Abstract
An association between animals and volatile anaesthetic requirements has been shown; however, evidence related to the postoperative outcome of human patients is lacking. Our aim was to investigate whether there is a difference in the requirement for sevoflurane among people undergoing gastrointestinal surgery.
We observed 390 adult patients who underwent gastrointestinal surgery with an American Society of Anesthesiologists physical status of I or II with an expected surgery duration of > 2 hours. We used the bispectral index (BIS) to guide the regulation of end-tidal sevoflurane concentration (ETsevo). The mean ETsevo from 20 minutes after endotracheal intubation to 2 hours after the start of surgery was calculated for all patients. Differential sevoflurane requirements were identified according to ETsevo. The BIS, ETsevo, heart rate, mean arterial pressure, dose of sufentanil and cisatracurium, tracheal extubation time, incidence of intraoperative awareness, and incidence of postoperative nausea and vomiting were compared between patients with a low requirement for sevoflurane (group L) and patients with a high requirement for sevoflurane (group H).
The mean ETsevo of the 390 patients was 1.55% ± 0.26%. Based on our definition, patients with an ETsevo of < 1.29% were allocated to the low requirement group (group L; n = 69), while patients with an ETsevo of > 1.81% were allocated to the high requirement group (group H; n = 78). The ETsevo of group L was significantly lower than the ETsevo of group H (1.29% ± 0.014% vs 1.82% ± 0.017%, P < .001). There was no significant difference in the ETsevo, BIS, heart rate, mean arterial pressure, dose of sufentanil and cisatracurium, tracheal extubation time, incidence of intraoperative awareness, and incidence of postoperative nausea and vomiting. The tracheal extubation time in the L group was significantly shorter than that in the H group. No intraoperative awareness occurred.
There was a significant difference in the requirement for sevoflurane in adult patients. The tracheal extubation time in group L was significantly shorter than that in group H.
Keywords: anesthetic requirement, bispectral index, end-tidal anesthetic gas concentration, sevoflurane
1. Introduction
The depth of general anaesthesia during surgery is closely associated with the postoperative recovery of patients. Previous studies have shown that a 21% increase in mortality, a delayed early postoperative recovery, a prolonged hospital stay, wasted anaesthetic, and an increased cost of hospitalization are associated with deep anaesthesia.[1–3] Low anaesthesia increases the risk of intraoperative awareness and adverse cardiovascular events, cerebrovascular events, and stress responses.[4,5] Therefore, it is crucial to identify a means to guide individually anaesthetized patients to improve postoperative recovery and avoid anaesthesia-related complications.
Clinical signs, such as heart rate (HR) and blood pressure, are unreliable when evaluating an anaesthetic depth and preventing intraoperative awareness.[6–8] Moreover, early attempts were made to monitor the depth of anaesthesia using electroencephalography,[9] the entropy index,[10] cerebral oxygen saturation,[11] and end-tidal concentrations of inhaled anaesthetics.[12] However, these indicators have limitations. Fortunately, the bispectral index (BIS) derived from electroencephalography was the first approach introduced into clinical practice to measure the depth of sedation, which was approved by the Food and Drug Administration in the USA.[13,14] BIS values between 40 and 60 indicate an adequate depth of general anaesthesia.[4] Previous studies have shown that the target BIS value range of between 40 and 60 is advocated to prevent anaesthetic awareness while allowing a reduction in the administration of anaesthetic agents.[15,16] Additionally, the BIS correlates with behavioural measures of sedation and anaesthesia in adult clinical utility studies and is recommended as an indicator of consciousness during anaesthesia.[14,17,18] With the development of the processed BIS, it is now possible to individualize the depth of anaesthesia.[2] A previous study identified that the mean end-tidal sevoflurane concentration (ETsevo) is significantly lower in patients with major depressive disorder than in healthy patients undergoing laparoscopic cholecystectomy below the target BIS range of 40 to 60.[19] However, it remains unclear whether there is a difference in the requirement for sevoflurane among different populations, which may affect postoperative outcomes.
Therefore, the present study aimed to screen patients with differential requirements for sevoflurane to further evaluate their early postoperative outcomes and complications, to analyse the differences in ETsevo based on sex, and to investigate the correlation between ETsevo, tracheal extubation time, and HR.
2. Methods
2.1. Participants
The observational study protocol was approved by the Ethics Committee of West China Hospital of Sichuan University (Chengdu, China; No. 78, approved on May 19, 2017) and registered in the Chinese Clinical Trial Registry (ChiCTR-1800014327) on Jan 6, 2018. We observed 390 subjects with an American Society of Anesthesiologists (ASA) physical status of I – II and an age of 18 to 65 years. All subjects provided written informed consent. These subjects underwent elective gastrointestinal surgery with an expected duration of > 2 hours between January 2018 and September 2018 at West China Hospital, Sichuan University. The exclusion criteria were cerebrovascular disease, psychiatric and opioid abuse, known allergy to volatile anaesthetics, severe cardiovascular disease, abnormal liver or kidney function, and a family history of malignant hyperthermia.
2.2. Management of general anaesthesia
No premedication was given to patients. Standard clinical anaesthetic monitoring was performed, including pulse oximetry, 3-lead electrocardiogram, non-invasive arterial blood pressure monitoring, end-tidal partial pressure of carbon dioxide (PETCO2) monitoring, temperature monitoring, and BIS measurement. After preoxygenation with 8 L/min oxygen for approximately 3 minutes, anaesthesia was induced with inhaled sevoflurane, a bolus of sufentanil (0.2 - 0.4 μg/kg), and cisatracurium (0.2 - 0.3 mg/kg). After endotracheal intubation, general anaesthesia was maintained with 50% oxygen balanced with air, the oxygen/air flow was maintained at 2 L/min and PETCO2 was maintained between 35 and 45 mmHg. According to the up and down method,[20] ETsevo was adjusted by turning the volatile tank concentration up or down (0.2%) to maintain the BIS value at 40 - 60, while continuous infusion of sufentanil at a rate of 0.1 - 0.2 μg/kg/h was adjusted according to vital signs. Patients received a bolus of cisatracurium and additional sufentanil according to their clinical requirements during maintenance of anaesthesia. ETsevo was automatically recorded using an anaesthetic gas monitor (M1026B; Philips MedizinSysteme, Boblingen, Germany). Sevoflurane and sufentanil were discontinued approximately 10 - 20 minutes before the end of surgery. The dose of vasoactive drugs, sufentanil and cisatracurium, the surgical method (open surgery vs. laparoscopic surgery), the duration of anaesthesia, the duration of surgery, the tracheal extubation time, and the incidence of postoperative nausea and vomiting were recorded.
All patients were followed up for intraoperative awareness to investigate whether the patient recalled the event during anaesthesia on 3 occasions: before they left the postanaesthesia care unit after surgery; 24 hours after surgery; and 72 hours after surgery. The following questions were asked:
-
(1)
Before you fell asleep, what was the last thing you remember?
-
(2)
What was the first thing you remember after you woke up?
-
(3)
Between these 2 time points, can you remember anything?
-
(4)
Did you dream during the operation?
2.3. Screening cases with differential requirements for sevoflurane
To screen cases with differential requirements for sevoflurane, patients were divided into the high requirement group and the low requirement group. The ETsevo from 20 minutes after endotracheal intubation to 2 hours after the start of surgery (steady state achieved by sevoflurane anaesthesia) was calculated. In all patients, the normal distribution was expressed as the mean ± standard deviation (SD). The high requirement group was defined by an ETsevo of 1 SD higher than the mean. The low requirement group was defined by an ETsevo of 1 SD lower than the mean.
2.4 Differences in the sevoflurane concentration between males and females. The difference and dispersion of ETsevo between males and females (n = 390 in total) were analysed.
2.4. Statistical analysis
Data analysis was performed using SPSS (version 22.0, IBM Corp., Armonk, NY). Normally distributed data are presented as the mean ± SD and were compared using Student's t-test. Categorical data are expressed as numbers and were compared using the chi-squared test. Linear regression analysis was used to determine the relationship between ETsevo and the BIS, mean arterial pressure (MAP), HR, BMI, age, dose of sufentanil and cisatracurium, and tracheal extubation time. In all analyses, statistical significance was accepted as P ≤ .05.
3. Results
3.1. Screening high requirement and low requirement cases
This study included 390 patients (Fig. 1). The ETsevo values of the 390 patients were normally distributed. The mean ETsevo of the 390 patients was 1.55% ± 0.26%. Based on our definition, patients with an ETsevo of < 1.29% were allocated to the low requirement group (group L; n = 69), while patients with an ETsevo of > 1.81% were allocated to the high requirement group (group H; n = 78). The ETsevo of low requirement for sevoflurane (group L) was significantly lower than the ETsevo of group H (1.29% ± 0.014% vs. 1.82% ± 0.017%, P < .001; Fig. 3A). Among the 69 patients in group L, 5 patients had an ETsevo of 0.46 - 0.5 MAC, 12 patients had an ETsevo of 0.51–0.6 MAC, and 26 patients had an ETsevo of 0.61 - 0.7 MAC. Among the 78 patients in group H, 11 patients had an ETsevo > 1.3 MAC (Fig. 2A and B).
Figure 1.
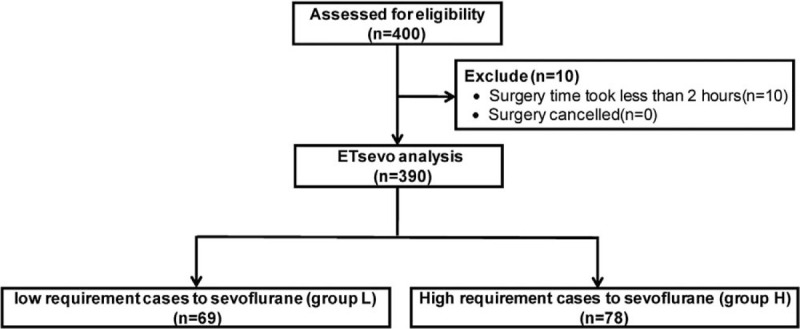
Study enrolment.
Figure 3.
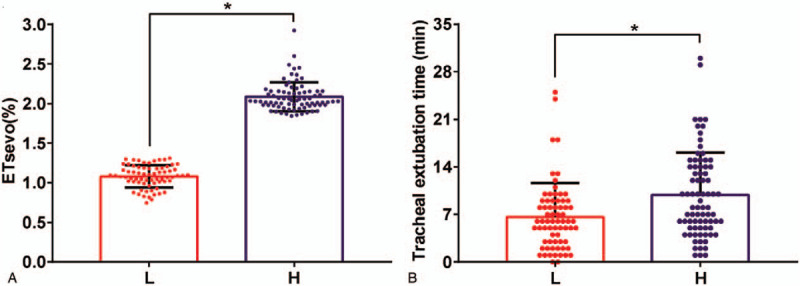
ETsevo (%) and tracheal extubation time in the H group compared with the L group. ∗P < .05.
Figure 2.
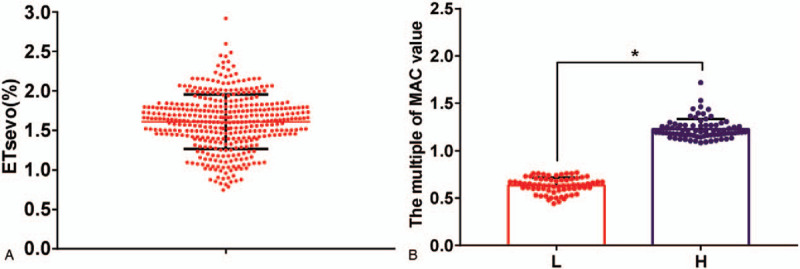
Scatter plot of ETsevo in 390 patients and MAC in the H group and L group. ∗P < .05.
3.2. Patient characteristics
The characteristics of group L and group H are shown in Table 1. The tracheal extubation time in group L was significantly lower than that in group H (6.62 min ± 0.60 min vs. 9.85 min ± 0.71 min, P < .001; Fig. 3B). There was no difference in the BIS in L group and H group (51.52 ± 0.38 vs. 50.66 ± 0.33, P = .087), MAP (P = .071), HR (P = .189), age (51.32 ± 1.10 vs 49.46 ± 1.11) or the open surgery/laparoscopic surgery ratio (69.6% vs 80.8%, P = .115) in L group and H group. Moreover, no significant differences were observed in sex, BMI, ASA grade, dose of sufentanil and cisatracurium, duration of surgery and anaesthesia, usage of nicardipine and esmolol, usage of aramine and ephedrine, and PETCO2 between group L and group H (P > .05). Additionally, no significant difference was observed in the incidence of postoperative nausea and vomiting between group L and group H (P > .296). The follow-up results of 390 patients showed that no intraoperative awareness occurred.
Table 1.
Patient characteristics and intraoperative variables in the L group and H group.
| Characteristics | L group (n = 69) | H group (n = 78) | P-value |
| Age (yr) | 51.32 ± 1.10 | 49.46 ± 1.11 | .219 |
| Gender (Male/Female) | 27/42 | 30/48 | .934 |
| BMI (kg m-2) | 22.35 ± 0.35 | 23.11 ± 0.35 | .129 |
| ASA (I-II) | 2/67 | 2/76 | .901 |
| Surgery (Open/ Laparoscopic) | 48/21 | 63/15 | .115 |
| MAP (mm Hg) | 86.69 ± 1.32 | 83.87 ± 0.88 | .071 |
| HR (Beats/min) | 73.12 ± 0.82 | 74.92 ± 1.12 | .189 |
| PETCO2 (mm Hg) | 34.39 ± 0.41 | 34.04 ± 0.32 | .500 |
| Mean BIS | 51.52 ± 0.38 | 50.66 ± 0.33 | .087 |
| Area under BIS-time curve | 8276.0 ± 145.2 | 8478.8 ± 179.4 | .182 |
| Sufentanil (Induction) (μg) | 20.92 ± 0.47 | 21.44 ± 0.41 | .412 |
| Cis-atracurium (Induction) (mg) | 13.59 ± 0.34 | 13.94 ± 0.24 | .409 |
| Sufentanil (Until to surgery 2 hours) (μg) | 33.39 ± 0.98 | 32.73 ± 0.98 | .633 |
| Cis-atracurium (Until to surgery 2 hours) (mg) | 11.44 ± 0.47 | 11.01 ± 0.42 | .501 |
| Sufentanil (maintenance)(μg) | 46.98 ± 1.70 | 45.05 ± 1.54 | .401 |
| Cis-atracurium (maintenance)(mg) | 15.84 ± 0.78 | 14.94 ± 0.68 | .389 |
| Duration of surgery (min) | 187.9 ± 8.1 | 190.9 ± 8.2 | .793 |
| Duration of anaesthesia (min) | 214.4 ± 9.2 | 218.5 ± 9.0 | .751 |
| Area under ETsevo-time curve (AUC-ETsevo) | 171.6 ± 3.46 | 361.7 ± 6.40∗ | .001 |
| Nicardipine esmolol | 9 | 6 | .285 |
| Aramine ephedrine | 18 | 20 | .951 |
| Postoperative nausea/vomiting | 10 | 7 | .296 |
| Awareness (number) | 0 | 0 | 1.000 |
| Mean ETsevo (%) | 1.079 ± 0.017 | 2.086 ± 0.020∗ | .001 |
| Tracheal extubation time (min) | 6.62 ± 0.60 | 9.85 ± 0.71∗ | .001 |
BIS = bispectral index, BMI = body mass index, ETsevo = end-tidal concentration of sevoflurane., HR = heart rate, MAP = mean arterial pressure, PETCO2 = end-tidal partial pressure of carbon dioxide. Data are presented as the mean ± SD, number (%). Normally distributed data were compared with Student's t-test. Categorical data were compared with the chi-squared test. In all analyses, statistical significance was accepted as P ≤ .05.
P < .05 vs the L group.
3.3. Differences in ETsevo between males and females
Among the 390 patients enrolled in the study, 230 were male and 160 were female. There was no significant difference in ETsevo between male and female patients (1.637% ± 0.266% vs 1.574% ± 0.232%, respectively; P = .863), but there was a significant individual difference in ETsevo for both sexes (coefficient of variation of 16.25% in males and 14.74% in females; Fig. 4).
Figure 4.
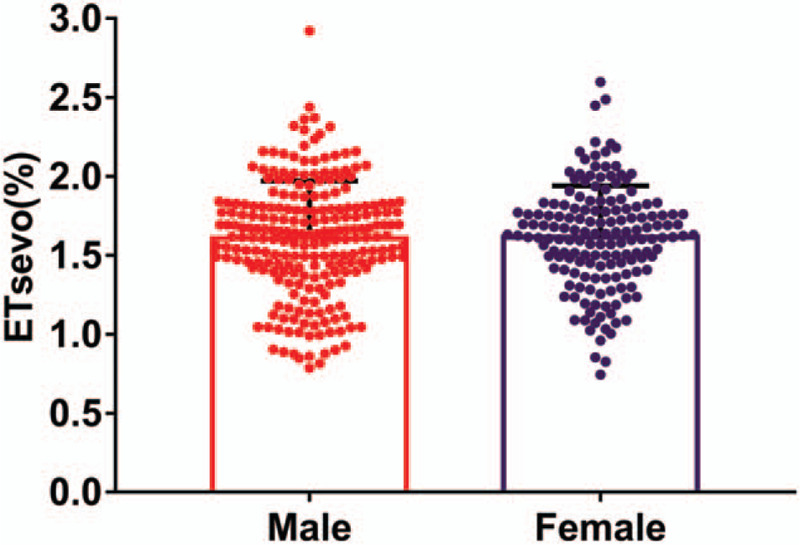
ETsevo of males compared with females.
3.4. Correlation analysis
There was no correlation between ETsevo and the BIS, MAP, age, BMI, or dose of sufentanil and cisatracurium in the steady state. At a significance level of 0.01, ETsevo was positively correlated with HR (R2 = 0.026, P < .001) and tracheal extubation time (R2 = 0.023, P < .01), but the correlation coefficients were low (Fig. 5A and B).
Figure 5.
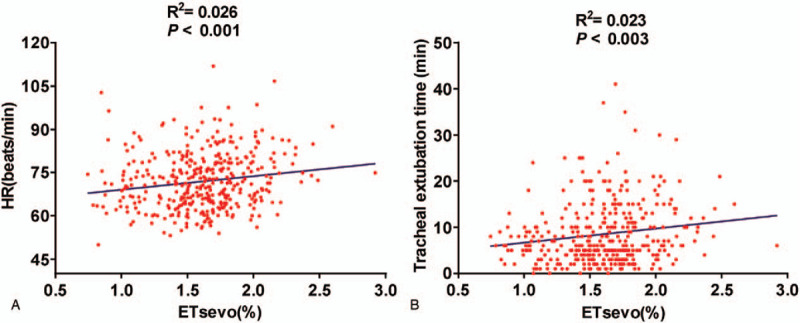
A The correlation between ETsevo and HR (R2 = 0.026, P < .001). B The correlation between ETsevo and the tracheal extubation time (R2 = 0.023, P < .01). The solid lines are linear regression lines.
4. Discussion
We adjusted ETsevo to maintain the BIS between 40 and 60. By doing so, we identified different requirements for sevoflurane among 390 patients. The mean ETsevo of the 390 patients was 1.55% ± 0.26% (approximately 0.91 MAC). The mean ETsevo of the 69 patients (17.7%) in group L was 1.079% ± 0.017% (approximately 0.63 MAC), and the mean ETsevo of the 78 patients (20%) in group H was 2.086% ± 0.020% (approximately 1.22 MAC). Our results show that the ETsevo of group L was significantly lower than that of group H. Sevoflurane is mainly eliminated through the lung, while < 5% of sevoflurane is metabolized through cytochrome P450(CYP)2E1 from the liver.[21] Consequently, at the same level of sedation, differences in ETsevo may reflect differences in sevoflurane sensitivity and may not be due to sevoflurane pharmacokinetics.
One of the most fundamental issues is whether the recommended value of 0.7 to 1.3 MAC can be extrapolated to all patients, which has yet to be investigated. Strikingly, after an analysis of the differential requirements for ETsevo, some patients were not in the recommended range of 0.7 to 1.3 MAC. This result was somewhat counterintuitive. In group L, 5 patients were in the range of 0.46 to 0.5 MAC, 12 patients were in the range of 0.5 to 0.6 MAC, and 26 patients were in the range of 0.6 to 0.7 MAC. Without BIS monitoring, these patients may suffer an overdose of sevoflurane and deep anaesthesia, which may affect postoperative outcomes, prolong extubation time, and increase medical expenses.[1,22] In group H, 11 patients had an ETsevo of >1.3 MAC. Without BIS monitoring, these patients may suffer low anaesthesia, which may lead to intraoperative awareness, haemodynamic fluctuation, and a stress response.[23] Our findings are consistent with previous observations. Specifically, Erden et al. identified that the mean ETsevo was significantly lower in patients with major depressive disorder (1.28% ± 0.15%) than in patients in the control group (1.52% ± 0.22%) during laparoscopic cholecystectomy. Thus, there was a significant difference in the sevoflurane requirement between patient groups in this study.[19] Another study showed that the MACawake of sevoflurane (0.8%) was higher in middle-aged females undergoing breast surgery with sleep disorders than in middle-aged females undergoing breast surgery with normal sleep habits (0.6%).[24] Additionally, the MAC awake of sevoflurane in patients with end-stage renal disease (0.56%) was significantly lower than that observed in the control group (0.67%).[25] These studies contributed to our understanding that patients have different sevoflurane sensitivities, suggesting that sevoflurane should be individually administered.
We found that there was no difference in the ETsevo requirement between males and females. Similarly, some studies have been unable to identify sex-specific differences in the requirements for sevoflurane and desflurane.[26,27] Some studies, however, have indicated that the MAC of xenon in elderly patients was higher in males than in females,[28] and BIS scores of females were higher than those of in males, despite equivalent doses of anaesthetic, which suggests that females are less sensitive to the hypnotic effects of anaesthetics.[29,30] Furthermore, we found a significant individual difference in ETsevo between males and females. We do not know exactly what caused this difference, but different sevoflurane sensitivities may be 1 explanation. The effects of sex on anaesthetic requirements warrant further investigation.
There was no significant difference in sex, age, BMI, ASA grade, MAP, HR, dose of sufentanil and cisatracurium, duration of surgery and anaesthesia, usage of nicardipine and esmolol, usage of aramine and ephedrine, and PETCO2 between group L and group H. However, the tracheal extubation time of group L was significantly shorter than that of group H. A series of studies have shown that BIS monitoring reduces the time to tracheal extubation, eye opening, orientation in time and place, leaving the operating room and postanaesthesia care unit, and the risk of nausea and vomiting after surgery, which clearly indicates that BIS monitoring is associated with early postoperative recovery.[31,32] There is still uncertainty about whether these benefits are due to a reduction in sevoflurane requirements under BIS monitoring. Interestingly, as mentioned in a literature review and meta-analysis, BIS-guided anaesthesia reduced the requirement for sevoflurane by 0.52 MAC and for desflurane by 1.02 MAC, improving early postoperative recovery.[2] As discussed above, BIS plays an important role in guiding individual administration of sevoflurane during surgery. Hence, patients in group H received more sevoflurane than patients in group L, which resulted in a longer tracheal extubation time and promoted early postoperative recovery.
There was no intraoperative awareness among the 390 patients enrolled in our study. It was reported that the incidence of intraoperative awareness is approximately 0.1% to 0.2% in the general surgical population.[8] To understand the correlation between the BIS and intraoperative awareness, Ekman et al and Myles et al found that there were 2 cases of awareness in the BIS monitoring group. Four patients were aware when they had high BIS values of > 60, while other patients were unaware when they had BIS values of 40 – 60.[9,33] Moreover, Avidan et al found that the BIS value was > 60 in 1 case of definite anaesthetic awareness, and the end-tidal anaesthetic gas concentration was < 0.7 MAC in 3 cases.[4] Compared with the 3 cases, the most surprising aspect of our data was that 43 patients whose MACs were < 0.7 suffered no anaesthetic awareness. Therefore, it is now understood that BIS monitoring is an important monitoring tool that can reduce the incidence of intraoperative awareness in patients with different requirements for sevoflurane.
Through linear regression analysis, we found that ETsevo was positively correlated with tracheal extubation time. This result is consistent with the observation that the tracheal extubation time in group H was longer than that in group L. In addition, we found that ETsevo was positively correlated with HR; however, the correlation was weak, which was probably due to different requirements for sevoflurane, interindividual variability, and the fact that the surgical procedure caused large changes in HR. Similarly, in 1 study, sevoflurane was used in children with an average age of 3.3 years, and Spearman's correlation analysis showed that ETsevo was only weakly correlated with MAP and was not correlated with HR.[34]
The present study has several limitations. First, compared with laparoscopic surgery, surgical trauma and consumption of sufentanil may be greater in open surgery. In patients undergoing open surgery, insufficient sufentanil during surgery will lead to a higher ETsevo during anaesthesia, which will affect the screening of patients with different ETsevo requirements. Although there was no difference in the ratio of open surgery to laparoscopic surgery between group L and group H, the proportion of open surgeries in group H (69.6%) was slightly lower than that in group L (80.8%). Therefore, the dose of sufentanil in group H may be higher than that in group L to meet the requirements of surgical analgesia. However, due to the lack of a gold standard to assess the depth of analgesia, we cannot evaluate whether sufentanil was sufficient in the 2 groups. Second, there is no gold standard for monitoring the depth of general anaesthesia. It is reasonable to use BIS values, which reflect the depth of general anaesthesia, and to assess whether the patient has a low or a group H according to ETsevo. With the development of devices to monitor the depth of general anaesthesia, it is better to evaluate patients with different sevoflurane requirements and use this information to individualize anaesthetic regimes.
5. Conclusion
In conclusion, our results show that in adult patients undergoing gastrointestinal surgery, there is a significant difference in the requirement for sevoflurane. Patients with a group H accounted for 17.7% of the 390 patients, while patients with a group L accounted for 20% of the 390 patients. The tracheal extubation time in patients with a group L was significantly shorter than that in patients with a group H. ETsevo was positively correlated with HR and tracheal extubation time, although this correlation was weak. Further studies are required to support this standpoint.
Acknowledgments
We thank professor Zhigang Jiang for assistance in statistical analysis.
Author contributions
Jia Li and Yi Yong Wei contributed equally to this work. Dong Hang Zhang generated the experimental hypothesis, designed the study. Jia Li and Yi Yong Wei contributed to the data collection, analyzed the experimental data, and wrote the first draft of manuscript. Dong Hang Zhang helped revise the manuscript. We also thank Dong Hang Zhang for her supervision in this study. All authors read and approved the final manuscript and agreed for publication.
Conceptualization: Dong Hang Zhang.
Data curation: Jia Li, Yi Yong Wei, Dong Hang Zhang.
Formal analysis: Jia Li.
Investigation: Jia Li, Yi Yong Wei.
Methodology: Yi Yong Wei, Dong Hang Zhang.
Project administration: Jia Li, Yi Yong Wei.
Supervision: Dong Hang Zhang.
Writing – original draft: Jia Li.
Writing – review & editing: Yi Yong Wei, Dong Hang Zhang.
Footnotes
Abbreviations: BIS = bispectral index, ETsevo = end-tidal sevoflurane concentration, group H = high requirement for sevoflurane, group L = low requirement for sevoflurane, HR = heart rate, MAP = mean arterial pressure, PETCO2 = end-tidal partial pressure of carbon dioxide.
How to cite this article: Li J, Wei YY, Zhang DH. Postoperative recovery of patients with differential requirements for sevoflurane after abdominal surgery: A prospective observational clinical study. Medicine. 2021;100:8(e24842).
This work was supported by the grants 2018SZ0211 (to L.Z.) from Science & Technology Department of Sichuan Province and 1, 3, 5 Project of West China Hospital.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are publicly available.
References
- [1].Zorrilla-Vaca A, Healy RJ, Wu CL, et al. Relation between bispectral index measurements of anesthetic depth and postoperative mortality: a meta-analysis of observational studies. Can J Anaesth 2017;64:597–607. [DOI] [PubMed] [Google Scholar]
- [2].Punjasawadwong Y, Phongchiewboon A, Bunchungmongkol N. Bispectral index for improving anaesthetic delivery and postoperative recovery. Cochrane Database Syst Rev 2014;6:CD003843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Bocskai T, Loibl C, Vamos Z, et al. Cost-effectiveness of anesthesia maintained with sevoflurane or propofol with and without additional monitoring: a prospective, randomized controlled trial. BMC Anesthesiol 2018;18:100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Avidan MS, Zhang L, Burnside BA, et al. Anesthesia awareness and the bispectral index. N Engl J Med 2008;358:1097–108. [DOI] [PubMed] [Google Scholar]
- [5].Deis AS, Schnetz MP, Ibinson JW, et al. Retrospective analysis of cases of intraoperative awareness in a large multi-hospital health system reported in the early postoperative period. BMC Anesthesiol 2020;20:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Phillips AA, McLean RF, Devitt JH, et al. Recall of intraoperative events after general anaesthesia and cardiopulmonary bypass. Can J Anaesth 1993;40:922–6. [DOI] [PubMed] [Google Scholar]
- [7].Struys MM, Jensen EW, Smith W, et al. Performance of the ARX-derived auditory evoked potential index as an indicator of anesthetic depth: a comparison with bispectral index and hemodynamic measures during propofol administration. Anesthesiology 2002;96:803–16. [DOI] [PubMed] [Google Scholar]
- [8].Sandin RH, Enlund G, Samuelsson P, et al. Awareness during anaesthesia: a prospective case study. Lancet 2000;355:707–11. [DOI] [PubMed] [Google Scholar]
- [9].Myles PS, Leslie K, McNeil J, et al. Bispectral index monitoring to prevent awareness during anaesthesia: the B-Aware randomised controlled trial. Lancet 2004;363:1757–63. [DOI] [PubMed] [Google Scholar]
- [10].Epstein RH, Maga JM, Mahla ME, et al. Prevalence of discordant elevations of state entropy and bispectral index in patients at amnestic sevoflurane concentrations: a historical cohort study. Can J Anaesth 2018;65:512–21. [DOI] [PubMed] [Google Scholar]
- [11].Park S, Yook K, Yoo KY, et al. Comparison of the effect of sevoflurane or propofol anesthesia on the regional cerebral oxygen saturation in patients undergoing carotid endarterectomy: a prospective, randomized controlled study. BMC Anesthesiol 2019;19:157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Wang J, Zhang L, Huang Q, et al. Monitoring the end-tidal concentration of sevoflurane for preventing awareness during anesthesia (MEETS-PANDA): a prospective clinical trial. Int J Surg 2017;41:44–9. [DOI] [PubMed] [Google Scholar]
- [13].Sigl JC, Chamoun NG. An introduction to bispectral analysis for the electroencephalogram. J Clin Monit 1994;10:392–404. [DOI] [PubMed] [Google Scholar]
- [14].Rampil IJ. A primer for EEG signal processing in anesthesia. Anesthesiology 1998;89:980–1002. [DOI] [PubMed] [Google Scholar]
- [15].Recart A, Gasanova I, White PF, et al. The effect of cerebral monitoring on recovery after general anesthesia: a comparison of the auditory evoked potential and bispectral index devices with standard clinical practice. Anesth Analg 2003;97:1667–74. [DOI] [PubMed] [Google Scholar]
- [16].Punjasawadwong Y, Boonjeungmonkol N, Phongchiewboon A. Bispectral index for improving anaesthetic delivery and postoperative recovery. Cochrane Database Syst Rev 2007;4:CD003843. [DOI] [PubMed] [Google Scholar]
- [17].Glass PS, Bloom M, Kearse L, et al. Bispectral analysis measures sedation and memory effects of propofol, midazolam, isoflurane, and alfentanil in healthy volunteers. Anesthesiology 1997;86:836–47. [DOI] [PubMed] [Google Scholar]
- [18].Sebel PS, Lang E, Rampil IJ, et al. A multicenter study of bispectral electroencephalogram analysis for monitoring anesthetic effect. Anesth Analg 1997;84:891–9. [DOI] [PubMed] [Google Scholar]
- [19].Erden V, Güler C, Seven S, et al. Bispectral-Index-measured sevoflurane requirement might be decreased in individuals with major depressive disorder. Minerva Anestesiol 2018;84:33–9. [DOI] [PubMed] [Google Scholar]
- [20].Zou ZY, Zhao YL, Yang XL, et al. Effects of different remifentanil target concentrations on MAC BAR of sevoflurane in gynaecological patients with CO2 pneumoperitoneum stimulus. Br J Anaesth 2015;114:634–9. [DOI] [PubMed] [Google Scholar]
- [21].De Hert S, Moerman A. Sevoflurane. F1000Res 2015;4:626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Liu YH, Qiu DJ, Jia L, et al. Depth of anesthesia measured by bispectral index and postoperative mortality: A meta-analysis of observational studies. J Clin Anesth 2019;56:119–25. [DOI] [PubMed] [Google Scholar]
- [23].Orser BA. Depth-of-anesthesia monitor and the frequency of intraoperative awareness. N Engl J Med 2008;358:1189–91. [DOI] [PubMed] [Google Scholar]
- [24].Cao Y, Zhang L, Peng X, et al. Increased minimum alveolar concentration-awake of Sevoflurane in women of breast surgery with sleep disorders. BMC Anesthesiol 2020;20:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Wu Y, Jin S, Zhang L, et al. Minimum alveolar concentration-awake of sevoflurane is decreased in patients with end-stage renal disease. Anesth Analg 2019;128:77–82. [DOI] [PubMed] [Google Scholar]
- [26].Eger EI, Laster MJ, Gregory GA, et al. Women appear to have the same minimum alveolar concentration as men: a retrospective study. Anesthesiology 2003;99:1059–61. [DOI] [PubMed] [Google Scholar]
- [27].Wadhwa A, Durrani J, Sengupta P, et al. Women have the same desflurane minimum alveolar concentration as men: a prospective study. Anesthesiology 2003;99:1062–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Goto T, Nakata Y, Morita S. The minimum alveolar concentration of xenon in the elderly is sex-dependent. Anesthesiology 2002;97:1129–32. [DOI] [PubMed] [Google Scholar]
- [29].Buchanan FF, Myles PS, Cicuttini F. Effect of patient sex on general anaesthesia and recovery. Br J Anaesth 2011;106:832–9. [DOI] [PubMed] [Google Scholar]
- [30].Buchanan FF, Myles PS, Leslie K, et al. Gender and recovery after general anesthesia combined with neuromuscular blocking drugs. Anesth Analg 2006;102:291–7. [DOI] [PubMed] [Google Scholar]
- [31].Yu H, Zhang L, Ma Y, et al. Early postoperative recovery in operating room after desflurane anesthesia combined with Bispectral index (BIS) monitoring and warming in lengthy abdominal surgery: a randomized controlled study. BMC Anesthesiol 2018;18:110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Oliveira CR, Bernardo WM, Nunes VM. Benefit of general anesthesia monitored by bispectral index compared with monitoring guided only by clinical parameters. Systematic review and meta-analysis. Braz J Anesthesiol 2017;67:72–84. [DOI] [PubMed] [Google Scholar]
- [33].Ekman A, Lindholm ML, Lennmarken C, et al. Reduction in the incidence of awareness using BIS monitoring. Acta Anaesthesiol Scand 2004;48:20–6. [DOI] [PubMed] [Google Scholar]
- [34].McCann ME, Bacsik J, Davidson A, et al. The correlation of bispectral index with endtidal sevoflurane concentration and haemodynamic parameters in preschoolers. Paediatr Anaesth 2002;12:519–25. [DOI] [PubMed] [Google Scholar]


