies cases, human-dog population densities, vaccination record on animals and humans and extensive data management and analysis are pivotal for rabies control and elimination [28].
4.2. Risk analysis and efficient surveillance system to capture both clinical and non-clinical cases of rabies in domestic and wild animals
Under-reporting and the current lack of cooperative and collaborative working among stakeholders mean there is a pressing need for a systematic application of OH in South Asia to control and eliminate rabies. Improvement of surveillance of animal and human rabies should be based on improving case definitions and standardizing clinical reporting and laboratory confirmation. Epidemiological and sociological surveys are needed in order determine the order and magnitude of risk factors. Prevalence studies in domestic animals, community and street dogs and wild animals will assist forecasting of the rabies situation in a given period and pattern and trend of rabies that will ultimately support the strengthening and effectiveness of rabies control programmes. Surveillance has an important role in the containment of rabies but there is no systematic and organized surveillance system in most of South Asia although Bangladesh and Bhutan are making significant progress [43]. Risk analysis via epidemiological research and surveys involving multisectoral stakeholders are essential for the formulation of control strategies and programmes. Oral Rabies Vaccination (ORV) is the best method for control of rabies in the wild. Rabies has been eliminated among red foxes (Vulpes vulpes) in various European countries; in coyotes in the USA [44], and racoons in Canada [45]. Trials and feasibility studies are under way among community dogs in India [46] and Bangladesh [47].
4.3. Strengthening laboratory capacities
Well-equipped laboratories and their diagnostic capacity are a major focus area for rabies prevention and control. Such laboratories are confined to big cities in South Asia but the rabies burden is high in underprivileged and rural areas [8] where no or minimal diagnostic facilities are available. Animal and human rabies are often neglected due to inadequate laboratory capacity inadequate knowledge of diagnosis. Upgrading existing laboratories to OIE standards and establishment of new laboratories are important for rabies prevention [28].
4.4. Increased vaccination coverage and improved efficiency of vaccination
Mass Dog Vaccination is considered an appropriate [48] and cost-effective way of rabies control [49,50]. Several developed Asian countries have successfully eradicated dog mediated rabies via MDV and dog population control [12]. Srilanka [12], Bangladesh [51] and Bhutan [22] have significantly reduced the number of human and animal rabies. According to WHO and OIE, vaccination of 70% or more of dog populations will decrease the rabies infection rate and subsequently reduce human exposure [28]. Vaccination, identification and record keeping of both domesticated and free-ranging dogs are necessary along with follow up booster doses. Vaccination cover and the quality and efficiency of the vaccination are important in rabies control and elimination. Vaccines should be authentic and certified by the manufacturers and care should be taken during storage, transportation and handling to increase the impact of control strategies.
4.5. Conducive and practical legal framework for rapid outbreak response and containment
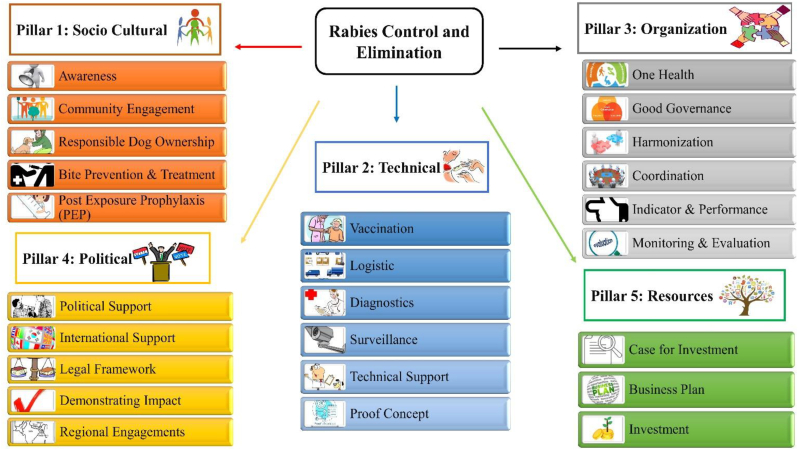
A global strategic plan has been developed to end human deaths from rabies by 2030 (Fig. 4) [52]. A regional strategy for control and elimination of dog mediated human rabies has also been developed by the WHO Regional Office for Southeast Asia in 2012 [53]. This plan should provide a conducive and practical legal framework for the rapid outbreak response and containment that is needed for successful rabies control in SAARC countries.
Fig. 4.
Global strategic framework: five pillars for rabies control and elimination (Content of the figure adapted from https://www.oie.int/fileadmin/Home/eng/Media_Center/docs/pdf/Rabies_portal/EN_TimeisnowGlobalFramework.pdf).
4.6. Advocacy and awareness campaigns
Education, advocacy and public awareness are of significance in the fight against all diseases. In South Asia, illiteracy is very high with women and children accounting for the major portion [54]. As children are more prone to rabies infection school awareness is key for rabies control.
Awareness programmes on radio and television, knowledge sharing via newspaper and online news, posters and banners on walls, educational seminars, mass rallies and school awareness are common in South Asia but usually conducted on special occasion such as World Rabies Day. There is need of regular education and awareness about rabies prevention, clinical manifestations, identification of rabid dogs and importance of vaccination especially among children and women. Education authorities need to include rabies in school course work focusing on general information on rabies, signs and symptoms, preventive measures, the necessity of dog vaccination, PEP and responsible dog ownership. Rabies awareness and education in youths and school students will disseminate to the entire family ensuring sustainable strategies and intervention in future generations [48].
4.7. Comprehensive risk reduction measure
Rabies is vaccine preventable. The risk of contracting rabies is higher in South Asia than anywhere else in the world. The region accounts for 45% of all the world's human deaths [55]. High numbers of stray dogs and unavailability of PEP immediately following a dog bite are major risks. Availability of PEP and the integrated dog bite case management (IBCM) approach together with surveillance involving public health and animal health officers are key factors for risk reduction in any area [56,57]. Waste management and Catch-Neuter-Vaccinate-Release (CNVR) programs should be put in practice as part of a comprehensive risk reduction strategy. Vaccination and ABC programmes need to be complemented by carrying capacity control via waste management for effective control [58].
4.8. Investigations of the bio-social conditions
Investigations of the bio-social conditions that contribute to dog-human confrontation are needed and actions must be implemented to mitigate the negative impacts (one example of a confrontation zone relates to the large heaps of foetid household waste food and other detritus where dog fights are common). Local knowledge should be tapped and built upon to develop techniques and materials for relatively safer cohabitation.
5. Conclusions
The best pathway to rabies control and elimination appears to be the OH one. OH requires coordination and exchange of actions and data among all parties and across all disciplines and countries. It is also important to provide educational programmes for young people that highlight the importance of wound treatment and the need for post-exposure prophylaxis (PEP). All this is feasible through a coordinated OH approach to achieving rabies prevention, control and eradication in South Asia.
Authors' contributions
Conceptualization: KPA. Data curation: KPA, DS & RTW. Formal analysis: KPA, DS & RTW. Investigation: KPA. Methodology: KPA, DS & RTW. Project administration: KPA. Resources: KPA. Software: KPA. Supervision: RTW. Validation: KPA & RTW. Visualization: KPA. Writing - original draft: KPA. Writing - review & editing: KPA, DS & RTW.
Ethics approval
Not applicable.
Funding
No external funding was used in the preparation of this paper.
Declaration of Competing Interest
There are no competing interests.
References
- 1.Destoumieux-Garzón D., Mavingui P., Boetsch G., Boissier J., Darriet F., Duboz P., Fritsch C., Giraudoux P., Le Roux F., Morand S., Paillard C., Pontier D., Sueur C., Voituron Y. The one health concept: 10 years old and a long road ahead. Front. Vet. Sci. 2018 doi: 10.3389/fvets.2018.00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marbán-Castro E., Mattar S., González T.M. Reemerging zoonoses with “One Health” approach. Rev. MVZ Córdoba. 2019 doi: 10.21897/rmvz.1777. [DOI] [Google Scholar]
- 3.Hossain M., Ahmed K., Bulbul T., Hossain S., Rahman A., Biswas M.N.U., Nishizono A. Human rabies in rural Bangladesh. Epidemiol. Infect. 2012;140:1964–1971. doi: 10.1017/S095026881100272X. [DOI] [PubMed] [Google Scholar]
- 4.Hampson K., Coudeville L., Lembo T., Sambo M., Kieffer A., Attlan M., Barrat J., Blanton J.D., Briggs D.J., Cleaveland S., Costa P., Freuling C.M., Hiby E., Knopf L., Leanes F., Meslin F.X., Metlin A., Miranda M.E., Müller T., Nel L.H., Recuenco S., Rupprecht C.E., Schumacher C., Taylor L., Vigilato M.A.N., Zinsstag J., Dushoff J. Estimating the Global Burden of Endemic Canine Rabies. PLoS Negl. Trop. Dis. 2015 doi: 10.1371/journal.pntd.0003709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chowdhury F.R., Basher A., Amin M., Hassan N., Patwary M. Rabies in South Asia: fighting for elimination. Recent Pat. Antiinfect. Drug Discov. 2015 doi: 10.2174/1574891x10666150410130024. [DOI] [PubMed] [Google Scholar]
- 6.Tauseef Ahmad H.J. Taha Hussein Musa, Rabies in Asian Countries: where we are stand? Biomed. Res. Ther. 2018;5:2719–2720. doi: 10.4103/2230-8598.109313. [DOI] [Google Scholar]
- 7.WHO SEARO Rabies Workshop Enhancing Progress Towards Rabies Elimination. 2019. http://origin.searo.who.int/entity/rabies/workshop-enhancing-progress-towards-rabies-elimination/ Available at:
- 8.Pantha S., Subedi D., Poudel U., Subedi S., Kaphle K., Dhakal S. Review of rabies in Nepal. One Heal. 2020;10:100155. doi: 10.1016/j.onehlt.2020.100155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gholami A., Alamdary A. The World Rabies Day 2020: collaborate and vaccinate, Iran. Biom. J. 2020;24:264–268. doi: 10.29252/ibj.24.5.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.WHO . 2006. The Control of Neglected Zoonotic Diseases: A Route to Poverty Alleviation: Report of a Joint WHO/DFID-AHP Meeting; pp. 1–65.www.who.int/zoonoses/Report_Sept06.pdf Available at: [Google Scholar]
- 11.Coleman P.G., Dye C. Immunization coverage required to prevent outbreaks of dog rabies. Vaccine. 1996 doi: 10.1016/0264-410X(95)00197-9. [DOI] [PubMed] [Google Scholar]
- 12.Tenzin T., Ward M.P. Review of rabies epidemiology and control in South, South East and East Asia: past, present and prospects for elimination. Zoonoses Public Health. 2012 doi: 10.1111/j.1863-2378.2012.01489.x. [DOI] [PubMed] [Google Scholar]
- 13.FAO, OIE W.H.O., SAARC Enhancing Progress towards Rabies Elimination ‘ Zero by 30 ’ in SAARC Region. 2019. https://www.saohnet.org/wp-content/uploads/2019/12/Enhancing-Progress-towards-Rabies-Elimination-Zero-by-30-in-SAARC-Region_V3.5_20191122.pdf Available at:
- 14.WHO Prevention and Control of Rabies in SAARC Countries, in: Colombo, Sri Lanka. 2015. http://origin.searo.who.int/entity/emerging_diseases/documents/sea_cd_316.pdf Available at:
- 15.Abdul-Jalil M. Working to Remove the Fear of Rabies from Kabul, Afghanistan. 2020. https://endrabiesnow.org/stories/view/working-to-remove-the-fear-of-rabies-from-kabul-afghanistan
- 16.Tenzin T., Ahmed R., Debnath N.C., Ahmed G., Yamage M. Free-roaming dog population estimation and status of the dog population management and rabies control program in Dhaka City, Bangladesh. PLoS Negl. Trop. Dis. 2015;9:1–14. doi: 10.1371/journal.pntd.0003784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hossain M., Bulbul T., Ahmed K., Ahmed Z., Salimuzzaman M., Shahidul M., Ali A., Hossain S., Yamada K., Moji K., Nishizono A. Five-year ( January 2004 – December 2008 ) surveillance on animal bite and rabies vaccine utilization in the Infectious Disease Hospital, Dhaka, Bangladesh. Vaccine. 2011;29:1036–1040. doi: 10.1016/j.vaccine.2010.11.052. [DOI] [PubMed] [Google Scholar]
- 18.Li A.J., Sreenivasan N., Ruman U., Tahmina S., Penjor K., Sovann L., Gunesekera A., Blanton J.D., Knopf L., Hyde T.B. Descriptive assessment of rabies post-exposure prophylaxis procurement, distribution, monitoring, and reporting in four Asian countries. Vaccine. 2019;37:A14–A19. doi: 10.1016/j.vaccine.2018.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.WHO . WHO; 2017. The Rabies Elimination Program of Bangladesh.https://www.who.int/neglected_diseases/news/Bangladesh-rabies-elimination-program/en/ Available at: [Google Scholar]
- 20.Rinchen S., Tenzin T., Hall D., Van Der Meer F., Sharma B., Dukpa K., Cork S. A community-based knowledge, attitude, and practice survey on rabies among cattle owners in selected areas of Bhutan. PLoS Negl. Trop. Dis. 2019;13(4):1–17. doi: 10.1371/journal.pntd.0007305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Penjor K., Tenzin T., Jamtsho R.K. Determinants of health seeking behavior of animal bite victims in rabies endemic South Bhutan: a community-based contact-tracing survey. BMC Public Health. 2019;19:1–11. doi: 10.1186/s12889-019-6559-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rinchen S., Tenzin T., Hall D., Cork S. A Qualitative risk assessment of rabies reintroduction into the rabies low-risk zone of Bhutan. Front. Vet. Sci. 2020;7:1–11. doi: 10.3389/fvets.2020.00366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Radhakrishnan S., Vanak A.T., Nouvellet P. Rabies as a public health concern in India — A historical perspective. Trop. Med. Infect. Dis. 2020;5(162):1–23. doi: 10.3390/tropicalmed5040162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.National Centre for Disease Control India Diseases under Surveillance: Integrated Disease Surveillance Programme(IDSP) 2020. https://idsp.nic.in/index1.php?lang=1&level=1&sublinkid=5985&lid=3925 Available at:
- 25.Government of India 11th Five Year Plan, 2015. 2007. https://niti.gov.in/planningcommission.gov.in/docs/plans/planrel/fiveyr/welcome.html Available at:
- 26.Gibson A.D., Wallace R.M., Rahman A., Bharti O.K., Isloor S., Lohr F., Gamble L., Mellanby R.J., King A., Day M.J. Reviewing solutions of scale for canine rabies elimination in India. Trop. Med. Infect. Dis. 2020;5:1–21. doi: 10.3390/tropicalmed5010047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rupprecht C.E., Abela-Ridder B., Abila R., Amparo A.C., Banyard A., Blanton J., Chanachai K., Dallmeier K., de Balogh K., Vilas V.D.R., Ertl H. Towards rabies elimination in the Asia-Pacific region: from theory to practice. Biologicals. 2020;64:83–95. doi: 10.1016/j.biologicals.2020.01.008. [DOI] [PubMed] [Google Scholar]
- 28.Acharya K.P., Acharya N., Phuyal S., Upadhyaya M., Lasee S. One-health approach: a best possible way to control rabies. One Heal. 2020;10:100161. doi: 10.1016/j.onehlt.2020.100161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Free Dog Rabies Vaccination in 24 Municipalities of Nepal. Vol. 14. Zoonoses and Food Hygiene News; 2008. pp. 1–5.http://nzfhrc.org.np/wp-content/uploads/2016/08/V14N1.pdf Available at: [Google Scholar]
- 30.EDCD National Guideline for Rabies Prophylaxis and Management in Nepal. 2019. http://www.edcd.gov.np/resources/download/national-guidelines-for-rabies-prophylaxis-and-management-in-nepal-new Available at:
- 31.GARC Pakistan rabies elimination progress. 2018. https://rabiesalliance.org/country/pakistan Available at:
- 32.Nihal P.D.B., Dangolla A., Hettiarachchi R., Abeynayake P., Stephen C. Surveillance Opportunities and the Need for Intersectoral Collaboration on Rabies in Sri Lanka. J. Vet. Med. 2019;2019:1–8. doi: 10.1155/2019/7808517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dahal R., Upadhyay A., Ewald B. One Health in South Asia and its challenges in implementation from stakeholder perspective. Vet. Rec. 2017 doi: 10.1136/vr.104189. [DOI] [PubMed] [Google Scholar]
- 34.Pal M., SK Siddiky. Veterinary Public Health and Zoonotic Disease Control in SAARC Countries. 2011. http://www.sac.org.bd/archives/publications/vph&zdc.pdf Available at:
- 35.McKenzie J.S., Dahal R., Kakkar M., Debnath N., Rahman M., Dorjee S., Naeem K., Wijayathilaka T., Sharma B.K., Maidanwal N., Halimi A., Kim E., Chatterjee P., Devleesschauwer B. One Health research and training and government support for One Health in South Asia. Infect. Ecol. Epidemiol. 2016 doi: 10.3402/IEE.V6.33842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Acharya K.P., Karki S., Shrestha K., Kaphle K. One health approach in Nepal: Scope, opportunities and challenges. One Heal. 2019 doi: 10.1016/j.onehlt.2019.100101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chatterjee P., Kakkar M., Chaturvedi S. Integrating one health in national health policies of developing countries: India's lost opportunities. Infect. Dis. Poverty. 2016 doi: 10.1186/s40249-016-0181-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hassell J.M., Begon M., Ward M.J., Fèvre E.M. Urbanization and Disease Emergence: Dynamics at the Wildlife–Livestock–Human Interface. Trends Ecol. Evol. 2017 doi: 10.1016/j.tree.2016.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Aguirre D.P. A One Health Alliance of South Asia (OHASA): predicting and preventing the next emerging disease on the Indian subcontinent - sponsored by the rockefeller foundation. 1st Int. One Heal. Congr. Abstr. Plenary. 2011;7:8–170. doi: 10.1007/s10393-010-0376-0. [DOI] [Google Scholar]
- 40.FAO, OIE, WHO A tripartite guide to addressing zoonotic diseases in countries taking a multisectoral. One Heal App. 2019 https://www.oie.int/fileadmin/Home/eng/Media_Center/docs/EN_TripartiteZoonosesGuide_webversion.pdf Available at: [Google Scholar]
- 41.Aikimbayev A., Briggs D., Coltan G., Dodet B., Farahtaj F., Imnadze P., Korejwo J., Moiseieva A., Tordo N., Usluer G., Vodopija R., Vranješ N. Fighting rabies in Eastern Europe, the Middle East and Central Asia - experts call for a regional initiative for rabies elimination. Zoonoses Public Health. 2014 doi: 10.1111/zph.12060. [DOI] [PubMed] [Google Scholar]
- 42.Gongal G., Wright A.E. Human rabies in the WHO Southeast Asia region: forward steps for elimination. Adv. Prev. Med. 2011 doi: 10.4061/2011/383870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.WHO . 2012. Strategic Framework for Elimination of Human Rabies Transmitted by Dogs in the South-East Asia Region; pp. 1–60.https://apps.who.int/iris/bitstream/handle/10665/205920/B4891.pdf?sequence=1&isAllowed=y Available at: [Google Scholar]
- 44.Slate D., Algeo T.P., Nelson K.M., Chipman R.B., Donovan D., Blanton J.D., Niezgoda M., Rupprecht C.E. Oral rabies vaccination in North America: opportunities, complexities, and challenges. PLoS Negl. Trop. Dis. 2009;3:1–9. doi: 10.1371/journal.pntd.0000549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Elmore S.A., Chipman R.B., Slate D., Huyvaert K.P., VerCauteren K.C., Gilbert A.T. Management and modeling approaches for controlling raccoon rabies: The road to elimination. PLoS Negl. Trop. Dis. 2017 doi: 10.1371/journal.pntd.0005249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gibson A.D., Mazeri S., Yale G., Desai S., Naik V., Corfmat J., Ortmann S., King A., Müller T., Handel I., Bronsvoort B.M.C., Gamble L., Mellanby R.J., Vos A. Development of a non-meat-based, mass producible and effective bait for oral vaccination of dogs against rabies in Goa State, India. Trop. Med. Infect. Dis. 2019;4:1–13. doi: 10.3390/tropicalmed4030118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bonwitt J., Bonaparte S., Blanton J., Gibson A.D., Hoque M., Kennedy E., Islam K., Siddiqi U.R., Wallace R.M., Azam S. Oral bait preferences and feasibility of oral rabies vaccination in Bangladeshi dogs. Vaccine. 2020;38:5021–5026. doi: 10.1016/j.vaccine.2020.05.047. [DOI] [PubMed] [Google Scholar]
- 48.Miranda M.E.G., Miranda N.L.J. Rabies and Rabies Vaccines. s. 2020. Rabies prevention in Asia: Institutionalizing implementation capacities; pp. 103–116. [DOI] [Google Scholar]
- 49.Kelly T.R., Machalaba C., Karesh W.B., Crook P.Z., Gilardi K., Nziza J., Uhart M.M., Robles E.A., Saylors K., Joly D.O., Monagin C., Mangombo P.M., Kingebeni P.M., Kazwala R., Wolking D., Smith W., Mazet J.A.K. Implementing One Health approaches to confront emerging and re-emerging zoonotic disease threats: lessons from PREDICT. One Heal. Outlook. 2020;2:1–7. doi: 10.1186/s42522-019-0007-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zinsstag J., Dürr S., Penny M.A., Mindekem R., Roth F., Menendez Gonzalez S., Naissengar S., Hattendorf J. Transmission dynamics and economics of rabies control in dogs and humans in an African city. Proc. Natl. Acad. Sci. U. S. A. 2009 doi: 10.1073/pnas.0904740106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ghosh S., Rana M.S., Islam M.K., Chowdhury S., Haider N., Kafi M.A.H., Ullah S.M., Shah M.R.A., Jahan A.A., Mursalin H.S., Marma A.S.P., Ali S.M.E., Hossain S., Bhowmik R., Debnath N.C., Shamsuzzaman A.K.M., Ahmed B.N., Siddiqi U.R., Jhora S.T. Trends and clinico-epidemiological features of human rabies cases in Bangladesh 2006–2018. Sci. Rep. 2020;10:1–12. doi: 10.1038/s41598-020-59109-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.WHO, FAO, OIE, GARC Zero by 30: The global strategic plan to prevent human deaths from dog-transmitted rabies by 2030 why eliminate rabies? Call Action. 2015:0–1. https://www.who.int/rabies/Executive_summary_draft_V3_wlogo.pdf?ua=1 Available at: [Google Scholar]
- 53.OIE ASEAN Rabies Elimination Strategy. 2016. https://asean.org/storage/2017/02/ASEAN-Rabies-Elimination-Strategy Available at:
- 54.Zakaria M., Tariq S., Iftikhar M. 2019. Socio-economic, Macroeconomic, Demographic, and Environmental Variables as Determinants of Child mortality In South Asia. [DOI] [PubMed] [Google Scholar]
- 55.Pant G.R. OIE; 2013. Rabies Control Strategy in SAARC member countries.https://www.oie.int/doc/ged/D12940.pdf Available at: [Google Scholar]
- 56.Undurraga E.A., Meltzer M.I., Tran C.H., Atkins C.Y., Etheart M.D., Millien M.F., Adrien P., Wallace R.M. Cost-effectiveness evaluation of a novel integrated bite case management program for the control of human rabies, Haiti 2014-2015. Am. J. Trop. Med. Hyg. 2017 doi: 10.4269/ajtmh.16-0785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pieracci E. Integrated bite case management (IBCM) Glob. Alliance Rabies Control. 2018 https://rabiesalliance.org/resource/emily-pieracciibcm-2018paracon-2018 Available at: [Google Scholar]
- 58.Masud M.A., Islam M.H., Adnan M.I., Oh C. Dog rabies in Dhaka, Bangladesh, and implications for control. Processes. 2020;8:1–15. doi: 10.3390/pr8111513. [DOI] [Google Scholar]