Abstract
Objective:
Trainee burnout is on the rise and negative training environments may contribute. In addition, as the proportion of women entering vascular surgery increases, identifying factors that challenge recruitment and retention is vital as we grow our workforce to meet demand. This study sought to characterize the learning environment of vascular residents and to determine how gender-based discrimination and bias (GBDB) affect the clinical experience.
Methods:
A survey was developed to evaluate the trainee experience; demographics and a two-item burnout index were also included. The instrument was sent electronically to all integrated (0 + 5) vascular surgery residents in the United States. Univariate analyses were performed and predictors of burnout identified.
Results:
A total of 284 integrated vascular residents were invited to participate and 212 (75%) completed the survey. Participants were predominantly male (64%) and white (56%), with a median age of 30 years (interquartile range, 28–32 years). Seventy-nine percent of respondents endorsed some form of negative workplace experience and 30% met high-risk criteria for burnout. More than a third (38%) of residents endorsed personally experiencing GBDB, with a significant difference between men and women (14% vs 80%; P < .001). Women were more likely than men to report witnessing GBDB (76% vs 56%; P = .003). Patients and nurses were the most frequently cited sources of GBDB (80% and 64%, respectively), with vascular surgery attendings cited by 41% of trainees. One in four female resident respondents indicated being sexually harassed during the course of training; this was significantly higher than for male residents (25% vs 1%; P < .001). Nearly half (46%) of trainees who witnessed or experienced GBDB thought that quality of patient care, job satisfaction, personal well-being, and personal risk of burnout were directly affected as a result of GBDB. GBDB was predictive of burnout (odds ratio, 1.9; 95% confidence interval, 1.1–3.5; P = .04), as were longer work hours (>80 h/wk; odds ratio, 2.8; 95% confidence interval, 1.1–7.1; P = .03).
Conclusions:
GBDB was experienced by 38% of integrated trainees, with women significantly more affected than men. GBDB is predictive of burnout, and this has significant implications for our specialty in the recruitment and retention of female physicians. Resources addressing these issues are needed to maintain a diverse workforce and to promote physician well-being.
Keywords: Surveys and questionnaires; Workplace; Burnout, professional; Physicians, women; Bias; Residency, vascular surgery
Resident burnout is on the rise, with recent studies showing that rates exceed 25% among vascular surgery trainees.1,2 The personal and professional ramifications of physician burnout are significant as 1 in 16 surgeons contemplate suicide each year, and physician discontent leads to suboptimal patient care and overall decreased productivity.3,4 Apart from the implementation of the 80-hour work week, educators have made little progress in combating resident burnout.5 One potential contributing factor that has received less attention is the learning environment itself.4
A meta-analysis from JAMA Surgery that looked at resident attrition showed that women are more likely to leave surgical residency than men are, which suggests that there may indeed be sex-related differences in the training experience.6 The significant rise in the number of female medical students in conjunction with the stagnancy of the percentage of women applying into integrated vascular surgery residencies makes understanding barriers to retention and recruitment more important than ever.7,8 Addressing these issues is vital not only in maintaining a diverse community and promoting resident well-being but also in growing our workforce to meet increasing demand.9 To that end, this study sought to characterize the perception that integrated (0 + 5) vascular surgery residents have of their learning environment and to describe how gender-based discrimination and bias (GBDB) affect the clinical experience.
METHODS
This study protocol was approved by our local Institutional Review Board. All trainees enrolled in an Accreditation Council for Graduate Medical Education-accredited integrated (0 + 5) vascular surgery training program in the United States were eligible to participate. Eligible participants were identified using publicly available information, and completeness was confirmed by at least one representative trainee within each program. A cross-sectional study design was implemented, and an electronic survey was distributed to all eligible participants in the spring of 2018. An initial e-mail was sent that included the goals of the project, survey structure, Institutional Review Board approval, and remuneration. Up to four reminder e-mails were subsequently sent during a 1-month period. Participation was voluntary, and direct consent was obtained electronically by all who chose to proceed with the survey. Participants who chose not to consent were routed out of the survey. All data were collected anonymously. As an incentive, on survey completion, respondents were offered the opportunity to enter their e-mail addresses into a separate, nonlinked database to receive a $10 gift certificate to an online merchant. REDCap, a secure web-based data collection service, was used for survey administration.10
Survey instrument
The first part of the survey collected data on demographics and training characteristics, including age, gender, relationship status, children, training region, average weekly work hours, and postgraduate year designation. Survey content on negative workplace experiences and GBDB was adapted from a proprietary institutional survey11 as well as from a survey by Bruce et al12 that, using members of the Association of Women Surgeons, studied women’s perceptions of gender-based discrimination in the surgical training and working environment. This survey was designed with the goal of characterizing the integrated vascular training experience. It was piloted with integrated vascular surgery residents across several institutions, checked for internal consistency, and adjusted on the basis of feedback. The final survey, on average, took less than 10 minutes to complete.
Burnout.
Burnout was assessed using two single-item measures adapted from the full Maslach Burnout Inventory, a 22-item index considered the standard for measuring burnout.13,14 This validated approach has been used in several large-scale national studies.15,16 These two items have a strong correlation with the emotional exhaustion and depersonalization domains of burnout, with positive predictive values for high levels of burnout of 88% and 90%, respectively.14,17 High levels of emotional exhaustion and depersonalization are defined as occurring at least weekly,14 and respondents with a high level of emotional exhaustion or depersonalization were considered to have a least one manifestation of burnout. This method has been used in several national studies, including one published by the American College of Surgeons.16,18
Negative workplace experiences.
Respondents were surveyed as to the frequency of generalized negative workplace experiences, including public humiliation, others taking credit for individual work, being assigned tasks as a form of punishment, being physically assaulted, threats to career or reputation, harassment or discrimination on the basis of race/ethnicity, harassment or discrimination on the basis of religion, and sexual harassment. Any positive report of these experiences prompted branching logic, which inquired as to the source of the behavior. Potential source choices included vascular surgery attendings, nonvascular surgery attendings, residents/fellows, medical students, nursing staff, patients, and patient visitors. As such experiences are not necessarily limited to one occurrence, respondents were allowed to choose multiple sources.
GBDB.
Finally, using a 7-point Likert scale, participants were asked about the frequency of experienced or witnessed GBDB (0, none; 6, very frequently). Positive responses prompted inquiries as to the form, sources, locations, and reporting of GBDB. Potential form choices included job satisfaction, quality of patient care, personal well-being, personal risk of burnout, and relationships with staff. Potential source choices were as previously described. Potential location choices included operating room, inpatient floor/ward, clinic, and other. As such experiences are not necessarily limited to one occurrence, respondents were allowed to choose multiple forms, sources, and locations. Respondents who experienced or witnessed GBDB were also asked whether these experiences were formally or informally reported. With respect to reporting mechanisms, participants were asked only about GBDB and not other negative workplace experiences: Have you ever chosen to formally report personal or witnessed GBDB experiences during your residency training?
Definitions
For the purposes of this survey, participants were informed to use the following definition of GBDB: “prejudicial treatment of or prejudice against a person on the basis of gender.” All geographic data presented are based on location of the training institution; respondents were allowed to choose one of four regional designations, as determined by the standard U.S. Census Bureau classification system: Midwest, Northeast, South, and West.19 Information on workplace experiences and observations was collected on the basis of frequency. For example, when asked, “Within the context of your career as a vascular surgery resident, how often have you personally experienced [public humiliation]?”, respondents were allowed to choose from one of the following six responses: never, a few times a year or less, once a month or less, a few times a month, a few times a week, or every day. For subsequent analyses, these responses were dichotomized into “never” vs “any experience.” In this paper, the term workplace refers specifically to the clinical training environment, including but not limited to hospital, clinic, and operating room; the participant was explicitly directed that all workplace experiences characterized in the survey should be referable to his or her experience as a trainee.
Statistical analysis
Statistical analysis was performed with Stata/SE 13 software (StataCorp LLC, College Station, Tex). Response bias analysis was performed using publicly available demographic data on gender and training institution. Dichotomous variables are described as a percentage of the cohort. Continuous variables are expressed as median (interquartile range [IQR]). Univariate analysis was performed to compare baseline demographics and workplace experiences. For each comparison, the χ2 test was used for discrete variables and the Mann-Whitney U test for continuous variables. Significant factors in univariate analysis were included in a logistic regression model to determine independent predictors of burnout, and subsequent goodness-of-fit (Hosmer-Lemeshow lack of fit) tests were performed. A P value of < .05 was considered significant.
RESULTS
Demographics.
There were 284 integrated trainees across 51 institutions who were invited to participate in the survey. Of these, 212 completed the survey for a response rate of 75%. At least one trainee from each of the 51 institutions participated, and 9 programs had 100% participation rates. Sixty-four percent (n = 136) of respondents were men and 36% (n = 76) were women; among all current integrated U.S. trainees, 34% (n = 97) are women. Median age was 30 years (IQR, 28–30 years), and most residents were white (n = 118 [56%]). Of the respondents, 27% (n = 57) were single and 23% (n = 78) had children. Men were more likely than women to have children (29% vs 13%; P = .01), but otherwise demographics were similar across genders (Table I).
Table I.
Demographic and training characteristics of integrated vascular surgery trainees, stratified by gender
| Total cohort (N = 212) | Men (n = 136 [64%]) | Women (n = 76 [36%]) | P | |
|---|---|---|---|---|
| Demographics | ||||
| Age, years | 30 (28–32) | 30 (28–32.5) | 30 (28–32) | .68 |
| Nonwhite race | 94 (44) | 66 (49) | 28 (37) | .10 |
| Relationship status: single | 57 (27) | 33 (24) | 24 (32) | .25 |
| Has children: yes | 49 (23) | 39 (29) | 10 (13) | .01 |
| Training characteristics | ||||
| Weekly work hours | 78 (70–80) | 78 (70–80) | 79.5 (70–80) | .70 |
| Region | .85 | |||
| Northeasta | 85 (40) | 55 (40) | 30 (39) | |
| Midwestb | 60 (28) | 36 (26) | 24 (32) | |
| Southc | 41 (19) | 27 (20) | 14 (18) | |
| Westd | 26 (12) | 18 (13) | 8 (11) | |
| Postgraduate year | .79 | |||
| 1 | 46 (22) | 28 (21) | 18 (24) | |
| 2 | 41 (19) | 27 (20) | 14 (18) | |
| 3 | 46 (22) | 29 (21) | 17 (22) | |
| 4 | 38 (18) | 27 (20) | 11 (14) | |
| 5 | 24 (11) | 13 (10) | 11 (14) | |
| Research | 17 (8) | 12 (9) | 5 (7) |
Categorical variables are presented as number (%). Continuous variables are presented as median (interquartile range). Region is based on location of training institution.
CT, MA, ME, NH, NJ, NY, PA, RI, VT.
IA, IL, IN, KS, MI, MN, MO, ND, NE, OH, SD, WI.
AL, AR, DE, FL, GA, KY, LA, MD, MS, NC, OK, SC, TN, TX, VA, WV, District of Columbia.
AK, AZ, CA, CO, HI, ID, MT, NV, NM, OR, UT, WA, WY.
Training characteristics.
The median time worked per week was 78 hours (IQR, 70–80 hours), with no difference between genders. Regional distribution of training institutions and postgraduate year distribution are demonstrated in Table I.
Negative workplace experiences.
Overall, 79% (n = 168) of respondents endorsed at least one negative workplace experience during the course of residency. More than half of trainees reported some form of public humiliation (55%), with women more likely than men to endorse this experience (64% vs 49%; P = .03); of note, when responses were dichotomized comparing monthly (or more) occurrences of public humiliation vs less than monthly, there was no longer a difference when stratified by gender (male, 18%; female, 20%; P = .81). Nine residents (4%) were physically assaulted, whereas 31 (15%) had threats to their career. The majority of participants (56%; n = 118) stated that someone else had taken credit for individual work at least once during training. Ten percent of residents were sexually harassed, with more women than men noting this experience (25% vs 1%; P < .001). Table II summarizes negative workplace experiences for the cohort.
Table II.
Negative workplace experiences of integrated vascular surgery trainees, stratified by gender
| Total cohort (N = 212) | Men (n = 136 [64%]) | Women (n = 76 [36%]) | P | |
|---|---|---|---|---|
| Public humiliation | 116 (55) | 67 (49) | 49 (64) | .03 |
| Others taking credit for work | 118 (56) | 71 (52) | 47 (62) | .18 |
| Physical assault | 9 (4) | 6 (4) | 3 (4) | .87 |
| Threats to career | 31 (15) | 20 (15) | 11 (14) | .96 |
| Harassment on the basis of | ||||
| Race/ethnicity | 20 (9) | 16 (12) | 4 (5) | .12 |
| Religion | 4 (2) | 3 (2) | 1 (1) | .65 |
| Sexual harassment | 21 (10) | 1 (1) | 19 (25) | <.001 |
| Personal experience of GBDB | 80 (38) | 19 (14) | 61 (80) | <.001 |
GBDB, Gender-based discrimination or bias.
Values are reported as number (%).
GBDB.
Thirty-eight percent of respondents (n = 80) endorsed experiencing some form of GBDB during training, with women significantly more likely than men to report this (80% vs 14%; P < .001). The most common sources of GBDB were patients (80%; n = 64/80) and nursing staff (64%; n = 51/80), whereas vascular surgery attendings were cited by 41% (n = 33/80) of residents (Fig 1). Receiving less patient trust was the most commonly cited form (74%), whereas inappropriate verbal exchange (61%) and being asked to perform a nonmedical task (56%) were also common (Fig 2).
Fig 1.
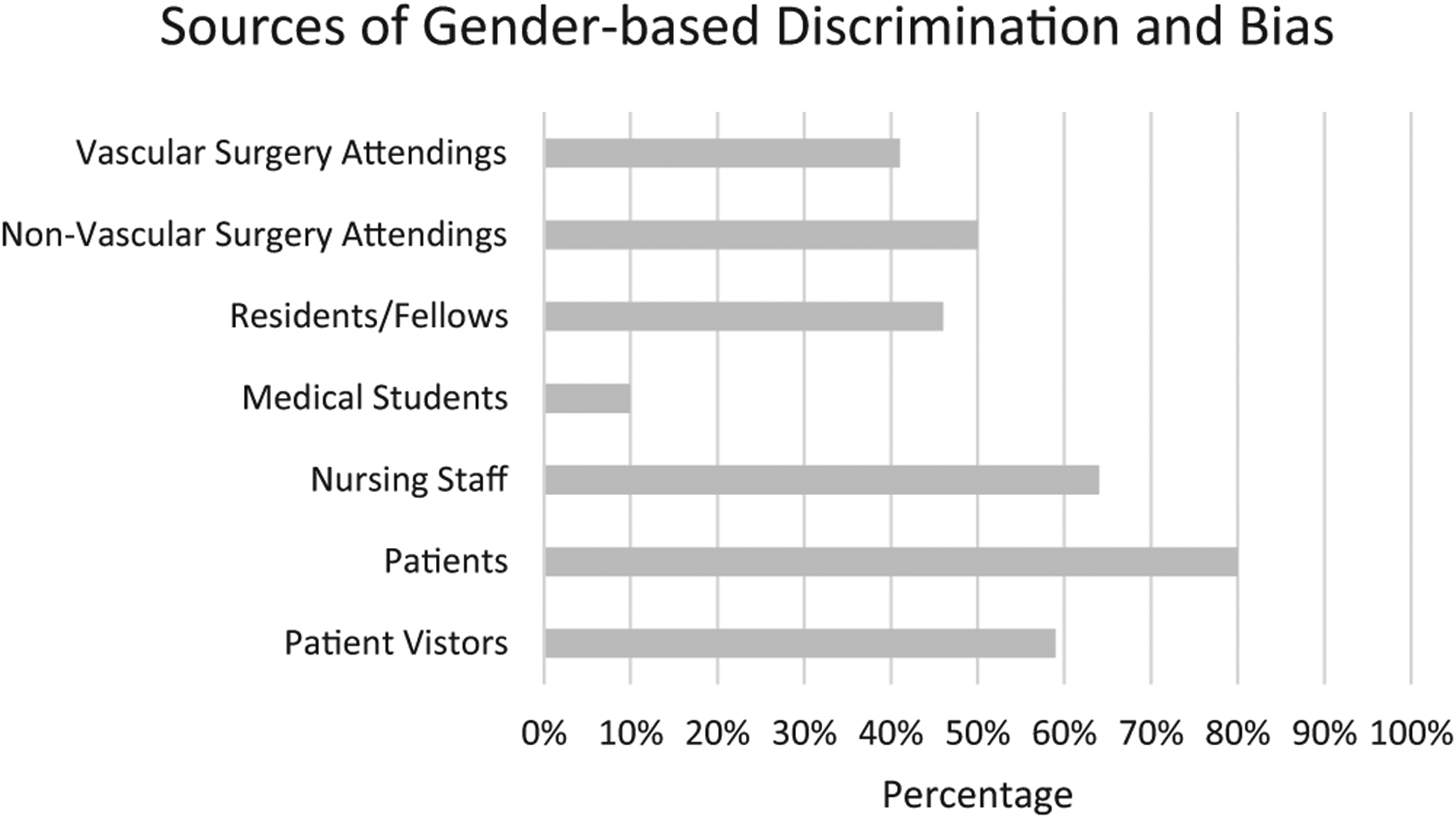
Reported sources of gender-based discrimination and bias (GBDB) among participants who endorsed experiencing GBDB in the workplace (n = 80). Sum is >100% as participants were allowed to choose multiple sources.
Fig 2.
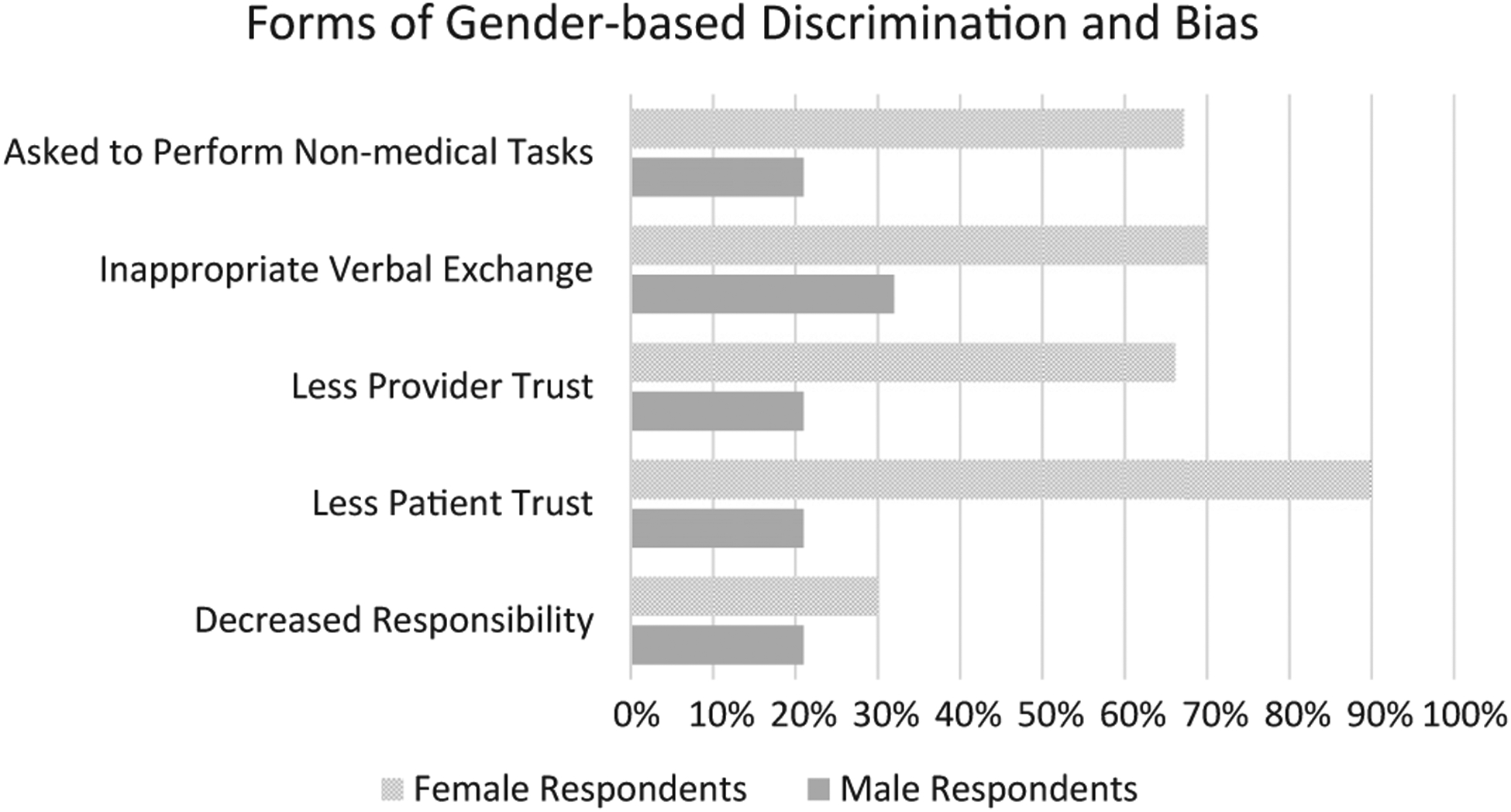
Reported forms of gender-based discrimination and bias (GBDB) among participants who endorsed experiencing GBDB in the workplace (n = 80), stratified by gender. Sum is >100% as participants were allowed to choose multiple forms.
More than half of men reported witnessing GBDB in the workplace (men, 56%; women, 76%; P = .003). Overall, 138 (65%) residents endorsed witnessing or experiencing GBDB. When asked about the factors affected by either witnessed or personally experienced GBDB, job satisfaction (39%; n = 54/138), personal risk of burnout (36%; n = 49/138), and nursing relationships (36%; n = 50/130) were the most commonly cited (Fig 3). When asked about the location of witnessed or experienced GBDB, 91% endorsed seeing or experiencing this on the inpatient ward, whereas 62% noted occurrences in the operating room and 43% in the clinic.
Fig 3.
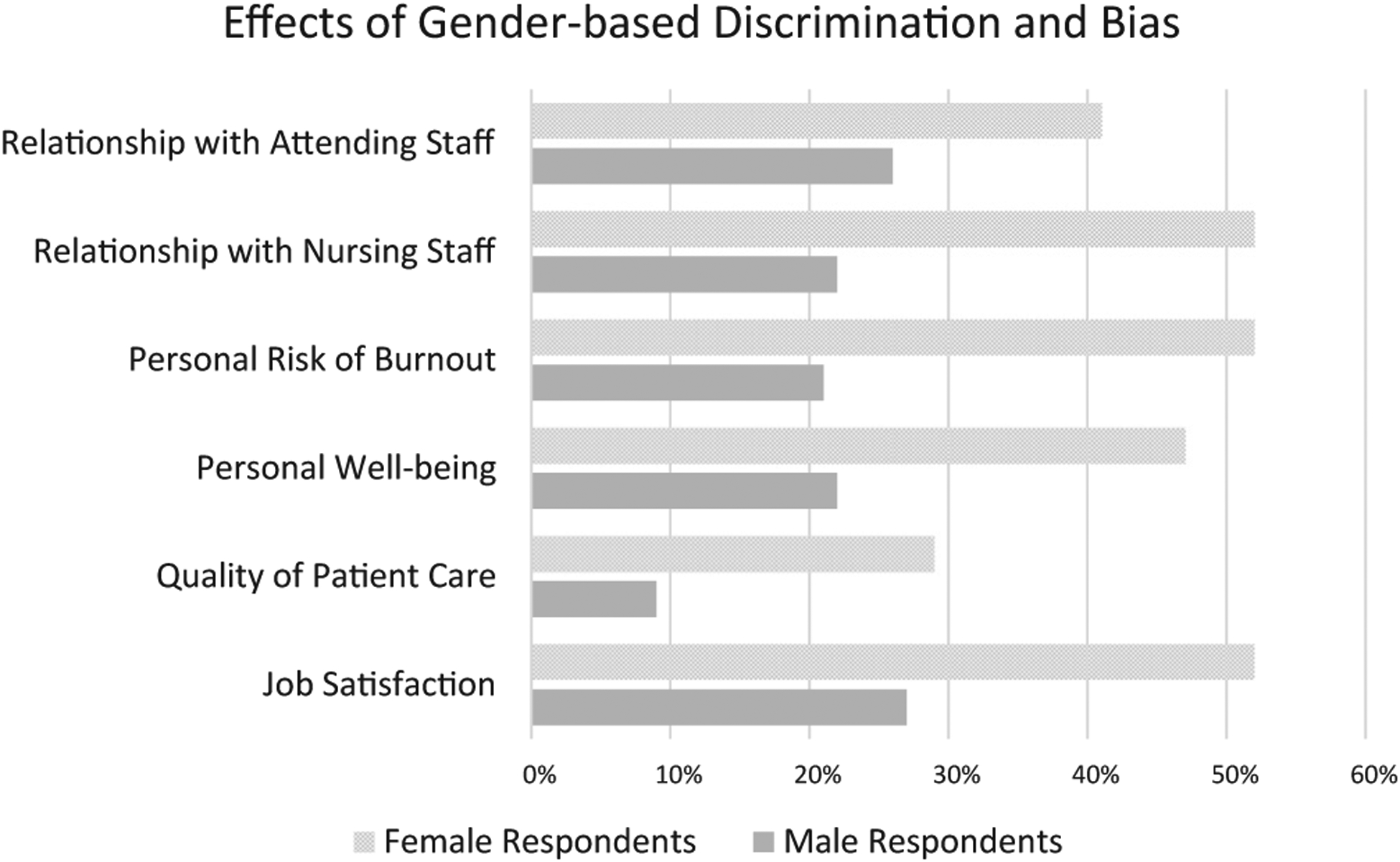
Reported perceived effects of gender-based discrimination and bias (GBDB) among participants who experienced or witnessed GBDB in the workplace (n = 138), stratified by gender. Sum is >100% as participants were allowed to choose multiple responses.
Only 7 of the 138 of residents (5%) who experienced or witnessed GBDB in the workplace chose to formally report it. Of the seven reports, four (57%) said nothing was done as a result of reporting. When the remaining 131 respondents were asked why they chose not to report it, the majority stated that they believed nothing would be done if the incident was reported (56%; n = 74); 34% (n = 45) said they were too busy, whereas 29% (n = 38) feared negative personal or professional consequences of reporting.
Burnout.
High levels of emotional exhaustion were noted in 19% of residents (n = 41), whereas high levels of depersonalization were seen in 22% (n = 47). Overall, 30% (n = 63) of residents demonstrated at least one manifestation of burnout. Predictors of burnout were identified. GBDB was predictive (odds ratio, 1.9; 95% confidence interval, 1.1–3.5; P = .04), as were longer work hours (>80 h/wk; odds ratio, 2.8; 95% confidence interval, 1.1–7.1; P = .03).
Response bias.
No response bias on the basis of gender or training region was detected. Women composed 36% of the “respondent” cohort and 29% of the “nonrespondent” cohort (P = .30). Furthermore, no one training region was more likely to respond than another (P = .11).
DISCUSSION
To our knowledge, this is the first study that has sought to characterize the vascular surgery training environment, and we present these results using the largest cohort of vascular surgery trainees studied to date. With a robust response rate of 75%, we found that among 212 integrated vascular residents across 51 institutions, 4 in 5 endorsed negative workplace experiences, ranging from public humiliation to physical assault. Notably, 10% of trainees were sexually harassed, with up to one in four female residents noting this experience. Thirty-eight percent of trainees had been discriminated against on the basis of gender, and women were significantly more likely to be affected. Furthermore, individuals who experienced GBDB were at a 90% increased risk of burnout.
These findings are important for several reasons. First, although burnout during residency has been recognized for nearly 20 years,20 educators have made little headway in mitigating this issue and continue to struggle with determining appropriate methods to effectively combat it.5 Progress has been made with the implementation of the 80-hour work week, and our study confirms what others have found, notably that longer (>80 hours) work weeks are associated with increased risk of burnout.2,21 Yet burnout rates remain high. Janko and Smeds2 recently surveyed 177 vascular trainees and found a 25% burnout rate, similar to our findings of 30%. Such statistics suggest that work remains to be done. We thus approached this study with the hypothesis that to better address trainee burnout, we must consider not only the constructs of the learning environment but also its milieu.4
Among integrated vascular surgery residents, 79% had experienced at least one negative workplace behavior during training, which is similar to reported percentages among general surgery residents, nonsurgical medical trainees, and nonmedical professionals.22–25 In a recent study by McKinley et al11 that surveyed general surgery, medicine, and anesthesia residents across two institutions, rates of GBDB ranged from 30% to 36% across the three specialties, which is slightly lower than the 38% we found. In this manuscript, GBDB was the most commonly cited negative workplace experience among female integrated residents, and the perceived consequences were meaningful. Job satisfaction, personal well-being, and personal risk of burnout were the most commonly cited effects of workplace GBDB. These findings are important not only for retention but for recruitment as well. In a survey of female medical students, 47% perceived sex discrimination during their surgical rotation and endorsed “surgical personality” and the perception of surgery as an “old boys’ network” as deterrents to a surgical career.26
Such statistics highlight the importance of a change in surgical culture and the need to provide an environment conducive to women. This is especially pertinent for vascular surgery as only 13% of its workforce are women; in contrast, women compose 35% of the active physician workforce in the United States.27 Furthermore, a 170% increase in the number of female residency applicants during the past 10 years has been noted, with women now representing nearly half of all residency applicants.7 With a predicted 10% shortage in the vascular surgery workforce during the next decade, our specialty cannot afford to ignore these trends.8,9 Indeed, the stagnancy of the percentage of women applying to integrated vascular residencies suggests that there is still room for improvement.
As of 2017, women composed 36% of integrated vascular residents, signaling that progress is indeed being made.28 Further signs of change are demonstrated in this study; even though only 14% of male residents reported experiencing GBDB, more than half (56%) reported witnessing it. Awareness of sex-related differences in the training experience is the first step in improving the learning environment, and it is our hope that armed with the information presented herein, program directors and division chiefs will be empowered and encouraged to start having a discussion about the training environment. However, the issue of patients being the most commonly cited source of GBDB is not lost on the authors. This challenging problem is not unique to surgery, and strategies for addressing these scenarios have been presented.24,29 Effective interventions include case discussions with simulated encounters, cultural competency and implicit bias education, and formalization of hospital policies and resources.30 More study on this topic is needed, but it would seem that most hospitals would benefit from ubiquitous distribution of institutional policies regarding the approach to the disruptive or discriminatory patient.
These interventions highlight the need for institutional reform in effecting change. In particular, our study found substantial deficits in current formal reporting mechanisms. Only 5% of trainees who witnessed or experienced GBDB formally reported it, and in 57% (n = 4/7) of cases, nothing was done. Furthermore, more than half of respondents stated that their primary reason for not filing a report was the belief that nothing would be done. Improving confidence in and access to mechanisms that enable residents to voice instances of mistreatment is essential in combating negative workplace behaviors; streamlining the reporting process may also prove beneficial. Such initiatives are likely to benefit trainees in other specialties as well because the issues presented herein have been shown to also be a problem among internal medicine, anesthesia, and general surgery residents.11
Factors responsible for burnout are multiple and complex. Whereas our results would suggest that GBDB and learning environment characteristics are likely to be contributory, there remain other factors at large. The high saturation of GBDB among female residents makes the role of gender less clear. Several studies analyzing large populations of practicing surgeons found that women were more prone to burnout than men,31,32 and this has been demonstrated in general surgery resident populations as well.21 Yet, recent studies focusing solely on vascular trainees found no association between sex and high levels of burnout.2 Similarly, we found that female sex did not correlate with burnout, but a trend toward higher rates of burnout among women was appreciated (36% vs 26%; P = .17).
Limitations.
This study has several limitations. The first lies in the inherent nature of self-reporting, in which responses are unable to be independently verified. Recall and reporting biases are acknowledged, and as this was a cross-sectional study, only one time point was captured. It is possible that based on clinical rotation, changes in weekly work hours and levels of burnout will oscillate. Even though this is the largest reported study to date surveying vascular trainees, the sample size is relatively small. Furthermore, as the study population was limited to integrated vascular surgery trainees, these results may not reflect the vascular surgery fellowship experience or other surgical training programs. Finally, as with all surveys, response bias is always a concern, and although we found no response bias with respect to gender or geographic region, other factors not accounted for may play a role. The payment incentive may have added an additional aspect of response bias; however, as residents are salaried on the basis of geographic cost of living, it is unlikely that this small remuneration was a significant factor.
CONCLUSIONS
We found that 79% of integrated vascular surgery residents have experienced at least one negative workplace behavior during the course of training. GBDB was the most commonly noted negative experience among female surgical residents, affecting up to four in five female trainees. Even though only 14% of male trainees experienced GBDB, more than half reported witnessing such behaviors, and this signals a positive change in surgical culture. GBDB is associated with higher risk of burnout, and this has significant implications for our specialty in the recruitment and retention of female physicians. Resources addressing these issues, with particular focus on formal reporting mechanisms, are needed to maintain a diverse workforce and to promote physician well-being.
ARTICLE HIGHLIGHTS.
Type of Research: Cross-sectional, anonymous national survey
Key Findings: Survey responses from 212 integrated (0 + 5) vascular surgery residents were collected and analyzed; 38% of trainees endorsed experiencing gender-based discrimination or bias (GBDB) during residency, with women significantly more affected than men; 43% of trainees thought that GBDB affected patient care, job satisfaction, or personal well-being, and GBDB was predictive of burnout.
Take Home Message: The authors suggest that GBDB plays an important role in the trainee experience and that resources addressing these issues are needed to maintain a diverse workforce and to promote physician well-being.
Acknowledgments
We would like to thank the following individuals for their support of this project: Dr Meena A. Archie (UCLA), Dr Melissa Baldwin (Icahn School of Medicine at Mount Sinai), Dr Jocelyn Beach (Cleveland Clinic), Dr Mina L. Boutrous (St. Louis University), Dr Avianne Bunnell (Medical University of South Carolina), Dr Meghan Davis (Charleston Area Medical Center), Dr Jeffrey B. Edwards (University of South Florida), Dr Marissa Famularo (Cooper University Hospital), Dr Julia Glaser (University of Pennsylvania), Dr Anthony Grieff (Rutgers University), Dr Katherin Holzem (Washington University in St. Louis), Dr Matthew R. Janko (University Hospitals Cleveland Medical Center), Dr Alison J. Kinning (TriHealth), Dr Julia Kleene (Albany Medical Center), Dr Mimmie Kwong (UC Davis), Dr Patric Liang (Beth Israel Deaconess Medical Center), Dr Thomas Loh (Houston Methodist Hospital), Dr Sean Malarkey (Allegheny General Hospital), Dr Kimberly T. Malka (University of Massachusetts), Dr Anna Marjan (University of Iowa), Dr Sara McKeever (University of Arkansas), Dr Vicent Noori (Maine Medical Center), Dr Anna Ohlsson (University of Washington), Dr Georgina Pappas (University of Rochester), Dr Jennifer L. Perri (Dartmouth), Dr John Phair (Montefiore Medical Center), Dr Willythssa S. Pierre-Louis (University of Cincinnati), Dr Neil Reddy (Keck School of Medicine of USC), Dr Brendon Reilly (University at Buffalo), Dr Scott T. Robinson (University of Michigan), Dr Indrani Sen (Mayo Clinic) Dr Michael Siah (MedStart Heart and Vascular Institute), Dr Rachael Snow (Pennsylvania State University), Dr Sarah Strot (Michigan State), Dr Shruthi Thiagarajasubramanian (University of Wisconsin), Dr Marta Vismer (Hofstra Northwell), and Dr Clay Wiske (New York University School of Medicine).
This work was funded using institutional research funds of the Division of Vascular and Endovascular Surgery at the Massachusetts General Hospital.
Footnotes
Author conflict of interest: none.
Presented at the Forty-seventh Annual Symposium of the Society for Clinical Vascular Surgery, Boca Raton, Fla, March 16–20, 2019, and winner of the 2019 Peter B. Samuels Award.
REFERENCES
- 1.Dimou FM, Eckelbarger D, Riall TS. Surgeon burnout: a systematic review. J Am Coll Surg 2016;222:1230–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Janko MR, Smeds MR. Burnout, depression, perceived stress, and self-efficacy in vascular surgery trainees. J Vasc Surg Article 2019;69:1233–42. [DOI] [PubMed] [Google Scholar]
- 3.Shanafelt TD, Balch CM, Dyrbye L, Bechamps G, Russell T, Satele D, et al. Special report: suicidal ideation among American surgeons. Arch Surg 2011;146:54–62. [DOI] [PubMed] [Google Scholar]
- 4.Dyrbye L, Shanafelt T. A narrative review on burnout experienced by medical students and residents. Med Educ 2016;50:132–49. [DOI] [PubMed] [Google Scholar]
- 5.Busireddy KR, Miller JA, Ellison K, Ren V, Qayyum R, Panda M. Efficacy of interventions to reduce resident physician burnout: a systematic review. J Grad Med Educ 2017;9:294–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khoushhal Z, Hussain MA, Greco E, Mamdani M, Verma S, Rotstein O, et al. Prevalence and causes of attrition among surgical residents: a systematic review and meta-analysis. JAMA Surg 2017;152:265–72. [DOI] [PubMed] [Google Scholar]
- 7.Arous EJ, Judelson DR, Simons JP, Aiello FA, Doucet DR, Arous EJ, et al. Increasing the number of integrated vascular surgery residency positions is important to address the impending shortage of vascular surgeons in the United States. J Vasc Surg 2018;67:1618–25. [DOI] [PubMed] [Google Scholar]
- 8.Association of American Medical Colleges. ERAS statistics. Available at: https://www.aamc.org/services/eras/stats/359278/stats.html. Accessed December 17, 2018.
- 9.Satiani B, Williams TE, Go MR. Predicted shortage of vascular surgeons in the United States: population and workload analysis. J Vasc Surg 2009;50:946–52. [DOI] [PubMed] [Google Scholar]
- 10.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)da metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McKinley SK, Wang LJ, Gartland RM, Westfal ML, Costantino CL, Schwartz D. “Yes, I’m the doctor”: One department’s approach to assessing and addressing gender-based discrimination in the modern medical training era. Acad Med 2019;94:1691–8. [DOI] [PubMed] [Google Scholar]
- 12.Bruce AN, Battista A, Plankey MW, Johnson LB, Marshall MB. Perceptions of gender-based discrimination during surgical training and practice. Med Educ Online 2015;20:25923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory manual. 3rd ed. Palo Alto, Calif: Consulting Psychologists Press; 1996. [Google Scholar]
- 14.West CP, Dyrbye LN, Sloan JA, Shanafelt TD. Single item measures of emotional exhaustion and depersonalization are useful for assessing burnout in medical professionals. J Gen Intern Med 2009;24:1318–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.West CP, Shanafelt TD, Kolars JC. Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA 2011;306:952–60. [DOI] [PubMed] [Google Scholar]
- 16.Dyrbye LN, Sotile W, Boone S, West CP, Tan L, Satele D, et al. A survey of U.S. physicians and their partners regarding the impact of work-home conflict. J Gen Intern Med 2014;29:155–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.West CP, Dyrbye LN, Satele DV, Sloan JA, Shanafelt TD. Concurrent validity of single-item measures of emotional exhaustion and depersonalization in burnout assessment. J Gen Intern Med 2012;27:1445–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shanafelt TD, Balch CM, Bechamps GJ, Russell T, Dyrbye L, Satele D, et al. Burnout and career satisfaction among American surgeons. Ann Surg 2009;250:463–71. [DOI] [PubMed] [Google Scholar]
- 19.United States Census Bureau. Geography: regions. Available at: https://www.census.gov/geo/reference/webatlas/regions.html. Accessed April 3, 2018.
- 20.Thomas NK. Resident burnout. JAMA 2004;292:2880–9. [DOI] [PubMed] [Google Scholar]
- 21.Elmore LC, Jeffe DB, Jin L, Awad MM, Turnbull IR. National survey of burnout among US general surgery residents. J Am Coll Surg 2016;223:440–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ling M, Young CJ, Shepherd HL, Mak C, Saw RP. Workplace bullying in surgery. World J Surg 2016;40:2560–6. [DOI] [PubMed] [Google Scholar]
- 23.Kulaylat AN, Qin D, Sun SX, Hollenbeak CS, Schubart JR, Aboud AJ, et al. Perceptions of mistreatment among trainees vary at different stages of clinical training. BMC Med Educ 2017;17:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li SF, Grant K, Bhoj T, Lent G, Garrick JF, Greenwald P, et al. Resident experience of abuse and harassment in emergency medicine: ten years later. J Emerg Med 2010;38:248–52. [DOI] [PubMed] [Google Scholar]
- 25.Samnani AK, Singh P. 20 Years of workplace bullying research: a review of the antecedents and consequences of bullying in the workplace. Aggress Violent Behav 2012;17: 581–9. [Google Scholar]
- 26.Gargiulo DA, Hyman NH, Hebert JC. Women in surgery: do we really understand the deterrents? Arch Surg 2006;141: 405–7; discussion: 407–8. [DOI] [PubMed] [Google Scholar]
- 27.Association of American Medical Colleges. 2018. AAMC physician specialty data report. Available at: https://www.aamc.org/download/493090/data/2018-aamc-physician-specialty-data-report.pdf. Accessed December 17, 2018.
- 28.Association of American Medical Colleges. Number of active residents, by type of medical school, GME specialty, and sex. Available at: https://www.aamc.org/data/484718/report-on-residents-2017-b3table.html. Accessed December 17, 2018.
- 29.Mullan CP, Shapiro J, McMahon GT. Interns’ experiences of disruptive behavior in an academic medical center. J Grad Med Educ 2013;5:25–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Whitgob EE, Blankenburg RL, Bogetz AL. The discriminatory patient and family: strategies to address discrimination towards trainees. Acad Med 2016;91(11 Association of American Medical Colleges Learn Serve Lead: Proceedings of the 55th Annual Research in Medical Education Sessions):S64–9. [DOI] [PubMed] [Google Scholar]
- 31.Dyrbye LN, Shanafelt TD, Balch CM, Satele D, Sloan J, Freischlag J. Relationship between work-home conflicts and burnout among American surgeons: a comparison by sex. Arch Surg 2011;146:211–7. [DOI] [PubMed] [Google Scholar]
- 32.Shanafelt TD, Oreskovich MR, Dyrbye LN, Satele DV, Hanks JB, Sloan JA, et al. Avoiding burnout: the personal health habits and wellness practices of US surgeons. Ann Surg 2012;255:625–33. [DOI] [PubMed] [Google Scholar]


