Abstract
Background/Objectives:
Older adults ≥65 years have the highest outpatient antibiotic prescribing rate of all age groups. We characterized antibiotics prescribed to older adults to guide efforts to improve antibiotic use.
Design:
Outpatient antibiotic prescriptions dispensed for older adults from 2011–2014 were extracted from the IQVIA Xponent database. A chi-square trend analysis was conducted to assess annual changes in antibiotic prescribing rates. A descriptive analysis of prescribing rates by antibiotic, age group, sex, state, census region, and provider specialty was completed.
Setting:
Ambulatory
Participants:
Adults aged ≥65 years in the United States
Results:
During 2011–2014, outpatient antibiotic prescribing rates remained stable in U.S. older adults (P = 0.89). In 2014, older adults were dispensed 51.6 million prescriptions (1115 prescriptions/1000 persons). Persons aged ≥75 years had a higher prescribing rate (1157 prescriptions/1000 persons) than persons aged 65–74 (1084 prescriptions/1000 persons). Prescribing rates were highest in the South and lowest in the West (1228 and 854 prescriptions/1000 persons, respectively). The most commonly prescribed class was quinolones, followed by penicillins and macrolides. Azithromycin was the most commonly prescribed drug, followed by amoxicillin and ciprofloxacin. Internists and family physicians prescribed 43% of antibiotic courses.
Conclusions:
On average, in 2014, U.S. adults ≥65 years received enough outpatient antibiotic courses for every older adult to receive at least one. Quinolones and azithromycin are potential targets for assessing the appropriateness of antibiotic prescribing among this population. Interventions to improve use targeting internist and family physicians in the South census region might have the potential to be more impactful.
Keywords: antibiotics, out-patients, elderly
INTRODUCTION:
Antibiotic resistance is a significant public health threat, and the use of antibiotics is the most important modifiable risk factor leading to antibiotic resistance 1. Antibiotic overuse leads to direct threats to patients such as allergic reactions and drug-induced adverse events 6, including Clostridium difficile infection which causes significant morbidity and mortality in older adults 7,8. Older adults ≥65 years old have the highest outpatient antibiotic prescribing rate of any age group in the United States 9. Between 2000–2010, rates of antibiotic prescribing decreased among children and adolescents, however increased among adults ≥65 years old 10. With 20% of the U.S. population expected to be ≥65 years old by 2030 2, a better understanding of antibiotic prescribing in this age group is important to better target interventions to improve antibiotic use. In this analysis, we describe antibiotic prescribing practices in outpatient adults ≥65 years old to highlight potential opportunities for antibiotic stewardship in this population.
METHODS:
Outpatient systemic oral antibiotic prescriptions dispensed in the United States for older adults (defined for this report as aged ≥65 years) were extracted from the IQVIA Xponent database for years 2011 to 2014. IQVIA Xponent is a proprietary database that collects data from U.S. pharmacies that report their entire pharmacy business to IQVIA weekly. This allows IQVIA to capture 74% in 2011 and 86% in 2014 of all outpatient prescriptions in the United States. Then captured sales are reconciled to wholesale deliveries that provide an estimate of total antibiotic use, and projected to 100% coverage of all outpatient prescriptions using a patented method based on a comprehensive sample of patient de-identified prescription transactions. Antibiotics were aggregated into categories according to the Uniform System of Classification (IQVIA internal documentation), a therapeutic classification system created by IQVIA, as follows: quinolones, penicillins, macrolides, cephalosporins, trimethoprim-sulfamethoxazole, tetracyclines, urinary anti-infectives, β-lactams with increased activity, lincosamides, and others.
A chi-square trend analysis for changes in antibiotic prescribing rates for the years 2011 to 2014 was completed. Total prescription counts and percentages were reported by antibiotic class, antibiotic drug, patient sex, patient age group (65–74 and ≥75 years), and U.S. census region 11 for 2014 only. Prescribing rates per 1000 population in 2014 were calculated using population data obtained from the U.S. census bridging files by sex, age group, state, and census region. Prescribing rates for antibiotic classes and specific drugs were further stratified by age groups (i.e., 65–74 and ≥75). Provider specialties were based on the American Medical Association self-designated practice specialties. Prescription counts and percentages for all antibiotics, quinolones and ciprofloxacin were calculated for the following specialties: family practice, internal medicine (including internal medicine-pediatrics), nurse practitioners and physician assistants, dentistry, urology, surgery, emergency medicine, dermatology, otolaryngology, obstetrics and gynecology, infectious diseases, medical subspecialty, others and unknown. All analyses were conducted using SAS, version 9.3 (SAS Institute, Cary, NC).
RESULTS:
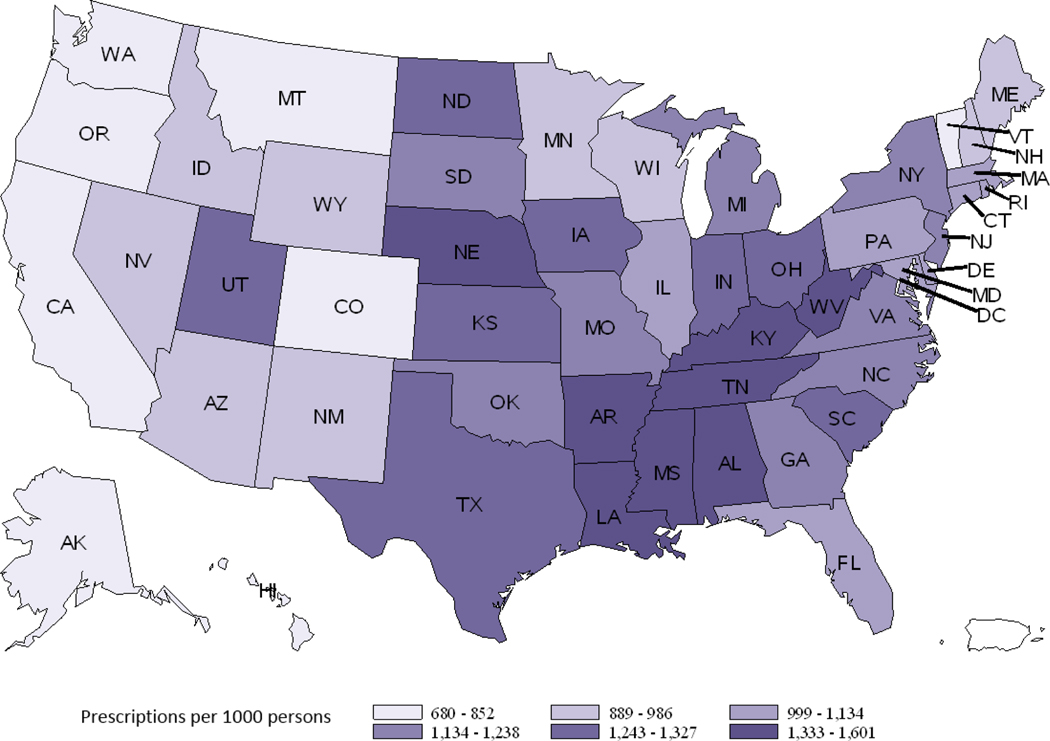
In 2011 and 2014, older adults ≥65 years old in the United States were prescribed 46 million (1113 prescriptions per 1000 persons) and 51.6 million (1115 prescriptions per 1000 persons) outpatient antibiotic prescriptions, respectively. Prescribing rates for outpatient antibiotics remained stable overall between 2011 and 2014 (P = 0.89). In 2014, Persons aged ≥75 years had a higher prescribing rate (1157 prescriptions per 1000 persons) than persons aged 65–74 (1084 prescriptions per 1000 persons) (Table 1). The antibiotic prescribing rate was higher among women (Table 1). Comparing rates of prescribing by geographic region, rates were highest in the South census region and lowest in the West (1228 and 854 prescriptions per 1000 persons, respectively) (Table 1). Among individual states, Alaska had the lowest prescribing rate (680 prescriptions per 1000 persons), and Mississippi had the highest rate (1601 prescriptions per 1000 persons) (Figure 1).
Table 1:
Outpatient Antibiotic Prescriptions According to Antibiotic Class, Antibiotic Drug, Sex, Age Group, and U.S. Census Region in Adults ≥65 years 2014
| Characteristic | Prescriptions | Prescriptions per 1000 persons, Rate | |
|---|---|---|---|
| #x106 | (%) | ||
| Antibiotic Class | |||
| Quinolones | 11.4 | (22) | 245 |
| Penicillins | 8.1 | (16) | 174 |
| Macrolides | 7.9 | (15) | 170 |
| Cephalosporins | 7.1 | (14) | 153 |
| Trimethoprim Sulfamethoxazole | 4.4 | (9) | 95 |
| Tetracyclines | 3.7 | (7) | 80 |
| Urinary anti-infectives | 3.5 | (7) | 76 |
| β-lactams (increased activity) | 3.4 | (7) | 74 |
| Lincosamides | 2.0 | (4) | 42 |
| Other | 0.2 | (<1) | 4 |
| Total | 51.6 | 1115 | |
| Antibiotic Drug (top 5) | |||
| Azithromycin | 7.3 | (14) | 157 |
| Amoxicillin | 7.1 | (14) | 153 |
| Ciprofloxacin | 7.0 | (14) | 151 |
| Cephalexin | 4.9 | (10) | 106 |
| Trimethoprim Sulfamethoxazole | 4.2 | (8) | 90 |
| Sex | |||
| Female | 31.7 | (62) | 1225 |
| Male | 19.8 | (38) | 974 |
| Age Group, years | |||
| 65–74 | 28.6 | (55) | 1084 |
| ≥75 | 23.0 | (45) | 1157 |
| US Census Region | |||
| South | 21.3 | (41) | 1228 |
| Midwest | 11.9 | (23) | 1184 |
| Northeast | 9.6 | (19) | 1114 |
| West | 8.7 | (17) | 854 |
Figure 1:
Antibiotic Prescribing per 1000 Persons by State in 2014 for Adults Aged ≥65 years
Quinolones were the most commonly prescribed outpatient antibiotic class in older adults at a rate of 245 prescriptions per 1000 persons; they accounted for 22% of all antibiotics prescribed. Quinolones were followed by penicillins (174 prescriptions per 1000 persons) and macrolides (170 prescriptions per 1000 persons) (Table 1). Prescribing rates stratified by age groups 65–74 and ≥75 years are shown in table S1, prescribing patterns among those ≥ 85 years were generally similar to those aged 75–85 years. Although quinolones were the most commonly prescribed antibiotic as a class, azithromycin was the most commonly prescribed antibiotic drug, followed by amoxicillin and ciprofloxacin (Table 1). However, ciprofloxacin was the most frequently prescribed drug among individuals aged ≥75 years (Table S1).
Internists (12 million prescriptions, 23%) and family physicians (10 million, 20%) prescribed 43% of all antibiotic prescriptions for older adults and 46% of quinolone prescriptions, followed by nurse practitioners and physician assistants (7 million, 14%). Of the remaining specialties, dentists were the next most common prescribers (6 million, 11%) (Table 2).
Table 2:
Antibiotic Prescriptions per Provider by Provider Specialty in 2014 for Adults ≥65 years
| Provider specialty | All Antibiotics |
Quinolones |
||
|---|---|---|---|---|
| #×106 | % | #×106 | % | |
| Family Practice | 12.0 | (23) | 2.9 | (26) |
| Internal Medicine | 10.4 | (20) | 3.0 | (26) |
| Nurse Practitioners/Physician Assistants | 7.1 | (14) | 1.6 | (14) |
| Dentistry | 5.9 | (11) | 0.1 | (<1) |
| Urology | 3.2 | (6) | 1.2 | (10) |
| Surgery (general) | 2.3 | (4) | 0.3 | (2) |
| Emergency Medicine | 1.9 | (4) | 0.5 | (5) |
| Dermatology | 1.1 | (2) | 0.1 | (<1) |
| Otolaryngology | 0.7 | (1) | 0.1 | (1) |
| Obstetrics/Gynecology | 0.6 | (1) | 0.1 | (1) |
| Infectious Diseases | 0.4 | (<1) | 0.1 | (<1) |
| Medical Subspecialty | 2.6 | (5) | 0.8 | (7) |
| Other/Unknown | 3.3 | (6) | 0.7 | (6) |
| Total | 51.6 | 11.4 | ||
DISCUSSION:
This study provides insight into outpatient antibiotic prescribing practices in older adults in the United States, specifically describing burden, geographic, drug choice and prescriber variation. In 2014, the antibiotic prescribing rate in outpatient older adults was 1115 prescriptions per 1000 persons, lower than the prescribing rate in a recent analysis of Medicare part D enrollees (1452 claims per 1000 enrollees) in 2013 12. The differences in the study populations could explain some of the differences in rates since not all Medicare part D enrollees are ambulatory, and a subset could reside in long-term care facilities. The rate of outpatient antibiotic prescribing remained stable between 2011 and 2014, and previously described increases in prescribing rates reported between 2000 and 2010 in older adults in the United States did not appear to persist in this analysis 10. Whether this reflects changes in prescribing practices in this age group or differences in data sources is unclear. An analysis of outpatient antibiotic use in adults ≥ 65 years in Ontario, Canada also reported stable use from 2006 to 2015 14. Follow up of antibiotic prescribing rates in this age group will be needed to confirm that prescribing is not increasing further, and to evaluate the effectiveness of antibiotic stewardship activities.
We found large variations in antibiotic prescribing rates by state and geographic region. The antibiotic prescribing rate in the South census region was 44% higher than the West census region, which had the lowest rate. Geographic variation in antibiotic prescribing in the United States has been previously reported; the South census region has been found to have higher prescribing rates in all age groups 18, and in older adults specifically 12,19. Previous studies assessing the appropriateness of antibiotic prescribing have concluded that the frequency of inappropriate antibiotic prescribing is higher in the South 19,20. The frequency of inappropriate prescribing was also higher for other medications in older adults in the South 21,22. Regional variation in antibiotic prescribing in this population is likely explained by multiple factors, and may include the frequency of comorbidities, socioeconomic factors, and patient and prescriber beliefs and attitudes about antibiotic use. A better understanding of these factors may help inform effective antibiotic stewardship interventions.
Quinolones were the most commonly prescribed antibiotic class in adults aged ≥65 years, whereas they were the third most commonly prescribed antibiotic class in a previous analysis in all adults ≥20 years behind macrolides and penicillins 18. Although declines in outpatient quinolone prescribing have been described in other countries 14, that was not observed in this analysis. Quinolones have a broad spectrum of activity and a favorable pharmacokinetic profile, which likely drive prescribing 24. And in those aged ≥75 years, ciprofloxacin was the most commonly prescribed drug. This could reflect the increasing incidence of urinary tract infections with age, especially in men 28,29. Urinary tract infection is one of the most common conditions associated with antibiotic prescribing in this age group 25, and urologists prescribed a higher proportion of quinolones compared to all antibiotics in this analysis (Table 2). In a recent analysis by Kobayashi et al, quinolones were the most frequently prescribed antibiotic for uncomplicated urinary tract infection in women, and patients aged ≥70 years were more likely to receive quinolones 30.
Azithromycin was the most common antibiotic prescribed, similar to the pattern previously reported for all adults 18. In 2010–2011, 18% of prescriptions in doctors’ offices and emergency room departments for adults ≥65 years old were considered unnecessary 25, and overuse of macrolides for respiratory tract infections is well documented among adults 26. Antibiotics were inappropriately prescribed for 46% of low risk older adults presenting with nonbacterial acute upper respiratory tract infections, and 70% of prescriptions were for broad-spectrum agents, like macrolides 27.
Appropriate antibiotic use is particularly important because of the high risk of adverse drug events and complications that can result from drug-drug interactions in this age group 6,8. Quinolones were the most commonly prescribed antibiotic class in this analysis. A recent Food and Drug Administration (FDA) warning highlighted the adverse events associated with quinolone prescribing, and advised against their use for conditions where safer alternatives are available and recommended 31. Antibiotic use is the most important risk factor for developing C. difficile infection, and older adults are at an increased risk for C. difficile infection and have a higher rate of associated mortality 7,32. Considering the potential for unintended consequences associated with antibiotic prescribing in older adults, improving antibiotic use in general, and quinolones in particular, has the potential to improve outcomes for this vulnerable patient population. The increased incidence of infections, infectious disease mortality, and prevalence of comorbidities pose unique challenges to the diagnosis and treatment of infections in older adults 23,33. Further analyses of the clinical indications associated with antibiotic prescriptions and the approaches to antibiotic selection in this patient population are needed.
Primary care providers prescribe the highest proportion of antibiotics in older adults in the outpatient setting, similar to other age groups 18. A study done in Ontario, Canada reported that primary care physicians, who are mid- to late-career, with high patient volume, and who trained outside Canada or the United States were more likely to prescribe antibiotics inappropriately for acute upper respiratory conditions in older adults27. In light of these factors, interventions targeting primary care providers have the potential to be the most impactful on improving outpatient antibiotic prescribing in older adults.
The results of this analysis represent a summary of antibiotics dispensed in the outpatient setting for older adults but is subject to several limitations. While this study characterized the volume of antibiotic use, it was not possible to assess the appropriateness of prescribing since associated clinical conditions, comorbidities, and drug allergies were not captured. Dispensing data may under- or overestimate actual antibiotic consumption, as adherence to antibiotic courses varies and the data sources does not account for non-prescription acquisition of antibiotics. While describing the volume of antibiotic prescribing can highlight opportunities for improvement, further analyses are needed to better describe specific conditions associated with outpatient antibiotic prescribing in older adults and to characterize antibiotic selection and duration of therapy for different infections. Analyses of claims data or point prevalence surveys that contain more details on the reason for the prescription can be useful to inform appropriate antibiotic use assessments.
Efforts to optimize antibiotic use in the outpatient setting are gaining momentum. In 2016, the Centers for Disease Control and Prevention published the Core Elements of Outpatient Antibiotic Stewardship, which recommend that outpatient clinicians implement policies to promote appropriate antibiotic prescribing practices 36. In 2017, Centers for Medicare & Medicaid Services-funded Quality Innovation Network and Quality Improvement Organizations recruited over 7,000 outpatient providers and practices to implement the core elements. Potential targets for improving antibiotic use in older adults include optimizing antibiotic selection, reducing quinolones and azithromycin prescribing and targeting primary care physicians in the South census region.
Supplementary Material
Impact Statement: We certify that this work is confirmatory of recent novel clinical research:
Arizpe A, Reveles KR, Aitken SL. Regional variation in antibiotic prescribing among medicare part D enrollees, 2013. BMC Infectious Diseases. 2016;16(1):744.
Hicks LA, Bartoces MG, Roberts RM, et al. US outpatient antibiotic prescribing variation according to geography, patient population, and provider specialty in 2011. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2015;60(9):1308-1316.
The paper by Arzipe et al described outpatient antibiotic prescribing in older adults. Our analysis shows similar results using a different data source, but in addition tracks antibiotic use over time, and describes provider groups prescribing the most antibiotics to outpatient older adults. The analysis by Hicks et al (also a coauthor for this manuscript) described antibiotic use in the whole U.S. population using the same data source for 2011. This analysis focuses on older adults, is more recent, and tracks antibiotic use over time. Overall this analysis is highlighting targets for improving antibiotic use in older adults.
ACKNOWLEDGMENTS:
The authors would like to thank Rebecca Roberts for her support providing resources and facilitating communication related to this manuscript.
Funding sources and meetings: No grants or funding supported this paper. The abstract was presented at ID Week 2017 (the meeting of the Infectious Disease Society of America).
Footnotes
Sponsor’s Role:
This study has no sponsor.
Title for Supplemental Material:
Age Stratified Antibiotic Prescribing Rates
Conflict of Interest:
The authors have no conflicts in the cover letter as well as in the manuscript.
REFERENCES:
- 1.Centers for Disease Control and Prevention. Antibiotic Resistant Threats in the United States, 2013. http://www.cdc.gov/drugresistance/threat-report-2013. Accessed August 24, 2016.
- 2.Centers for Disease Control and Prevention. The State of Aging and Health in America 2013. http://www.cdc.gov/aging/pdf/state-aging-health-in-america-2013.pdf. Accessed August 24, 2016.
- 3.WHO. Global action plan on antimicrobial resistance. 2014; http://apps.who.int/iris/bitstream/10665/112642/1/9789241564748_eng.pdf. Accessed August 30, 2016.
- 4.File TM, Srinivasan A, Bartlett JG. Antimicrobial stewardship: importance for patient and public health. Clinical Infectious Diseases. 2014;59(suppl 3):S93–S96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Van De Sande-Bruinsma N, Grundmann H, Verloo D, Tiemersma E, Monen J, Goossens H. Antimicrobial drug use and resistance in Europe. Emerging Infectious Diseases. 2008;14(11):1722–1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shehab N, Lovegrove MC, Geller AI, Rose KO, Weidle NJ, Budnitz DS. US Emergency Department Visits for Outpatient Adverse Drug Events, 2013–2014. Journal of American Medical Association. 2016;316(20):2115–2125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lessa FC, Mu Y, Bamberg WM, et al. Burden of Clostridium difficile infection in the United States. New England Journal of Medicine. 2015;372(9):825–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Faulkner CM, Cox HL, Williamson JC. Unique aspects of antimicrobial use in older adults. Clinical Infectious Diseases. 2005;40(7):997–1004. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Antibiotic Resistance Patient Safety Atlas. https://gis.cdc.gov/grasp/PSA/indexAU.html. Accessed May 8, 2018.
- 10.Lee GC, Reveles KR, Attridge RT, et al. Outpatient antibiotic prescribing in the United States: 2000 to 2010. BMC medicine. 2014;12(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.U.S Census Bureau. Census Regions and Divisions of the United States. http://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf. Accessed May 8, 2018.
- 12.Arizpe A, Reveles KR, Aitken SL. Regional variation in antibiotic prescribing among medicare part D enrollees, 2013. BMC Infectious Diseases. 2016;16(1):744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nicolle LE, Bentley DW, Garibaldi R, Neuhaus EG, Smith PW. Antimicrobial use in long-term-care facilities. SHEA Long-Term-Care Committee. Infection control and hospital epidemiology. 2000;21(8):537–545. [DOI] [PubMed] [Google Scholar]
- 14.Tan C, Graves E, Lu H, et al. A decade of outpatient antimicrobial use in older adults in Ontario: a descriptive study. CMAJ open. 2017;5(4):E878–e885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mor A, Frøslev T, Thomsen RW, et al. Antibiotic use varies substantially among adults: a cross-national study from five European Countries in the ARITMO project. Infection. 2015;43(4):453–472. [DOI] [PubMed] [Google Scholar]
- 16.Blix HS, Engeland A, Litleskare I, Ronning M. Age- and gender-specific antibacterial prescribing in Norway. The Journal of antimicrobial chemotherapy. 2007;59(5):971–976. [DOI] [PubMed] [Google Scholar]
- 17.Franchi C, Sequi M, Bonati M, et al. Differences in outpatient antibiotic prescription in Italy’s Lombardy region. Infection. 2011;39(4):299–308. [DOI] [PubMed] [Google Scholar]
- 18.Hicks LA, Bartoces MG, Roberts RM, et al. US outpatient antibiotic prescribing variation according to geography, patient population, and provider specialty in 2011. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2015;60(9):1308–1316. [DOI] [PubMed] [Google Scholar]
- 19.Zhang Y, Steinman MA, Kaplan CM. Geographic variation in outpatient antibiotic prescribing among older adults. Archives of internal medicine. 2012;172(19):1465–1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roberts RM, Hicks LA, Bartoces M. Variation in US outpatient antibiotic prescribing quality measures according to health plan and geography. The American journal of managed care. 2016;22(8):519–523. [PMC free article] [PubMed] [Google Scholar]
- 21.Bauer MS, Lee A, Li M, Bajor L, Rasmusson A, Kazis LE. Off-label use of second generation antipsychotics for post-traumatic stress disorder in the Department of Veterans Affairs: time trends and sociodemographic, comorbidity, and regional correlates. Pharmacoepidemiology and drug safety. 2014;23(1):77–86. [DOI] [PubMed] [Google Scholar]
- 22.Zhang Y, Baicker K, Newhouse JP. Geographic variation in the quality of prescribing. The New England journal of medicine. 2010;363(21):1985–1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.El Bcheraoui C, Mokdad AH, Dwyer-Lindgren L, et al. Trends and Patterns of Differences in Infectious Disease Mortality Among US Counties, 1980–2014. Jama. 2018;319(12):1248–1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Almalki ZS, Alahmari AK, Guo JJ, Cavanaugh TM. Off-label use of oral fluoroquinolone antibiotics in outpatient settings in the United States, 2006 to 2012. Pharmacoepidemiology and drug safety. 2016;25(9):1042–1051. [DOI] [PubMed] [Google Scholar]
- 25.Fleming-Dutra KE, Hersh AL, Shapiro DJ, et al. Prevalence of inappropriate antibiotic prescriptions among US ambulatory care visits, 2010–2011. Journal of American Medical Association 2016;315(17):1864–1873. [DOI] [PubMed] [Google Scholar]
- 26.Hersh AL, Fleming-Dutra KE, Shapiro DJ, Hyun DY, Hicks LA. Frequency of First-line Antibiotic Selection Among US Ambulatory Care Visits for Otitis Media, Sinusitis, and Pharyngitis. JAMA Internal Medicine. 2016;176(12):1870–1872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Silverman M, Povitz M, Sontrop JM, et al. Antibiotic Prescribing for Nonbacterial Acute Upper Respiratory Infections in Elderly Persons. Annals of internal medicine. 2017;166(11):765–774. [DOI] [PubMed] [Google Scholar]
- 28.Rowe TA, Juthani-Mehta M. Urinary tract infection in older adults. Aging health. 2013;9(5):519–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Foxman B, Brown P. Epidemiology of urinary tract infections: transmission and risk factors, incidence, and costs. Infectious disease clinics of North America. 2003;17(2):227–241. [DOI] [PubMed] [Google Scholar]
- 30.Kobayashi M, Shapiro DJ, Hersh AL, Sanchez GV, Hicks LA. Outpatient Antibiotic Prescribing Practices for Uncomplicated Urinary Tract Infection in Women in the United States, 2002–2011. Open forum infectious diseases. 2016;3(3):ofw159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.U.S. Food and Drug Administration. FDA Drug Safety Communication: FDA advises restricting fluoroquinolone antibiotic use for certain uncomplicated infections. 2016; http://www.fda.gov/Drugs/DrugSafety/ucm500143.htm. Accessed Sepetmber 2, 2016.
- 32.Redelings MD, Sorvillo F, Mascola L. Increase in Clostridium difficile-related mortality rates, United States, 1999–2004. Emerg Infect Dis. 2007;13(9):1417–1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jump RLP, Canaday DH. Aging Has Unique Effects on the Risks, Presentation, Diagnosis, Treatment, and Prognosis of Infectious Diseases. Infectious disease clinics of North America. 2017;31(4):xiii–xv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gurwitz JH, Field TS, Harrold LR, et al. Incidence and preventability of adverse drug events among older persons in the ambulatory setting. Jama. 2003;289(9):1107–1116. [DOI] [PubMed] [Google Scholar]
- 35.Dingle KE, Didelot X, Quan TP, et al. Effects of control interventions on Clostridium difficile infection in England: an observational study. The Lancet. Infectious diseases. 2017;17(4):411–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sanchez GV, Fleming-Dutra KE, Roberts RM, Hicks LA. Core Elements of Outpatient Antibiotic Stewardship. MMWR. Recommendations and reports : Morbidity and mortality weekly report. Recommendations and reports. 2016;65(6):1–12. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.