Abstract
Background
The COVID-19 has had an enormous impact worldwide and is still spreading. Globally confirmed infections have surpassed 41.1 million, of which more than 1 million resulted in deaths. Considering the relationship between public health disasters and emotional disorders, it is essential to examine psychological well-being related to this pandemic.
Method
We performed a systematic search on psychological problems from PubMed to 10 October 2020, and conducted a meta-analysis using Comprehensive Meta-Analysis V.3 software.
Results
The results showed a 19.4% and 26.8% pooled incidence for depression and post-traumatic stress disorder (PTSD), respectively, during the SARS and Middle East Respiratory Syndrome (MERS)-related coronavirus outbreaks. However, overall prevalence of depression was somewhat higher at 27.0% during the COVID-19 period. The pooled incidence of PTSD during COVID-19 compared with SARS and MERS outbreaks, was lower, at 16.4%.
Conclusion
The results suggest that there are shared and distinct psychological responses following SARS, MERS and COVID-19, and show pessimistic estimates of a wide range of potentially upcoming psychological problems.
Keywords: communicable diseases, epidemics, meta analysis
Introduction
The outbreak of COVID-19 is posing a public health disaster. As of 22 October 2020, the number of confirmed infections internationally has exceeded 41.1 million, including more than 1.1 million mortalities.1 Research has shown public health disasters can cause an onset of emotional disorders.2 Hence, it is essential to pay attention to psychological well-being during the COVID-19 pandemic.
The three coronavirus outbreaks since the start of the 21st century are: SARS, Middle East respiratory syndrome (MERS) and COVID-19. Considering research related to SARS, several studies have shown people who were infected with the virus were more likely to have experienced negative emotions despite physical rehabilitation.3 4 Furthermore, people who were quarantined at home during the SARS and MERS epidemic were also more prone to have suffered from mental illness.5–7 Several studies indicated negative mental health states, such as post-traumatic stress disorder (PTSD), among patients with SARS, healthcare workers (HCW) and the general public.8–10 With regard to COVID-19, various studies have examined the psychological effects thereof and found evidence of severe distress.11–14 Thus, it has been established that all three of the outbreaks are linked to emotional distress.
A review of the latest literature, having removed repeated studies and research involving complications, followed by a meta-analysis to derive at pooled prevalence, was needed. By comparing the prevalence of psychological illness thus far during COVID-19 with previous coronavirus outbreaks, such as SARS and MERS, we expect to provide a warning related to mental health issues. Therefore, we conducted this meta-analysis to evaluate the updated psychological prevalence of COVID-19 and historical coronavirus-related data. Specifically, we compared the pooled incidence between COVID-19 and SARS and MERS, and analysed the incidence among HCW, the general public and patients. Furthermore, we analysed the current severity of mental problems, compared historical data to explore possible deterioration trends, and ultimately, give early warnings related to mental health.
Methods
Search strategy
We systematically searched the literature in the PubMed and Web of Science databases until 10 October 2020. Our search terms were ‘(severe acute respiratory syndrome or Middle East respiratory syndrome) and (psychological or psychiatry or mental or anxiety or depression)’ for SARS and MERS, ‘coronavirus disease 2019 and (psychological or psychiatry or mental or anxiety or depression)’ for COVID-19.
Inclusion criteria
To be eligible for inclusion, the studies had to fulfil the following criteria: (1) published in peer-reviewed journals; (2) written in English; (3) reported mental health status of the population affected by SARS, MERS or COVID-19 and (4) data were quantitatively analysed as a percentage.
Exclusion criteria
The studies were excluded if: (1) the study population consisted of individuals already suffering from a psychiatric or mental health disorder before the disease outbreak or having other complications; (2) it failed the review by the local ethics committee; (3) it was not published in English and (4) it was grey or unpublished studies.
Screening of articles
We searched for related articles using keywords and filtering titles. Articles were downloaded and the abstracts screened using inclusion criteria, deleting any irrelevant or repetitive articles. Thereafter, we manually searched the reference lists of the chosen papers for any other relevant studies not found in our initial search. Finally, a full-text search was performed to extract and then analyse the data from articles. The information we extracted included aspects such as: name of the author, publication year, country, population (HCW, the general public or patients), instruments used, psychological or mental health problems, psychological or mental health disorder rate and check time (time between the end of epidemic and investigation).
Statistical analysis
The meta-analyses implemented in this study conforms to guidelines from the Preferred Reporting Items for Systematic Reviews and Meta-analyses statement.15 Statistical analysis was done using Comprehensive Meta-Analysis V.3 software. Between-study heterogeneity was assessed by I2 statistic,16 which was used to evaluate the impact of heterogeneity, highlighting inconsistencies across studies. In this regard, I2 results of 0.25, 0.5 and 0.75 indicated small, moderate and high levels of between-study heterogeneity, respectively. When significant heterogeneity was detected, the random-effect model with the restricted likelihood method was applied for meta-analysis. Otherwise, the fixed-effect model was used. Furthermore, p<0.05 was considered statistically significant in the meta-analysis except where noted differently.
Results
Search results
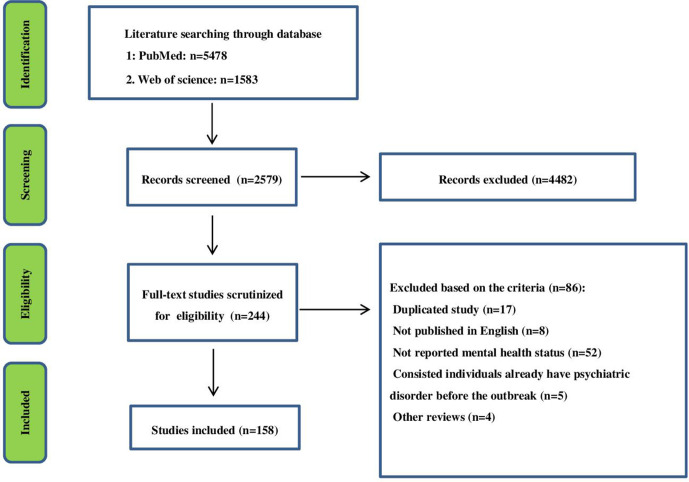
The original search identified 7061 references from the database (SARS and MERS: n=1649; COVID-19: n=5412), and after title filtering, 244 articles (SARS and MERS: n=53; COVID-19: n=191) met the requirements. Following a full-text screening, 158 (SARS and MERS: n=28; COVID-19: n=130) of these contained specific data (figure 1) and were summarised in a table (online supplemental table 1).
Figure 1.
Flow chart of the literature search.
jech-2020-215927supp001.pdf (216.1KB, pdf)
The 28 studies included 11 661 participants from 6 countries around the world during SARS and MERS, and 748 616 participants from 30 countries during COVID-19. Moreover, of these 158 studies, 25 were conducted among HCW (SARS and MERS: n=5; COVID-19: n=20), 113 among the general public (SARS and MERS: n=6; COVID-19: n=107) and 20 among patients (SARS and MERS: n=7; COVID-19: n=13). A methodological quality assessment of the risks of bias for each study has been analysed. ‘Risk-of-bias’ domain ratings are shown per study in online supplemental figures 1 and 2. The overall risk of bias for most studies was either unclear or low.
jech-2020-215927supp002.pdf (12.7KB, pdf)
jech-2020-215927supp003.pdf (7.3MB, pdf)
Depression
Eight of the 84 articles mentioned incidence of depression during SARS and MERS (table 1, figure 2). The heterogeneity of the studies was evaluated using the I2 test; I2=96.911% was obtained, indicating a high heterogeneity among the included studies. Therefore, the random-effects model was used to combine the results of the studies together. Furthermore, the possibility of publication bias in the studies was assessed using a Funnel plot (online supplemental figure 3). The pooled estimate for depression was 19.4% (95% CI 0.102 to 0.339; p<0.001). Of these eight studies, one was conducted among HCW, three among the general public and four among patients. The overall depression prevalence of HCW, general public and patients, was 27.5%, 16.8% and 20.3%, respectively.
Table 1.
Summary of comparative outcomes for measurements of pooled incidence
| Group | No of studies |
No with participants | Main effect | Heterogeneity | |||||
| Pooled incidence (95% CI) |
Z score | P value | Q statistic | df | P value | I2 statistic | |||
| Psychological illness | |||||||||
| SARS and MERS | |||||||||
| Depression | 8 | 2484 | 0.194 (0.102 to 0.339) | −3.696 | 0.000 | 226.616 | 7 | 0.000 | 96.911 |
| PTSD | 10 | 3340 | 0.268 (0.188 to 0.366) | −4.307 | 0.000 | 207.992 | 9 | 0.000 | 95.673 |
| COVID-19 | |||||||||
| Depression | 108 | 515 452 | 0.270 (0.248 to 0.293) | −17.256 | 0.000 | 27 525.374 | 107 | 0.000 | 99.611 |
| PTSD | 18 | 51 721 | 0.164 (0.108 to 0.240) | −6.680 | 0.000 | 5246.998 | 17 | 0.000 | 99.676 |
| Anxiety | 109 | 127 703 | 0.279 (0.246 to 0.315) | −10.724 | 0.000 | 61 270.178 | 108 | 0.000 | 99.824 |
| Insomnia | 35 | 156 069 | 0.287 (0.238 to 0.341) | −7.094 | 0.000 | 11 906.587 | 34 | 0.000 | 99.714 |
MERS, Middle East respiratory syndrome; PTSD, post-traumatic stress disorder.
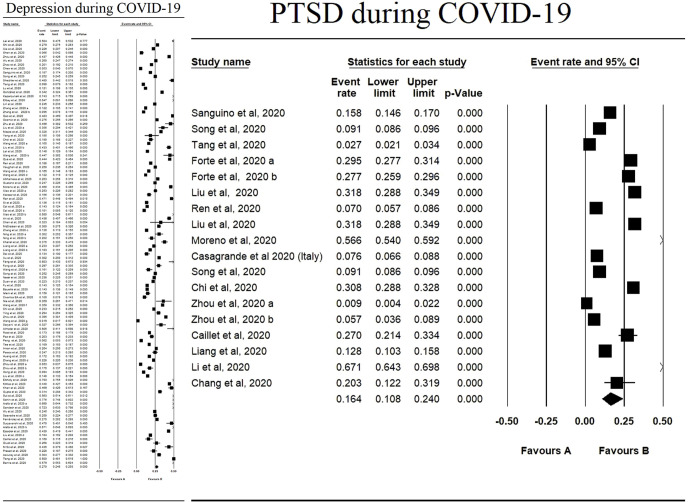
Figure 2.
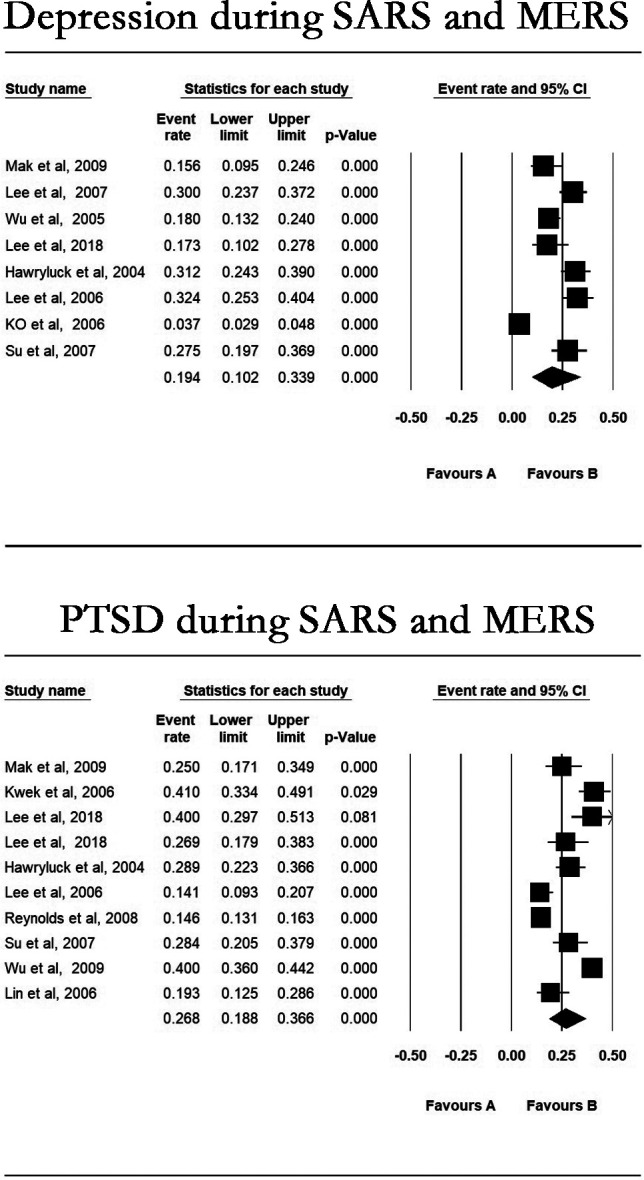
Meta-analysis of the pooled incidence of depression and PTSD during SARS and MERS. MERS, Middle East respiratory syndrome; PTSD, post-traumatic stress disorder.
jech-2020-215927supp004.pdf (67.8KB, pdf)
In terms of COVID-19 studies, 130 articles, 20 conducted among HCW, 107 among general public and 13 among patients, mentioned incidence of depression during the outbreak (figure 3). The overall prevalence of depression was 27.0% (95% CI 0.248 to 0.293; p<0.001, I2=99.611%), and the pooled prevalence of patients, HCW and the general public was 18.6%, 32.3% and 25.8%, respectively (online supplemental figures 4–6).
Figure 3.
Meta-analysis of the pooled incidence of depression and PTSD during COVID-19. PTSD, post-traumatic stress disorder.
jech-2020-215927supp005.pdf (157.6KB, pdf)
jech-2020-215927supp006.pdf (73.3KB, pdf)
jech-2020-215927supp007.pdf (13.1MB, pdf)
Post-traumatic stress disorder
Only 10 of the 28 studies conducted during SARS and MERS, reported incidence of PTSD (figure 2). Of these, four were undertaken among HCW, three among the general public, and three among patients. Following a meta-analysis, we found a pooled PTSD incidence of 26.8% (95% CI 0.188 to 0.366; p<0.001, I2=95.673%). The pooled prevalence was highest in HCW (31.9%) compared with patients (31.2%) and the general public (18.3%).
Of the 130 studies related to COVID-19, 18 mentioned the incidence of PTSD (figure 3). Of these, 3 was conducted among HCW, 14 among the general public and 1 among patients. A meta-analysis revealed a pooled PTSD incidence of 16.4% (95% CI 0.108 to 0.240; p<0.001, I2=99.676%), considerably lower than that reported during SARS and MERS. Interestingly, prevalence rates for HCW (19.0%), patients (20.3%) and the general public (15.7%) in particular (table 2, online supplemental figures 7–9).
Table 2.
Depression and PTSD pooled incidence in different population
| Pooled incidence | Patients, % | HCW, % | General public, % |
| SARS and MERS | |||
| Depression | 20.3 | 27.5 | 16.8 |
| PTSD | 31.2 | 31.9 | 18.3 |
| COVID-19 | |||
| Depression | 18.6 | 29.6 | 25.8 |
MERS, Middle East respiratory syndrome; PTSD, post-traumatic stress disorder.
jech-2020-215927supp008.pdf (2.3MB, pdf)
jech-2020-215927supp009.pdf (1.8MB, pdf)
jech-2020-215927supp010.pdf (4.2MB, pdf)
Anxiety and insomnia
Various researchers conducted anxiety and insomnia-related studies during the COVID-19 pandemic. Thirty-five articles mentioned incidence of insomnia during COVID-19 (online supplemental figure 10). Our meta-analysis of the 109 studies related to anxiety showed a pooled incidence of 27.9% (95% CI 0.246 to 0.315; p<0.001) (online supplemental figure 11). We conducted a meta-analysis of these articles and found the pooled incidence being 28.7% (95% CI 0.238 to 0.341; p<0.001).
jech-2020-215927supp011.pdf (533.2KB, pdf)
jech-2020-215927supp012.pdf (196KB, pdf)
Sensitivity analysis
The sensitivity analysis was used by one study removed method. The publication bias was analysed for the main variables using funnel plots. The sensitivity analysis did not show large differences with respect to the main analysis (online supplemental figures 12 and 13).
jech-2020-215927supp013.pdf (203.2KB, pdf)
jech-2020-215927supp014.pdf (112.4KB, pdf)
Main cause
Several reasons could explain the prevalence of mental disorders among patients: having tested positive for a highly infectious disease, uncertainty regarding the treatment outcome, negative media reports, being quarantined for 21 days or more and lonely for lacking the solace of visitors, physical deterioration, concerns about having transmitted the virus to family members unknowingly and a high reported mortality rate.17 Furthermore, increased stigmatisation,18 leads to fear, pessimism, passive defensiveness and indifference.
For HCW, many expressed conflicts between their roles as HCW and patients. On the one hand, they felt altruism and professional responsibility. On the other hand, they experienced fear and guilt about possibly infecting their families.10 The indirect impact of the virus, such as fear of infecting loved ones, being stigmatised by others or losing patients, seems to be paramount. Second to that is the potential personal bodily harm caused by the virus.10 19
It appears that the general public may be more prone to depression possibly due to poor economic conditions and insufficient social support.20 21 Lack of formal education may increase the likelihood of depression during the pandemic. In this regard, one study found that those among the general public who have no formal education were more at risk during the pandemic. In terms of sex, it appears females are more at risk for higher levels of stress, anxiety, and depression. Specifically, being female was significantly associated with higher levels of stress, anxiety and depression.22 Women, who are 30–40 years and have only received primary school education, were more likely to have greater anxiety.23
Discussion
Key findings
In the current meta-analysis, we compared pooled psychological prevalence between SARS, MERS and COVID-19. In addition, we analysed the incidence shift in different populations, being patients, HCW and the general public, for depression and PTSD.
Depression and PTSD were the most serious emotional disorders reported in all the research identified and sufficient studies were available to justify the use of meta-analysis. The pooled incidence of depression is 19.4% and that of PTSD is 26.8% in SARS and MERS, and the respective prevalence was 27.0% and 16.4% in COVID-19. Results show that the overall prevalence of depression during COVID-19 is higher than during SARS and MERS. In contrast, the prevalence of PTSD seems to be much lower during COVID-19 than SARS and MERS, which creates the impression that it may not be as serious this time around. However, it is important to note the onset of PTSD could be immediate, over weeks, months or even years. The global COVID-19 outbreak is not over yet. Considering that the pooled incidence of PTSD after SARS and MERS was much higher than that of depression, it could be predicted that PTSD prevalence is likely to increase following the after the COVID-19 pandemic.
When we divide the results of depression and PTSD during SARS and MERS into three groups according to population, we find that HCW had the worst mental health with the highest pooled incidences in both depression and PTSD. The patients’ group followed with slightly similar PTSD prevalence rates. The incidences of mental illness among the general public are lower than the former two groups, although still higher than 15%.
During COVID-19, only one study in the patients group remained after removing articles with complications, but it does not affect the overall trend. The pooled incidence of depression in HCW and the general public is higher than that of the SARS and MERS period, indicating that the stress level of the population is higher during this COVID-19 period.
Furthermore, the incidence of PTSD in HCW and the general public is lower than that in SARS and MERS, which may be since the pandemic is not over yet. It is worth noting that compared with the SARS and MERS data, it is found that the mental health status of the general public deteriorated significantly during the COVID-19 period. The level of depression in the general public is almost the same as that of HCW, and the level of PTSD is higher than that of HCW. This result may be related to the worldwide policy of long-term home segregation and Given the large number of people impacted by the pandemic, it is a warning of the extensive need for psychological intervention that may arise post-COVID-19.
Other findings
Other mental health indicators widely discussed across the COVID-19 studies were anxiety and insomnia. The respective prevalence of each were 27.9% and 28.7%, showing approximately a quarter of people feeling anxious and insomnia. This could be indicative of considerable social pressure during the epidemic.
Interesting data also emerged around respondent subgroups within the above three main categories. Specifically, senior citizens seem more affected when they suffer this kind of adversity. The incidence of PTSD in the elderly during the SARS epidemic was significantly higher than that of general public.24 At the time, the suicide rate among this group also increased significantly.25 In terms of gender, women appear to be more likely to suffer psychological problems than men. For example, in the patients group, the mental state of women was shown to be worse,26 27 and in the HCW group, their rates of psychiatric morbidity were also higher.28 Interestingly, somewhat different results were reported for pregnant women who, despite being generally considered more vulnerable, managed to have maintained relatively good moods during the outbreak. This may have been due to widespread concern from others during the outbreak.29 Furthermore, students also reported slightly different results. Specifically, those who study medicine felt pressure30 during the epidemic, while international students thought of this period as an inconvenience. However, these results were not significant enough to be considered a mental health disorder.31 Among HCW, two studies reported that nurses in the first-line intensive care unit had better mental states than other nurses.32 33
The general public’s tendency to depression may be due to poor economic conditions, insufficient social support and alienation experience.20 21 Due to the education, sex, age and social status, people have different levels of psychological responses to coronavirus. For patients, there several reasons why they are more likely to suffer from mental disorders, including that they have been confirmed to have highly contagious diseases; uncertainty of treatment outcome; negative media reports; isolation for 21 days or more and lonely for lacking the solace of visitors; physical deterioration; deteriorating physical condition; fear that they may unwittingly transmit the virus to families and high mortality rate.17 For HCW, many people expressed conflict between their roles as HCW and parents. On the one hand, they felt altruism and professional responsibility. On the other hand, they felt fear and guilt about the possible infection of their families.10
What can people do to prevent mental disorder? In terms of the general public, mental health problems can be prevented by providing mental health support to individuals with weak mental health, and providing accurate information and appropriate supplies, including food, clothing and accommodation, 4–6 months after home segregation.5 Specific measures may include assessing the accuracy of the information disclosed, strengthening social security systems, eliminating the spread of stigma associated with the COVID-19 virus, maintaining a normal life, staying safe and making use of psychological services available.34 For HCW, an adaptive response to stress and the positive effects of infection control training may play a protective role in future outbreaks.35 This means receiving proper infection control training and learning ways to cope with stress, is likely to enhance medical staff’s ability to cope with various emergencies, protect their mental health, and provide improved health services to society.36 Additionally, during a pandemic, transparent and timely distribution of related information announcement is likely to lessen resulting psychosocial problems.33 In terms of communication, the internet was the main channel of public health information distribution during the outbreak.22 Additionally, smart phones’ information spreading capability should be optimally used to reduce unnecessary panic among the public.37
Considering the impact of COVID-19 spreading around the globe, marked by city and nationwide lockdowns, we are expecting a mental health crisis in the aftermath of the pandemic. Measures to curb its impact include but are not limited to accurate and timely release of relevant information to reduce the accumulation of anxiety, provision of extensive psychological care to reduce the occurrence of panic emotions, and ultimately, reducing the number of post-COVID-19 depression and PTSD cases.33 38
Fortunately, several tools already exist to lessen the negative impact of outbreaks such as COVID-19. For example, social networks through smartphones, have widespread reach, which is potentially beneficial in the accelerated spread of information to reduce panic in society. Furthermore, compared with SARS which showcased an unprepared, immediate response by role players, this time around various countries had plans put in place leading to a quicker response, while also focusing on the prevention of mental illness.39
Limitations
The following reasons may also cause some differences among the results of the study. For the interpretation of the present results, the following limitations need to be considered. First, different instruments used among studies should be taken into consideration. The Impact of Event Scale-Revised21 40 is the psychometric instrument most used to evaluate PTSD. Some studies used the Chinese versions of the Impact of Event Scale-Revised)24 and the Davidson Trauma Scale32 as PTSD evaluation instruments. Whereas depression is mostly diagnosed by administering the Hospital Anxiety and Depression Scale,8 27 other diagnostic instruments, such as the Center for Epidemiologic Studies-Depression Scale,6 24 Taiwanese Depression Questionnaire20 and Beck depression inventory32 have also been used in research. Despite a difference in instruments, the goal remains the same: to accurately assess the prevalence/existence of a mood disorder. Still, a difference in standards is inevitable, which contributes to the incidence heterogeneity among related diseases.
Second, the scope of the literature may have influenced data heterogeneity both positively and negatively. Specifically, the studies used in this review were limited to those published in English. This measure was intended to capitalise on the relatively small difference between the evaluation criteria of articles using the same language. In addition, it served to limit the heterogeneity between different studies. Unfortunately, this measure also led to the exclusion of studies published in Chinese, essentially withholding information from an important data source as far as SARS and early COVID-19 spread are concerned. This increased the skewness of the data.
Conclusion
We conducted a meta-analysis to compare different pooled incidence rates between SARS, MERS and COVID-19. Results suggest shared and distinct psychological responses following SARS, MERS and COVID-19, and show pessimistic estimates of a wide range of potentially upcoming psychological problems. We call for policy-makers, international health organisations and trained psychologists to work together to enhance preparedness for the ongoing and/or upcoming mental health catastrophe related to COVID-19.
What is already known on this subject.
The number of deaths due to COVID-19 has surpassed 41.1 million, of which more than 1 million resulted in deaths.
Considering the relationship between public health disasters and emotional disorders, it is essential to examine psychological well-being related to this pandemic.
What this study adds.
Meta-analysis links the latest COVID-19 psychological research with mental health trends reported from previous coronavirus outbreaks like SARS and Middle East respiratory syndrome.
Results showed a 19.4% and 26.8% pooled incidence for depression and post-traumatic stress disorder (PTSD), respectively, during the previous coronavirus outbreaks.
Pooled incidence for depression and PTSD is 27.0% and 16.4% during COVID-19.
Meta-analysis includes a separate discussion of three different population (patients, healthcare workers and the general public).
Footnotes
FCF and SYZ contributed equally.
Contributors: FCF and SYZ collected and analysed the data, prepared figures. FCF and SYZ wrote the manuscript. YC designed the research.
Funding: This study was supported by the National Science Foundation of China (81703492), the Beijing Natural Science Foundation (7182092), the Minzu University Research Fund (2018CXTD03) and the MUC 111 project.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article or uploaded as online supplemental information. The data used to support the findings of this study are included within the article.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
References
- 1.WHO . Coronavirus disease (COVID-19) outbreak; 2020.
- 2.Naushad VA, Bierens JJ, Nishan KP, et al. A systematic review of the impact of disaster on the mental health of medical responders. Prehosp Disaster Med 2019;34:632–43. 10.1017/S1049023X19004874 [DOI] [PubMed] [Google Scholar]
- 3.Tsang HWH, Scudds RJ, Chan EYL. Psychosocial impact of SARS. Emerg Infect Dis 2004;10:1326–7. 10.3201/eid1007.040090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maunder RG. Was SARS a mental health catastrophe? Gen Hosp Psychiatry 2009;31:316–7. 10.1016/j.genhosppsych.2009.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jeong H, Yim HW, Song Y-J, et al. Mental health status of people isolated due to middle East respiratory syndrome. Epidemiol Health 2016;38:e2016048. 10.4178/epih.e2016048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hawryluck L, Gold WL, Robinson S, et al. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis 2004;10:1206–12. 10.3201/eid1007.030703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim YG, Moon H, Kim S-Y, et al. Inevitable isolation and the change of stress markers in hemodialysis patients during the 2015 MERS-CoV outbreak in Korea. Sci Rep 2019;9:5676. 10.1038/s41598-019-41964-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kwek S-K, Chew W-M, Ong K-C, et al. Quality of life and psychological status in survivors of severe acute respiratory syndrome at 3 months postdischarge. J Psychosom Res 2006;60:513–9. 10.1016/j.jpsychores.2005.08.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee SH, Shin H-S, Park HY, et al. Depression as a mediator of chronic fatigue and post-traumatic stress symptoms in middle East respiratory syndrome survivors. Psychiatry Investig 2019;16:59–64. 10.30773/pi.2018.10.22.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maunder R, Hunter J, Vincent L, et al. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ 2003;168:1245–51. [PMC free article] [PubMed] [Google Scholar]
- 11.Huang Y, Zhao N. Chinese mental health burden during the COVID-19 pandemic. Asian J Psychiatr 2020;51:102052. 10.1016/j.ajp.2020.102052 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 12.Saurabh K, Ranjan S. Compliance and psychological impact of quarantine in children and adolescents due to Covid-19 pandemic. Indian J Pediatr 2020;87:532–6. 10.1007/s12098-020-03347-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Choi EPH, Hui BPH, Wan EYF. Depression and anxiety in Hong Kong during COVID-19. Int J Environ Res Public Health 2020;17:3740. 10.3390/ijerph17103740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shen Y, Cui Y, Li N, et al. Emergency responses to Covid-19 outbreak: experiences and lessons from a general Hospital in Nanjing, China. Cardiovasc Intervent Radiol 2020;43:810–9. 10.1007/s00270-020-02474-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339:b2535. 10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Qin X-Y, Wu H-T, Cao C, et al. A meta-analysis of peripheral blood nerve growth factor levels in patients with schizophrenia. Mol Psychiatry 2017;22:1306–12. 10.1038/mp.2016.235 [DOI] [PubMed] [Google Scholar]
- 17.Chua SE, Cheung V, McAlonan GM, et al. Stress and psychological impact on SARS patients during the outbreak. Can J Psychiatry 2004;49:385–90. 10.1177/070674370404900607 [DOI] [PubMed] [Google Scholar]
- 18.Mak IWC, Chu CM, Pan PC, et al. Long-Term psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry 2009;31:318–26. 10.1016/j.genhosppsych.2009.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Verma S, et al. Post-SARS psychological morbidity and stigma among general practitioners and traditional Chinese medicine practitioners in Singapore. Ann Acad Med 2004;33:743–8. [PubMed] [Google Scholar]
- 20.Ko C-H, Yen C-F, Yen J-Y, et al. Psychosocial impact among the public of the severe acute respiratory syndrome epidemic in Taiwan. Psychiatry Clin Neurosci 2006;60:397–403. 10.1111/j.1440-1819.2006.01522.x [DOI] [PubMed] [Google Scholar]
- 21.Reynolds DL, Garay JR, Deamond SL, et al. Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiol Infect 2008;136:997–1007. 10.1017/S0950268807009156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu J, Zhu Q, Fan W, et al. Online mental health survey in a medical college in China during the COVID-19 outbreak. Front Psychiatry 2020;11:459. 10.3389/fpsyt.2020.00459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leung GM, Ho L-M, Chan SKK, et al. Longitudinal assessment of community psychobehavioral responses during and after the 2003 outbreak of severe acute respiratory syndrome in Hong Kong. Clin Infect Dis 2005;40:1713–20. 10.1086/429923 [DOI] [PubMed] [Google Scholar]
- 24.Lee TMC, Chi I, Chung LWM, et al. Ageing and psychological response during the post-SARS period. Aging Ment Health 2006;10:303–11. 10.1080/13607860600638545 [DOI] [PubMed] [Google Scholar]
- 25.Chan SMS, Chiu FKH, Lam CWL, et al. Elderly suicide and the 2003 SARS epidemic in Hong Kong. Int J Geriatr Psychiatry 2006;21:113–8. 10.1002/gps.1432 [DOI] [PubMed] [Google Scholar]
- 26.Lee AM, Wong JGWS, McAlonan GM, et al. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can J Psychiatry 2007;52:233–40. 10.1177/070674370705200405 [DOI] [PubMed] [Google Scholar]
- 27.Wu KK, Chan SK, Ma TM. Posttraumatic stress, anxiety, and depression in survivors of severe acute respiratory syndrome (SARS). J Trauma Stress 2005;18:39–42. 10.1002/jts.20004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chong M-Y, Wang W-C, Hsieh W-C, et al. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br J Psychiatry 2004;185:127–33. 10.1192/bjp.185.2.127 [DOI] [PubMed] [Google Scholar]
- 29.Lee DTS, Sahota D, Leung TN, et al. Psychological responses of pregnant women to an infectious outbreak: a case-control study of the 2003 SARS outbreak in Hong Kong. J Psychosom Res 2006;61:707–13. 10.1016/j.jpsychores.2006.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wong JGWS, Cheung EPT, Cheung V, et al. Psychological responses to the SARS outbreak in healthcare students in Hong Kong. Med Teach 2004;26:657–9. 10.1080/01421590400006572 [DOI] [PubMed] [Google Scholar]
- 31.Zheng G, Jimba M, Wakai S. Exploratory study on psychosocial impact of the severe acute respiratory syndrome (SARS) outbreak on Chinese students living in Japan. Asia Pac J Public Health 2005;17:124–9. 10.1177/101053950501700211 [DOI] [PubMed] [Google Scholar]
- 32.Su T-P, Lien T-C, Yang C-Y, et al. Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: a prospective and periodic assessment study in Taiwan. J Psychiatr Res 2007;41:119–30. 10.1016/j.jpsychires.2005.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open 2020;3:e203976. 10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu Y, Wang L, Chen L, et al. Mental health status of paediatric medical workers in China during the COVID-19 outbreak. Front Psychiatry 2020;11:702. 10.3389/fpsyt.2020.00702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lung F-W, Lu Y-C, Chang Y-Y, et al. Mental symptoms in different health professionals during the SARS attack: a follow-up study. Psychiatr Q 2009;80:107–16. 10.1007/s11126-009-9095-5 [DOI] [PubMed] [Google Scholar]
- 36.Lu Y-C, Shu B-C, Chang Y-Y, et al. The mental health of hospital workers dealing with severe acute respiratory syndrome. Psychother Psychosom 2006;75:370–5. 10.1159/000095443 [DOI] [PubMed] [Google Scholar]
- 37.Liem A, Wang C, Wariyanti Y, et al. The neglected health of international migrant workers in the COVID-19 epidemic. Lancet Psychiatry 2020;7:e20. 10.1016/S2215-0366(20)30076-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kang X, Fang Y, Li S, et al. The benefits of indirect exposure to trauma: the relationships among vicarious posttraumatic growth, social support, and resilience in ambulance personnel in China. Psychiatry Investig 2018;15:452–9. 10.30773/pi.2017.11.08.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Emerging understandings of 2019-nCoV. Lancet 2020;395:311. 10.1016/S0140-6736(20)30186-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lee SM, Kang WS, Cho A-R, et al. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr Psychiatry 2018;87:123–7. 10.1016/j.comppsych.2018.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jech-2020-215927supp001.pdf (216.1KB, pdf)
jech-2020-215927supp002.pdf (12.7KB, pdf)
jech-2020-215927supp003.pdf (7.3MB, pdf)
jech-2020-215927supp004.pdf (67.8KB, pdf)
jech-2020-215927supp005.pdf (157.6KB, pdf)
jech-2020-215927supp006.pdf (73.3KB, pdf)
jech-2020-215927supp007.pdf (13.1MB, pdf)
jech-2020-215927supp008.pdf (2.3MB, pdf)
jech-2020-215927supp009.pdf (1.8MB, pdf)
jech-2020-215927supp010.pdf (4.2MB, pdf)
jech-2020-215927supp011.pdf (533.2KB, pdf)
jech-2020-215927supp012.pdf (196KB, pdf)
jech-2020-215927supp013.pdf (203.2KB, pdf)
jech-2020-215927supp014.pdf (112.4KB, pdf)