Key Points
Question
Is risk-reducing salpingo-oophorectomy associated with a reduction in breast cancer risk for women with pathogenic variants in the BRCA1 and BRCA2 genes?
Findings
In this case series of 876 families, risk-reducing salpingo-oophorectomy was associated with a reduced risk of breast cancer in women with BRCA1 and BRCA2 pathogenic variants within 5 years after surgery, with weaker association more than 5 years postsurgery. For BRCA1 and BRCA2 carriers who underwent risk-reducing salpingo-oophorectomy at age 40 years, the cumulative risk of breast cancer was 49.7% and 52.7%, respectively, by 70 years.
Meaning
Risk-reducing salpingo-oophorectomy was associated with a reduction in breast cancer risk for women carrying the BRCA1 and BRCA2 pathogenic gene variants, with a longer-term association with cumulative risk among women carrying BRCA1 pathogenic variants.
This case series uses data from 876 families with BRCA1 and BRCA2 variants from the Breast Cancer Family Registry to assess whether risk-reducing salpingo-oophorectomy is associated with a reduction in breast cancer risk for women carrying these pathogenic variants.
Abstract
Importance
Women with pathogenic variants in BRCA1 and BRCA2 are at high risk of developing breast and ovarian cancers. They usually undergo intensive cancer surveillance and may also consider surgical interventions, such as risk-reducing mastectomy or risk-reducing salpingo-oophorectomy (RRSO). Risk-reducing salpingo-oophorectomy has been shown to reduce ovarian cancer risk, but its association with breast cancer risk is less clear.
Objective
To assess the association of RRSO with the risk of breast cancer in women with BRCA1 and BRCA2 pathogenic variants.
Design, Setting, and Participants
This case series included families enrolled in the Breast Cancer Family Registry between 1996 and 2000 that carried an inherited pathogenic variant in BRCA1 (498 families) or BRCA2 (378 families). A survival analysis approach was used that was designed specifically to assess the time-varying association of RRSO with breast cancer risk and accounting for other potential biases. Data were analyzed from August 2019 to November 2020.
Exposure
Risk-reducing salpingo-oophorectomy.
Main Outcomes and Measures
In all analyses, the primary end point was the time to a first primary breast cancer.
Results
A total of 876 families were evaluated, including 498 with BRCA1 (2650 individuals; mean [SD] event age, 55.8 [19.1] years; 437 White probands [87.8%]) and 378 with BRCA2 (1925 individuals; mean [SD] event age, 57.0 [18.6] years; 299 White probands [79.1%]). Risk-reducing salpingo-oophorectomy was associated with a reduced risk of breast cancer for BRCA1 and BRCA2 pathogenic variant carriers within 5 years after surgery (hazard ratios [HRs], 0.28 [95% CI, 0.10-0.63] and 0.19 [95% CI, 0.06-0.71], respectively), whereas the corresponding HRs were weaker after 5 years postsurgery (HRs, 0.64 [95% CI, 0.38-0.97] and 0.99 [95% CI; 0.84-1.00], respectively). For BRCA1 and BRCA2 pathogenic variant carriers who underwent RRSO at age 40 years, the cause-specific cumulative risk of breast cancer was 49.7% (95% CI, 40.0-60.3) and 52.7% (95% CI, 47.9-58.7) by age 70 years, respectively, compared with 61.0% (95% CI, 56.7-66.0) and 54.0% (95% CI, 49.3-60.1), respectively, for women without RRSO.
Conclusions and Relevance
Although the primary indication for RRSO is the prevention of ovarian cancer, it is also critical to assess its association with breast cancer risk in order to guide clinical decision-making about RRSO use and timing. The results of this case series suggest a reduced risk of breast cancer associated with RRSO in the immediate 5 years after surgery in women carrying BRCA1 and BRCA2 pathogenic variants, and a longer-term association with cumulative breast cancer risk in women carrying BRCA1 pathogenic variants.
Introduction
Women carrying pathogenic variants in BRCA1 and BRCA2 are at high risk of developing breast cancer (BC) and ovarian cancer (OC). Large meta-analyses reported mean cumulative BC risks by age 70 years of 57% for BRCA1 pathogenic variant carriers and 49% for BRCA2 pathogenic variant carriers.1,2 The equivalent OC risks are estimated at 40% for BRCA1 and 18% for BRCA2 pathogenic variant carriers. Women with BRCA1 or BRCA2 pathogenic variants undergo intensive cancer surveillance and may also consider surgical interventions, such as risk-reducing mastectomy (RRM) or risk-reducing salpingo-oophorectomy (RRSO), which has been shown to reduce OC risk, although its association with BC risk is less clear. Specifically, early studies consistently supported a BC risk reduction of up to 50% following RRSO.3,4,5,6 These results were later refuted by analyses that considered RRSO as a time-varying covariate, ie, assuming that the association of RRSO with BC only starts after surgery rather than counting all cancer-free time as time attributed to RRSO.7,8 Additional studies confirmed that when RRSO is treated as a time-varying covariate, there is no association between RRSO and BC risk in women with BRCA1 pathogenic variants9,10,11 as well as in other high-risk women. The association in women with BRCA2 pathogenic variants, although not statistically significant, showed a reduced association in each of these same studies. These studies, which treated RRSO as a time-varying covariate, assumed that the association with RRSO remains constant each year from the time of surgical intervention, also known as the permanent exposure hypothesis. Interestingly, a recent study that treated RRSO as an intermediate event before the occurrence of BC (known as a multistate approach) concluded that the risk of BC after premenopausal RRSO decreased significantly in BRCA1 carriers (hazard ratio [HR], 0.45) but was not conclusive in BRCA2 carriers (HR, 0.77).12 A systematic review performed by the same authors suggested that premenopausal RRSO was associated with a decrease of BC risk in both BRCA1 and BRCA2 carriers.
The current recommendation for RRSO as an OC-preventive measure is that it should be offered between the ages of 35 and 40 years and may be delayed to ages 40 to 45 years for BRCA2 carriers.13 Additionally, RRM or breast surveillance with annual contrast-enhanced magnetic resonance imaging and mammography are offered to premenopausal BRCA1 and BRCA2 carriers. Assessing the association of RRSO with BC risk could therefore be critical for women deciding between surveillance and prophylactic surgery. The risk-benefit ratio of such a strategy needs also to be assessed carefully, because offering RRSO at a young age might induce adverse effects such as reduced quality of life, cardiovascular disease, or osteoporosis.14
In this study, we estimated the association between RRSO and BC risk using a family-based analysis of BRCA1 and BRCA2 pathogenic variant carrier families recruited through the Breast Cancer Family Registry (BCFR), taking into consideration the complex nature of RRSO association with BC over time and additional potential methodologic issues including the permanent exposure hypothesis.
Methods
Breast Cancer Family Registry
This case series evaluated family data from the BCFR, which was established in 1995 with 6 participating sites from the US, Australia, and Canada.15 The BCFR enrolled most of the families from 1996 to 2000 while continuing to recruit additional families satisfying certain eligibility criteria. Clinic-based families were included whenever they carried BRCA1 or BRCA2 pathogenic variants, exhibited multiple cases of BC or OC, were of Ashkenazi Jewish ancestry, or were from specific racial and ethnic groups. For the population-based families, newly diagnosed BC cases were ascertained through population-based cancer registries, and those individuals were enrolled as probands. Their first- and second-degree relatives were also enrolled. During follow-up, extensive information was collected on ages at the time of BC or OC diagnosis since enrollment in the BCFR, surgeries, and mammographic screening compiled from baseline and follow-up questionnaires as well as pathogenic variant status in BRCA1 and BRCA2 genes.16 We restricted our data analyses to families that were known to carry BRCA1 or BRCA2 pathogenic variants.17 All centers in these consortia obtained written informed consent from study participants, and local ethical review committees approved protocols.
Statistical Analysis
Statistical analyses were performed from August 2019 to November 2020. Our methodology is based on a survival analysis approach that was developed specifically to model the occurrence of competing events (ie, invasive primary BC, invasive primary OC, or death from causes other than BC or OC) in family studies.18 We performed separate analyses for families carrying BRCA1 and BRCA2 pathogenic variants. The risk of each competing event (BC, OC, or death) was specified by the hazard function,19 which depends on the pathogenic variant carrier status for BRCA1/2 and for BC on RRSO, modeled as a time-varying covariate. Mammographic screenings were considered as confounding variables for the association between RRSO and BC risk and modeled as binary time-varying covariates (up to 3 mammographic screenings). Indeed, women with more intensive mammographic screenings might have a different history of RRSO (frequency and time to uptake) and association with BC than those with fewer screenings. The follow-up time was defined using age starting from 16 years until a first event (BC, OC, or death) or last observed time. Risk-reducing mastectomy was considered a censoring event for BC and RRSO a censoring event for OC.
We considered the 3 following assumptions for the time-varying association of RRSO with BC: (1) permanent exposure,19 in which this association stays constant since the time of the intervention; (2) exponential decay, in which the association decays over time with a given rate parameter for the exponential decay19; and (3) exponential decay with a threshold parameter (known as Cox and Oakes model),20,21 in which the hazard function for BC decreases until a certain level and then plateaus after that. When the age at RRSO was less than 1 year from the age at BC onset, we considered that both events occurred at the same time and thus RRSO was not associated with BC (n = 12).
The time-varying association of RRSO with BC can be assessed by the HR or by the BC cumulative incidence (ie, the penetrance function). To decide which type of time-dependent association to use for RRSO, we used the Akaike Information Criterion following previously published work.18 We also provide the time-dependent association of RRSO with BC within a specific time interval (≤5 years and >5 years after RRSO uptake) by the average HR over the interval. The 95% CIs for the RRSO-related HRs and BC age-specific cumulative risks (penetrance functions) are based on 1000 simulated sets of the parameters generated from the multivariate normal distribution, with the parameter estimates and their robust variance matrix obtained from the model. We also considered the correlated nature of family-based data; family members who were not tested for BRCA1 and BRCA2 pathogenic variants had their carrier status imputed based on empirical carrier probabilities estimated conditional on the competing risk event status (BC, OC, or death) and on the type of familial relationship to the proband. This permits inclusion of individuals not tested for BRCA1 or BRCA2 pathogenic variants but who contribute information on the association between RRSO and BC risks. Residual familial correlation was also accounted for using a shared frailty (ie, a random component shared by all individuals within the same family that accounts for additional genetic contribution or shared environmental exposures within families).22 Finally, we also corrected for ascertainment bias as these families were recruited through probands with either BC or OC.18 Statistical analyses were conducted using R software, version 3.6.1 (R Core Team). All P values were 2 sided, and P < .05 was considered significant.
Results
Characteristics of BRCA1 and BRCA2 Pathogenic Variant Carrier Families
Our study included a total of 876 families, including 498 with BRCA1 (2650 individuals; mean [SD] event age, 55.8 [19.1] years; 437 White probands [87.8%]) and 378 with BRCA2 (1925 individuals; mean [SD] event age, 57.0 [18.6] years; 299 White probands [79.1%]). The description of these families with respect to the number of events (BC, OC, and deaths), event age distribution, and number of individuals with RRSO is given in Table 1. In BRCA1 and BRCA2 families, the mean (SD) age at RRSO was 44.5 (9.3) years and 46.9 (9.8) years, respectively, and the mean (SD) age at a first BC diagnosis was 44.2 (12.0) years and 47.9 (12.8) years, respectively.
Table 1. Characteristics of BRCA1 and BRCA2 Families From the Breast Cancer Family Registry.
| Characteristic | No. (%)a | ||||
|---|---|---|---|---|---|
| Breast cancer | Ovarian cancer | Death | Unaffected and alive | Total | |
| BRCA1 (498 families) | |||||
| Individuals | 924 (34.9) | 182 (6.9) | 958 (36.2) | 586 (22.1) | 2650 |
| Probands | 391 (78.5) | 43 (8.6) | 5 (1.0) | 59 (11.9) | 498 |
| Proband’s race/ethnicity | |||||
| White | 339 (86.7) | 40 (93.0) | 2 (40) | 56 (94.9) | 437 |
| Black | 23 (5.9) | 0 | 1 (20) | 1 (1.7) | 25 |
| Other | 10 (2.6) | 2 (4.7) | 2 (40) | 2 (3.4) | 16 |
| Unknown | 19 (4.9) | 1 (2.3) | 0 | 0 | 20 |
| Event age, mean (SD) [range], y | 44.2 (12.0) [21.0-86.0] | 53.0 (11.5) [28.0-89.0] | 70.5 (17.9) [18.5-102.5] | 50.9 (16.2) [18.1-95.0] | 55.8 (19.1) [18.1-102.5] |
| BRCA1 variant status | |||||
| Noncarrier | 29 (3.1) | 4 (2.2) | 14 (1.5) | 229 (39.1) | 276 (10.4) |
| Carrier | 483 (52.3) | 55 (30.2) | 16 (1.7) | 192 (32.8) | 746 (28.2) |
| Untested | 412 (44.6) | 123 (67.6) | 928 (96.9) | 165 (28.2) | 1628 (61.4) |
| No. of mammographic screenings | |||||
| 0 | 722 (78.1) | 158 (86.8) | 944 (98.5) | 257 (43.9) | 2081 (78.5) |
| 1 | 160 (17.3) | 19 (10.4) | 7 (0.7) | 174 (29.7) | 360 (13.6) |
| 2 | 31 (3.4) | 4 (2.2) | 3 (0.3) | 63 (10.8) | 101 (3.8) |
| ≥3 | 11 (1.2) | 1 (0.5) | 4 (0.4) | 92 (15.7) | 108 (4.1) |
| RRSO | |||||
| No. (%) | 28 (3.0) | 0 | 9 (0.9) | 129 (22.0) | 166 (6.3) |
| Age at RRSO, y | |||||
| <40 | 15 (53.6) | 0 | 1 (11.1) | 34 (26.4) | 50 (30.1) |
| 40-44 | 18 (64.3) | 0 | 4 (44.4) | 73 (56.6) | 95 (57.2) |
| 45-49 | 24 (85.7) | 0 | 5 (55.6) | 97 (75.2) | 126 (75.9) |
| Age, mean (SD), y | 41.1 (9.0) | NA | 53.4 (14.1) | 44.6 (8.6) | 44.5 (9.3) |
| Gap time to BC, mean (SD), y | 11.3 (8.4) | NA | NA | NA | NA |
| RRM | |||||
| No. (%) | 0 | 1 (0.5) | 3 (0.3) | 60 (10.2) | 64 (2.4) |
| Age at RRM, mean (SD), y | NA | 23.5 (NA) | 49.8 (3.1) | 41.6 (8.7) | 41.7 (8.9) |
| BRCA2 (378 families) | |||||
| Individuals | 715 (37.1) | 62 (3.2) | 698 (36.3) | 450 (23.4) | 1925 |
| Probands | 308 (81.5) | 15 (4.0) | 3 (0.8) | 52 (13.8) | 378 |
| Proband’s race/ethnicity | |||||
| White | 238 (77.3) | 13 (86.7) | 1 (33.3) | 47 (90.4) | 299 |
| Black | 30 (9.7) | 2 (13.3) | 0 | 0 | 32 |
| Other | 26 (8.4) | 0 | 2 (66.7) | 4 (7.7) | 32 |
| Unknown | 14 (4.6) | 0 | 0 | 1 (1.9) | 15 |
| Event age, mean (SD) [range], y | 47.9 (12.8) [21.8-94.0] | 54.3 (11.3) [30.0-80.0] | 69.9 (18.2) [16.5-109.5] | 51.8 (16.3) [19.7-97.0] | 57.0 (18.6) [16.5-109.5] |
| BRCA2 variant status | |||||
| Noncarrier | 31 (4.3) | 3 (4.8) | 17 (2.4) | 196 (43.6) | 247 (12.8) |
| Carrier | 373 (52.2) | 18 (29.0) | 10 (1.4) | 175 (38.9) | 576 (29.9) |
| Untested | 311 (43.5) | 41 (66.1) | 671 (96.1) | 79 (17.6) | 1102 (57.2) |
| No. of mammographic screenings | |||||
| 0 | 566 (79.2) | 58 (93.5) | 685 (98.1) | 170 (37.8) | 1479 (76.8) |
| 1 | 108 (15.1) | 4 (6.5) | 7 (1.0) | 146 (32.4) | 265 (13.8) |
| 2 | 25 (3.5) | 0 | 4 (0.6) | 46 (10.2) | 75 (3.9) |
| ≥3 | 16 (2.2) | 0 | 2 (0.3) | 88 (19.6) | 106 (5.5) |
| RRSO | |||||
| No. (%) | 8 (3.9) | 0 | 9 (1.3) | 107 (23.8) | 144 (7.5) |
| Age at RRSO, y | |||||
| <40 | 6 (21.4) | 0 | 3 (33.3) | 25 (23.4) | 34 (23.6) |
| 40-44 | 14 (50.0) | 0 | 3 (33.3) | 42 (39.3) | 59 (41.0) |
| 45-49 | 17 (60.7) | 0 | 5 (55.6) | 70 (65.4) | 92 (63.9) |
| Age, mean (SD), y | 47.0 (10.0) | NA | 47.4 (17.3) | 46.9 (9.0) | 46.9 (9.8) |
| Gap time to BC, mean (SD), y | 10.7 (7.0) | NA | NA | NA | NA |
| RRM | |||||
| No. (%) | 0 | 0 | 0 | 32 (7.1) | 32 (1.7) |
| Age at RRM, mean (SD), y | NA | NA | NA | 46.3 (9.2) | 46.3 (9.2) |
Abbreviations: BC, breast cancer; NA, not available; OC, ovarian cancer; RRM, risk-reducing mastectomy; RRSO, risk-reducing salpingo-oophorectomy.
Values are expressed as No. (%) unless otherwise indicated.
Time-Varying Association of RRSO With BC in Women With BRCA1 or BRCA2 Pathogenic Variants
Based on the Akaike Information Criterion, the time-dependent association we retained for RRSO was exponential decay for BRCA1 families and BRCA2 families, but for women with BRCA1 pathogenic variants, the association of RRSO with BC risk diminished over time until reaching a threshold, ie, an HR of 0.64 (95% CI, 0.38-0.97). For BRCA2 families, there was no threshold, and the HR reached unity approximately 5 to 6 years after RRSO. The time-dependent association of RRSO with BC was averaged within 2 time intervals (≤5 years and >5 years after RRSO was introduced) (Table 2) and also estimated on a continuous scale from 1 to 10 years after surgery (Figure 1 and eTables 1 and 2 in the Supplement). The overall association of RRSO with BC risk was statistically significant in women with BRCA1 or BRCA2 pathogenic variants: in BRCA1 pathogenic variant carriers, the association of RRSO with BC diminished over time (HR, 0.28 [95% CI, 0.10-0.63] for ≤5 years vs 0.64 [95% CI, 0.38-0.97] for >5 years; P = .002). The same trend was observed in BRCA2 carriers (HR, 0.19 [95% CI, 0.06-0.71] for ≤5 years vs 0.99 [95% CI, 0.84-1.00] for >5 years; P = .002). We noted that the permanent exposure assumption, which assumes a constant association of RRSO with BC after surgery, did not fit as well as a model with an exponential decay pattern based on the Akaike Information Criterion. Under this former assumption, the association with RRSO was not statistically significant for women with either BRCA1 or BRCA2 pathogenic variants (eTables 1 and 2 in the Supplement), similar to what has been reported previously.7,8,9,10,11
Table 2. Hazard Ratios and 95% CIs Measuring the Time-Dependent Outcome of RRSO on Breast Cancer Risks Based on Different Time-Varying Covariate Models in BRCA1 and BRCA2 Families From the Breast Cancer Family Registry.
| Time-dependent outcome for RRSO | HR (95% CI) | |||||
|---|---|---|---|---|---|---|
| BRCA1 families | BRCA2 families | |||||
| Exponential decay with threshold | Exponential decay | Permanent exposure | Exponential decay with threshold | Exponential decay | Permanent exposure | |
| Time since RRSO, y | ||||||
| ≤5 | 0.28 (0.1-0.63)a | 0.31 (0.08-0.99) | 0.57 (0.38-0.84) | 0.19 (0.07-0.45) | 0.19 (0.06-0.71)a | 0.62 (0.41-0.96) |
| >5b | 0.64 (0.38-0.97)a | 0.99 (0.87-1.00) | 0.57 (0.38-0.84) | 0.76 (0.47-1.21) | 0.99 (0.84-1.00)a | 0.62 (0.41-0.96) |
| LRTc | 15.23a | 11.12 | 9.04 | 13.77 | 12.86a | 5.65 |
| P value | .002a | .004 | .003 | .003 | .002a | .02 |
Abbreviations: HR, hazard ratio; LRT, likelihood ratio test; RRSO, risk-reducing salpingo-oophorectomy; TVC, time-varying covariate.
Indicates the best TVC.
Maximum follow-up time is 15 years.
LRT indicates the likelihood ratio test statistics comparing to the null model with no RRSO effect.
Figure 1. Hazard Ratios and 95% CIs Measuring the Time-Dependent Outcome of Risk-Reducing Salpingo-Oophorectomy (RRSO) on Breast Cancer Risks by Years After RRSO Uptake.
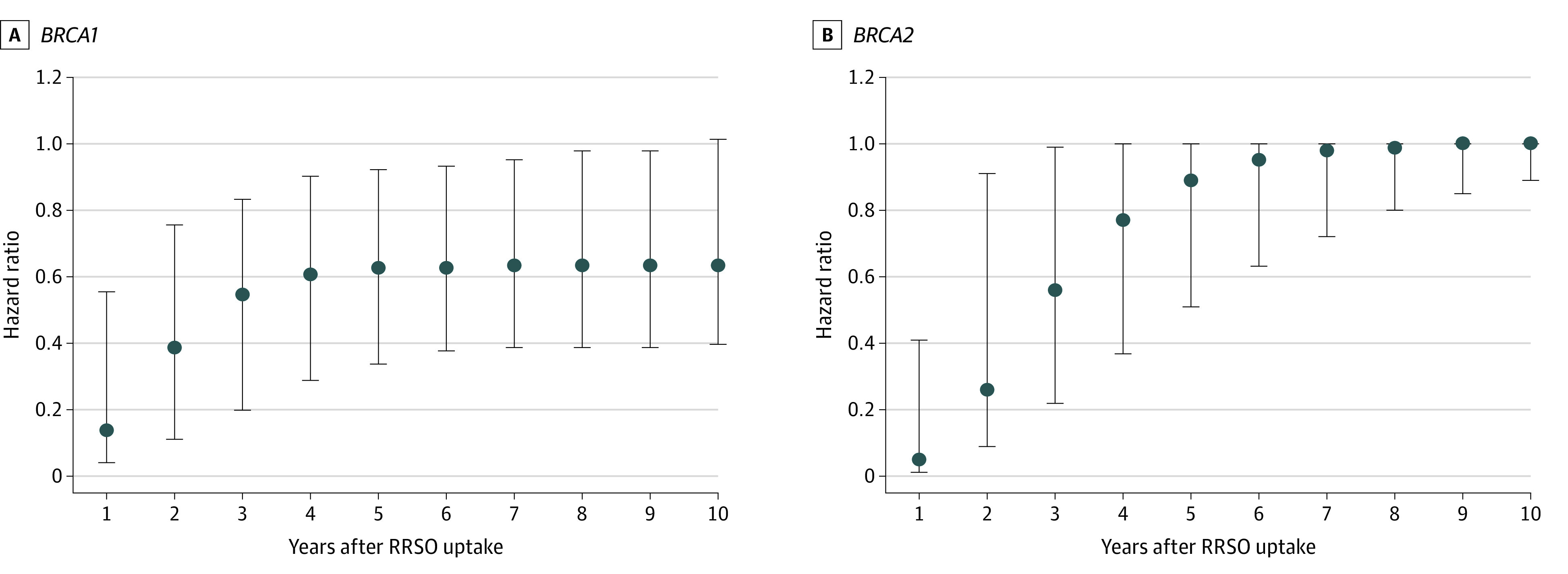
Hazard ratios and 95% CIs for (A) BRCA1 and (B) BRCA2.
Cumulative Risk of BC Among Women With BRCA1 or BRCA2 Pathogenic Variants With Respect to RRSO Status and Age at RRSO Uptake
Within BRCA1 pathogenic variant carrier families, the cumulative risk (also known as penetrance) of BC for women without an RRSO was 61.0% (95% CI, 56.7%-66.0%) by age 70 years for women with a BRCA1 pathogenic variant and 12.1% (95% CI, 10.3%-14.3%) for women who did not carry a pathogenic variant (Table 3). For a woman with a BRCA1 pathogenic variant having RRSO at age 30 years, BC penetrance was 48.2% (95% CI, 36.1%-60.5%), whereas it was 49.7% (95% CI, 40.0%-60.3%) and 52.8% (95% CI, 46.2%-60.7%) for RRSO uptake at 40 and 50 years, respectively. Within BRCA2 families, the penetrance of BC by age 70 years was 54.0% (95% CI, 49.3%-60.1%) and 10.3% (95% CI, 8.4%-12.5%), respectively, for women without RRSO but with and without carriage of a BRCA2 pathogenic variant. For a woman with a BRCA2 pathogenic variant having RRSO at age 30 years, this penetrance was 53.5% (95% CI, 48.6%-59.5%) and reached 52.7% (95% CI, 47.9%-58.7%) and 51.7% (95% CI, 46.8%-57.9%) for RRSO uptake at 40 and 50 years, respectively (Figure 2 and Table 3). Therefore, the age at RRSO did not appear to be associated with BC cumulative risk among BRCA2 pathogenic variant carriers.
Table 3. Penetrance Estimates in BRCA1 and BRCA2 Families From the Breast Cancer Family Registry.
| Breast cancera | % (95% CI) | |||
|---|---|---|---|---|
| BRCA1 families | BRCA2 families | |||
| Age 50 y | Age 70 y | Age 50 y | Age 70 y | |
| No RRSO | ||||
| Carriers | 33.3 (30.4-37.3) | 61.0 (56.7-66.0) | 23.4 (20.7-27.0) | 54.0 (49.3-60.1) |
| Noncarriers | 4.5 (3.7-5.5) | 12.1 (10.3-14.3) | 3.5 (2.7-4.4) | 10.3 (8.4-12.5) |
| Carriers | ||||
| RRSO at 30 y | 23.7 (16.9-32.2) | 48.2 (36.1-60.5) | 22.2 (19.4-25.6) | 53.5 (48.6-59.5) |
| RRSO at 35 y | 24.6 (19.0-31.6) | 48.8 (37.6-60.2) | 21.4 (18.3-24.8) | 53.1 (48.2-59.0) |
| RRSO at 40 y | 26.6 (21.9-31.8) | 49.7 (40.0-60.3) | 20.4 (17.3-24.3) | 52.7 (47.9-58.7) |
| RRSO at 50 y | NA | 52.8 (46.2-60.7) | NA | 51.7 (46.8-57.9) |
Abbreviations: NA, not available; RRSO, risk-reducing salpingo-oophorectomy.
Corresponds to a first breast cancer.
Figure 2. Penetrance of a First Breast Cancer Among Pathogenic Variant Carriers.
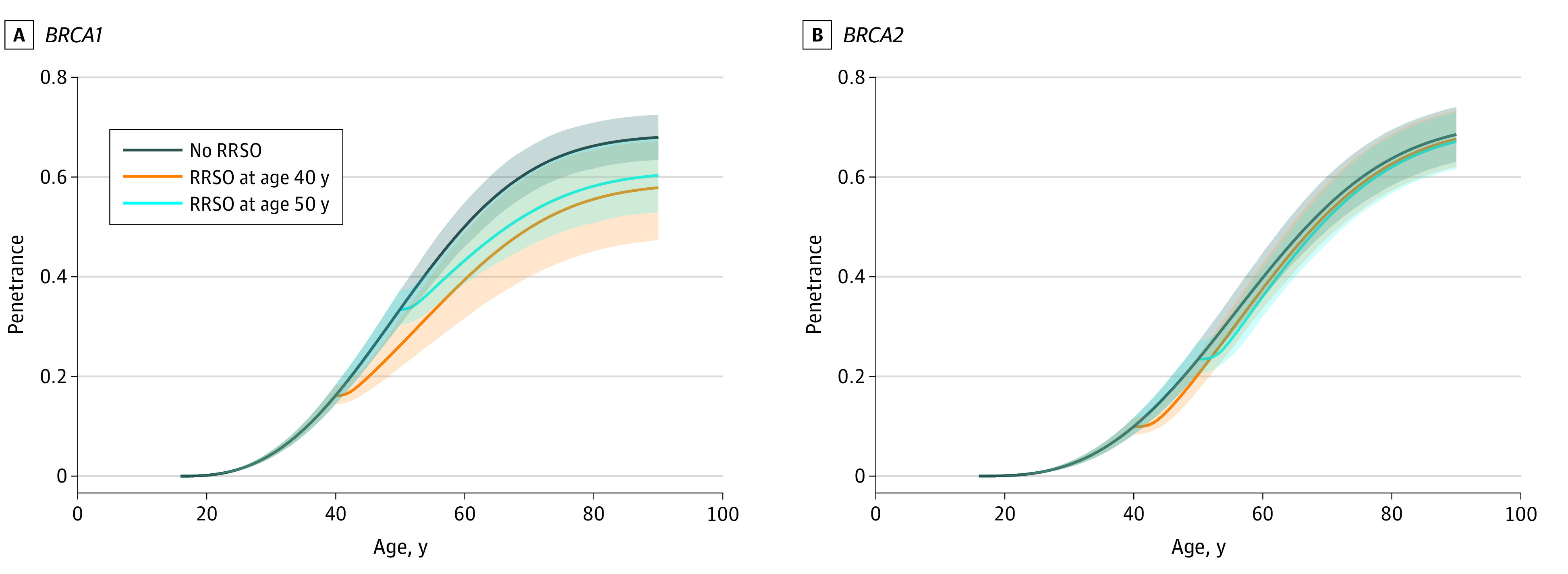
Breast cancer risk for pathogenic variants (A) BRCA1 and (B) BRCA2. RRSO indicates risk-reducing salpingo-oophorectomy. Shaded areas represent 95% CIs.
Discussion
The evaluation of RRSO uptake and its timing in association with BC risk is critical for the clinical management of women carrying pathogenic variants in BRCA1 and BRCA2 genes. Our study brings new insights by investigating BC risk after RRSO in a large series of BRCA1 and BRCA2 pathogenic variant carrier families from the BCFR and by additionally assessing the time-varying association of RRSO with BC through specifically examining the permanent exposure hypothesis. We have therefore added to previous work10 supporting the idea that the nature of the time-varying association of RRSO with BC could alter conclusions about this association.7,8,9,10,11
To our knowledge, all the previous studies that considered RRSO as a time-varying covariate assumed its association to be constant throughout life after surgery.7,8,9,10,11 This assumption is likely too restrictive, particularly for the association with RRSO, which may wane over time and particularly long after menopause. Our analyses brought new insights by suggesting that this association decays exponentially over time after surgery. This finding influences our final results, because we found an overall risk-reducing association of RRSO with BC risk for women with BRCA1 or BRCA2 pathogenic variants.
Although previous studies9,10,11 did not find an association with RRSO in BRCA2 carriers, probably because of a lack of statistical power, the estimates were of similar magnitude.11 Our results differ from those of previous studies mostly in terms of the results among BRCA1 carriers. Terry et al10 reported an HR of 1.33, but their study included a cohort of women enriched for familial risk but highly unlikely to carry BRCA1 or BRCA2 pathogenic variants. Mavaddat et al11 yielded a combined risk estimate (ie, over all the studies) HR of 1.12 for RRSO association more than 5 years after surgery. This latter study noticed substantial risk heterogeneity across studies, but their estimate in the BCFR (HR = 0.77) for the association at more than 5 years after surgery was close to our own result. It is also noteworthy that among the 6 main studies they included,11 the largest gap time between the age at RRSO and BC corresponded to findings of the BCFR, ie, 8.7 years among women carrying BRCA1 pathogenic variants (eTable 3 in the Supplement).11
The discrepancies regarding RRSO’s associations in BRCA1 carriers could be partly explained by the fact that RRSO occurs often after the age at which BC incidence peaks in these women (mean of 44.5 years vs 44.2 years in BCFR). This possibility means that many women with BRCA1 pathogenic variants may have undergone RRSO too late for it to have an influence on the carcinogenic process and disease incidence,11 or that the gap time between the age at RRSO and the age at which BC is usually detected is short. In this context, a model that assumes constant risk changes after surgery (the permanent exposure assumption) might not capture well the potential benefits of this intervention compared with an exponential decay model, which induces stronger BC risk reduction immediately after surgery.
It is also noteworthy that BC risk reduction after RRSO spreads over a longer time period for BRCA1 pathogenic variant carriers (albeit inducing a smaller association) compared with BRCA2 pathogenic variant carriers. The exponential decay assumption with a threshold used for BRCA1 carriers assumes that RRSO-related HR decays over time but then plateaus about 5 years after RRSO without ever reaching unity. Instead, the exponential decay assumption (without threshold) used for BRCA2 pathogenic variant carriers assumes that the RRSO-related risk-reducing association decays gradually until reaching unity about 5 to 6 years after RRSO. This differential effect of RRSO could reflect the different natural histories of the 2 types of breast cancers with earlier age at onset in BRCA1 vs BRCA2 tumors,9 consistent with larger cumulative effects in the former group of tumors the earlier an RRSO is performed. This finding is also in line with studies of mice, which suggested the central role of ovarian hormones in BRCA1-associated tumorigenesis.23 The consequence of this differential effect is that RRSO is associated with a larger reduction in BC cumulative risk (penetrance) for women with BRCA1 vs BRCA2 pathogenic variants, because the influence of the relative risk (HR) is maintained over a longer time period in the former group of women. Although we did find that an earlier age at RRSO was associated with lower BC reduction, the changes based on age were relatively modest (Table 3). The determination of the best timing of RRSO uptake for women with BRCA1 pathogenic variants should consider the reported age-specific incidences of OC but also could be optimized to account for the time-varying association of RRSO with BC risks.
Some studies also reported reduced mortality from BC for women with BRCA1 or BRCA2 pathogenic variants undertaking RRSO,24,25,26 and there is evidence that BCs diagnosed after RRSO are more indolent compared with those arising without this intervention.27 Risk-reducing salpingo-oophorectomy is also associated with a reduction in the risk of contralateral BC.28 A recent meta-analysis29 concluded that BC mortality may decrease for women with RRSO vs no RRSO, but only for those with BRCA1 pathogenic variants and not those with BRCA2 pathogenic variants. However, the meta-analysis showed improved overall survival for women with BRCA1 or BRCA2 pathogenic variants.
Limitations
There are some methodologic limitations that warrant discussion. First, we assumed RRM was a random censoring event for BC, but another option could have been to treat it as another competing risk event for BC. For our sensitivity analyses, we (1) excluded women who underwent RRM and (2) used RRM as a competing risk instead of OC. In both situations, the HR for an RRSO association over time did not change much, but BC penetrance was reduced in the second scenario. We also did not consider hormone replacement therapy after RRSO in our analyses. In BRCA1 and BRCA2 pathogenic variant carriers, hormone replacement therapy is more commonly used in women who undergo RRSO vs those who do not10 and is more generally associated with increased BC risk in the general population. Hormone replacement therapy is therefore more likely to attenuate the risk reduction associated with RRSO than exaggerate its association with BC. We assumed a very general residual familial correlation in our models. A more specific polygenic risk score based on genotype data30 could have been used. Finally, the proportion of family members who undertook RRSO was 6.3% in BRCA1 families and 7.5% in BRCA2 families. Large cohorts of BRCA1 or BRCA2 pathogenic variant carriers are warranted to better assess the time-varying association of RRSO on BC.
Conclusions
In summary, our findings may have important clinical implications for the treatment of women with BRCA1 or BRCA2 pathogenic variants. Although the primary indication for RRSO is the prevention of OC, assessing its association with BC risk is critical to guide clinical decision-making and the timing of such a decision. Our results suggest a reduced BC risk associated with RRSO in women carrying BRCA1 and BRCA2 pathogenic variants, but the association with cumulative risk was stronger among women carrying BRCA1 pathogenic variants. Further work is needed to confirm this result in larger cohorts and to assess carefully the optimal timing of RRSO uptake.
eTable 1. Hazard Ratios and 95% CIs Measuring the Time-Dependent Effect of Risk-Reducing Salpingo-Oophorectomy (RRSO) on BC Risks Based on Different TVC Models in BRCA1 and BRCA2 Families From the BCFR
eTable 2. Hazard Ratios and 95% CIs Measuring the Time-Dependent Effect of Risk-Reducing Salpingo-Oophorectomy (RRSO) on BC Risks Based on the Best TVC Model With or Without Competing Risks and Without Adjustment for Mammography Screening (MS) History in BRCA1 and BRCA2 Families From the BCFR
eTable 3. Hazard Ratios and 95% CIs Measuring the Time-Dependent Effect of Risk-Reducing Salpingo-Oophorectomy (RRSO) on BC Risks Based on a Piece-Wise TVC Model With or Without Competing Risks and With or Without Adjustment for Mammography Screening (MS) in BRCA1 and BRCA2 Families From the BCFR
eMethods
References
- 1.Chen S, Parmigiani G. Meta-analysis of BRCA1 and BRCA2 penetrance. J Clin Oncol. 2007;25(11):1329-1333. doi: 10.1200/JCO.2006.09.1066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kuchenbaecker KB, Hopper JL, Barnes DR, et al. ; BRCA1 and BRCA2 Cohort Consortium . Risks of breast, ovarian, and contralateral breast cancer for brca1 and brca2 mutation carriers. JAMA. 2017;317(23):2402-2416. doi: 10.1001/jama.2017.7112 [DOI] [PubMed] [Google Scholar]
- 3.Kauff ND, Domchek SM, Friebel TM, et al. Risk-reducing salpingo-oophorectomy for the prevention of BRCA1- and BRCA2-associated breast and gynecologic cancer: a multicenter, prospective study. J Clin Oncol. 2008;26(8):1331-1337. doi: 10.1200/JCO.2007.13.9626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rebbeck TR, Kauff ND, Domchek SM. Meta-analysis of risk reduction estimates associated with risk-reducing salpingo-oophorectomy in BRCA1 or BRCA2 mutation carriers. J Natl Cancer Inst. 2009;101(2):80-87. doi: 10.1093/jnci/djn442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eisen A, Lubinski J, Klijn J, et al. Breast cancer risk following bilateral oophorectomy in BRCA1 and BRCA2 mutation carriers: an international case-control study. J Clin Oncol. 2005;23(30):7491-7496. doi: 10.1200/JCO.2004.00.7138 [DOI] [PubMed] [Google Scholar]
- 6.Domchek SM, Friebel TM, Singer CF, et al. Association of risk-reducing surgery in BRCA1 or BRCA2 mutation carriers with cancer risk and mortality. JAMA. 2010;304(9):967-975. doi: 10.1001/jama.2010.1237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Heemskerk-Gerritsen BA, Seynaeve C, van Asperen CJ, et al. ; Hereditary Breast and Ovarian Cancer Research Group Netherlands . Breast cancer risk after salpingo-oophorectomy in healthy BRCA1/2 mutation carriers: revisiting the evidence for risk reduction. J Natl Cancer Inst. 2015;107(5):djv033. doi: 10.1093/jnci/djv033 [DOI] [PubMed] [Google Scholar]
- 8.Heemskerk-Gerritsen BA, Hooning MJ, Rookus MA; all authors . Response. J Natl Cancer Inst. 2015;107(9):djv218. doi: 10.1093/jnci/djv218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kotsopoulos J, Huzarski T, Gronwald J, et al. ; Hereditary Breast Cancer Clinical Study Group . Bilateral oophorectomy and breast cancer risk in BRCA1 and BRCA2 mutation carriers. J Natl Cancer Inst. 2016;109(1). doi: 10.1093/jnci/djw177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Terry MB, Daly MB, Phillips KA, et al. Risk-reducing oophorectomy and breast cancer risk across the spectrum of familial risk. J Natl Cancer Inst. 2019;111(3):331-334. doi: 10.1093/jnci/djy182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mavaddat N, Antoniou AC, Mooij TM, et al. Risk-reducing salpingo-oophorectomy, natural menopause, and breast cancer risk: an international prospective cohort of BRCA1 and BRCA2 mutation carriers. Breast Cancer Res. 2020;22(1):8. doi: 10.1186/s13058-020-1247-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stjepanovic N, Villacampa G, Nead KT, et al. Association of premenopausal risk-reducing salpingo-oophorectomy with breast cancer risk in BRCA1/2 mutation carriers: maximising bias-reduction. Eur J Cancer. 2020;132:53-60. doi: 10.1016/j.ejca.2020.03.009 [DOI] [PubMed] [Google Scholar]
- 13.Paluch-Shimon S, Cardoso F, Sessa C, et al. ; ESMO Guidelines Committee . Prevention and screening in BRCA mutation carriers and other breast/ovarian hereditary cancer syndromes: ESMO Clinical Practice Guidelines for cancer prevention and screening. Ann Oncol. 2016;27(suppl 5):v103-v110. doi: 10.1093/annonc/mdw327 [DOI] [PubMed] [Google Scholar]
- 14.Finch A, Evans G, Narod SA. BRCA carriers, prophylactic salpingo-oophorectomy and menopause: clinical management considerations and recommendations. Womens Health (Lond). 2012;8(5):543-555. doi: 10.2217/WHE.12.41 [DOI] [PubMed] [Google Scholar]
- 15.John EM, Hopper JL, Beck JC, et al. ; Breast Cancer Family Registry . The Breast Cancer Family Registry: an infrastructure for cooperative multinational, interdisciplinary and translational studies of the genetic epidemiology of breast cancer. Breast Cancer Res. 2004;6(4):R375-R389. doi: 10.1186/bcr801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Terry MB, Phillips KA, Daly MB, et al. Cohort profile: the Breast Cancer Prospective Family Study Cohort (ProF-SC). Int J Epidemiol. 2016;45(3):683-692. doi: 10.1093/ije/dyv118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Neuhausen SL, Ozcelik H, Southey MC, et al. ; Breast Cancer Family Registry . BRCA1 and BRCA2 mutation carriers in the Breast Cancer Family Registry: an open resource for collaborative research. Breast Cancer Res Treat. 2009;116(2):379-386. doi: 10.1007/s10549-008-0153-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Choi YH, Jung H, Buys S, et al. A competing risks model with binary time varying covariates for estimation of breast cancer risks in BRCA1 families. Accessed November 10, 2020. https://arxiv.org/abs/2002.05249 [DOI] [PMC free article] [PubMed]
- 19.Prentice RL, Kalbfleisch JD, Peterson AV Jr, Flournoy N, Farewell VT, Breslow NE. The analysis of failure times in the presence of competing risks. Biometrics. 1978;34(4):541-554. doi: 10.2307/2530374 [DOI] [PubMed] [Google Scholar]
- 20.Keown-Stoneman CDG, Horrocks J, Darlington G. Exponential decay for binary time-varying covariates in Cox models. Stat Med. 2018;37(5):776-788. doi: 10.1002/sim.7539 [DOI] [PubMed] [Google Scholar]
- 21.Cox DR, Oakes D. Analysis of Survival Data . Chapman & Hall; 1984. [Google Scholar]
- 22.Gorfine M, Hsu L. Frailty-based competing risks model for multivariate survival data. Biometrics. 2011;67(2):415-426. doi: 10.1111/j.1541-0420.2010.01470.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nolan E, Vaillant F, Visvader JE, Lindeman GJRE. RE: bilateral oophorectomy and breast cancer risk in BRCA1 and BRCA2 mutation carriers. J Natl Cancer Inst. 2017;109(10). doi: 10.1093/jnci/djx038 [DOI] [PubMed] [Google Scholar]
- 24.Domchek SM, Friebel TM, Neuhausen SL, et al. Mortality after bilateral salpingo-oophorectomy in BRCA1 and BRCA2 mutation carriers: a prospective cohort study. Lancet Oncol. 2006;7(3):223-229. doi: 10.1016/S1470-2045(06)70585-X [DOI] [PubMed] [Google Scholar]
- 25.Metcalfe K, Lynch HT, Foulkes WD, et al. Effect of oophorectomy on survival after breast cancer in BRCA1 and BRCA2 mutation carriers. JAMA Oncol. 2015;1(3):306-313. doi: 10.1001/jamaoncol.2015.0658 [DOI] [PubMed] [Google Scholar]
- 26.Huzarski T, Byrski T, Gronwald J, et al. ; Polish Breast Cancer Consortium . The impact of oophorectomy on survival after breast cancer in BRCA1-positive breast cancer patients. Breast Cancer Res Treat. 2016;156(2):371-378. doi: 10.1007/s10549-016-3749-4 [DOI] [PubMed] [Google Scholar]
- 27.van Verschuer VM, Heemskerk-Gerritsen BA, van Deurzen CH, et al. Lower mitotic activity in BRCA1/2-associated primary breast cancers occurring after risk-reducing salpingo-oophorectomy. Cancer Biol Ther. 2014;15(4):371-379. doi: 10.4161/cbt.27628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Metcalfe K, Gershman S, Lynch HT, et al. Predictors of contralateral breast cancer in BRCA1 and BRCA2 mutation carriers. Br J Cancer. 2011;104(9):1384-1392. doi: 10.1038/bjc.2011.120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eleje GU, Eke AC, Ezebialu IU, Ikechebelu JI, Ugwu EO, Okonkwo OO. Risk-reducing bilateral salpingo-oophorectomy in women with BRCA1 or BRCA2 mutations. Cochrane Database Syst Rev. 2018;8:CD012464. doi: 10.1002/14651858.CD012464.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kuchenbaecker KB, McGuffog L, Barrowdale D, et al. Evaluation of polygenic risk scores for breast and ovarian cancer risk prediction in BRCA1 and BRCA2 mutation carriers. J Natl Cancer Inst. 2017;109(7):djw302. doi: 10.1093/jnci/djw302 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Hazard Ratios and 95% CIs Measuring the Time-Dependent Effect of Risk-Reducing Salpingo-Oophorectomy (RRSO) on BC Risks Based on Different TVC Models in BRCA1 and BRCA2 Families From the BCFR
eTable 2. Hazard Ratios and 95% CIs Measuring the Time-Dependent Effect of Risk-Reducing Salpingo-Oophorectomy (RRSO) on BC Risks Based on the Best TVC Model With or Without Competing Risks and Without Adjustment for Mammography Screening (MS) History in BRCA1 and BRCA2 Families From the BCFR
eTable 3. Hazard Ratios and 95% CIs Measuring the Time-Dependent Effect of Risk-Reducing Salpingo-Oophorectomy (RRSO) on BC Risks Based on a Piece-Wise TVC Model With or Without Competing Risks and With or Without Adjustment for Mammography Screening (MS) in BRCA1 and BRCA2 Families From the BCFR
eMethods


