Abstract
Background
The unique phenotypic and genetic aspects of obsessive-compulsive (OCD) and attention-deficit/hyperactivity disorder (ADHD) among individuals with Tourette syndrome (TS) are not well characterized. Here, we examine symptom patterns and heritability of OCD and ADHD in TS families.
Method
OCD and ADHD symptom patterns were examined in TS patients and their family members (N=3494) using exploratory factor analyses (EFA) for OCD and ADHD symptoms separately, followed by latent class analyses (LCA) of the resulting OCD and ADHD factor sum scores jointly; heritability and clinical relevance of the resulting factors and classes were assessed.
Results
EFA yielded a 2-factor model for ADHD and an 8-factor model for OCD. Both ADHD factors (inattentive and hyperactive/impulsive symptoms) were genetically related to TS, ADHD, and OCD. The doubts, contamination, need for sameness, and superstitions factors were genetically related to OCD, but not ADHD or TS; symmetry/exactness and fear-of-harm were associated with TS and OCD while hoarding was associated with ADHD and OCD. In contrast, aggressive urges were genetically associated with TS, OCD, and ADHD. LCA revealed a three-class solution: few OCD/ADHD symptoms [LC1], OCD & ADHD symptoms [LC2], and symmetry/exactness, hoarding, and ADHD symptoms [LC3]. LC2 had the highest psychiatric comorbidity rates (≥50% for all disorders).
Conclusions
Symmetry/exactness, aggressive urges, fear-of-harm, and hoarding show complex genetic relationships with TS, OCD, and ADHD, and, rather than being specific subtypes of OCD, transcend traditional diagnostic boundaries, perhaps representing an underlying vulnerability (e.g., failure of top-down cognitive control) common to all three disorders.
Introduction
Tourette syndrome (TS) is phenotypically and etiologically heterogeneous, characterized by motor and phonic tics (American Psychiatric Association 2013), often with symptoms of obsessive-compulsive disorder (OCD) and attention-deficit/hyperactivity disorder (ADHD) (Hirschtritt et al 2015), both of which consist of multiple symptom subgroups. Between 3–5 OCD symptom groups have been identified, including contamination/cleaning, taboo/forbidden thoughts, and hoarding, and less consistently symmetry, superstitions/repeating rituals, doubts, fear-of-harm, and checking (Bloch et al 2008, Delucchi et al 2011, Leckman et al 2010). Between 2–3 symptom groups have been identified for ADHD: inattentive, impulsive, and hyperactive symptoms (the latter two are often combined) (Collett et al 2000, Dumenci et al 2004, Pillow et al 1998, Toplak et al 2009). For both OCD and ADHD, parsing these symptom subtypes has led to improved understanding of the pathophysiology of these disorders (Freitag et al 2010, Katerberg et al 2010).
Subgroups of OCD and ADHD may also exist in TS samples; however, they may also (1) differ from those seen in OCD or ADHD populations, and (2) be associated with distinct pathophysiology or treatment outcomes. Early studies in TS samples primarily examined these dimensions at the diagnostic level (e.g., combinations of TS, OCD, and ADHD diagnoses) (Mathews and Grados 2011, Pauls et al 1993, Robertson et al 2008). Only a few have conducted symptom-level analyses across ≥3 disorders (e.g., TS, OCD, and ADHD, ± autism) (Darrow et al 2016, Huisman-van Dijk et al 2016). These studies are useful in identifying cross-disorder phenotypes (Darrow et al 2016); however, subtle but important disorder-specific patterns may not be discernable in cross-disorder studies because the strong internal cohesion of any single group of symptoms (e.g., tics) can lead to a somewhat over-simplified cross-disorder model, thus prohibiting further investigation of potentially relevant, but less dominant, symptom subgroups. Thus, there is utility in examining specific symptom types (e.g., tics, OCD symptoms, and ADHD symptoms) separately, providing a nuanced characterization that complements the cross-disorder approach. For example, we conducted both cross-disorder analyses (Darrow et al 2016) and a separate tic-only analysis in the same TS family sample (Hirschtritt et al 2016). The cross-disorder analysis yielded a tic symptom group, an OCD symptom group, and symmetry and disinhibition symptom groups that included both tics and OC symptoms. In contrast, the tic-only analysis identified six tic symptom subgroups that paralleled the somatotopic representation of the somatosensory cortex, a finding that was not identified in the larger cross-disorder analysis, but which has potential relevance for future etiological studies.
As with the tic-only analysis, separate examinations of the patterns of OCD and ADHD symptoms in TS families may also be useful, given the substantial comorbidity and likely genetic pleiotropy between TS, OCD and ADHD. Thus, in this report, to clearly elucidate the complex relationships of OCD and ADHD symptoms in TS, we used factor and latent class analyses to identify OCD and ADHD symptom patterns and subsequently examined the heritability and clinical associations of these symptom subgroups in a well-phenotyped sample of subjects with TS and their family members.
We hypothesized that, in addition to finding empirically based OCD- and ADHD-symptom dimensions similar to those found in non-TS samples, we would identify additional, unique heritable symptom patterns with specific relevance to TS. We also hypothesized that individual OCD and ADHD symptom subgroups would be differentially associated with other clinically relevant characteristics, such as comorbid psychiatric disorders and/or symptom severity. For example, based on our previous work we hypothesized that we would identify specific symmetry and disinhibition dimensions from within the OCD and ADHD symptoms that would be more closely associated with TS than with OCD or ADHD.
Methods
Sample
Sample characteristics and assessments used in this study are described in detail elsewhere (Darrow et al 2016, Hirschtritt et al 2015, Hirschtritt et al 2016). Subjects included 3,494 individuals from 1,365 families collected by the multi-site Tourette Syndrome Association International Consortium for Genetics (TSAICG) for genetic studies; all participants provided written informed consent (parental consent and written assent was obtained for individuals <18 years). This study was approved by the Institutional Review Boards of all participating sites. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
The sample included 283 sib-pair families (two or more TS-affected siblings plus parents) and 1,082 trio families (TS-affected individuals plus both parents). In addition to parents and TS-affected sibling pairs, there were 91 TS-unaffected siblings; 26 families had extended family members (grandparents, uncles or aunts, and cousins). Sib-pair families were excluded if both parents had TS, chronic tics, or OCD; no such exclusions were made for trio families. Inclusion criteria for probands (the first identified TS-affected individual in a given family) were: age ≥6 years, established TS diagnosis, and availability of living parents for family-based analyses. Exclusion criteria included: intellectual disability, and tics caused by neurologic disorders other than TS. All analyses except for the exploratory factor analysis used all family members with sufficient data, independent of TS diagnosis.
Procedure
Research staff assessed demographic data, tic severity, OCD and ADHD symptoms using the TSAICG Tic and Comorbid Symptom (TICS) Inventory (Tourette Syndrome Association International Consortium for Genetics 1999, Tourette Syndrome Association International Consortium for Genetics 2007), which also includes detailed checklists of lifetime-encountered OCD and ADHD symptoms, age-of-onset, and (for OCD symptoms only) global severity (Online Supplement 1).
Other psychiatric diagnoses were assessed using the Structured Clinical Interview for the DSM (First et al 1995) or the Schedule for Affective Disorders and Schizophrenia-Lifetime Version, Modified for the Study of Anxiety Disorders (Fyer et al 1985) for adults and the Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (Kaufman et al 1997) and Epidemiologic Version (Polanczyk et al 2003) for children. These data were only collected during the first wave of recruitment and were available for ~19% of participants. We established all psychiatric diagnoses using a best-estimate approach (Hirschtritt et al 2015, Leckman et al 1982). Psychiatric diagnoses other than TS, OCD, and ADHD were combined into categories; mood (depression and bipolar disorder), anxiety (panic, generalized anxiety, social phobia, and separation anxiety), and disruptive behavior disorders (conduct disorder and oppositional defiant disorder).
Statistical Analyses
Exploratory factor analyses (EFA).
We performed separate EFA on OCD and ADHD symptom data in probands using robust weighted least squares estimation for dichotomous variables (Muthén et al 1997) and oblique rotation (geomin), which allows for correlation among factors, in MPlus version 7.1 (Muthén and Muthén 1998–2012). We subsequently used orthogonal (varimax) rotation as a secondary sensitivity analysis. As the orthogonal rotation yielded similar results, they are not presented here. We limited data to probands to examine independent cases. The best-factor solution was chosen using a stepwise approach based on established criteria (Preacher et al 2013). First, we only considered models containing eigenvalues ≥1. Second, we examined the root mean square error of approximation (RMSEA) (Loehlin 2004, Raykov and Marcoulides 2006) and chi-square difference test (Floyd and Widaman 1995) values among models to provide quantitative measures of fit. Third, we prioritized models with minimal “cross-loading” (i.e., had fewer variables that loaded on ≥1 factor at ≥.40), and finally, we assessed the clinical applicability and interpretability of the models. Within each model, we retained items if factor loadings were ≥.40; items that loaded on ≥2 latent factors at ≥.40 were assigned to the factor with the higher loading. Items with loadings <.40 were excluded from the final model. We assessed the internal consistency of each factor using Cronbach’s alpha and calculated mean factor sum scores for each factor in each participant by dividing the number of items the individual endorsed by the total number of items answered for each factor (Katerberg et al 2010). These factor sum scores were used in the latent class analysis and in all clinical and heritability analyses.
Using generalized estimating equation models clustering on family and controlling for age at interview, we tested the association between OCD and ADHD factor sum scores and lifetime diagnoses of TS, OCD, ADHD, anxiety, mood, and disruptive behavior disorders; sex; TS, OCD, and ADHD age-of-onset; and tic and OCD severity. To account for multiple testing, we set our selection threshold to P<.005 (.05/10, the total number of OCD and ADHD factors).
Latent class analyses (LCA).
We conducted latent class analysis in MPlus version 7.1, and fit latent classes to EFA-derived ADHD and OCD factor sum scores among all participants. We chose the best-fit models based on those with the lowest Bayesian Information Criterion (Schwarz 1978) and a significant Lo, Mendel, and Rubin likelihood ratio test (P<.05) (Lo et al 2001). If these criteria left the model choice unclear, we examined the clinical interpretability of the solutions. We performed an additional step by fitting latent classes to EFA-derived ADHD and OCD factor sum scores among probands only to examine the robustness of the LCA solution. For each latent class model, we added classes until the model failed to converge. In all LCA models, the probability distributions for class membership (ranging from 0 [no probability] to 1 [100% probability]) approximated a binary distribution; therefore, we assigned each individual to his/her most likely class. Class membership was categorical and mutually exclusive. We next examined the rates of psychiatric comorbidity in each class using the auxiliary variable function of MPlus, which accounts for uncertainty in class membership.
Heritability.
We calculated heritability estimates for factor sum scores using the Sequential Oligogenic Linkage Analysis Routine statistical package (Almasy and Blangero 1998), covarying for age, sex, and sex×age. We inverse-normalized all factor sum scores to account for any skewing in the distributions of the raw data. We first examined the heritability of the OCD and ADHD factors individually. To estimate the genetic relationships between these symptom-based phenotypes and the core diagnoses (TS, OCD, and ADHD), we then conducted heritability analyses for TS, OCD, and ADHD, covarying for all OCD and ADHD factors (separately for both sets of factors). Because TS, OCD, and ADHD are heritable in TS-affected families (Hirschtritt et al 2015), we included the factors as covariates in the heritability analysis for each diagnosis to partition out any heritability in the model that was due to the symptom factor. We then used log-likelihood and associated P-values (representing the model with and without the given factor) to determine which factors significantly changed the estimated heritability of each diagnosis, thus indicating a significant genetic relationship between the factor and the diagnosis.
Results
Sample Characteristics
The final sample included 1,191 probands (254 from sib-pair families, 937 from trios) and 3,494 total participants (1,147 from sib-pair families and 2,347 from trios). Missing data patterns did not differ by site. All 1,191 probands (by definition) and 28.2% of family members had TS (1,841 participants, 52.7% of the total sample). 34.2% of participants (probands and family members) had OCD, while 31.5% had ADHD (Supplemental Table 1).
EFAs
EFA of OCD symptoms.
Models containing up to eleven factors had eigenvalues ≥1.0 (Supplemental Figure S1). We only examined models with up to 8 factors, as those with >8 had one or more factor(s) without any significant loadings. All models had RMSEA values <.05, and the chi-square difference tests were significant for all comparisons up to the 8-factor model (Supplemental Table S2). We chose the 8-factor model for further examination, which separated items into: 1) doubts/scrupulosity, 2) symmetry/exactness, 3) contamination/cleaning, 4) aggressive urges, 5) fear-of-harm, 6) need for sameness, 7) superstitions, and 8) hoarding (Table 1, Supplemental Table S3). All factors were significantly correlated with one another (correlations between .21 and .56, all p values ≤.05), except the need for sameness factor, which did not correlate with any of the other OCD symptom factors (Supplemental Table S4).
Table 1.
Factor loadings and internal consistency for OCD exploratory factor model
| F1 | F2 | F3 | F4 | F5 | F6 | F7 | F8 | |
|---|---|---|---|---|---|---|---|---|
| Doubts/Scrupulosity | Symmetry/Exactness | Contamination | Aggressive urges | Fear-of-harm | Need for sameness | Superstitions | Hoarding | |
| Cronbach’s alpha | 0.76 | 0.85 | 0.76 | 0.77 | 0.65 | 0.60 | 0.72 | 0.75 |
| Item | ||||||||
| Checks that did not make mistakes | 0.81 | 0.27 | 0.03 | −0.13 | −0.10 | 0.00 | −0.03 | 0.02 |
| Re-reads or re-writes things | 0.60 | 0.50 | −0.12 | 0.01 | 0.00 | −0.01 | −0.18 | 0.04 |
| Checks that did not or will not harm others | 0.60 | 0.00 | 0.08 | 0.17 | 0.04 | 0.21 | 0.04 | −0.02 |
| Needs to tell, ask, or confess things | 0.57 | 0.05 | 0.07 | 0.11 | 0.12 | 0.19 | −0.01 | −0.05 |
| Is excessively concerned with right or wrong (morality) | 0.54 | 0.01 | 0.16 | −0.03 | 0.05 | 0.07 | 0.17 | 0.01 |
| Is concerned with upsetting thoughts having to do with God, religious teachings or beliefs | 0.51 | −0.13 | 0.10 | 0.16 | 0.04 | −0.19 | 0.08 | 0.08 |
| Has mental rituals (other than checking or counting) done intentionally to feel better | 0.40 | 0.12 | 0.02 | 0.07 | 0.05 | −0.12 | 0.24 | 0.10 |
| Has obsessions about symmetry | 0.00 | 0.83 | 0.08 | 0.03 | 0.02 | −0.09 | 0.02 | −0.04 |
| Needs certain things to be symmetrical | 0.02 | 0.78 | 0.07 | 0.08 | −0.06 | −0.04 | 0.04 | −0.09 |
| Often has thoughts about lining things up | −0.09 | 0.78 | 0.00 | −0.01 | 0.17 | 0.06 | −0.03 | 0.12 |
| Has ordering or arranging compulsions | 0.02 | 0.75 | 0.02 | 0.03 | 0.05 | 0.20 | 0.03 | 0.05 |
| Has obsessions about exactness | 0.25 | 0.66 | −0.02 | −0.08 | 0.09 | 0.06 | 0.00 | 0.07 |
| Needs to have certain things evened-up | 0.03 | 0.61 | 0.01 | 0.08 | −0.02 | −0.39 | 0.16 | −0.06 |
| Often has thoughts about evening things up | −0.05 | 0.61 | 0.00 | 0.08 | 0.02 | −0.46 | 0.14 | 0.06 |
| Has counting compulsions | 0.28 | 0.48 | −0.03 | 0.01 | −0.01 | −0.08 | 0.05 | 0.03 |
| Needs to repeat routine activities (like going in and out of a doorway or getting up and down from a chair) | 0.15 | 0.43 | 0.03 | 0.01 | 0.09 | −0.08 | 0.15 | −0.02 |
| Does other things to prevent or remove contact with contaminants | −0.01 | 0.14 | 0.82 | 0.06 | −0.01 | −0.02 | −0.04 | −0.06 |
| Is concerned with dirt or germs | −0.05 | 0.15 | 0.80 | 0.02 | 0.09 | 0.06 | 0.01 | 0.01 |
| Is concerned will get ill because of contamination | 0.01 | −0.07 | 0.78 | −0.08 | 0.19 | −0.07 | 0.13 | −0.01 |
| Is concerned with illness or disease | 0.18 | −0.08 | 0.56 | −0.03 | 0.12 | −0.02 | 0.21 | 0.06 |
| Is concerned or disgusted with bodily waste or secretions (like urine, feces, or saliva) | 0.06 | 0.11 | 0.56 | 0.21 | −0.01 | −0.07 | −0.02 | 0.01 |
| Is excessively concerned with environmental contaminants (like asbestos, radiation, or toxic waste) | 0.31 | −0.03 | 0.55 | 0.02 | −0.09 | −0.17 | 0.09 | 0.05 |
| Is excessively concerned with animals (like insects) | 0.00 | 0.16 | 0.49 | −0.01 | −0.06 | 0.08 | −0.03 | 0.24 |
| Is bothered by sticky substances or residues | 0.02 | 0.24 | 0.48 | 0.01 | 0.05 | 0.04 | −0.12 | −0.02 |
| Has experienced unreasonable urges to be destructive | −0.12 | 0.09 | 0.05 | 0.87 | −0.02 | 0.04 | −0.05 | 0.08 |
| Has experienced urges to injure or mutilate others | −0.18 | −0.08 | 0.01 | 0.84 | 0.04 | 0.21 | 0.02 | 0.06 |
| Has experienced unreasonable urges to offend others | −0.06 | −0.02 | 0.04 | 0.82 | −0.03 | 0.09 | 0.03 | 0.07 |
| Has experienced unreasonable urges to injure self | 0.04 | 0.01 | 0.04 | 0.67 | 0.18 | −0.14 | −0.05 | 0.01 |
| Has experienced unreasonable urges to do sudden and reckless things (behaviors) | 0.03 | 0.16 | −0.05 | 0.64 | 0.05 | −0.05 | 0.06 | −0.06 |
| Fears acting on an unwanted impulse | 0.18 | 0.09 | −0.02 | 0.53 | 0.26 | −0.06 | −0.02 | −0.04 |
| Has experienced a strong need to explore surroundings | 0.05 | 0.03 | −0.10 | 0.41 | −0.06 | 0.11 | 0.04 | 0.38 |
| Fears blurting out obscenities | 0.18 | 0.06 | −0.04 | 0.41 | 0.32 | −0.06 | −0.11 | −0.03 |
| Fears will steal things | 0.04 | −0.20 | 0.05 | 0.40 | 0.06 | −0.23 | 0.09 | 0.32 |
| Fears that might harm self | −0.07 | 0.04 | 0.22 | 0.01 | 0.83 | 0.03 | 0.02 | −0.01 |
| Fears that might harm other people | 0.12 | −0.03 | −0.02 | 0.01 | 0.74 | 0.01 | 0.15 | 0.07 |
| Takes measures (other than checking) to prevent harm to self or others, or terrible consequences | 0.32 | 0.05 | 0.26 | 0.02 | 0.53 | 0.04 | −0.05 | −0.05 |
| Needs to touch, tap, or rub things | 0.08 | 0.30 | 0.04 | 0.05 | 0.41 | −0.14 | 0.02 | 0.04 |
| Has to keep a strict timetable or routine for doing ordinary activities | −0.03 | 0.26 | 0.10 | −0.01 | 0.00 | 0.51 | 0.37 | 0.10 |
| Has to do things the same way every time | 0.02 | 0.41 | −0.01 | 0.01 | 0.01 | 0.47 | 0.33 | 0.09 |
| Has unreasonable, silly thoughts that may influence the outcome of some events if does certain things | 0.02 | −0.02 | −0.07 | 0.05 | 0.27 | 0.05 | 0.84 | −0.01 |
| Has silly thoughts that can influence the outcome of some events if does certain things | 0.00 | 0.00 | 0.01 | 0.03 | 0.23 | −0.01 | 0.82 | −0.16 |
| Has superstitious fears | 0.05 | 0.06 | 0.16 | 0.02 | −0.05 | −0.26 | 0.64 | 0.04 |
| Has superstitious behaviors | −0.03 | 0.11 | 0.10 | 0.02 | 0.06 | −0.23 | 0.54 | 0.07 |
| Has colors with special significance | 0.07 | 0.03 | −0.02 | 0.20 | −0.04 | −0.05 | 0.50 | 0.05 |
| Has lucky or unlucky numbers | 0.00 | 0.19 | 0.12 | −0.07 | 0.03 | −0.21 | 0.44 | 0.16 |
| Has obsessions about hoarding or saving things | 0.04 | 0.01 | 0.00 | 0.04 | 0.01 | 0.02 | 0.01 | 0.93 |
| Has compulsions to hoard or collect things | 0.00 | 0.07 | 0.03 | 0.06 | −0.02 | 0.01 | −0.09 | 0.90 |
| Fears losing things | 0.22 | 0.08 | 0.12 | 0.08 | 0.03 | −0.02 | 0.12 | 0.41 |
Items that loaded on 2 latent factors ≥0.40 were assigned to the factor with the higher loading.
All factors except superstitions were significantly associated with OCD severity, although only symmetry/exactness and hoarding were significantly associated with OCD diagnosis (Table 2). The symmetry/exactness, aggressive urges, and fear-of-harm factors were associated with a TS diagnosis, and the aggressive urges and hoarding factors were associated with an ADHD diagnosis. Symmetry/exactness was also associated with increased tic severity, while aggressive urges were associated with DBD diagnoses, male sex, earlier TS age-of-onset and increased tic severity. Notably, the contamination factor was only significantly associated with anxiety disorders and with OCD severity. None of the OCD factors demonstrated significant association with mood disorders, or with age-of-onset of OCD or ADHD.
Table 2.
Association of OCD factor sum scores with clinical characteristics among individuals with TS and their family members
| OCD 8-factor solution | ADHD 2-factor solution | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Clinical characteristic | F1 Doubts/scrupulosity | F2 Symmetry/exactness | F3 Contamination | F4 Aggressive urges | F5 Fear-of-harm | F6 Need for sameness | F7 Superstitions | F8 Hoarding | F1 Inattentive | F2 Hyperactive/Impulsive |
| Psychiatric comorbiditya | ||||||||||
| TS | 0.5 (0.2, 1.2) | 5.1 (2.4, 10.6)*** | 0.3 (0.1, 0.7) | 7.2 (2.6, 19.9)** | 9.8 (4.2, 23.0)*** | 1.4 (0.8, 2.2) | 0.8 (0.4, 1.9) | 1.4 (0.9, 2.3) | 3.2 (2.2, 4.6)*** | 4.3 (2.8, 6.6)*** |
| OCD | 3.2 (1.3, 7.9) | 3.2 (1.6, 6.7)* | 3.3 (1.3, 8.5) | 1.6 (0.6, 4.2) | 1.0 (0.4, 2.2) | 1.6 (1.0, 2.5) | 1.3 (0.5, 3.4) | 2.0 (1.3, 3.2)* | 3.3 (2.5, 4.4)*** | 2.5 (1.9, 3.4)*** |
| ADHD | 0.8 (0.4, 1.6) | 0.5 (0.3, 1.0) | 1.2 (0.6, 2.4) | 12.1 (5.9, 2.4)*** | 1.2 (0.6, 2.2) | 1.6 (1.1, 2.4) | 0.5 (0.2, 1.0) | 2.1 (1.4, 2.9)*** | 46.9 (31.8, 68.9)*** | 21.3 (14.1, 32.4)*** |
| Anxiety | 2.4 (1.2, 5.1) | 0.5 (0.3, 1.0) | 3.9 (1.9, 7.9)*** | 0.8 (0.4, 1.8) | 1.2 (0.6, 2.5) | 1.0 (0.6, 1.4) | 1.2 (0.6, 2.5) | 1.1 (0.8, 1.0) | 1.9 (1.3, 2.7)** | 1.3 (0.9, 2.0) |
| Mood | 1.2 (0.6, 2.6) | 1.0 (0.5, 1.8) | 1.7 (0.8, 3.5) | 1.7 (0.8, 3.5) | 0.7 (0.4, 1.4) | 0.8 (0.5, 1.2) | 1.8 (0.9, 3.6) | 1.0 (0.7, 1.4) | 1.8 (1.2, 2.6)* | 0.8 (0.5, 1.2) |
| Disruptive behavior | 0.3 (0.1, 1.0) | 0.6 (0.2, 1.5) | 1.9 (0.7, 5.3) | 19.6 (6.7, 55.6)*** | 1.0 (0.5, 1.8) | 1.0 (0.5, 1.8) | 0.5 (0.1, 1.8) | 1.6 (0.9, 1.0) | 2.8 (1.5, 5.2)* | 3.0 (1.6, 5.8)** |
| Sexa, b | 1.7 (0.9, 2.9) | 1.4 (0.9, 2.1) | 1.7 (1.0, 3.0) | 0.3 (0.2, 0.6)** | 0.5 (0.3, 0.9) | 0.8 (0.6, 1.1) | 1.9 (1.1, 3.2) | 0.9 (0.7, 1.2) | 0.6 (0.5, 0.8)** | 0.7 (0.5, 0.9) |
| Age at interviewc | 1.9 × 104 (3.7 × 10−2, 9.4 × 109) | 2.4 × 103 (5.0 × 10−2, 1.2 × 108) | 7.2 × 102 (1.5 × 10−4, 3.4 × 107) | 7.1 × 10−3 (1.5 × 10−8, 3.3 × 103) | 1.3 × 10−7 (8.7 × 10−13, 1.8 × 10−2) | 7.1 × 10−5 (5.3 × 10−8, 9.4 × 10−2) | 1.2 × 106 (5.0, 3.1 × 1011) | 1.9 (2.1 × 10−3, 1.7 × 103) | 1.0 × 10−6 (8.0 × 10−9, 1.3 × 10−4)*** | 2.2 × 10−5 (9.5 × 10−8, 5.2 × 10−3)** |
| TS age-of-onsetc | 3.5 (1.4, 9.0) | 1.6 (0.8, 3.5) | 0.9 (0.4, 2.3) | 0.2 (0.1, 0.5)** | 0.3 (0.1, 0.6) | 0.8 (0.5, 1.3) | 5.1 (2.0, 12.6)** | 1.0 (0.6, 1.6) | 0.6 (0.4, 0.9) | 0.6 (0.3, 0.7)** |
| Tic severityc | 0.2 (0.1, 0.7) | 17.0 (6.2, 26.8)*** | 0.2 (0.1, 0.7) | 12.2 (3.6, 41.5)*** | 59.0 (19.0, 182.7)*** | 1.3 (0.7, 2.6) | 0.0 (0.0, 0.1) | 1.2 (0.6, 2.2) | 74.3 (42.2, 131.0)*** | 16.9 (9.0, 31.8)*** |
| OCD age-of-onsetc | 1.5 (0.1, 17.5) | 0.2 (0.0, 2.3) | 0.1 (0.0, 1.5) | 0.3 (0.0, 4.2) | 0.7 (0.1, 5.8) | 0.7 (0.2, 3.1) | 0.5 (0.0, 5.4) | 0.7 (0.2, 2.7) | 0.3 (0.1, 1.0) | 0.4 (0.1, 1.4) |
| OC severityc | 17.1 (8.8, 33.3)*** | 13.9 (8.0, 23.9)*** | 8.5 (4.4, 16.7)*** | 21.1 (10.9, 40.8)*** | 3.5 (1.9, 6.5)*** | 1.9 (1.3, 2.7)* | 1.7 (0.9, 3.2) | 1.7 (1.2, 2.4)* | 6.3 (4.1, 10.0)*** | 10.1 (6.2, 16.5)*** |
| ADHD age-of-onsetc | 1.8 (0.7, 4.5) | 0.9 (0.4, 2.1) | 0.5 (0.2, 1.4) | 0.7 (0.3, 1.6) | 1.0 (0.4, 2.4) | 1.0 (0.6, 1.7) | 0.9 (0.3, 2.5) | 1.5 (0.9, 2.5) | 1.6 (1.0, 2.5) | 0.3 (0.2, 0.5)*** |
ADHD, attention-deficit/hyperactivity disorder; OC(D), obsessive-compulsive (disorder); TS, Tourette syndrome Generalized estimating equation models, clustering on family, simultaneously covary for all OCD or ADHD factor sum scores, age at interview (except in the model in which age at interview is the outcome), and OC severity (except in the model in which OC severity is the outcome), and define each clinical characteristic as the outcome variable in separate models.
Values represent odds ratios (95% confidence interval),
Odds ratios > 1 indicate higher odds of female sex,
Values represent standardized beta coefficient (95% confidence interval)
P < .005,
P < .001,
P < .0001
EFA of ADHD symptoms.
We fit models with up to 4 factors using the 18 ADHD symptoms based on RMSEA scores and clinical utility of the models (Supplemental Table S5, Supplemental Figure S1). A 2-factor model (Supplemental Table S6) (inattentive and hyperactive/impulsive symptoms) was the best fit, mirroring the DSM-5 categorization of ADHD symptoms.
Both ADHD factors were significantly associated with TS, OCD, ADHD, and DBD (Table 2), and with tic and OC symptom severity. The inattentive factor was also significantly associated with anxiety and mood disorders and with male sex, while the hyperactive/impulsive factor was associated with earlier TS and ADHD age-of-onset. Neither ADHD factor demonstrated significant association with OCD age-of-onset.
Heritability analyses
Table 3 presents the heritabilities of the individual OCD and ADHD factors, and outlines the genetic relationships between the factors and TS, OCD, and ADHD. Heritability for OCD factors ranged from .19 to .37 (all P-values≤4×10−12; symmetry/exactness had the highest heritability, h2r=.37, SE=.03), and need for sameness the lowest (h2r=.20, SE=.03). The ADHD factors had heritabilities of .41 (inattentive, SE=.03, P=1.0×1−38) and .38 (hyperactive/impulsive, SE=.03, P=8.5×10−34). While the loglikelihoods suggest that both ADHD factors are genetically related to TS, OCD, and ADHD (e.g., the heritabilities of ADHD, TS, and OCD were significantly reduced when the ADHD factors were included as covariates), the results for the OCD factors suggested more specific relationships. Although the heritability models for OCD changed when the OCD factors were included as covariates, the models for TS changed significantly with the addition of three OCD factors (symmetry/exactness, aggressive urges, and fear-of-harm), suggesting that these and not the other OCD factors are genetically related to TS. Similarly, only two OCD factors (aggressive urges and hoarding) significantly modified ADHD heritability estimates. Figure 1 shows a schematic of the relationships, both clinical and genetic, between the OCD factors and psychiatric diagnoses, including those that are OCD-specific, those associated with both OCD and TS, those that are associated with OCD and anxiety, and those that are associated with OCD, TS, and ADHD.
Table 3.
Heritability of OCD and ADHD factors and their modification of the heritability of TS, OCD, and ADHD diagnoses
| Heritability of diagnoses significantly changed by inclusion of given factor as a covariate | ||||||
|---|---|---|---|---|---|---|
| Factor | h2ra | SE | P-value | TS | OCD | ADHD |
| OCD factors: | ||||||
| OCD F1 (doubts/scrupulosity) | .35 | .03 | 1.25 × 10−27 | X | ||
| OCD F2 (symmetry/exactness) | .37 | .03 | 1.24 × 10−29 | X | X | |
| OCD F3 (contamination) | .31 | .03 | 1.06 × 10−22 | X | ||
| OCD F4 (aggressive urges) | .31 | .03 | 3.89 × 10−28 | X | X | X |
| OCD F5 (fear-of-harm) | .24 | .03 | 3.20 × 10−15 | X | X | |
| OCD F6 (need for sameness) | .20 | .03 | 5.26 × 10−12 | X | ||
| OCD F7 (superstitions) | .23 | .03 | 1.27 × 10−12 | X | ||
| OCD F8 (hoarding) | .33 | .03 | 3.74 × 10−28 | X | X | |
| ADHD factors: | ||||||
| ADHD F1 (inattentive) | .41 | .03 | 1.03 × 10−38 | X | X | X |
| ADHD F2 (hyperactive/impulsive) | .38 | .03 | 8.54 × 10−34 | X | X | X |
ADHD, attention-deficit/hyperactivity disorder; h2r, estimated heritability value; OCD, obsessive-compulsive disorder; SE, standard error; TS, Tourette Syndrome.
‘X’ indicates P≤0.05, uncorrected.
Controlling for age, sex, and age×sex
Figure 1:
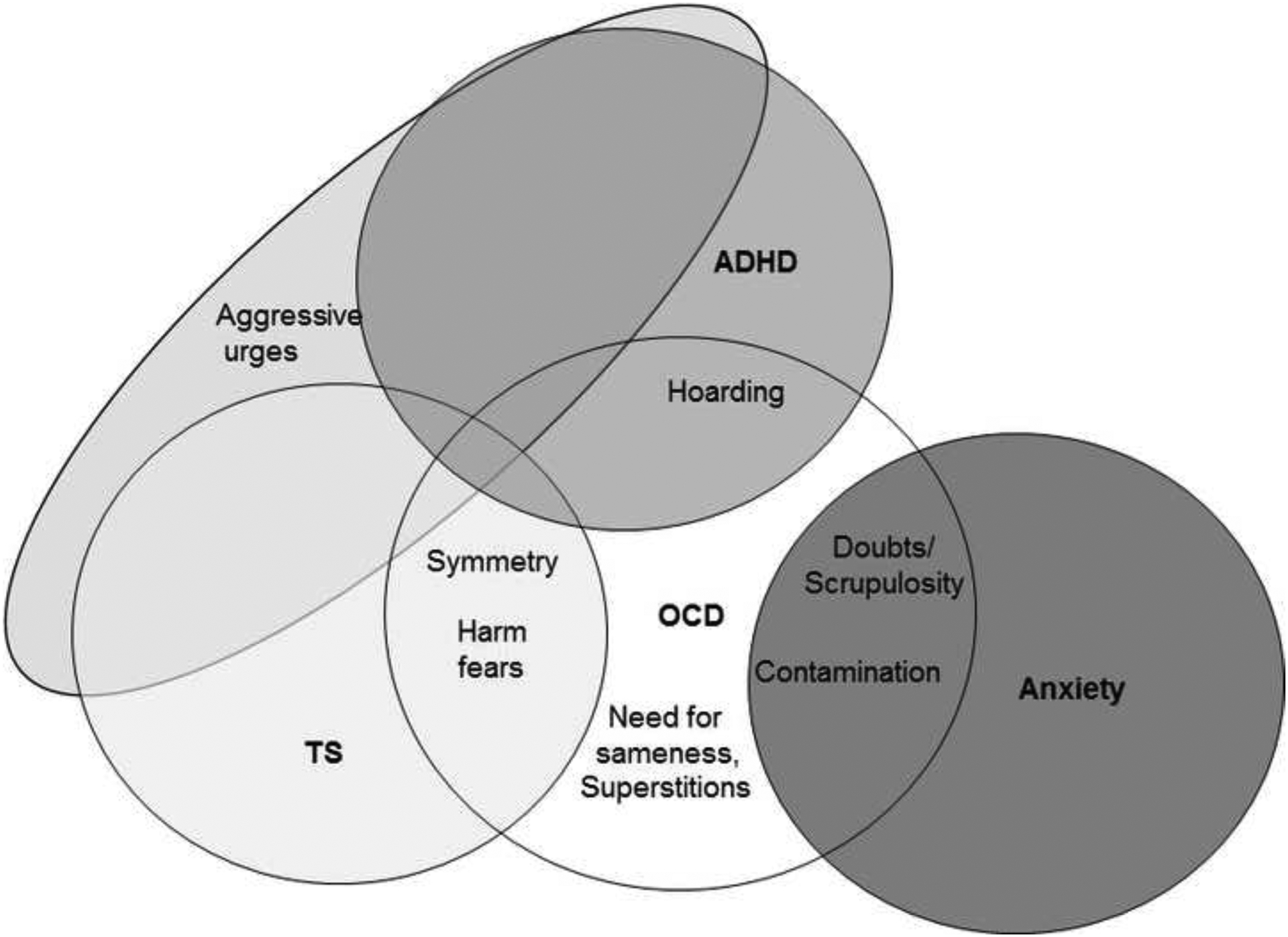
Schematic representation of the relationships between the OCD factors and psychiatric diagnoses.
LCAs
LCA of EFA-based ADHD and OCD factor sum scores.
The results of the nested LCA, incorporating both ADHD and OCD factor sum scores for all participants supported a 3-class solution: [LC1] few symptoms, [LC2] OCD&ADHD symptoms, and [LC3] symmetry/exactness, hoarding, and ADHD symptoms (Supplemental Table S7; Supplemental Figure S2). The probability of endorsement was <30% and <10% for the ADHD and OCD factors, respectively, in LC1, and >50% for all factors in LC2. The probability of endorsement was >40% for the symmetry/exactness, hoarding, inattentive, and hyperactive/impulsive factors for LC3. Significant differences in comorbidity rates were observed between classes (Figure 2) for OCD (χ2=2454.35, df=2, P≤0.001), ADHD (χ2=1943.89, df=2, p≤0.001), mood disorders (χ2=61.61, df=2, P≤0.001), anxiety disorders (χ2= 86.69, df=2, P≤0.001), and disruptive behavior disorders (χ2=21.16, df=2, P≤0.001). LC1 (few/no OCD/ADHD symptoms) had the lowest rates of all psychiatric disorders; the most common was TS, endorsed by ~40% of individuals in LC1. LC2 (OCD&ADHD symptoms) was characterized by high rates of all psychiatric disorders, with OCD present in >90%, TS present in >80%, and ADHD present in 50%. This class also had higher rates of mood, anxiety, and disruptive behavior disorders than LC1 and LC3 (symmetry, exactness, hoarding and ADHD symptoms). LC3 was characterized by high rates of TS, OCD, and ADHD (over 75% of individuals in this class had these three disorders) and comparatively low rates of other psychiatric diagnoses.
Figure 2.
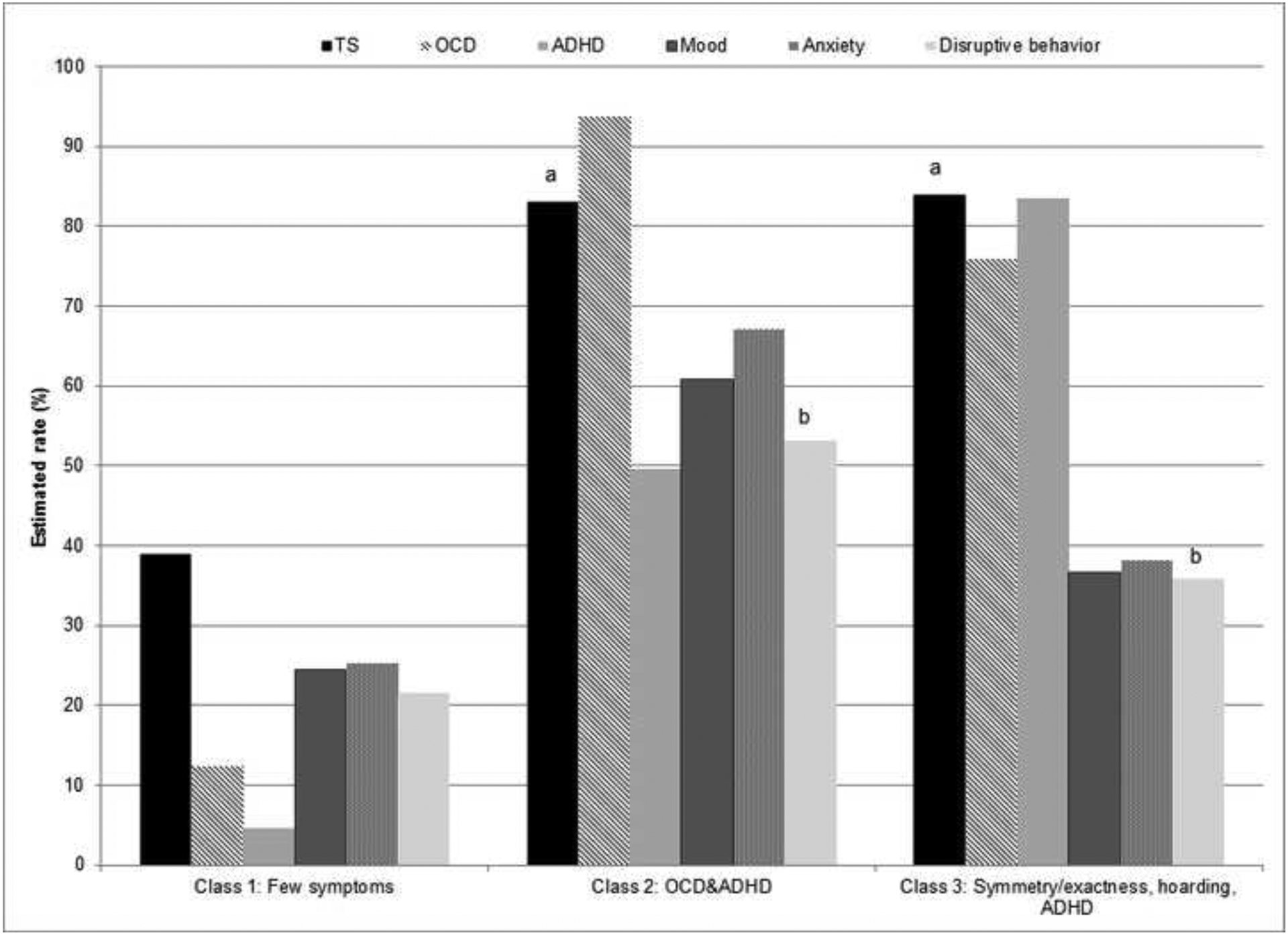
Rates of comorbid psychiatric disorders among latent classes using OCD and ADHD factor sum scores in probands and family members.
ADHD, attention-deficit/hyperactivity disorder; OCD, obsessive-compulsive disorder
Letters above bars indicate pairwise comparisons that are not significantly different at P<0.05.
The results of the LCA limited to probands only also supported a 3-class solution. In this solution, the “symmetry/exactness, hoarding, and ADHD symptoms” and “ADHD&OCD symptoms” classes paralleled those derived from the entire sample; the remaining class was similar to the original “few symptoms” class, but had higher rates of ADHD symptoms (46% had inattentive symptoms and 36% had hyperactive/impulsive symptoms) (data not shown).
Discussion
Although OCD, ADHD, and TS are hypothesized to share underlying genetic factors (Davis et al 2013, Hirschtritt et al 2016, McGrath et al 2014), the reasons behind their significant comorbidity, and the clinical and etiological relationships between them, are complex and not yet clearly elucidated. This study extends upon previous work (Cavanna et al 2011, Darrow et al 2016, Eapen et al 2004, Grados and Mathews 2009, Hirschtritt et al 2016, Huisman-van Dijk et al 2016, Storch et al 2004) to examine ADHD and OCD symptoms separately using factor analysis, and jointly, using latent class analysis, in a sample of TS families. Taken together, our results both confirm and extend the growing body of literature that suggests that individual OCD symptom groups are differentially associated with specific psychopathologies, while ADHD symptoms may represent more general global underlying psychopathology.
We identified eight OCD symptom subgroups (instead of the four or five typically identified in OCD samples (Bloch et al 2008)), some of which appear to be differentially related to TS (symmetry/exactness, fear-of-harm), ADHD (hoarding), and anxiety disorders (doubts/scrupulosity, contamination), some of which are OCD-specific (superstitions, need for sameness), and one that appears to be related to multiple manifestations of psychopathology in this sample (aggressive urges). In contrast, the ADHD factor analysis identified two symptom subgroups that parallel the DSM-5 classifications (inattentive and hyperactive/impulsive symptoms) (Collett et al 2000, Dumenci et al 2004, Pillow et al 1998, Toplak et al 2009) and are also globally associated with measures of increased psychopathology. We discuss each of these observed patterns below.
Tics:
Two of the eight identified OCD factors (symmetry/exactness and fear-of-harm) were clinically and genetically related to TS, as indicated by the change in TS heritability when either factor was added as a covariate to the model. One of these, symmetry/exactness, not only replicates and expands on earlier work in this sample that also found a relationship between symmetry symptoms and tics (Darrow et al 2016, Hirschtritt et al 2016), but is also in line with the new DSM-5 classification system that recognizes a specific tic-related subtype of OCD (Leckman et al 2010). The symmetry/exactness factor had the highest internal reliability and heritability of all the OCD factors, and these symptoms were also a core feature of LC2, suggesting that this phenotype is robust and of relevance to genetic studies of TS. Previous studies of TS samples also identified a relationship between tics and symmetry symptoms (Darrow et al 2016, Huisman-van Dijk et al 2016), and recent work in the current sample indicates that symmetry symptoms in the absence of tics are associated with TS genetic susceptibility but not with OCD genetic susceptibility (Darrow et al 2016).
The other factor that was genetically and clinically associated with TS was fear-of-harm. These symptoms, which include fears of harming oneself or others, taking measures to prevent harm, and touching, tapping and rubbing, typically cluster with aggressive urges and taboo fears in OCD samples (Bloch et al 2008, Katerberg et al 2010). However, our analysis suggests that further investigation of these symptoms as a separate phenotype in individuals with TS may also be important. Fears-of-harm were among the most highly endorsed OCD symptoms in our TS sample, and also showed evidence of genetic relationships with TS.
OCD:
Two symptom subgroups, superstitions and need for sameness, were OCD-specific, and did not show any strong clinical or genetic associations with other psychiatric diagnoses or severity measures. Although often excluded from factor analyses as “miscellaneous” symptoms, superstitious symptoms have been previously identified as a distinct subgroup in at least one item-level factor analysis of OCD-affected individuals (Katerberg et al 2010). The current study indicated good heritability for the superstitions factor, although it had no genetic relationships with the other OCD symptom factors, or with OCD symptom severity. The second OCD-specific symptom subgroup, need for sameness, comprises two items, need to do things in exactly the same way every time, and the need to keep a strict timetable for routine activities. These symptoms are also typically not included in OCD factor analyses; in our cross-disorder analysis in this sample, the first symptom was included in the symmetry factor, while the second did not reliably load on any factor (Darrow et al 2016). It is likely that the sameness factor is more closely associated with obsessive-compulsive personality disorder than frank OCD, accounting for its nonsignificant correlation with the remaining OCD factors. Neither superstitions nor need for sameness were associated with OCD diagnosis or age-of-onset, nor with any other psychiatric diagnosis, although need for sameness was associated with increased OCD severity, and superstitions were associated with a later TS age-of-onset. In the latent class analysis, superstitions were the least frequently endorsed symptom group for all classes, while need for sameness was the third most commonly endorsed symptom group in LC3 (symmetry/exactness, hoarding and ADHD), and the fifth most frequently endorsed in LC2 (OCD&ADHD). In addition, while superstitions were positively correlated with other OCD symptom subgroups, need for sameness was not, suggesting that this symptom subgroup may tap into a different clinical phenomenon than the other OCD symptoms (e.g., obsessive compulsive personality disorder).
ADHD:
Only one OCD factor was associated with ADHD both clinically and genetically—hoarding (hoarding obsessions and compulsions and fear of losing things). Hoarding symptoms were also clinically and genetically related to OCD and to OCD symptom severity, although not to TS, anxiety, mood or DBDs. Hoarding symptoms were elevated in both LC2 and LC3, as were inattentive and hyperactive symptoms. These findings parallel recent literature that finds elevated rates of ADHD (Frost et al 2011) and executive dysfunction patterns that mimic ADHD (Tolin et al 2011) among individuals with hoarding symptoms; furthermore, there is complementary evidence supporting a genetic relationship between hoarding and ADHD (Fullana et al 2013). It should be considered that the presence of ADHD symptoms in this sample may, in part, result from an “executive-overload model” of OCD (Abramovitch et al 2015), in which disrupted neuronal maturation found in pediatric OCD leads to ADHD-like symptoms (Abramovitch et al 2013). This model has been used to explain the mis-diagnosis of ADHD in OCD pediatric samples.
Anxiety:
Two OCD symptom groups, are arguably among the most pathognomonic and recognizable OCD symptoms, were clinically associated with anxiety disorders—contamination/cleaning and doubts/scrupulosity (which includes religious and morality obsessions, checking for mistakes and for inadvertent harm, need to confess, mental rituals, and re-reading/re-writing). Although we do not have sufficient power to examine the genetic relationships between these factors and anxiety disorders, a recent twin study demonstrated strong genetic relationships between washing and religious/sexual obsessions (parallel to our contamination and doubts factors) and anxiety disorders (Lopez-Sola et al 2016).
Global psychopathology:
Finally, one OCD symptom group, aggressive urges, and both ADHD symptom subgroups were associated with multiple forms of psychopathology in our sample, and were genetically related to the three core diagnoses, TS, OCD, and ADHD. The OCD aggressive urges factor, which in this study is comprised primarily of unreasonable (ego-dystonic) urges to be destructive or harm one’s self or others, has been identified previously in TS samples (Alsobrook and Pauls 2002, Storch et al 2004), and parallels symptom subtypes identified in the tic-only analysis (which identified socially inappropriate or disinhibited tics) (Hirschtritt et al 2016) and the cross-disorder analysis (a disinhibition factor comprised of socially inappropriate tics plus aggressive and hoarding symptoms, but not ADHD symptoms) (Darrow et al 2016).
Both of the ADHD factors (inattentive and hyperactive/impulsive) were also non-specifically, and strongly, associated with the majority of the severity and age-of-onset measures of psychopathology, as well as with TS, OCD, ADHD, and DBD diagnoses (the inattentive factor was additionally associated with mood and anxiety disorders). ADHD symptoms were elevated in all three latent classes, although to a lesser extent in the “unaffected” class, LC1, and the heritability analyses suggested that both factors had strong genetic relationships with ADHD, TS, and OCD. As with the aggressive urges factor, this pattern suggests that ADHD symptoms, at least in this TS sample, may be manifestations of a global underlying psychopathology rather than being specific for any particular DSM-based categorical disorder (including ADHD). Together with previous tic-only and cross-disorder analyses (Darrow et al 2016, Hirschtritt et al 2016), the current findings also suggest a common underlying failure of top-down cognitive control represented by symptoms from all three diagnostic categories (e.g., multiple ADHD symptoms, copro- and echo-phenomena, aggressive obsessions). Specifically, evidence from functional neuroimaging and neuropsychological paradigms in ADHD (Friedman-Hill et al 2010), OCD (Zhang et al 2011), and TS (Wang et al 2011) suggest the presence of disrupted connectivity between various regions of the prefrontal cortex and posterior cortical regions that corresponds to dysregulated behavioral control (e.g., failure of dorsolateral prefrontal cortical inhibition of involuntary movements regulated by the basal ganglia in TS) (Arnsten and Rubia 2012).
Limitations
The data for this study were gathered over multiple years, and for ADHD, using different symptom surveys, and we only had psychiatric diagnoses for a subset of the sample. Nonetheless, we arrived at the conventional two-factor solution for ADHD that demarcated inattentive from hyperactive/impulsive symptoms, suggesting the robust nature of this factor model. Factor and latent class analyses are inherently subjective; however, the use of a priori criteria for choosing among models reduced the arbitrary nature of these psychometric techniques. Last, although we analyzed OCD and ADHD symptoms separately to identify subtle symptom patterns for future research, in TS families, OCD and ADHD are highly etiologically related to one another. Although it is possible that such relationships could confound our results, our previous cross-disorder analyses suggests that, in fact, OCD and ADHD symptoms factor separately, somewhat alleviating this concern.
Implications
This work suggests that OCD and ADHD symptom subgroups in TS families may represent markers for distinct underlying patterns of psychopathology. Symptom-based phenotypes could be exploited in future research to identify additional genes or gene pathways relevant to the etiology of neuropsychiatric disorders. For example, converging evidence from multiple studies suggests that OCD symmetry symptoms may represent a robust endophenotype of TS (rather than an endophenotype of OCD) that could be an independent target for genetic studies, whereas contamination and scrupulosity symptoms may be relevant to understanding the pathophysiology of anxiety disorders. Finally, the genetic overlap between OCD and TS in disinhibition symptoms supports further investigation of “top-down” cortical control in subsequent neuroimaging studies among family members with high familial TS loading. From a clinical perspective, the association between aggressive and superstitious symptoms (and to a lesser extent symmetry and fear-of-harm symptoms) and increased tic severity or earlier age-of-onset, and between contamination symptoms and increased risk for anxiety disorders may prove useful in predicting and monitoring the course of TS in children and adolescents. Additionally, the identification of contamination symptoms might then lead to ongoing monitoring for, and thus earlier identification of and intervention for subsequent anxiety disorders.
Supplementary Material
Acknowledgements
We wish to thank the families who participated in this research, the TSAICG study coordinators at each site for their assistance in study logistics, as well as Dr. Lea Davis (Division of Genetic Medicine, Department of Medicine, Vanderbilt University) for her advice on heritability analyses. An earlier version of this report was presented as a poster at the Society of Biological Psychiatry Annual Meeting on May 20, 2017 (San Diego, CA, USA).
Study funding
This work was supported by the National Institutes of Health, grant numbers R01MH096767 (“Refining the Tourette syndrome phenotype across diagnoses to aid gene discovery,” PI: Carol Mathews), U01NS040024 (“A genetic linkage study of GTS,” PI: David Pauls/Jeremiah Scharf), K23MH085057 (“Translational phenomics and genomics of Gilles de la Tourette syndrome,” PI: Jeremiah Scharf), K02MH00508 (“Genetics of a behavioral disorder: Tourette syndrome,” PI: David Pauls), and R01NS016648 (“A genetic study of GTS, OCD, and ADHD,” PI: David Pauls), and from the Tourette Syndrome Association.
Footnotes
Conflict of interest
Drs. Darrow, Hirschtritt, Illmann, Greenberg, McGrath, and Delucchi, and Ms. Osiecki reported no biomedical financial interests or potential conflicts of interest. Drs. Grados, Sandor, McMahon, Pauls, Dion, King, Budman, Cath, Lyon, and Lee received research support from the Tourette Association of America (TAA). Dr. Cath has received speakers’ honoraria from Pfizer BV. Dr. Budman reported funding for clinical research studies from Psyadon Pharmaceuticals, Assurex/TEVA Pharmaceuticals, Synchroneuron Pharmaceuticals, Neurocrine Pharmaceuticals, and Otsuka Pharmaceutical; she also serves as a consultant for Bracket and a speaker for the Tourette Association of America-Center for Disease Control Partnership. Dr. Lyon serves on advisory boards for GenePeeks, Inc. and Omicia, Inc., and has served a consultant to Good Start Genetics. Dr. Sandor has received unrestricted educational grants from Purdue and Shire, clinical research from Otsuka Pharmaceutical, a speaker fee from Purdue, and was a member of the data safety monitoring committee for Psyadon Pharmaceuticals. Drs. Scharf and Mathews have received research support, honoraria and travel support from the TAA. Dr. Scharf is a member of the TAA Scientific Advisory Board and has received consulting fees from Nuvelution Pharma, Inc. Dr. Mathews is the co-chair of the TAA Scientific Advisory Board. None of the funding agencies for this project (NINDS, NIMH, TAA) had any influence or played any role in a) the design or conduct of the study; b) management, analysis or interpretation of the data; c) preparation, review or approval of the manuscript. The views expressed in this publication are those of the authors and do not reflect the official policy or position of the Department of the Army, Department of Defense, or the U.S. Government.
References
- Abramovitch A, Dar R, Mittelman A, Wilhelm S (2015). Comorbidity between attention deficit/hyperactivity disorder and obsessive-compulsive disorder across the lifespan: A systematic and critical review. Harvard review of psychiatry 23, 245–262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abramovitch A, Dar R, Mittelman A, Schweiger A (2013). Don’t judge a book by its cover: ADHD-like symptoms in obsessive compulsive disorder. Journal of Obsessive-Compulsive and Related Disorders 2, 53–61 [Google Scholar]
- Almasy L, Blangero J (1998). Multipoint quantitative-trait linkage analysis in general pedigrees. American Journal of Human Genetics 62, 1198–1211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alsobrook JP 2nd, Pauls DL (2002). A factor analysis of tic symptoms in Gilles de la Tourette’s syndrome. The American Journal of Psychiatry 159, 291–296 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders. American Psychiatric Publishing: Arlington, VA [Google Scholar]
- Arnsten AF, Rubia K (2012). Neurobiological circuits regulating attention, cognitive control, motivation, and emotion: disruptions in neurodevelopmental psychiatric disorders. Journal of the American Academy of Child and Adolescent Psychiatry 51, 356–367 [DOI] [PubMed] [Google Scholar]
- Bloch MH, Landeros-Weisenberger A, Rosario MC, Pittenger C, Leckman JF (2008). Meta-analysis of the symptom structure of obsessive-compulsive disorder. The American Journal of Psychiatry 165, 1532–1542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavanna AE, Critchley HD, Orth M, Stern JS, Young MB, Robertson MM (2011). Dissecting the Gilles de la Tourette spectrum: a factor analytic study on 639 patients. Journal of Neurology, Neurosurgery, and Psychiatry 82, 1320–1323 [DOI] [PubMed] [Google Scholar]
- Collett BR, Crowley SL, Gimpel GA, Greenson JN (2000). The factor structure of DSM-IV attention deficit-hyperactivity symptoms: A confirmatory factor analysis of the ADHD-SRS. Journal of Psychoeducational Assessment 18, 361–373 [Google Scholar]
- Darrow SM, Hirschtritt ME, Davis LK, Illmann C, Osiecki L, Grados M, Sandor P, Dion Y, King R, Pauls D, Budman CL, Cath DC, Greenberg E, Lyon GJ, Yu D, McGrath LM, McMahon WM, Lee PC, Delucchi KL, Scharf JM, Mathews CA, Tourette Syndrome Association International Consortium for Genetics (2016). Identification of two heritable cross-disorder endophenotypes for Tourette syndrome. The American Journal of Psychiatry, appiajp201616020240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis LK, Yu D, Keenan CL, Gamazon ER, Konkashbaev AI, Derks EM, Neale BM, Yang J, Lee SH, Evans P, Barr CL, Bellodi L, Benarroch F, Berrio GB, Bienvenu OJ, Bloch MH, Blom RM, Bruun RD, Budman CL, Camarena B, Campbell D, Cappi C, Cardona Silgado JC, Cath DC, Cavallini MC, Chavira DA, Chouinard S, Conti DV, Cook EH, Coric V, Cullen BA, Deforce D, Delorme R, Dion Y, Edlund CK, Egberts K, Falkai P, Fernandez TV, Gallagher PJ, Garrido H, Geller D, Girard SL, Grabe HJ, Grados MA, Greenberg BD, Gross-Tsur V, Haddad S, Heiman GA, Hemmings SM, Hounie AG, Illmann C, Jankovic J, Jenike MA, Kennedy JL, King RA, Kremeyer B, Kurlan R, Lanzagorta N, Leboyer M, Leckman JF, Lennertz L, Liu C, Lochner C, Lowe TL, Macciardi F, McCracken JT, McGrath LM, Mesa Restrepo SC, Moessner R, Morgan J, Muller H, Murphy DL, Naarden AL, Ochoa WC, Ophoff RA, Osiecki L, Pakstis AJ, Pato MT, Pato CN, Piacentini J, Pittenger C, Pollak Y, Rauch SL, Renner TJ, Reus VI, Richter MA, Riddle MA, Robertson MM, Romero R, Rosario MC, Rosenberg D, Rouleau GA, Ruhrmann S, Ruiz-Linares A, Sampaio AS, Samuels J, Sandor P, Sheppard B, Singer HS, Smit JH, Stein DJ, Strengman E, Tischfield JA, Valencia Duarte AV, Vallada H, Van Nieuwerburgh F, Veenstra-Vanderweele J, Walitza S, Wang Y, Wendland JR, Westenberg HG, Shugart YY, Miguel EC, McMahon W, Wagner M, Nicolini H, Posthuma D, Hanna GL, Heutink P, Denys D, Arnold PD, Oostra BA, Nestadt G, Freimer NB, Pauls DL, Wray NR, Stewart SE, Mathews CA, Knowles JA, Cox NJ, Scharf JM (2013). Partitioning the heritability of Tourette syndrome and obsessive compulsive disorder reveals differences in genetic architecture. PLoS genetics 9, e1003864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delucchi KL, Katerberg H, Stewart SE, Denys DA, Lochner C, Stack DE, den Boer JA, van Balkom AJ, Jenike MA, Stein DJ, Cath DC, Mathews CA (2011). Latent class analysis of the Yale-Brown Obsessive-Compulsive Scale symptoms in obsessive-compulsive disorder. Comprehensive psychiatry 52, 334–341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumenci L, McConaughy SH, Achenbach TM (2004). A hierarchical three-factor model of inattention-hyperactivity-impulsivity derived from the Attention Problems syndrome of the Teacher’s Report Form. School Psychology Review 33, 287–301 [Google Scholar]
- Eapen V, Fox-Hiley P, Banerjee S, Robertson M (2004). Clinical features and associated psychopathology in a Tourette syndrome cohort. Acta Neurologica Scandinavica 109, 255–260 [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW (1995). Structured Clinical Interview for DSM-IV Axis I Disorders–Non-Patient Edition (SCID-I/NP, version 2.0). Biometrics Research Department, New York State Psychiatric Institute: New York [Google Scholar]
- Floyd FJ, Widaman KF (1995). Factor analysis in the development and refinement of clinical assessment instruments. Psychological Assessment 7, 286–299 [Google Scholar]
- Freitag CM, Rohde LA, Lempp T, Romanos M (2010). Phenotypic and measurement influences on heritability estimates in childhood ADHD. European child & adolescent psychiatry 19, 311–323 [DOI] [PubMed] [Google Scholar]
- Friedman-Hill SR, Wagman MR, Gex SE, Pine DS, Leibenluft E, Ungerleider LG (2010). What does distractibility in ADHD reveal about mechanisms for top-down attentional control?. Cognition 115, 93–103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frost RO, Steketee G, Tolin DF (2011). Comorbidity in hoarding disorder. Depression and anxiety 28, 876–884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fullana MA, Vilagut G, Mataix-Cols D, Adroher ND, Bruffaerts R, Bunting B, de Almeida JM, Florescu S, de Girolamo G, de Graaf R, Haro JM, Kovess V, Alonso J (2013). Is ADHD in childhood associated with lifetime hoarding symptoms? An epidemiological study. Depression and anxiety 30, 741–748 [DOI] [PubMed] [Google Scholar]
- Fyer A, Endicott J, Mannuzza S, Klein DF (1985). Schedule for Affective Disorders and Schizophrenia-Lifetime Version, Modified for the Study of Anxiety Disorders (SADS-LA). Anxiety Disorders Clinic, New York State Psychiatric Institute: New York: [DOI] [PubMed] [Google Scholar]
- Grados MA, Mathews CA (2009). Clinical phenomenology and phenotype variability in Tourette syndrome. Journal of psychosomatic research 67, 491–496 [DOI] [PubMed] [Google Scholar]
- Hirschtritt ME, Darrow SM, Illmann C, Osiecki L, Grados M, Sandor P, Dion Y, King RA, Pauls DL, Budman CL, Cath DC, Greenberg E, Lyon GJ, Yu D, McGrath LM, McMahon WM, Lee PC, Delucchi KL, Scharf JM, Mathews CA, Tourette Syndrome Association International Consortium for Genetics (TSAICG) (2016). Social disinhibition is a heritable subphenotype of tics in Tourette syndrome. Neurology 87, 497–504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirschtritt ME, Lee PC, Pauls DL, Dion Y, Grados MA, Illmann C, King RA, Sandor P, McMahon WM, Lyon GJ, Cath DC, Kurlan R, Robertson MM, Osiecki L, Scharf JM, Mathews CA, Tourette Syndrome Association International Consortium for Genetics (2015). Lifetime prevalence, age of risk, and genetic relationships of comorbid psychiatric disorders in Tourette syndrome. JAMA psychiatry 72, 325–333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huisman-van Dijk HM, Schoot R, Rijkeboer MM, Mathews CA, Cath DC (2016). The relationship between tics, OC, ADHD and autism symptoms: A cross- disorder symptom analysis in Gilles de la Tourette syndrome patients and family-members. Psychiatry research 237, 138–146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katerberg H, Delucchi KL, Stewart SE, Lochner C, Denys DA, Stack DE, Andresen JM, Grant JE, Kim SW, Williams KA, den Boer JA, van Balkom AJ, Smit JH, van Oppen P, Polman A, Jenike MA, Stein DJ, Mathews CA, Cath DC (2010). Symptom dimensions in OCD: Item-level factor analysis and heritability estimates. Behavior genetics 40, 505–517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N (1997). Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. Journal of the American Academy of Child & Adolescent Psychiatry 36, 980–988 [DOI] [PubMed] [Google Scholar]
- Leckman JF, Denys D, Simpson HB, Mataix-Cols D, Hollander E, Saxena S, Miguel EC, Rauch SL, Goodman WK, Phillips KA, Stein DJ (2010). Obsessive-compulsive disorder: a review of the diagnostic criteria and possible subtypes and dimensional specifiers for DSM-V. Depression and anxiety 27, 507–527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leckman JF, Sholomskas D, Thompson WD, Belanger A, Weissman MM (1982). Best estimate of lifetime psychiatric diagnosis: A methodological study. Archives of General Psychiatry 39, 879–883 [DOI] [PubMed] [Google Scholar]
- Lo Y, Mendell NR, Rubin DB (2001). Testing the number of components in a normal mixture. Biometrika 88, 767–778 [Google Scholar]
- Loehlin JC (2004). Goodness of Fit Indices: Latent Variable Models. Lawrence Erlbaum Associates: Mahwah, NJ [Google Scholar]
- Lopez-Sola C, Fontenelle LF, Verhulst B, Neale MC, Menchon JM, Alonso P, Harrison BJ (2016). Distinct etiological influences on obsessive-compulsive symptom dimensions: a multivariate twin study. Depression and anxiety 33, 179–191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathews CA, Grados MA (2011). Familiality of Tourette syndrome, obsessive-compulsive disorder, and attention-deficit/hyperactivity disorder: Heritability analysis in a large sib-pair sample. Journal of the American Academy of Child and Adolescent Psychiatry 50, 46–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGrath LM, Yu D, Marshall C, Davis LK, Thiruvahindrapuram B, Li B, Cappi C, Gerber G, Wolf A, Schroeder FA, Osiecki L, O’Dushlaine C, Kirby A, Illmann C, Haddad S, Gallagher P, Fagerness JA, Barr CL, Bellodi L, Benarroch F, Bienvenu OJ, Black DW, Bloch MH, Bruun RD, Budman CL, Camarena B, Cath DC, Cavallini MC, Chouinard S, Coric V, Cullen B, Delorme R, Denys D, Derks EM, Dion Y, Rosario MC, Eapen V, Evans P, Falkai P, Fernandez TV, Garrido H, Geller D, Grabe HJ, Grados MA, Greenberg BD, Gross-Tsur V, Grunblatt E, Heiman GA, Hemmings SM, Herrera LD, Hounie AG, Jankovic J, Kennedy JL, King RA, Kurlan R, Lanzagorta N, Leboyer M, Leckman JF, Lennertz L, Lochner C, Lowe TL, Lyon GJ, Macciardi F, Maier W, McCracken JT, McMahon W, Murphy DL, Naarden AL, Neale BM, Nurmi E, Pakstis AJ, Pato MT, Pato CN, Piacentini J, Pittenger C, Pollak Y, Reus VI, Richter MA, Riddle M, Robertson MM, Rosenberg D, Rouleau GA, Ruhrmann S, Sampaio AS, Samuels J, Sandor P, Sheppard B, Singer HS, Smit JH, Stein DJ, Tischfield JA, Vallada H, Veenstra-VanderWeele J, Walitza S, Wang Y, Wendland JR, Shugart YY, Miguel EC, Nicolini H, Oostra BA, Moessner R, Wagner M, Ruiz-Linares A, Heutink P, Nestadt G, Freimer N, Petryshen T, Posthuma D, Jenike MA, Cox NJ, Hanna GL, Brentani H, Scherer SW, Arnold PD, Stewart SE, Mathews CA, Knowles JA, Cook EH, Pauls DL, Wang K, Scharf JM (2014). Copy number variation in obsessive-compulsive disorder and tourette syndrome: a cross-disorder study. Journal of the American Academy of Child and Adolescent Psychiatry 53, 910–919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén B, du Toit SHC, Spisic D (1997). Robust inference using weighted least squares and quadratic estimating equations in latent variable modeling with categorical and continuous outcomes
- Muthén LK, Muthén BO (1998–2012). Mplus User’s Guide. Seventh Edition. Muthén & Muthén: Los Angeles, CA [Google Scholar]
- Pauls DL, Leckman JF, Cohen DJ (1993). Familial relationship between Gilles de la Tourette’s syndrome, attention deficit disorder, learning disabilities, speech disorders, and stuttering. Journal of the American Academy of Child and Adolescent Psychiatry 32, 1044–1050 [DOI] [PubMed] [Google Scholar]
- Pillow DR, Pelham WE Jr, Hoza B, Molina BS, Stultz CH (1998). Confirmatory factor analyses examining attention deficit hyperactivity disorder symptoms and other childhood disruptive behaviors. Journal of abnormal child psychology 26, 293–309 [DOI] [PubMed] [Google Scholar]
- Polanczyk GV, Eizirik M, Aranovich V, Denardin D, da Silva TL, da Conceicao TV, Pianca TG, Rohde LA (2003). Interrater agreement for the schedule for affective disorders and schizophrenia epidemiological version for school-age children (K-SADS-E). Revista brasileira de psiquiatria (Sao Paulo, Brazil : 1999) 25, 87–90 [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Zhang G, Kim C, Mels G (2013). Choosing the optimal number of factors in exploratory factor analysis: A model selection perspective. Multivariate Behavioral Research 48, 28–56 [DOI] [PubMed] [Google Scholar]
- Raykov T, Marcoulides GA (2006). Parameter and Model Identification: A First Course in Structural Equation Modeling. Lawrence Erlbaum Associates: Mahwah, NJ [Google Scholar]
- Robertson MM, Althoff RR, Hafez A, Pauls DL (2008). Principal components analysis of a large cohort with Tourette syndrome. The British journal of psychiatry : the journal of mental science 193, 31–36 [DOI] [PubMed] [Google Scholar]
- Schwarz G (1978). Estimating the dimension of a model. Annals of Statistics 6, 461–464 [Google Scholar]
- Storch EA, Murphy TK, Geffken GR, Soto O, Sajid M, Allen P, Roberti JW, Killiany EM, Goodman WK (2004). Further psychometric properties of the Tourette’s Disorder Scale-Parent Rated version (TODS-PR). Child psychiatry and human development 35, 107–120 [DOI] [PubMed] [Google Scholar]
- Tolin DF, Villavicencio A, Umbach A, Kurtz MM (2011). Neuropsychological functioning in hoarding disorder. Psychiatry research 189, 413–418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toplak ME, Pitch A, Flora DB, Iwenofu L, Ghelani K, Jain U, Tannock R (2009). The unity and diversity of inattention and hyperactivity/impulsivity in ADHD: evidence for a general factor with separable dimensions. Journal of abnormal child psychology 37, 1137–1150 [DOI] [PubMed] [Google Scholar]
- Tourette Syndrome Association International Consortium for Genetics (2007). Genome scan for Tourette disorder in affected-sibling-pair and multigenerational families. American Journal of Human Genetics 80, 265–272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tourette Syndrome Association International Consortium for Genetics (1999). A complete genome screen in sib pairs affected by Gilles de la Tourette syndrome. American Journal of Human Genetics 65, 1428–1436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z, Maia TV, Marsh R, Colibazzi T, Gerber A, Peterson BS (2011). The neural circuits that generate tics in Tourette’s syndrome. The American Journal of Psychiatry 168, 1326–1337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang T, Wang J, Yang Y, Wu Q, Li B, Chen L, Yue Q, Tang H, Yan C, Lui S, Huang X, Chan RC, Zang Y, He Y, Gong Q (2011). Abnormal small-world architecture of top-down control networks in obsessive-compulsive disorder. Journal of psychiatry & neuroscience : JPN 36, 23–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


