Abstract
Background
Water pipe smoking (WPS) is re-gaining widespread use and popularity among various groups of people, especially adolescents. Despite different adverse health effects of WPS, many of the WPS interventions have failed to control this type of tobacco smoking. This study was conducted to identify experienced management interventions in preventing and controlling WPS worldwide.
Methods
A systematic literature review was conducted. Electronic databases were searched for recordes which were published from beginning 1990 to August 2018. Studies aiming at evaluating, at least, one intervention in preventing and controlling WPS were included in this review, followed by performing the quality assessment and data extraction of eligible studies by two independent investigators. Finally, interventions that were identified from the content analysis process were discussed and classified into relevant categories.
Results
After deleting duplications, 2228 out of 4343 retrieved records remained and 38 studies were selected as the main corpus of the present study. Then, the identified 27 interventions were grouped into four main categories including preventive (5, 18.51%) and control (8, 29.62%) interventions, as well as the enactment and implementation of legislations and policies for controlling WPS at national (7, 25.92%) and international (7, 25.92%) levels.
Conclusion
The current enforced legislations for preventing and controlling WPS are not supported by rigorous evidence. Informed school-based interventions, especially among adolescents can lead to promising results in preventing and controlling WPS and decreasing the effects of this important social and health crisis in the global arena.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-021-10306-w.
Keywords: Management interventions, water pipe, smoking, Tobacco control
Background
Tobacco smoking is one of the main preventable causes of diseases and deaths claiming the lives of 7.2 million annually around the world [1, 2]. Although cigarette smoking is the dominant form of tobacco use in many countries, Water Pipe Smoking (WPS) with other names such as hookah, shisha, narghile, arghile. Goza, oriented pipe, hubble bubble, Mada’s and glaze base, accounts for a significant and growing share of tobacco use globally [3, 4]. In addition, WPS is a culture-based (there are some other types of tobacco smoking behavior) method of tobacco use [5] and its history goes back to 500 years ago in Middle East, North Africa and Asia. However, it has experienced a worldwide re-emergence since 1990 [6] and is regaining popularity among different groups of populations, especially in school and university students [7, 8]. Although WPS is most prevalent in Asia (specifically the Middle East region) and Africa, it has now been changed to a rapidly emerging problem in other continents such as Europe, North, and South America [9, 10]. In recent years, there has been 6–34% increase in tobacco use among 13–15 year olds, most of whom attribute to WPS [10, 11]. In European regions such as Latvia and Czech Republic 22.7 and Estonia 21.9% of people smoke water pipe, while in the Eastern Mediterranean region, the prevalence of WPS is 39.0 and 31.0% of boys and girls, respectively [12]. In average, Lebanon has the highest reported rate (37%) in this regard [12, 13]. In the United States, more than 30% of university students of both genders and 23% of high school students have experienced WPS [14, 15]. Similarly, WPS is also prevalent among highly educated groups. Nearly 20% of health professionals in Jordan and 11% of medical students in London smoked WP [16, 17]. Based on a report, 29.5% of physicians also experience WPS in Pakistan [18].
It has been shown that WPS’ smoking rate can be more addictive compared to that of the cigarette. It also contains more toxic and carcinogenic substances [19, 20] with deleterious effects on the respiratory and cardiovascular systems, as well as oral cavity and teeth [21]. Furthermore, it has a huge negative impact on health costs and the gross domestic product of the countries. For example, the direct and indirect cost of smoking-related diseases is up to $300 billion in the United States annually [22, 23].
Considering the extension of WP businesses, some groups support its expansion [24]. In recent years, the number of WP cafes has increased over many countries. As an example, there are nearly 400 WP cafes in London [25].
Using deceptive advertising, many cafes and restaurants offer WP services along with their orthodox services in order to earn more profit and lure more customers. Moreover, several factors contribute to attracting children and adolescents to WP cafes that leads to an increase in new cases of WPS [26–28]. These factors include the provision of flavored tobacco products or psychotropic WP, the proximity of WP cafe to the public settings such as educational or residential settings, sports clubs, and residential areas, tempting decoration, the provision of study places for students, live music, a variety of games and gambling, and the possibility of watching live movie and sport matches [6, 25, 29, 30].
All this shows that WPS has been turning to a public health crisis. WP business has remained largely unregulated and uncontrolled, which may result in the increasing prevalence of WPS [31]. Moreover, WPS is one of the main factors that can lead to failure in tobacco control [32]. Despite the concerns about WPS outcomes and nearly three decades of using control measures, the prevalence of WPS has increased over the world. Due to the unique nature of WP (multi-components), little is known about the prevention and control of WPS [33]. Thus, special actions and interventions might be required to prevent and control WP tobacco use [33]. Over the recent decade, there has been growing interest among researchers and policymakers regarding addressing the gaps in knowledge about interventions that can be useful in controlling and preventing WPS. Accordingly, this study aimed to identify the management interventions in international and national levels for preventing and controlling water pipe smoking.
Methods
Study design
A systematic literature review was conducted. The Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) guideline [3] was used for performing and reporting the review.
Inclusion criteria
Primary studies aiming at evaluating, at least, one intervention in preventing and controlling WPS were included.
Population
WP consumers or people who are likely to be WP consumers in the near future.
Intervention
Activities, programs, or strategies at the management level aiming at preventing and controlling WP use.
Outcome
A categorized array of themes presenting a comprehensive picture of management interventions which are targeting WPS prevention and control.
Search strategy
PubMed, ISI Web of Science, Embase, Scopus, Science Direct, and Ovid were searched for published records from beginning 1990 to August 2018. Further, the first 10 pages of Google Scholar function, World Health Organization (WHO) and World Bank websites were also searched for relevant studies. Additional file 1 provides the terms and search strategy in PubMed.
Exclusion criteria
Studies were excluded if their focus were on various forms of tobacco use and not just WP use or if they did not distinguish WPS from other forms of tobacco use.
Quality appraisal
According to the type of the included studies, the critical appraisal checklists of the Joanna Briggs Institute [34] were used for quality appraisal. The Joanna Briggs Institute (JBI) is an international, membership based research and development organization within the Faculty of Health Sciences at the University of Adelaide. JBI Critical appraisal tools have been developed by the JBI and collaborators and approved by the JBI Scientific Committee following extensive peer review. These tools were preliminary for use in systematic reviews. Based on a scoring approach (number of “yes” answers divided by all questions), included studies were categorized to high, moderate, or low quality.
Data extraction
The data extraction parameters included author, year, country, study design and setting, type of study, participants, the level and type of interventions, study duration, sample size, and main outcomes.
Data synthesis
Management interventions which influenced controlling and preventing WPS were retrieved and categorized through content analysis method. The interventions were identified and categorized by two researchers (L. D. & J.B) using the following process.
Reading the selected records;
Identifying and extracting the related interventions after calibration to ensure consistency and accuracy;
Grouping the identified interventions into categories and sub-categories based on their conceptual similarity;
Solving disagreements between researchers by discussions. Whenever disagreement persisted the third author was approached. In some cases, the identified interventions were placed in more than one category;
Confirming categories and subcategories.
Results
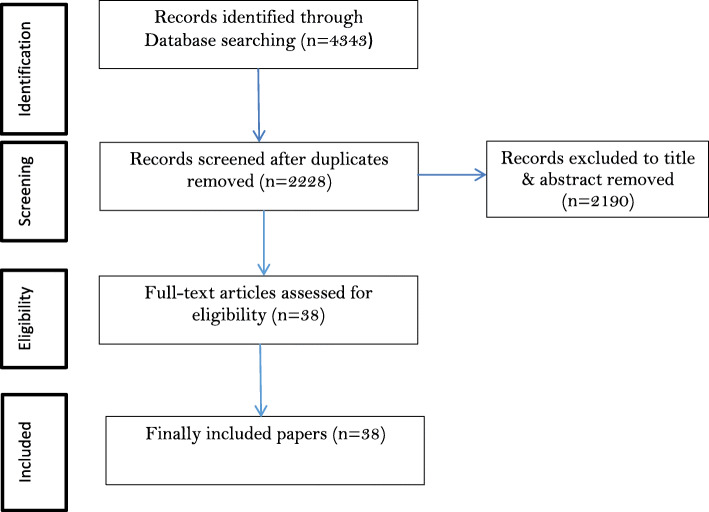
The searching process resulted in 4353 studies with 2125(48.81%) of these being repetitions. Out of 2228 screened articles (after removing the duplicates), 38 articles were selected through on the title& abstract screening process. Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram was used to show the number of records in each phase (Fig. 1).
Fig. 1.
Flow diagram of the search and screening process
The included studies were of moderate-to-high quality. The characteristics of included studies are provided in Table 1.
Table 1.
Characteristics of included studies
| Author/Year | Country | Design | Setting | Method | Target group | Intervention | Study duration | Sample size | Outcome | Quality |
|---|---|---|---|---|---|---|---|---|---|---|
| Lock Karen 2010 | United Kingdom | Qualitative | Community | Interviews | WP smokers | Smoke-free legislation (SFL) | 2007 | 32 | Increase of private smoking | Moderate |
| Highet G. 2011 | United Kingdom | Qualitative | community | Interviews | WP smokers | Implementation of the smoke-free law | April 2007–December 2008 | 120 | Increase of WPS | Moderate |
| Jawad M. 2013 | United Kingdom | Qualitative | universities | Interviews | Regular water pipe smokers | Dispel the misconception about WPS | January–April 2012 | 32 | Decrease of WPS | Moderate |
| Javad M.2014 | United Kingdom | Qualitative | Community | Interviews | local authority staff | Use the experiences of executive authority | May–June 2013 | 26 | Identifying executive problems. | Moderate |
| Mohd Zin F. 2016 | Malaysia | Qualitative | Schools | Semi-structured interviews | Adolescents | Developing new interventions | 2015 | 40 | Urgent need to new interventions | Moderate |
| Grant A.2016 | United Kingdom | Exploratory qualitative | Tweets | Documentation | No human subjects | Prevention of web advertising | Jul-05 | 4439 tweets | WP smoking as an enjoyable activity and a challenge for public health | Moderate |
| Colditz J. B. 2017 | United States | Qualitative (grounded theory) | Web sites | Documentation | No human subjects | Implement of existing tobacco control policies | April–July2013 | - | Current interventions are old | Moderate |
| O’Neill N. 2017 | United Kingdom | Qualitative | Modified Delphi Technique | Experts and scientists of behavioral science | Developing of behavior change techniques | Jul-05 | 24 | Effective interventions in quit of WPS | Good | |
| Mostafa A. 2018 | Egypt | Qualitative | Community | Interviews | Men and women ≥18 | Append of placing pictorial health warnings on WP devices | 2015–2016 | 90 | Effective interventions in WPS prevention and stop | Moderate |
| Anjum Qudsia 2008 | Pakistan | Cross-sectional | School | Pre& post-tested | School students 14–19 years old | Health messages | 2006 | 646 | Improving knowledge of the students | Moderate |
| Shishani K. 2011 | Jordan | Survey | Hospital | Questionnaire | nurses and physicians | Involving of nurses and physicians’ in WPS control | 2010 | 918 | Low incentive and skill to cooperate in WPS control programs. | Moderate |
| Salti Nisreen 2013 | Lebanon | Cross-sectional | Household | Questionnaires | adults | Increasing taxes | 2005 | 13,003 | Decrease of WP tobacco demand | Moderate |
| Ali Quadri M. F.2014 | Saudi Arabia | Cross-sectional | Community | Questionnaire | students 15–25 years | Improving the knowledge | 2013 | 1051 | Increasing knowledge | Moderate |
| Kassem N. O. F. 2015 | United States | Cross-sectional | University | Questionnaire | Undergraduate Student ≥18 | Prohibiting from opening in close to educational places | spring 2007 | 1332 United States | Effective in WPS | Good |
| Erdöl C. 2015 | Turkey | Survey | Community | Questionnaire | Adults ≥15 years | Increasing of excise taxes and size of pictorial health warnings | 2008 and 2012 | 9030 and 9851 | Decrease of WTS | Good |
| Salloum R. G.2015 | United States | Survey | University (Internet-based) | Questionnaire | university students> 18 old & WP smoker | Control fruit-flavored and sweet tobaccos | June–October 2014 | 367 | Decrease of demand for WPS by youth. | Good |
| Islam F. 2016 | United States | Cross-sectional survey | University | Questionnaire | university students smokers > 18 | Append of warning labels | June–October 2014 | 367 | Effective to control WPS. | Good |
| Kingsbury J. H. 2016 | United States | Cross-sectional | Community | Questionnaire | Adults≥18 | Control of occasional and group smokers | 2014 | 242 | Effective to control WPS. | Good |
| Smith D. M. 2016 | United States | Cross-sectional | Telephone-based | Interview | smokers ≥18 | Prevention of first use fruit-flavored and sweet tobacco | November 2012–April 2013 | 1443 | More effective in being non user | Moderate |
| Jaam M.2016 | Qatar | Cross-sectional | Community | Interviews | WP smokers | Empowering the families | July–October 2013 | 181 | Decrease of WTS | Moderate |
| Riggs N. R. 2016 | United States | Survey | School base | Questionnaire | School students | Inhibitory Control and Free Lunch | 2015 | 407 | Decrease of WPS | Moderate |
| Jawad M. 2017 | Germany | Cross-sectional | WP Fair of International | Observation | Tobacco products | Control of packaging and labelling with guidelines | Jul-05 | 35 | More effective in prevention of WPS | Moderate |
| Hamadeh R. R. 2017 | Bahrain | Cross sectional | Quit clinics | Interview | Male patients smokers | Drugs treatment along with counseling | August–December 2015 | 194 | Effective in quit | Moderate |
| VanDevanter N.2017 | United States | Cross-sectional | Web-based | Questionnaire | nursing students | Training of patients by nurses | February–April 2014 | 820 | Effective in decrease of WPS | Good |
| Joudrey P. J.2016 | US-UAE | Cross-sectional survey | Businesses | Observations and interviews | business owners or managers | control of marketing | January–March 2014. | 97 | Need to WP-specific legislation. | Moderate |
| Kowitt S. D.2017 | United States | Survey | Community | Checklist | smokers ≥18 | Use of FDA Regulation for WP | September 2014 to August 2015 | 1520 | More effective to quit | Good |
| Deshpande A 2010. | India | Pre & post test | Hospitality venues | (PM2.5) measurements | No human subjects. | Implementation of the smoke free law in hospitality settings | 2008–2009 | 25 | Decrease of WPS | Low |
| Lipk Isaac M. 2011 | United States | Randomised controlled | Web-based | questionnaire | University students | Educational interventions of online for colleges’ WP smokers | 2009–2010 | 91 | Decrease of WPS | Moderate |
| Stamm-Balderjahn S. 2012 | Germany | Quasi-Experimental | Hospital | Questionnaire | High school students | Educational interventions in clinical settings. | September 2007–July 2008 | 760 | Effective in prevention of smoking | Moderate |
| Mohlman M. K.2013 | Egypt | Quasi-experimental | Community | interviewer | General population | Educational and behavioral interventions | 2005–2006 | 5934 | Increase in the attitudes that WP is harmful | Moderate |
| Asfar T. 2014 | Syria | Randomised controlled | clinical | Adults≥18 | Brief behavioral interventions clinical settings. | November 2007–October 2008 | 50 | Effective in being none smoking | Moderate | |
| Tomaszek S. 2014 | Switzerland | Quasi-Experimental | Hospital | Questionnaire | School students | Brief behavioral interventions by lung specialists. | 2009 - February 2013 | 470 | Effective in prevention of school students smoking. | Moderate |
| Essa-Hadad J.2015 | Israel | Quasi-experimental | Web-based | mixed-methods | Students | Web-based education programs. | 2007–2010 | 225 | Decrease of WPS | Moderate |
| Little M. A. 2016 | United States | Interventional | Military | questionnaire | Air Force trainees | Brief Tobacco Intervention | October 2014–March 2015 | 1055 | Increase of knowledge | Moderate |
| Rozema A. D.2018 | Dutch | Quasi-experimental | Schools | questionnaire | School students | Outdoor school ground smoking bans | 2014–2015 | 7733 | Effective in prevention of WPS | Moderate |
| Momenabadi V. 2017 | Iran | Quasi-experimental | Dormitory | Questionnaire | Students | Educational intervention: BASNEF model | 2014 | 80 | Improving of attitudes that WP is harmful | Low |
| Mahoozi S.2017 | Iran | Semi experimental | Medical and hygienic centers | questionnaire | women | Education of women in health center | November 2015–October 2016 | 60 | Improving attitudes that WP is harmful | Moderate |
| Leavens E. L. S. 2018 | United States | RCT | WPS settings | questionnaire | smokers ≥18 | Testing exhaled carbon monoxide (CO) before and after and personalized feedback | August–December 2014 | 109 | Effective in quitting WPS | Moderate |
The selected studies were published between 1990 and 2018 and focused on 19 different countries including the United States (13.15%) [6, 29, 30, 35, 36], the United Kingdom (7.89%) [25, 37, 38], Germany (5.26%) [12, 39], Iran (5.26%) [40, 41], Egypt [42, 43] (5.26%), Malaysia (2.63%) [44], India (2.63%) [45], Dutch(2.63%) [46], Pakistan (2.63%) [47], Qatar (2.63%) [48], Jordan(2.63%) [16], Lebanon(2.63%) [49], Syria(2.63%) [50], Turkey(2.63%) [51], Bahrain [52] (2.63%), Israel(2.63%) [53], the United Arab Emirates (2.63%) [29], Saudi Arabia [54](2.63%), and Switzerland(2.63%) [55]. Additionally, the type of study design included cross-sectional (31.57%), quasi-experimental (15.78%), and qualitative types (23.68%).
Seventy eight management interventions were identified. After combining interventions with similar concepts into one category, the total number of exclusive interventions condensed to twenty seven.
In the next step, the interventions were assigned to four main subcategories including preventive interventions (18.51%) [12, 35, 40, 44, 46, 48, 54, 56] and control interventions (29.62%) [25, 30, 37, 45, 57, 58], as well as interventions at the international (25.92%) [6, 29, 39, 43, 44, 51, 53, 59, 60] and national (25.92%) [10, 16, 25, 30, 46, 49, 51, 57, 61, 62] levels. The details of the included interventions are presented in Table 2.
Table 2.
Effective Interventions in Preventing and Controlling Water Pipe Smoking
| Main Category | Interventions |
|---|---|
| Preventive interventions |
1-Community-based informing interventions [1–4] 2-College-based education [1, 5, 6] 3-Decreasing social acceptability and occasional smoking [4, 7] |
| Control interventions |
1-Controlling WP industry marketing [16] 2-Enforcement of new FDA rules [17] 3-Coordinated enforcement of WPS control in adjacent area [18] 4-Involving policymakers to support executive authority in WPS control [19] 5-Licensing and control of all none-WP activities [18] 6-Reducing youth access to WP locations and products [63] 7-Strong implementation of current legislations [20–22] 8-Using successful experiences of authority in WPS control [18] |
| Enactment and implementation of legislatives and policies on international levels |
1-Monitoring activities of WP industry marketing and designing proper control measures [16, 23] 2-Compulsion of industry to append evidence-base health warning labelling in proper places and sizes in WP device, accessories, and other products [24–27] 3-Developing evidence-based control programs tailored to the needs of new generation [9] 4-Encouraging scientists to develop effective interventions of WP control for policymakers [28] 5-Compulsion of industry to decrease the production of various fruit-flavored and sweet tobaccos [29, 30] 6-Preventing social pages and websites from deceptive advertising [31, 32] |
| Enactment and implementation of legislatives and policies on national levels |
1-Restricting WP settings [12, 19] 2-Determining proper taxation for WP tobacco packs, devices, and all products [27, 63, 64] 3-Monitoring consumption of medical and nursing students and health care professionals for designing control measures [34] 4-Involving health care professionals to cooperate in the WPS control program [35, 36] 5-Offering evidence-based counseling knowledge about WPS control to health professionals [37] 6-Improving quality of training curricula and informing medical sciences students about WPS control [35] 7-Encouraging executive authorities in developing innovative ways of WPS control [17, 18] |
Discussion
In this study, the management interventions affecting the prevention and control of WPS worldwide were identified through a systematic literature review. In this regard, 27 interventions were experienced in the world for WSP control that was categorized into four main themes and four sub-themes.
Preventive interventions
Preventive interventions refer to measures that their focus is on abatement of WPS consumption. Some studies suggested that more evidence and investigations are needed to prevent and control WPS [33, 38, 65, 66]. Lopez et al. found that evidence related to WPS control is very rare, and more investigations and studies are required in this respect [33]. Some other studies were related to the current interventions for the prevention and control of WPS that were incompatible with the various needs of the new generations of adolescents. They are poly-users, occasional and social users, and have fast access to new products via the web [5, 44, 67].
To prevent WPS, most studies focused on school-based educational interventions [68]. In many countries, for first time smoking occures in school students and adolescents [69], and students are considered as the current water pipe smokers [12, 41, 46, 48, 54, 55, 70, 71]. For example, the rapidly growing prevalence of experiencing WPS among younger age groups in Lebanon, is going to be considered as an epidemic phenomena [72, 73]. The younger generations have always been lured by fancy advertisements in the media. There have easy access to water pipe bars and are under the illusion and medical myth that the passage of smoke through the water in water-pipes “purifies” the smoke of all harmful elements [74].
NidalEshah et al. (2017) showed that more than 70% of smokers begin WPS in adolescence [75]. In fact, in many countries, young and adolescents’ easy access to café which are providing water pipe facilitates, make them prone to try WPS out [31]. Studies conducted by Aboaziza (2015), Stamm-Balderjahn (2012), and Tugay (2012) revealed that many adolescents become dependent after the first use of WP, which makes the quitting process extremely hard and the educational programs less effective [12, 19, 76]. Thus, access restriction regulations in the time of licensing and controlling their services can be considered as potential intervention.
Control interventions
Control interventions are activities that try to reduce WPS consumption. The lack of WPS control interventions among students has been reported. Harvey and Phan Thu, P (2016) confirmed that health care professionals have a key role in WPS prevention and control [10, 77]. In a study conducted by Moyer VJP (2013), health care professionals were found to be helping adolescents to change their behavior [78]. On the other hand, Kumar et al.(2015) reported that the prevalence of WPS among health care professionals, especially medical and nursing students [79], can act as a positive vision to WP and cause low motivation to cooperate in WPS control programs [80, 81].
Public education about high-risk behaviors such as WPS was another experienced intervention. Social media, the Internet and mass media are the main factors in promoting or preventing WPS among adolescents.
In recent years, WPS has become a common social behavior and recreation and it is a catering item in many familiar parties. Social acceptance and being an essential part of the family, peer, and public gatherings and café and restaurant culture are highly influential factors contributing to the growth and its popularity. Therefore, exploring the general public’s knowledge and attitude toward WPS is useful in designing and formulating appropriate interventions in controlling WPS [74]. Further, communication and dissemination strategies to facilitate the use of health-related evidence regarding the WPS alongside the role of community health workers, especially in the resource-poor and underprivileged areas of the society and agencies involved in raising public awareness on this issue are essential to be considered [82, 83].
Enactment and implementation of legislatives and policies in international level
According to the study findings, the WHO Framework Convention on Tobacco Control (FCTC) is a global treaty enacting the actions to control all tobacco products [84]. However, controlling cigarettes and WP-specific actions has received less attention among national policies, and it just has been applied in some studies [85, 86]. It has been shown that using the proposed actions by the FCTC to manage WPS can lead to progress in its prevention and control [51].
Despite the WHO FCTC Article [87] on the taxation of all tobacco products, WP products are still tax-exempt. Although, some studies reported the effectiveness of taxation in reducing tobacco smoking [48, 49, 86], cheap or expensive prices may not be effective in WPS [48, 88]. Several studies suggested that executive authorities have main roles in controlling WPS and should be supported by legislative enforcers and policymakers [25, 30, 89].
According to different studies, the lack of proper interventions in WP industry, including packaging, labeling, advertising, fruit-flavored and sweet tobacco, settings, and diversified services can lead to a failure in WPS control programs [6, 29, 30, 43, 44, 59, 60]. Other studies represented that there is a strong relationship between fruit-flavored and sweet WP tobacco products and the expansion of WP use and act as the main barrier for WPS control [90, 91]. Therefore, measures to ban these additives proposed to be considered [6, 92, 93]. Furthermore, previous evidence shows that proper warning labels accompanied by a clear and intelligible packaging can be more effective in controlling WPS [25, 43, 51, 94, 95].
Enactment and implementation of legislatives and policies in national level
Although there are extensive WPS restrictive rules in countries [65], the lack of coordination between the involved organizations and the lack of executive support have led to their inefficiency [96]. Community involvement and advocacy were found among the strongest WPS prevention measures [97, 98]. Moreover, community representatives, local and identical groups, and local community centers advocacy had shown some extend of efficacy as management interventions [99].
Some researchers believe that smoking related harms could not be completely prevented. Therefor harm reduction strategies were proposed in studies [100]. Although, those strategies might be interesting for cigarette, they do not necessarily applicable for hookah [101]. Recently, three harm reduction components (quick-light charcoal, electric heating and bubble diffuser quick-light charcoal and bubble diffuser) have been examined [102], however such strategies are not yet agreed upon and needs some more evidences [100].
Strengths and limitations of the study
Although this study was not aimed to evaluate interventions and provide some information about their efficacy, summarizing the intervention effects across themes would be valuable. However, we could not find well-defined interventional studies using a common evaluation means. Additionally, most found interventions were complex interventions with a variety of components making the synthesis of intervention effects more challenging.
Conclusion
In general, our findings indicated WPS related social and health crisis have not come into attention in high levels of decision making. The current enforced legislations are old, unclear, and incompatible with the needs of the adolescents and are not backed by rigorous evidence. In addition, the WP industry is rapidly expanding without monitoring and controlling measures. Informing and empowering adolescents for those who have not yet experienced smoking is a sensible intervention in this regard. Besides, empowering and involving health students and professionals in WPS control programs can lead to promising results in preventing and controlling WPS. It seems that there is a paucity of evidence regarding strategies on controlling and preventing WTS, thus further research in the society is warranted in this respect.
Supplementary Information
Acknowledgements
This study is part of MSc. thesis in School of Management and Medical Informatics, Tabriz University of Medical Sciences, Tabriz, Iran. The authors express their gratitude to Tabriz University of Medical Sciences for supporting this study.
Abbreviations
- WPS
Water Pipe Smoking
- WP
Water Pipe
- GDP
Gross Domestic Product
- WHO
World Health Organization
- FCTC
Framework Convention on Tobacco Control
Authors’ contributions
GA collected and reviewed the papers and analyzed and prepared the Figs. LD contributed in designing, analyzing, drafting and finalizing the paper. JB contributed in categorizing of factors, developing the framework, and reviewing. AA analyzed and critically revised the manuscript for important intellectual content. All authors read and approved the final version of the paper.
Funding
The research has not received any financial grant from any organization or funding agency.
Availability of data and materials
All of the included papers are available in PubMed, ISI Web of Science, Embase, Scopus, Science Direct, and Ovid databases.
Ethics approval and consent to participate
This study reviewed and approved by Tabriz University of medical Sciences research ethical committee. Ethical code: IR.TBZMED.REC.1397.115.
Consent for publication
Not applicable.
Competing interests
The authors state they have no conflict of interests to declare.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Forouzanfar MH, Afshin A, Alexander LT, Anderson HR, Bhutta ZA, Biryukov S, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the global burden of disease study 2015. Lancet. 2016;388(10053):1659–1724. doi: 10.1016/S0140-6736(16)31679-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Organization WH . WHO report on the global tobacco epidemic 2017: Monitoring tobacco use and prevention policies. 2017. [Google Scholar]
- 3.Organization WH . Control and prevention of waterpipe tobacco products report. Geneva: World Health Organization; 2016. [Google Scholar]
- 4.Meeting WSGoTPR, Organization WH . WHO study group on tobacco product regulation: report on the scientific basis of tobacco product regulation: third report of a WHO study group: World Health Organization. 2009. [PubMed] [Google Scholar]
- 5.Horn K, Pearson JL, Villanti AC. Polytobacco use and the “customization generation”-new perspectives for tobacco control. J Drug Educ. 2016;46(3–4):51–63. doi: 10.1177/0047237917722771. [DOI] [PubMed] [Google Scholar]
- 6.Salloum RG, Maziak W, Hammond D, Nakkash R, Islam F, Cheng X, et al. Eliciting preferences for waterpipe tobacco smoking using a discrete choice experiment: implications for product regulation. BMJ Open. 2015;5(9):e009497. doi: 10.1136/bmjopen-2015-009497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Primack BA, Shensa A, Kim KH, Carroll MV, Hoban MT, Leino EV, et al. Waterpipe smoking among U.S. university students. Nicotine Tobacco Res. 2013;15(1):29–35. doi: 10.1093/ntr/nts076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barnett TE, Curbow BA, Weitz JR, Johnson TM, Smith-Simone SY. Water pipe tobacco smoking among middle and high school students. Am J Public Health. 2009;99(11):2014–2019. doi: 10.2105/AJPH.2008.151225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Akl EA, Gunukula SK, Aleem S, Obeid R, Jaoude PA, Honeine R, et al. The prevalence of waterpipe tobacco smoking among the general and specific populations: a systematic review. BMC Public Health. 2011;11(1):244. doi: 10.1186/1471-2458-11-244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harvey J, Chadi N. Strategies to promote smoking cessation among adolescents. Paediatr Child Health. 2016;21(4):201–208. doi: 10.1093/pch/21.4.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pandey P. Rising popularity of “tobacco-free” hookah among youth: A burgeoning public health challenge for India! International Journal of Noncommunicable Diseases. 2017;2(2):30. [Google Scholar]
- 12.Jawad M, Lee JT, Millett C. Waterpipe tobacco smoking prevalence and correlates in 25 eastern Mediterranean and eastern European countries: cross-sectional analysis of the global youth tobacco survey. Nicotine Tob Res. 2015;18(4):395–402. doi: 10.1093/ntr/ntv101. [DOI] [PubMed] [Google Scholar]
- 13.Stamm-Balderjahn S, Groneberg DA, Kusma B, Jagota A, Schonfeld N. Smoking prevention in school students: positive effects of a hospital-based intervention. Dtsch Arztebl Int. 2012;109(44):746–752. doi: 10.3238/arztebl.2012.0746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arrazola RA, Singh T, Corey CG, Husten CG, Neff LJ, Apelberg BJ, et al. Tobacco use among middle and high school students—United States, 2011–2014. MMWR Morb Mortal Wkly Rep. 2015;64(14):381. [PMC free article] [PubMed] [Google Scholar]
- 15.Barnett TE, Tomar SL, Lorenzo FE, Forrest JR, Porter L, Gurka MJ. Hookah use among Florida high school students, 2011-2014. Am J Prev Med. 2017;52(2):220–223. doi: 10.1016/j.amepre.2016.10.027. [DOI] [PubMed] [Google Scholar]
- 16.Shishani K, Nawafleh H, Jarrah S, Froelicher ES. Smoking patterns among Jordanian health professionals: a study about the impediments to tobacco control in Jordan. Eur J Cardiovasc Nurs. 2011;10(4):221–227. doi: 10.1016/j.ejcnurse.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 17.Jawad M, Wilson A, Lee JT, Jawad S, Hamilton FL, Millett C. Prevalence and predictors of water pipe and cigarette smoking among secondary school students in London. Nicotine Tobacco Res. 2013;15(12):2069–2075. doi: 10.1093/ntr/ntt103. [DOI] [PubMed] [Google Scholar]
- 18.Kumar A, Baig S, Raif A. Comparison of knowledge attitude and practice of shisha use among medical students and pharmacy students. Eur Respir J. 2015;46.
- 19.Aboaziza E, Eissenberg T. Waterpipe tobacco smoking: what is the evidence that it supports nicotine/tobacco dependence? Tob Control. 2015;24(Suppl 1):i44–i53. doi: 10.1136/tobaccocontrol-2014-051910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bou Fakhreddine HM, Kanj AN, Kanj NA. The growing epidemic of water pipe smoking: health effects and future needs. Respir Med. 2014;108(9):1241–1253. doi: 10.1016/j.rmed.2014.07.014. [DOI] [PubMed] [Google Scholar]
- 21.Waziry R, Jawad M, Ballout RA, Al Akel M, Akl EA. The effects of waterpipe tobacco smoking on health outcomes: an updated systematic review and meta-analysis. Int J Epidemiol. 2017;46(1):32–43. doi: 10.1093/ije/dyw021. [DOI] [PubMed] [Google Scholar]
- 22.Rezaei S, Sari AA, Arab M, Majdzadeh R, Poorasl AM. Economic burden of smoking: a systematic review of direct and indirect costs. Med J Islam Repub Iran. 2016;30:397. [PMC free article] [PubMed] [Google Scholar]
- 23.Xu X, Bishop EE, Kennedy SM, Simpson SA, Pechacek TF. Annual healthcare spending attributable to cigarette smoking: an update. Am J Prev Med. 2015;48(3):326–333. doi: 10.1016/j.amepre.2014.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Buice ME. Smoke signals: an analysis of policies to reduce hookah use among adolescents in Washington state. 2015. [Google Scholar]
- 25.Jawad M. Legislation enforcement of the waterpipe tobacco industry: a qualitative analysis of the London experience. Nicotine & tobacco research. 2014;16(7):1000–1008. doi: 10.1093/ntr/ntu022. [DOI] [PubMed] [Google Scholar]
- 26.Martinasek MP, McDermott RJ, Martini L. Waterpipe (hookah) tobacco smoking among youth. Curr Probl Pediatr Adolesc Health Care. 2011;41(2):34–57. doi: 10.1016/j.cppeds.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 27.Hammal F, Wild TC, Nykiforuk C, Abdullahi K, Mussie D, Finegan BA. Waterpipe (hookah) smoking among youth and women in Canada is new, not traditional. Nicotine and Tobacco Research. 2016;18(5):757–762. doi: 10.1093/ntr/ntv152. [DOI] [PubMed] [Google Scholar]
- 28.McKelvey K, Attonito J, Madhivanan P, Jaber R, Yi Q, Mzayek F, et al. Determinants of waterpipe smoking initiation among school children in Irbid, Jordan: a 4-year longitudinal analysis. Drug Alcohol Depend. 2014;142:307–313. doi: 10.1016/j.drugalcdep.2014.06.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Joudrey PJ, Jasie KA, Pykalo L, Singer T, Woodin MB, Sherman S. The operation, products and promotion of waterpipe businesses in new York City, Abu Dhabi and Dubai. East Mediterr Health J. 2016;22(4):237–243. doi: 10.26719/2016.22.4.237. [DOI] [PubMed] [Google Scholar]
- 30.Kassem NOF, Jackson SR, Boman-Davis M, Kassem NO, Liles S, Daffa RM, et al. Hookah smoking and facilitators/barriers to lounge use among students at a US university. Am J Health Behav. 2015;39(6):832–848. doi: 10.5993/AJHB.39.6.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Maziak W, Taleb ZB, Bahelah R, Islam F, Jaber R, Auf R, et al. The global epidemiology of waterpipe smoking. Tob Control. 2015;24:i3–i12. doi: 10.1136/tobaccocontrol-2014-051903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maziak W. The global epidemic of waterpipe smoking. Addict Behav. 2011;36(1–2):1–5. doi: 10.1016/j.addbeh.2010.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lopez AA, Eissenberg T, Jaafar M, Afifi R. Now is the time to advocate for interventions designed specifically to prevent and control waterpipe tobacco smoking. Addict Behav. 2017;66:41–47. doi: 10.1016/j.addbeh.2016.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Institute JB. Critical Appraisal tools for use in JBI Systematic Reviews. Checklist for Prevalence Studies Available online: http://joannabriggs.org/research/critical-appraisal-tools.html (accessed on 12 Dec 2019). 2017.
- 35.Lipkus IMPD, Eissenberg TPD, Schwartz-Bloom RDPD, Prokhorov AVMDPD, Levy JPD. Affecting perceptions of harm and addiction among college Waterpipe tobacco smokers. Nicotine Tob Res. 2011;13(7):599–610. doi: 10.1093/ntr/ntr049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Leavens ELS, Meier E, Tackett AP, Miller MB, Tahirkheli NN, Brett EI, et al. The impact of a brief cessation induction intervention for waterpipe tobacco smoking: a pilot randomized clinical trial. Addict Behav. 2018;78:94–100. doi: 10.1016/j.addbeh.2017.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lock K, Adams E, Pilkington P, Duckett K, Gilmore A, Marston C. Evaluating social and behavioural impacts of English smoke-free legislation in different ethnic and age groups: implications for reducing smoking-related health inequalities. Tobacco control. 2010;tc. 2009:032318. doi: 10.1136/tc.2009.032318. [DOI] [PubMed] [Google Scholar]
- 38.O'Neill N, Dogar O, Jawad M, Kanaan M, Siddiqi K. Which Behavior Change Techniques May Help Waterpipe Smokers to Quit? An Expert Consensus Using a Modified Delphi Technique (ntw297, 2016). Nicotine & Tobacco Research. 2017;19(9):1123-. [DOI] [PubMed]
- 39.Jawad M, Darzi A, Lotfi T, Nakkash R, Hawkins B, Akl EA. Waterpipe product packaging and labelling at the 3rd international hookah fair; does it comply with article 11 of the framework convention on tobacco control? J Public Health Policy. 2017;38(3):303–313. doi: 10.1057/s41271-017-0078-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mahoozi S, Heidari M, Shahbazi S, Naseh L. Influence of training about carcinogenic effects of hookah smoking on the awareness, attitude, and performance of women. Asian Pac J Cancer Prev. 2017;18(7):1967–1971. doi: 10.22034/APJCP.2017.18.7.1967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Momenabadi V, Kaveh MH, Hashemi SY. Effect of educational intervention on intention of university students’ disuse of hookah smoking: BASNEF model. J Subst Abus. 2017:1–6.
- 42.Mohlman MK, Boulos DNK, Setouhy ME, Radwan G, Makambi K, Jillson I, et al. A randomized, controlled community-wide intervention to reduce environmental tobacco smoke exposure. Nicotine and Tobacco Research. 2013;15(8):1372–1381. doi: 10.1093/ntr/nts333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mostafa A, Mohammed HT, Hussein WM, Elhabiby M, Safwat W, Labib S, et al. Would placing pictorial health warnings on waterpipe devices reduce waterpipe tobacco smoking? Tob Control: A qualitative exploration of Egyptian waterpipe smokers' and non-smokers' responses; 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mohd Zin F, Hillaluddin AH, Mustaffa J. Adolescents' perceptions regarding effective tobacco use prevention strategies for their younger counterparts: a qualitative study in Malaysia. Asian Pac J Cancer Prev. 2016;17(12):5113–5119. doi: 10.22034/APJCP.2016.17.12.5113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Deshpande A, Kudtarkar P, Dhaware D, Chowgule R. Study of secondhand smoke levels pre and post implementation of the comprehensive smoking ban in Mumbai. Indian J Community Med. 2010;35(3):409–413. doi: 10.4103/0970-0218.69269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rozema AD, Hiemstra M, Mathijssen JJP, Jansen MWJ, van Oers H. Impact of an Outdoor Smoking Ban at Secondary Schools on Cigarettes, E-Cigarettes and Water Pipe Use among Adolescents: An 18-Month Follow-Up. Int J Environ Res Public Health. 2018;15:2. doi: 10.3390/ijerph15020205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Anjum Q, Ahmed F, Ashfaq T. Knowledge, attitude and perception of water pipe smoking (shisha) among adolescents aged 14-19 years. JPMA The Journal of the Pakistan Medical Association. 2008;58(6):312. [PubMed] [Google Scholar]
- 48.Jaam M, Al-Marridi W, Fares H, Izham M, Kheir N, Awaisu A. Perception and intentions to quit among waterpipe smokers in Qatar: a cross-sectional survey. Public Health Action. 2016;6(1):38–43. doi: 10.5588/pha.15.0054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Salti N, Chaaban J, Nakkash R, Alaouie H. The effect of taxation on tobacco consumption and public revenues in Lebanon. Tobacco control. 2013:tobaccocontrol-2012-050703. [DOI] [PubMed]
- 50.Asfar T, Al Ali R, Rastam S, Maziak W, Ward KD. Behavioral cessation treatment of waterpipe smoking: the first pilot randomized controlled trial. Addict Behav. 2014;39(6):1066–1074. doi: 10.1016/j.addbeh.2014.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Erdöl C, Ergüder T, Morton J, Palipudi K, Gupta P, Asma S. Waterpipe tobacco smoking in Turkey: policy implications and trends from the global adult tobacco survey (GATS) Int J Environ Res Public Health. 2015;12(12):15559–15566. doi: 10.3390/ijerph121215004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hamadeh RR, Ahmed J, Al-Kawari M, Bucheeri S. Quit tobacco clinics in Bahrain: Smoking cessation rates and patient satisfaction. Tobacco Induced Diseases. 2017;15:1. doi: 10.1186/s12971-017-0115-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Essa-Hadad J, Linn S, Rafaeli S. A web-based program to increase knowledge and reduce cigarette and nargila smoking among Arab university students in Israel: mixed-methods study to test acceptability. J Med Internet Res. 2015;17(2):e39. doi: 10.2196/jmir.2988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ali Quadri MF, Saleh SM, Alsanosy R, Abdelwahab SI, Tobaigy FM, Maryoud M, et al. Effectiveness of an intervention program on knowledge of oral cancer among the youth of Jazan, Saudi Arabia. Asian Pac J Cancer Prev. 2014;15(5):1913–1918. doi: 10.7314/APJCP.2014.15.5.1913. [DOI] [PubMed] [Google Scholar]
- 55.Tomaszek S, Schuurmans MM, Schneiter D, Weder W, Hillinger S. Smoking prevention intervention with school classes at a university hospital by thoracic surgeon und pulmonologist. Cancer Research. 2014;74:19. doi: 10.1016/j.pmedr.2022.101964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Riggs NR, Pentz MA. Inhibitory control and the onset of combustible cigarette, e-cigarette, and hookah use in early adolescence: the moderating role of socioeconomic status. Child Neuropsychol. 2016;22(6):679–691. doi: 10.1080/09297049.2015.1053389. [DOI] [PubMed] [Google Scholar]
- 57.Freiberg M. Options for state and local governments to regulate non-cigarette tobacco products. Ann Health Law. 2012;21(2):407-45. [PubMed]
- 58.Highet G, Ritchie D, Platt S, Amos A, Hargreaves K, Martin C, et al. The re-shaping of the life-world: male British Bangladeshi smokers and the English smoke-free legislation. Ethn Health. 2011;16(6):519–533. doi: 10.1080/13557858.2011.578734. [DOI] [PubMed] [Google Scholar]
- 59.Islam F, Salloum RG, Nakkash R, Maziak W, Thrasher JF. Effectiveness of health warnings for waterpipe tobacco smoking among college students. Int J Public Health. 2016;61(6):709–715. doi: 10.1007/s00038-016-0805-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Grant A, O'Mahoney H. Portrayal of waterpipe (shisha, hookah, nargile) smoking on twitter: a qualitative exploration. Public Health. 2016;140:128–135. doi: 10.1016/j.puhe.2016.07.007. [DOI] [PubMed] [Google Scholar]
- 61.Kowitt SD, Goldstein AO, Schmidt AM, Hall MG, Brewer NT. Attitudes toward FDA Regulation of newly deemed tobacco products. Tob Regul Sci. 2017;3(4):504–515. doi: 10.18001/TRS.3.4.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.VanDevanter N, Katigbak C, Naegle M, Zhou S, Sherman S, Weitzman M. Nursing education to reduce use of tobacco and alternative tobacco products: change is imperative. J Am Psychiatr Nurses Assoc. 2017;23(6):414–421. doi: 10.1177/1078390317711252. [DOI] [PubMed] [Google Scholar]
- 63.Sepetdjian E, Abdul Halim R, Salman R, Jaroudi E, Shihadeh A, Saliba NA. Phenolic compounds in particles of mainstream waterpipe smoke. Nicotine & tobacco research. 2013;15(6):1107–1112. doi: 10.1093/ntr/nts255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Jawad M, El Kadi L, Mugharbil S, Nakkash R. Waterpipe tobacco smoking legislation and policy enactment: a global analysis. Tob Control. 2015;24(Suppl 1):i60–ii5. doi: 10.1136/tobaccocontrol-2014-051911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Consortium TCL. Regulatory Options for Hookahs and Water Pipes. Tobacco Control Legal Consortium, Washington, DC, http://publichealthlawcenter.org/sites/default/files/pdf/tclc-fs-regulatory-options-hookahs-2013.pdf. 2013.
- 67.Kingsbury JH, Parks MJ, Amato MS, Boyle RG. Deniers and admitters: examining smoker identities in a changing tobacco landscape. Nicotine & tobacco Res. 2016;18(11):2130–2137. doi: 10.1093/ntr/ntw110. [DOI] [PubMed] [Google Scholar]
- 68.Villanti AC, Pearson JL, Cantrell J, Vallone DM, Rath JM. Patterns of combustible tobacco use in U.S. young adults and potential response to graphic cigarette health warning labels. Addict Behav. 2015;42:119–125. doi: 10.1016/j.addbeh.2014.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Crone M, Reijneveld S, Willemsen M, Van Leerdam F, Spruijt R, Sing RH. Prevention of smoking in adolescents with lower education: a school based intervention study. J Epidemiol Community Health. 2003;57(9):675–680. doi: 10.1136/jech.57.9.675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Smith DM, Bansal-Travers M, Huang JD, Barker D, Hyland AJ, Chaloupka F. Association between use of flavoured tobacco products and quit behaviours: findings from a cross-sectional survey of US adult tobacco users. Tobacco Control. 2016;25:ii73–ii80. doi: 10.1136/tobaccocontrol-2016-053313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Little MA, Talcott GW, Bursac Z, Linde BD, Pagano LA, Messler EC, et al. Efficacy of a brief tobacco intervention for tobacco and nicotine containing product use in the US air force. Nicotine & tobacco Res. 2016;18(5):1142–1149. doi: 10.1093/ntr/ntv242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Jawad M, Charide R, Waziry R, Darzi A, Ballout RA, Akl EA. The prevalence and trends of waterpipe tobacco smoking: a systematic review. PLoS One. 2018;13(2):e0192191. doi: 10.1371/journal.pone.0192191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Farah R, Haddad C, Sacre H, Hallit S, Salameh P. Knowledge and attitude toward waterpipe smoking: scale validation and correlates in the Lebanese adult population. Environ Sci Pollut Res Int. 2020. [DOI] [PubMed]
- 74.Yadav S, G. R. Waterpipe Tobacco Smoking: A Mini-review. J Translational Int Med 2018;6:173–175. [DOI] [PMC free article] [PubMed]
- 75.Nidal Eshah NF, Froelicher ES. Understanding hookah smoking behaviors among non current cigarettes smokers: implications for prevention programs. Eur J Prev Cardiol. 2017;24(1):S129. [Google Scholar]
- 76.Tugay BU, Ilhan B, Çatak T. Kabakc¸i T, Koc¸ H, Tugay N. what do the adolescents think about smoking and ban strategies in Turkey? Eur Respir J. 2012;40.
- 77.Phan Thu P, Ngo Quy C, Vu Van G, Pham Le Q. Evaluate the demands for smoking cessation services of smokers at the outpatient departement of Bach Mai Hospital. Respirology. 2016;21:69. doi: 10.1111/resp.12754_19. [DOI] [PubMed] [Google Scholar]
- 78.Moyer VA. Primary care interventions to prevent tobacco use in children and adolescents: US preventive services task force recommendation statement. Ann Intern Med. 2013;159(8):552–557. doi: 10.7326/0003-4819-159-8-201310150-00697. [DOI] [PubMed] [Google Scholar]
- 79.Arshad A, Matharoo J, Arshad E, Sadhra SS, Norton-Wangford R, Jawad M. Knowledge, attitudes, and perceptions towards waterpipe tobacco smoking amongst college or university students: a systematic review. BMC Public Health. 2019;19(1):439. doi: 10.1186/s12889-019-6680-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kumar A, Ghazal S, Malik M, Rizvi N, Ismail S. Knowledge attitudes and practices of shisha smoking among medical practitioners in Karachi. Pakistan Journal of Smoking Cessation. 2015;10(1):44–49. doi: 10.1017/jsc.2013.29. [DOI] [Google Scholar]
- 81.Mughal F, Rashid A, Jawad M. Tobacco and electronic cigarette products: awareness, cessation attitudes, and behaviours among general practitioners. Prim Health Care Res Dev. 2018:1–5. [DOI] [PMC free article] [PubMed]
- 82.Yadav S, Rawal G. Healthcare information for all-Is it achievable. Int J Sci Res Rev. 2015;4:101–105. [Google Scholar]
- 83.Yadav S. G. R. role of integrating community health workers in achieving healthcare information for all. Int J Sci Res Rev. 2015;4:106–110. [Google Scholar]
- 84.World HEalth Organization framework convention on tobacco control. WHO Regional Office for South-East Asia: WHO; 2004.
- 85.Advisory note: waterpipe tobacco smoking: health effects, research needs and recommended actions by regulators. Regulation WSGoTP. 2005. [DOI] [PMC free article] [PubMed]
- 86.Zaatari GS, Bazzi A. Impact of the WHO FCTC on non-cigarette tobacco products. Tob Control. 2019;28(Suppl 2):s104–12. doi: 10.1136/tobaccocontrol-2018-054346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.World Health Organization. WHO Framework Convention on Tobacco Control. 2003.Available in: https://apps.who.int/iris/bitstream/handle/10665/42811/9241591013.pdf?sequence=1, Access date: 1 Nov 2020.
- 88.Maziak W, Nakkash R, Bahelah R, Husseini A, Fanous N, Eissenberg T. Tobacco in the Arab world: old and new epidemics amidst policy paralysis. Health Policy Plan. 2014;29(6):784–794. doi: 10.1093/heapol/czt055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Morris DS, Fiala SC, Pawlak R. Opportunities for policy interventions to reduce youth hookah smoking in the United States. Prev Chronic Dis. 2012;9:E165. doi: 10.5888/pcd9.120082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Regulation TP. Waterpipe tobacco smoking: health effects. Research Needs and Recommended Actions by Regulators. [DOI] [PMC free article] [PubMed]
- 91.Ben Taleb Z, Breland A, Bahelah R, Kalan ME, Vargas-Rivera M, Jaber R, et al. Flavored versus nonflavored waterpipe tobacco: a comparison of toxicant exposure, puff topography, subjective experiences, and harm perceptions. Nicotine and Tobacco Research. 2019;21(9):1213–1219. doi: 10.1093/ntr/nty131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Villanti AC, Johnson AL, Ambrose BK, Cummings KM, Stanton CA, Rose SW, et al. Flavored tobacco product use in youth and adults: findings from the first wave of the PATH study (2013–2014) Am J Prev Med. 2017;53(2):139–151. doi: 10.1016/j.amepre.2017.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Smith-Simone S, Maziak W, Ward KD, Eissenberg T. Waterpipe tobacco smoking: knowledge, attitudes, beliefs, and behavior in two U.S. samples. Nicotine & tobacco research. 2008;10(2):393–398. doi: 10.1080/14622200701825023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Roskin J, Aveyard P. Canadian and English students' beliefs about waterpipe smoking: a qualitative study. BMC Public Health. 2009;9:10. doi: 10.1186/1471-2458-9-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Jawad M, Bakir A, Ali M, Grant A. Impact of waterpipe tobacco pack health warnings on waterpipe smoking attitudes: a qualitative analysis among regular users in London. Biomed Res Int. 2015;2015. [DOI] [PMC free article] [PubMed]
- 96.Jawad M, Jawad S, Waziry RK, Ballout RA, Akl EA. Interventions for waterpipe tobacco smoking prevention and cessation: a systematic review. Sci Rep. 2016;25872. [DOI] [PMC free article] [PubMed]
- 97.Gezer T, Dagli E, Yildiz F, Elbek O. Analysis of tobacco control in Turkey through political mapping. Eur Respir J. 2016;48.
- 98.Khayatzadeh-Mahani A, Breton E, Ruckert A, Labonte R. Banning shisha smoking in public places in Iran: an advocacy coalition framework perspective on policy process and change. Health Policy Plan. 2017;32(6):835–846. doi: 10.1093/heapol/czx015. [DOI] [PubMed] [Google Scholar]
- 99.Danaei M, Jabbarinejad-Kermani A, Mohebbi E, Momeni M. Waterpipe tobacco smoking prevalence and associated factors in the southeast of Iran. Addiction & health. 2017;9(2):72. [PMC free article] [PubMed] [Google Scholar]
- 100.Dawson A, Verweij M. No smoke without fire: harm reduction, E-cigarettes and the smoking endgame. Public Health Ethics. 2017;10(1):1–4. doi: 10.1093/phe/phx003. [DOI] [Google Scholar]
- 101.Chaouachi K. Harm reduction techniques for hookah (shisha, narghile, "water pipe") smoking of tobacco based products. Med Hypotheses. 2009;73(4):623–624. doi: 10.1016/j.mehy.2009.06.016. [DOI] [PubMed] [Google Scholar]
- 102.C Brinkman M, Kim H, S. SB, M Adetona A, M Gordon S, I Clark P. Evidence of compensation among waterpipe smokers using harm reduction components. BMJ,. 2018;29(1). [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All of the included papers are available in PubMed, ISI Web of Science, Embase, Scopus, Science Direct, and Ovid databases.