Abstract
Objective:
To examine the role of executive functioning (EF) in health self-management and the transition to adult health care among college students.
Participants:
A total of 378 undergraduate students from a public university participated in the study.
Methods:
Participants reported on EF, health self-management skills, and their readiness to transition to adult care. Mediation analyses were conducted to evaluate indirect effects of EF on readiness to transition via health self-management skills.
Results:
Students with greater EF difficulties were less ready to transition to adult care. Specific aspects of health self-management (Medication management/Appointment keeping) mediated the relationship between EF and readiness to transition.
Conclusion:
EF is a key developmental aspect of health self-management and transition readiness. Assessing EF strengths/weaknesses in students with suboptimal health self-management skills may provide valuable information for informing the development of individually-tailored transition plans in university health centers, thereby enhancing developmentally appropriate care during the college years.
Keywords: transition, executive functioning, health self-management, health education
There are approximately 18 million 18–21 year olds in the United States,1 the majority of whom will likely transition from pediatric to adult-centered health care settings. Transition to adult health care has been conceptualized as a complex, multi-dimensional and multi-systemic process that involves the gradual acquisition of health self-management skills and the eventual transfer from pediatric to adult care.2 The American Academy of Pediatrics, the American Academy of Family Physicians, and the American College of Physicians have developed practice-level guidelines stressing the conceptual and clinical importance of providing developmentally appropriate care during the transition years for all youth.3 Unfortunately, few youth receive comprehensive transition preparation, and in many cases, chronological age or practical considerations (e.g., moving away to attend college), rather than developmental maturity or skill mastery, is used as a primary marker of youths’ readiness to assume responsibility for their health care and transition to adult care (i.e., transition readiness).4 These are critical issues to consider during the college years given that difficulties assuming responsibility for one’s own health care during this time may set the stage for poor self-management and health problems later in life. Adequate preparation and gradual skill acquisition, on the other hand, can have a profound impact on later health and prevent some of these negative outcomes. A growing body of empirical research has begun to examine neurocognitive factors, such as executive functioning (EF), as key variables that can guide transition efforts in clinical care;4 however, much work remains to be done in this area.
Social-ecological and developmental models of transition have conceptualized EF, a set of higher order neurocognitive skills involved in goal-directed behaviors, as a relevant and developmentally-sensitive factor implicated in youth’s readiness to assume responsibility for their healthcare and transition from pediatric to adult health care.2,4 According to the Social-ecological Model of Transition Readiness,2 neurocognitive factors can impact transition-related processes, including health self-management skills, which in turn may affect youth’s perceptions of their readiness to transition to adult health care providers. Consistent with this theoretical model, neurocognitive factors may facilitate or hinder transition readiness via health self-management skills. For example, difficulties with EF skills such as planning, organizing or working memory, may negatively affect one’s ability to complete important tasks for managing different aspects of health (e.g., remembering to make and attend doctor’s appointments, filling prescription refills, following up on referrals, or reporting on their family’s medical history). These difficulties, in turn, can decrease one’s readiness to transition to adult care. EF is a particularly relevant factor during the college years because brain regions implicated in EF continue to mature during emerging adulthood.5 In addition, college students are expected to assume increasing responsibility for their health care during this developmental period. This is particularly true for college students who are away from their home, their caregivers, and the primary health care provider familiar with their medical history. Further, if a student’s new healthcare provider overestimates EF abilities in their patient, the provider may expect higher levels of health self-management responsibility than the patient may be developmentally ready to assume.
Preliminary empirical evidence has demonstrated that better EF skills are related to better health self-management skills and greater readiness to transition among youth with chronic conditions.6–9 However, no research to date has examined if or how these factors may play a role in the transition preparation of the vast majority of college students who do not have chronic conditions. This question is particularly salient during the college years because students begin to experience not only greater levels of independence in their health self-management and day-to-day functioning, but also many of the stressors associated with young adulthood, which may negatively impact health. Highlighting the importance of this period, recent research demonstrates that college students who do not have a chronic condition have underdeveloped transition readiness skills compared to peers with chronic conditions.10 Moreover, college students without chronic conditions are less likely to work intensively and regularly with physicians to gain health self-management and transition readiness skills. This is due in part to the fact that healthy youth have lower levels of health care utilization11 compared to peers with chronic conditions, which can lead to a poorer understanding of the transition process.12 Better information about the role of EF in the acquisition of health self-management skills and transition readiness among college students could provide health care providers in university health care settings with practical information to guide health care delivery.
Further, although the consequences of poor transition planning are particularly dire for youth with chronic medical conditions,13 continuity of care and access to health care is paramount for individuals across the spectrum of medical needs. As noted by the American Academic of Pediatrics14 “All youth and young adults deserve seamless access to a primary care medical home and any necessary specialty care through all of life’s transitions.” From a prevention/early intervention standpoint, identifying factors that may help us understand students’ readiness to transition to adult care is especially important, as they will become adults who will need to navigate the health care system as their medical needs change. Tasks such as calling the doctor’s office to make an appointment, filling out medical history forms, talking with medical providers, or filling prescription medications for acute illness are all basic health self-management skills that all college students will need to engage in over their lifetime. The college years may be a particularly important period to practice and build mastery of these critical skills. Moreover, from a public health perspective, enhancing transition readiness skills among college students is critical to prevent the onset of major health problems, particularly given the projected increases in the prevalence and cost of medical conditions.15–17
Guided by the existing body of theoretical and empirical literature, the current study aimed to address a critical gap in the health care transition literature by empirically testing how difficulties with EF may function as a barrier to transition readiness via health self-management skills among college students. We hypothesize that: a) greater EF difficulties will act as barriers and be associated with less health self-management skills and less readiness to transition to adult care, and b) health self-management skills will mediate the association between EF and readiness to transition, such that more EF difficulties will relate to lower health self-management skills which, in turn, will be related to poorer readiness to transition.
Materials and Methods
Procedures
All study procedures were approved by the investigators’ Institutional Review Board. Participants were college students at a large, public university in the United States who were invited to participate in the study through an online research pool. Inclusion criteria required that participants were: a) 18–25 years and b) enrolled in an undergraduate psychology course with a research participation requirement. Exclusion criteria included the presence of a self-reported chronic condition. Participants provided informed consent and self-report measures on Qualtrics™, a secure survey system. Participants received research credit towards course completion as compensation for their time.
Participants
Participants included 378 undergraduate students between the ages of 18 to 25 years (M = 19.22 years, SD = 1.28) and most identified as White/Caucasian (68%) and female (73%). The majority of participants (52%) were in their first year of college. Detailed demographic information is presented in Table 1.
Table 1.
Demographic Information
| Variable | N (Percent of Sample) |
|---|---|
| Sex | |
| Male | 104 (28%) |
| Female | 274 (72%) |
| Race/Ethnicity | |
| White/Caucasian | 256 (68%) |
| Black/African-American | 34 (9%) |
| Asian | 59 (16%) |
| Hispanic | 13 (3%) |
| Multiracial/Other | 16 (4%) |
| College Student Income | |
| $999 or less | 98 (26%) |
| $1,000–$2,999 | 89 (24%) |
| $3,000–$4,999 | 69 (19%) |
| $5,000–$9,999 | 61 (16%) |
| Over $10,000 | 56 (15%) |
| Family Income | |
| $0–$49,999 | 51 (14%) |
| $50,000–$99,999 | 89 (24%) |
| $100,000–$149,999 | 67 (18%) |
| $150,000–$199,999 | 46 (12%) |
| $200,000 or more | 68 (18%) |
| Unknown/Missing | 58 (14%) |
| Relationship Status | |
| Single, Never Married | 241 (64%) |
| Dating, Not Married | 133 (35%) |
| Married/Committed Partnership/Other |
4 (1%) |
| Transfer Status | |
| Pediatrician | 163 (44%) |
| Adult Provider | 204 (56%) |
| Health Insurance | |
| Private Insurance/Tricare | 295 (78%) |
| Medicare/Medicaid | 54 (14.3%) |
| Student Health Insurance | 28 (7.4%) |
| No Insurance | 19 (5%) |
| Year in College | |
| 1st | 196 (52%) |
| 2nd | 85 (22%) |
| 3rd | 46 (12%) |
| 4th | 40 (11%) |
| >5th | 11 (3%) |
Measures
Executive Functioning
EF was assessed using the Behavior Rating Inventory of Executive Function-Adult Version (BRIEF-A)18, a 75-item measure designed to assess both the behavioral regulation (e.g., inhibition, shifting, emotional control, self-monitor) and metacognitive (e.g., initiation, working memory, planning/organization, task monitoring, organization of materials) aspects of EF. Items are rated on a 3-point Likert scale (e.g., from 1 = Never to 3 = Often). Scores on each item were summed to create the Global Executive Composite score and converted to age- and gender-matched T-Scores (M = 49.04, SD = 11.44). T-scores at or above 65 are considered clinically significant by the measure developers,18 indicating significant deficits in EF skills. Internal consistency was excellent (Cronbach’s α = .97).
Health Self-Management
Participants reported on their knowledge and ability to complete different skills required to manage their health care needs using the Transition Readiness Assessment Questionnaire (TRAQ).19 The 20-item measure asks participants’ to describe their ability to manage various health care tasks (e.g., “Do you fill a prescription when you need to?” “Do you call the doctor’s office to make an appointment?” “Do you know what your health insurance covers?”). Items are rated on a 5-point Likert scale (e.g., 1 = No, I don’t know how to 5 = Yes, I always do this when I need to). The four subscales included in the study were Managing Medications (M = 3.93, SD = .99, α = .81), Appointment Keeping (M = 3.55, SD = .83, α = .83), Tracking Health Issues (M = 3.82, SD = .85, α = 64), and Talking with Health Care Providers (M = 4.70, SD = .66, α = .87). Higher scores represent greater perceived abilities to manage health care tasks.
Transition Readiness
Transition readiness was assessed with the Readiness for Transition Questionnaire (RTQ).20 In contrast to the TRAQ, this measure did not assess health self-management, but rather participants’ perceptions of their overall readiness to assume complete responsibility for their health care and transition to adult care. Higher scores indicate greater perceived readiness to assume complete responsibility for their care, indicating greater transition readiness. Items are rated on a 4-point Likert scale. Of note, the wording of the response options for this item was slightly modified in the current study to increase the relevance of response options for all participants. While the original measure employs a 4-point Likert scale ranging from “1-Not at all ready” to “4-Completely ready,” we divided the last response into two response options to capture high levels of responsibility with greater granularity (i.e., “4-Completely ready but my parents are still responsible for my health care in some ways” and “5-I already assume complete responsibility for my health care”). In keeping with the original format of the measure, and given that (1) the 4- and 5-point response items conceptually reflect similar levels of transition readiness, and (2) a similar proportion of participants who endorsed the 4- and 5-point responses had transferred to adult care (62% and 58% respectively), these responses were collapsed back to the original format for analyses (M = 2.42, SD = .98).
Statistical Analyses
Statistical analyses were conducted using IBM Statistical Package for the Social Sciences, version 24 IBM.21 Preliminary analyses examined descriptive statistics for the main study variables and correlations between these variables and several demographic factors. Bivariate correlations examined relations between EF, health self-management skills, and transition readiness.
Mediation analyses evaluated indirect effects of EF on transition readiness via health self-management abilities. All models were analyzed using PROCESS22 model 4 with 5,000 bootstrapped 95% confidence intervals. EF was the independent variable, the four TRAQ domains were parallel mediators (i.e., the TRAQ subscales were entered as mediators simultaneously), and transition readiness was the dependent variable. In parallel mediation models run in PROCESS, mediators are not assumed to be independent (Hayes, 2013). Significant mediation was indicated when the 95% confidence intervals for the indirect effects did not include zero. Significant Kolmogorov-Smirnov tests across the main study variables suggested non-normality. Bootstrapping, as was used in the present mediation analyses, is optimal for dealing with non-normal data as it does not make assumptions about the shape of the distributions of the variables (e.g., Preacher & Hayes, 2004).
Results
Preliminary Analyses
A total of 40 (11%) students endorsed global EF skill deficits that were in the clinical range. Both age and transfer status (i.e., whether transfer to adult care had occurred) were significantly and positively correlated with transition readiness (r = .14, p < .01, r = .14, p < .01), such that older participants who had transferred to an adult provider reported higher transition readiness. These demographic variables were also significantly associated with domains of health self-management skills. Specifically, age was positively associated with appointment keeping (r = .13, p < .05) and transfer status was also positively associated with appointment keeping (r = .15, p < .01), as well as with tracking health issues (r = .10, p < .05) and talking with providers (r = .11, p < .05). Sex was associated with all health self-management domains, such that females endorsed higher skills in managing medications (r = .22, p < .001), appointment keeping (r = .11, p < .05), tracking health issues (r = .27, p < .001), and talking with providers (r = .16, p < .01). Based on these significant associations, transfer status, age, and sex were used as covariates in mediation analyses.
Is EF Related to Health Self-Management and Transition Readiness?
EF skills were negatively correlated with all health self-management subscale scores, with effect sizes in the small range. Specifically, more EF difficulties were associated with lower abilities to manage medications (r = −.16; p < .01), keep appointments (r = −.21; p < .001), track health issues (r = −.16; p < .01), and talk with providers (r = −.16; p < .01). More EF difficulties were also associated with less transition readiness (r = −.21; p < .001).
Is EF Indirectly Related to Transition Readiness through Health Self-Management Skills?
As illustrated in Figure 1, medication self-management and appointment keeping mediated the relationship between EF and transition readiness, such that greater deficits in EF skills were indirectly related to lower levels of transition readiness via less health self-management skills in the domains of medication taking, (b = −.002, SE = .001, 95% CI[−.005, −.001]), and appointment keeping, (b = −.005, SE = .002, 95% CI[−.009, −.002]). Effect sizes ranged from small to medium. No significant indirect effects were found for health tracking, (b = −.0002, SE = .001, 95% CI[−.002, .001]), or talking to providers, (b = .0004, SE = .001, 95% CI[−.001, .002]). The direct effect of EF difficulties on transition readiness remained significant after the inclusion of mediators (b = −.01, SE = .004, t = −2.75, p<.01, 95% CI[−.02, −.003]), indicating partial mediation with an effect size in the small range. The model with EF, all mediator variables, and covariates accounted for 22% of the variance in transition readiness (F(8, 368) = 13.14, p < .001).
Figure 1.
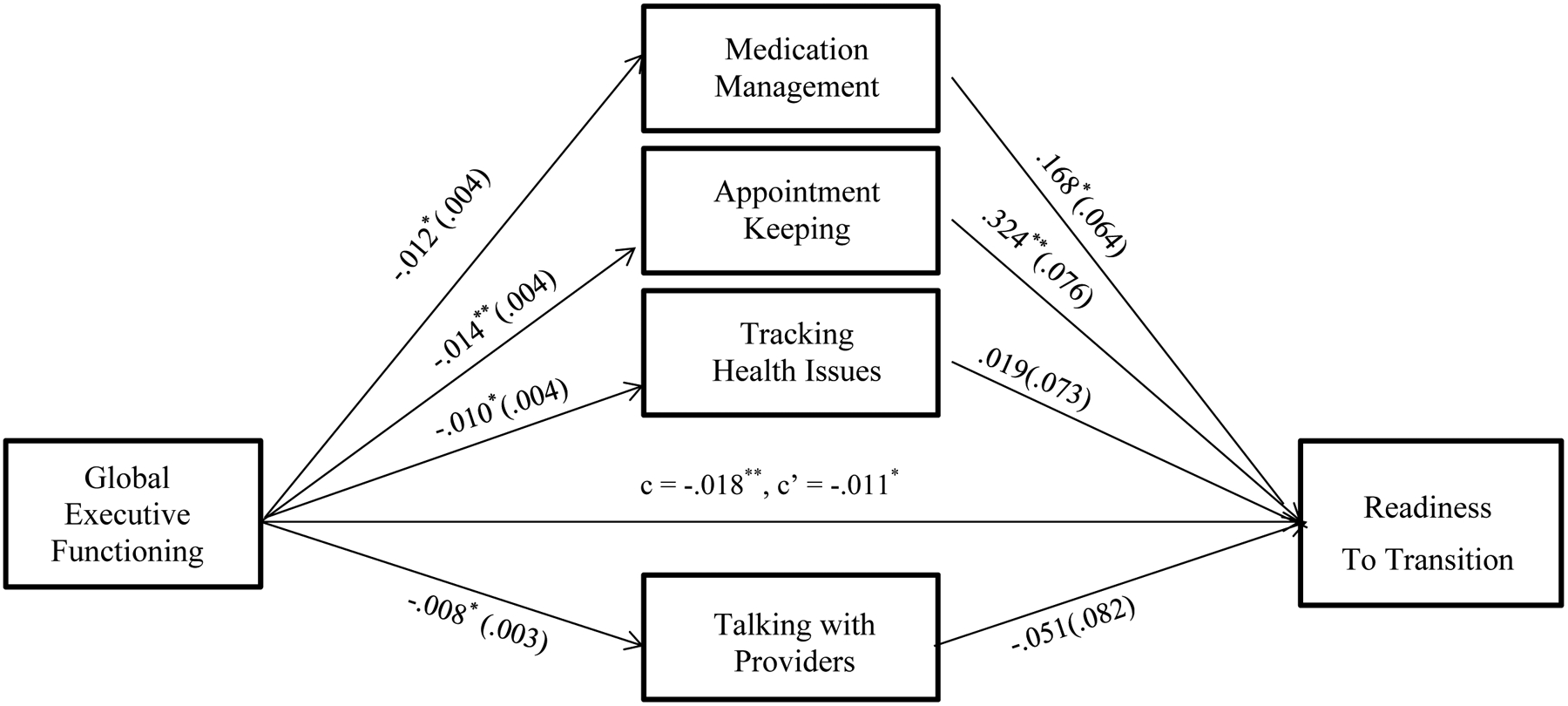
Theorized model of how executive functioning relates to transition readiness via healthcare self-management skills among college students. Path values represent unstandardized coefficients, with standard errors in parentheses. The c represents the total effect and c’ represents the direct effect. *p < .01; **p < .001. The model with EF, all mediator variables, and covariates accounted for 22% of the variance in transition readiness (F(8, 368) = 13.14, p < .001). Post-hoc analyses were also conducted to evaluate the role of EF subcomponents (metacognitive and behavioral regulation domains) on self-management and transition readiness. These analyses demonstrated an identical pattern of results (see Supplemental figures S1 and S2).
Discussion
Medical care that takes into account individuals’ developmental competencies has been recognized as a key aspect in the implementation of patient-centered medical homes across the lifespan, particularly during the vulnerable transition period of the college years. Despite ongoing efforts by the medical and health care community, including the American Academy of Pediatrics, the American Academy of Family Physicians, the American Academy of College Physicians, and the American Osteopathy Association23, most emerging adults receive limited transition preparation and poor integration into adult health care. College students who do not have a chronic condition demonstrate greater deficits in health self-management skills relative to peers with chronic conditions,10 making them a particularly vulnerable group. The current study builds upon existing models of transition readiness2–4 by addressing a critical gap in the literature and testing an empirical model of how EF may influence transition readiness through health self-management skills in a sample of college students without a chronic condition. The findings highlight potential areas of early intervention work for enhancing self-management skills and transition readiness among emerging adults attending college.
Approximately 11% of the current sample had clinically significant deficits in global EF (e.g., organization, planning, emotional control and self-monitoring), which is similar to existing research involving college samples.24 The functional role that mild to significant EF deficits may have in college students’ ability to acquire the health self-management skills necessary for health care independence was confirmed by demonstrating that EF difficulties were negatively associated with all domains of health self-management skills. Specifically, students with greater EF difficulties were at risk for having less competency carrying out medical recommendations, keeping scheduled medical appointments, tracking health issues, and communicating with medical providers. Findings from the current study highlight that for those students who are struggling with health self-management, the assessment of EF skills may provide a more nuanced understanding of the challenges and vulnerabilities that may be contributing to their difficulties with completing health care tasks. Assessing EF in routine health care appointments (e.g., annual well visits) may provide key information about specific aspects of executive functioning (e.g., planning ahead, organization) that need to be targeted to promote health self-management during the college years, a critical time for developing and increasing medical independence.
College students with more EF difficulties also reported less readiness to transition and assume complete responsibility for their health care. These outcomes are consistent with models of transition readiness that highlight EF as an important developmental factor in promoting transition readiness2,4 and replicate empirically documented associations between EF and health self-management in youth with chronic medical conditions.6–9 Mediation analyses further demonstrated that both medication management and appointment keeping, which includes issues related to health insurance management, are two potential mechanisms through which EF is associated with students’ ratings of their readiness to transition to adult care. It is possible that college students perceive medication management and appointment keeping as the primary health self-management skills needed to prepare for the transition to adult care, which coincides with the strong emphasis placed on these domains in clinical practice. Differential results by health self-management domain highlight the importance of considering health self-management skills in particular domains (e.g., medication management) in order to better understand the specific mechanisms through which EF may promote or hinder students’ readiness to transition. Further, the fact that partial mediation was found supports the robust direct relation between EF and readiness to transition to adult providers.
These results additionally demonstrate that although healthy college students are expected to have fewer immediate health care demands, when inevitably faced with future medical needs and responsibilities during college and beyond, those with difficulties in EF may struggle to complete recommended medical tasks and navigate the adult health care system. Individuals exhibiting difficulties with working memory, for example, may attempt to remember important information provided during a medical visit but forget to ask relevant questions when given the opportunity. This may negatively affect health care knowledge acquisition. Similarly, those with organization and planning difficulties may face challenges keeping a list of medical appointments or fail to pick up prescribed medications for acute illnesses in a timely manner, thereby hindering their ability to develop health care independence and foster optimal health. Both metacognitive (e.g., planning/organizing) and behavioral regulation (e.g., inhibition) domains of EF have been linked to health self-management and transition readiness,8 highlighting the importance of considering EF as a global neurocognitive construct when screening for EF difficulties. This type of assessment may provide valuable information that is not readily accessible with traditional health self-management assessments. Following a positive screen, more in depth assessment of EF subdomains would help providers identify specific EF weaknesses. Sequential screening such as this would minimize stakeholder burden, while facilitating individually tailored care that targets identified weaknesses in EF. This kind of personalized care is critical to minimize the dire consequences of poor transition planning,13 and reduce the likelihood that these emerging adults will develop chronic health problems after the college years.
Despite the novelty of these findings, a number of important limitations should be noted. Our investigation used self-report data from a single reporter, and assessed perceived abilities in health self-management rather than actual behavior. As a result, ratings of self-perceived ability may not accurately capture actual behavioral performance in self-management, but rather students’ confidence in their ability to complete health self-management tasks. Future investigations should incorporate objective assessments of self-management behaviors (e.g., data on number of medication refills fulfilled), multi-informant reports, and/or ecological momentary assessment methods (e.g., electronic systems for tracking health self-management behaviors via mobile health technology) in order to obtain a more comprehensive and objective picture of the role of EF in the transition process. Additionally, the measure used to assess our dependent variable was originally developed and validated with kidney transplant recipients, although it has been subsequently used in college students with and without chronic conditions.10 This study was cross-sectional, thus precluding our ability to determine causality and leaving open the possibility of alternate ordering of effects, despite theoretical support for the temporal order tested in the current model.4 Further, although hypothesized relationships reached statistical significance, the effect sizes ranged from small to medium. The large sample size of this study, along with the possibility of unscreened chronic conditions (e.g., depression, ADHD) related to EF, may be partially driving these findings. As a result, the present results should be interpreted as preliminary evidence for the relations between EF, health self-management, and transition readiness among medically healthy college students. Lastly, only about 30% of our sample was male and although sex was not related to our primary outcome, it was associated with self-management skills. Thus, although we controlled for sex in our analyses and this breakdown is typical in other studies involving college samples, replication of the current results is needed using more balanced groups to evaluate to robustness of these findings across sexes. Future studies are also needed to evaluate EF as a long-term predictor of health self-management and transition readiness among emerging adults without medical conditions.
Conclusions
Executive functioning is an important neurocognitive factor that can provide health care professionals in university settings with valuable information about the ways in which clinical practice may be tailored to enhance health self-management skills and transition readiness among vulnerable students. By evaluating the contributing role of EF skills to difficulties with health self-management tasks, providers can identify at-risk young adults who may need additional supports to acquire the skills necessary for health independence. The use of short EF screeners (e.g., NIH PROMIS’ Pediatric Cognitive Function measure)25 in students that demonstrate suboptimal health self-management skills may provide new avenues for identifying precursors to problems completing health-related tasks, as well as students who lack readiness to navigate the adult health care system. In addition to sequential screening practices, medical providers working with students who exhibit weaknesses in EF or who are diagnosed with conditions characterized by disruptions in EF skills (e.g., ADHD, learning disabilities, traumatic brain injury) may also benefit from partnering with their behavioral health colleagues. In particular, providers in integrated primary care settings and pediatric psychologists in specialty medical settings can assist with providing targeted guidance and resources aimed at facilitating the acquisition of self-management skills. Environmental modifications, such as alarms, health apps, or automatic medication refills (e.g., for antibiotics or oral contraception), are likely to be helpful for youth with deficits in EF (e.g., difficulties with planning ahead, attention shifting, organization).4 Further, when EF deficits are apparent, providers may model performing challenging behaviors (e.g., creating an appointment calendar) and monitor progress in those domains as students gain greater skill mastery. By considering the ways in which EF difficulties may challenge the progressive acquisition of health self-management skills during the college years, health providers in university settings can facilitate developmentally informed care that takes into consideration the evolving developmental needs and limitations of college students. This approach will not only facilitate the gradual mastery of health self-management skills but also enhance students’ abilities to navigate the adult health care system during the college years and beyond.
Supplementary Material
Table 2.
Mediation Analyses Involving EF, Medication Management, Appointment Keeping, Talking with Providers, and Health Tracking
| Path A | Path B | Path C | Path C’ | Mediated Effect (AXB) | 95% CI for Mediated Effect | |
|---|---|---|---|---|---|---|
| (b, SE) | (b, SE) | (b, SE) | (b, SE) | (b, SE) | ||
| EF—Medication—Transition Readiness | −.01 (.004)* | .17 (0.06)* | −.02 (.004)* | −.01 (.004)* | −.002 (.001)* | −.005, −.001 |
| EF—Appointment—Transition Readiness | −.01 (.004)* | .32 (.08)* | −.02 (.004)* | −.01 (.004)* | −.005 (.002)* | −.009, −.002 |
| EF—Talking—Transition Readiness | −.01 (.003)* | −.05 (.08) | −.02 (.004)* | −.01 (.004)* | .0004 (.001) | −.001, .002 |
| EF—Tracking—Transition Readiness | −.01 (.004)* | .02 (.07) | −.02 (.004)* | −.01 (.004)* | −.0002 (.001) | −.002, .001 |
Note. All path coefficients are unstandardized. Path A = effect of EF on mediator. Path B = effect of mediator on Transition Readiness controlling for EF. Path C = total effect. Path C’ = direct effect of EF on transition readiness. The mediation model includes age, sex, and transfer status as covariates.
path is significant at p<0.05.
Acknowledgements
We would like to thank the research staff and participants who made this study possible.
Funding
The preparation of this manuscript was supported by: Ana Gutierrez-Colina is supported by a T32 fellowship (T32HD068223; PI Kevin Hommel). Molly Davis is supported by a T32 fellowship (T32MH109433; PIs Rinad Beidas and David Mandell).
Footnotes
Declaration of Interest Statement
The authors have no conflicts of interest to report. The authors confirm that the research presented in this article met the ethical guidelines, including adherence to the legal requirements, of the United States. The surveys were designated as exempt from institutional review board review by the University of Georgia Institutional Review Board.
References
- 1.United States Census Bureau. Current Population Survey. 2013; https://www.census.gov/data/tables/2013/demo/foreign-born/cps-2013.html, 2018.
- 2.Schwartz LA, Tuchman LK, Hobbie WL, Ginsberg JP. A social-ecological model of readiness for transition to adult-oriented care for adolescents and young adults with chronic health conditions. Child Care Health Dev. 2011;37(6):883–895. [DOI] [PubMed] [Google Scholar]
- 3.American Academy of P, American Academy of Family P, American College of P, Transitions Clinical Report Authoring Group, White, P, Cooley W. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2018;142(5); e20182587. [DOI] [PubMed] [Google Scholar]
- 4.Reed-Knight B, Blount RL, Gilleland J. The transition of health care responsibility from parents to youth diagnosed with chronic illness: a developmental systems perspective. Fam Syst Health. 2014;32(2):219–234. [DOI] [PubMed] [Google Scholar]
- 5.Blakemore SJ, Choudhury S. Development of the adolescent brain: implications for executive function and social cognition. J Child Psychol Psychiatry. 2006;47(3–4):296–312. [DOI] [PubMed] [Google Scholar]
- 6.Duke DC, Harris MA. Executive function, adherence, and glycemic control in adolescents with type 1 diabetes: a literature review. Curr Diab Rep. 2014;14(10):532. [DOI] [PubMed] [Google Scholar]
- 7.Gutierrez-Colina AM, Eaton CK, Lee JL, et al. Executive Functioning, Barriers to Adherence, and Nonadherence in Adolescent and Young Adult Transplant Recipients. J Pediatr Psychol. 2016;41(7):759–767. [DOI] [PubMed] [Google Scholar]
- 8.Gutierrez-Colina AM, Reed-Knight B, Eaton C, et al. Transition readiness, adolescent responsibility, and executive functioning among pediatric transplant recipients: Caregivers’ perspectives. Pediatr Transplant. 2017;21(3). [DOI] [PubMed] [Google Scholar]
- 9.Miller MM, Rohan JM, Delamater A, et al. Changes in executive functioning and self-management in adolescents with type 1 diabetes: a growth curve analysis. J Pediatr Psychol. 2013;38(1):18–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eaton CK, Davis MF, Gutierrez-Colina AM, LaMotte J, Blount RL, Suveg C. Different demands, same goal: promoting transition readiness in adolescents and young adults with and without medical conditions. Journal of Adolescent Health. 2017;60(6):727–733. [DOI] [PubMed] [Google Scholar]
- 11.Weller WE, Minkovitz CS, Anderson GF. Utilization of medical and health-related services among school-age children and adolescents with special health care needs (1994 National Health Interview Survey on Disability [NHIS-D] Baseline Data). Pediatrics. 2003; 112(3), 593–603. [DOI] [PubMed] [Google Scholar]
- 12.Lebrun-Harris LA, McManus MA, Ilango S., Cyr M, McLellan SB, Mann MY, White PH. Transition Planning Among US Youth With and Without Special Health Care Needs. Pediatrics. 2018; 142(4), e20180194. [DOI] [PubMed] [Google Scholar]
- 13.Gabriel P, McManus M, Rogers K, White P. Outcome Evidence for Structured Pediatric to Adult Health Care Transition Interventions: A Systematic Review. J Pediatr. 2017;188:263–269 e215. [DOI] [PubMed] [Google Scholar]
- 14.American Academy of Pediatrics. Helping Adolescents Transition to Adult Health Care. 2011. https://www.aap.org/en-us/about-the-aap/aap-press-room/Pages/Helping-Adolescents-Transition-to-Adult-Health-Care.aspx
- 15.Boyle JP, Thompson TJ, Gregg EW, Barker LE, Williamson DF. Projection of the year 2050 burden of diabetes in the US adult population: dynamic modeling of incidence, mortality, and prediabetes prevalence. Popul Health Metr. 2010;8:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heidenreich PA, Trogdon JG, Khavjou OA, Butler J., Dracup K, Ezekowitz M,…woo Y.. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123(8):933–944. [DOI] [PubMed] [Google Scholar]
- 17.Zhang P, Zhang X, Brown J, Vistisen D., Sicree R., Shaw J., & Nichols G. Global healthcare expenditure on diabetes for 2010 and 2030. Diabetes research and clinical practice. 2010;87(3):293–301. [DOI] [PubMed] [Google Scholar]
- 18.Roth RM, Isquith PK, & Gioia GA, ed Behavior rating inventory of executive functioning: Adult Version. Lutz, FL: Psychological Assessment Resources Inc.; 2005. [Google Scholar]
- 19.Wood DL, Sawicki GS, Miller MD, et al. The Transition Readiness Assessment Questionnaire (TRAQ): its factor structure, reliability, and validity. Acad Pediatr. 2014;14(4):415–422. [DOI] [PubMed] [Google Scholar]
- 20.Gilleland J, Amaral S, Mee L, Blount R. Getting ready to leave: transition readiness in adolescent kidney transplant recipients. J Pediatr Psychol. 2012;37(1):85–96. [DOI] [PubMed] [Google Scholar]
- 21.IBM SPSS Statistics for Windows [computer program]. Version 24.0. Armonk, NY: 2016. [Google Scholar]
- 22.Hayes AF. An Index and Test of Linear Moderated Mediation. Multivariate Behav Res. 2015;50(1):1–22. [DOI] [PubMed] [Google Scholar]
- 23.American Academy of Family Physicians, American Academy of Pediatrics, American College of Physicians, American Osteopathic Association. Guidelines for Patient-Centered Medical Home (PCMH) Recognition and Accreditation Programs. February, 2011. Accessed August 4, 2018. http://www.acponline.org/running_practice/pcmh/understanding/guidelines_pcmh.pdf.
- 24.Rabin LA, Fogel J, Nutter-Upham KE. Academic procrastination in college students: the role of self-reported executive function. J Clin Exp Neuropsychol. 2011;33(3):344–357. [DOI] [PubMed] [Google Scholar]
- 25.Ader D Developing the Patient-Reported Outcomes Measurement Information System (PROMIS). Medical Care. 2007;45(Suppl 1):S1–S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


