Abstract
Background:
The primary purpose of this study was to examine the feasibility and acceptability of participation in a randomized waitlist-controlled intervention of mindfulness-based stress reduction (MBSR) in a young adult cancer sample. A secondary aim was to examine patterns of change in patient reported outcomes (PROs) of physical, social, and emotional functioning.
Methods:
Participants were enrolled at a large Midwestern comprehensive cancer center and randomized to MBSR or a waitlist control. Feasibility and acceptability were examined through enrollment metrics and a survey. PROs were gathered at baseline, 8-weeks, and 16-weeks. Descriptive statistics and mixed models were used in analyses.
Results:
Of 597 eligible participants, 151 (26.5%) consented from which 126 (83.4%) completed baseline measures. Sixty-seven participants were randomized to MBSR, and 59 to the waitlist. Immediately following MBSR, the majority of respondents (72%−78%) reported their experience with mindfulness was very logical and useful to increasing their wellbeing. Compared to waitlist members, MBSR participant’s scores on PROs improved in expected directions.
Conclusions:
Our findings suggest that recruitment for an intensive, in-person, multi-week supportive intervention can be challenging with young adults with cancer, similar to other cancer survivor populations; however once enrolled, feasibility and acceptability of MBSR was supported. Further, initial evidence on the role of MBSR on short-term changes in select PROs with this population was also demonstrated.
Keywords: feasibility, mindfulness, oncology, randomized controlled trail, young adults
1 |. BACKGROUND
Each year up to 70 000 young adults in their 20’s and 30’s are diagnosed with cancer,1 many of whom are challenged with a host of negative short and long-term effects that can significantly impact their psychosocial wellbeing and functioning. As young adult cancer survivors make the transition from “cancer patient” to “cancer survivor,” psychosocial and physical challenges abound. A cancer diagnosis and its treatment can significantly derail the normative developmental milestones of young adulthood, often affecting educational and career aspirations, peer-group membership, formation of romantic relationships, changes in appearance, family planning and fertility, finances, and overall quality of life.2–5 It is well established that cancer survivors in general report late effects of treatment including fatigue, pain, fear of recurrence or secondary complications, and uncertainty about the future.6–8 However, young adults may experience these sequelae at greater rates than other age cohorts.9–11 Given the psychosocial and physical complications young adult cancer survivors face, they may benefit from mind-body supportive interventions that promote wellness and coping skills across mental, social, and physical domains.4,5
Mind-body practices are defined as those that “focus on the interactions among the brain, mind, body, and behavior, with the intent to use the mind to affect physical functioning and promote health.”12 The use of mind-body practices has steadily increased in recent years, especially among younger adults.13 Based primarily on the instruction of mindfulness meditation and Hatha yoga, mindfulness-based stress reduction (MBSR)14 has become an empirically supported, gold standard mind-body approach for helping people reduce stress and manage disease and treatment related sequelae across multiple medical conditions.15–18 MBSR facilitates the cultivation of mindful awareness through an 8-week program that uses an in-person group format to guide participants in the practice of mindfulness meditation and gentle Hatha yoga.19,20
Despite numerous randomized controlled trials of MBSR in cancer patient populations (predominantly in breast cancer) demonstrating significant improvements in emotional distress (depression, anxiety), pain, sleep, and health related quality of life,21,22 only a few small studies have examined the impact of mindfulness-based interventions in young adult cancer survivors. This includes a qualitative examination of the impact of Mindfulness-Based Cognitive Therapy (n = 14),23 a single arm study of a mindfulness-based intervention for young adult cancer survivors (n = 16),24 and a single-arm study on the role of self-compassion resulting from mindfulness training (n = 25).25 To date no randomized controlled trials (RCTs) have been conducted using MBSR with this population.
Given the sparse nature of this previous study, prior to conducting a full-fledged RCT to examine the potential health benefits of mindfulness-based interventions in this population, it is important to first determine several key components regarding feasibility and acceptability of recruitment, randomization, and retention; intervention delivery, outcomes assessment, and overall design.26 A smaller scale randomized pilot study of MBSR with this population would serve as a “dress rehearsal” to identify the readiness of a full RCT that is powered for efficacy and effectiveness. Therefore, the primary purpose of this study was to examine the feasibility and acceptability of participation in a randomized waitlist-controlled intervention of MBSR in a young adult cancer sample. A secondary aim was to examine initial patterns of change in PROs of physical, social and emotional functioning.
2 |. METHODS
This study was made possible through research grant funding from the American Cancer Society, Illinois Division. All study procedures and materials were approved by the Institutional Review Board (IRB) of the participating university. The trial was registered on www.clinicaltrials.gov (NCT02495376).
2.1 |. Recruitment and inclusion/exclusion criteria
Participants were recruited from medical clinics at a large, Midwestern NCI-designated comprehensive cancer center. IRB-approved study flyers were posted in approved locations throughout the hospital. The flyer included the study title, “Reducing Emotional Distress, Enhancing Function and Improving Network Engagement in Adolescent and Young Adult Oncology.” Initial scripted recruitment language included the following to describe the study’s purpose: “intended to reduce anxiety and improve the quality of life of adolescents and young adults diagnosed with cancer.” Not until participants were further along in the consenting process did they learn that this was a mediation and yoga study. A designated medical team member identified and referred potential study participants to speak with a trained research assistant, who described the study, answered questions, and conducted informed consent and HIPAA authorization. All participants signed an informed consent and HIPAA authorization form.
Inclusion criteria required participants’ current age and age of diagnosis (of any cancer type) to be between the ages of 18–39. They also had to be English-speaking, cognitively and emotionally capable of participating in an intensive, multi-week mindfulness course (as informally determined by referring medical staff), and able to use a touchscreen keypad and tablet device. Patients were also excluded if they reported high use of mindfulness meditation or yoga (eg, ≥3 times per week for the past 2 weeks).
2.2 |. Procedures
Following enrollment, participants completed a baseline assessment of socio-demographic and clinical information and PRO measures. Then, participants were randomized to either the MBSR course (Mindfulness Group) or a waitlist control condition (Control Group) using a computer generated randomization procedure, following a 1:1 randomization schedule, of which the assignment was determined at the time of enrollment for each participant. PROs were assessed again at 8-weeks, and then again at 16 weeks following 8-additional weeks where some participants were randomized to receive a brief, weekly email message about mindfulness (this was a secondary aim of this study and is beyond the scope of these findings, however receipt of a weekly email was included as a covariate in all analyses). No financial compensation was provided.
2.2.1 |. MBSR intervention
The MBSR intervention was delivered by qualified MBSR instructors who were trained on study-specific protocols, including the use of a standardized manual that adhered to the principles and pedagogy of MBSR. Classes were held at conveniently located meeting rooms at the hospital and nearby community support centers that were large enough to accommodate meditation and yoga activities. Participants met weekly for approximately 2.5 h for 8 weeks and participated in a half-day retreat near the end of the intervention period. Sessions were video and audio recorded to ensure intervention fidelity among MBSR instructors across sessions. Additionally, instructors received regular supervision from the Principal Investigator and other co-investigators. Participants who missed a class were contacted by the instructor who provided them an overview of the session and home practice exercises. After course completion, Mindfulness Group participants were randomized to receive 8-weekly email messages about mindfulness (eg, “Notice what is happening in your body right now”) or receive no emails as a part of a follow-up exploratory study to examine longer-term maintenance gains from receiving weekly mindfulness messages. To control for this, we included whether or not Mindfulness Group participants received weekly mindfulness messages as a covariate in all analyses.
2.2.2 |. Waitlist control
Participants on the waitlist completed all study assessments at baseline, 8-weeks, and 16-weeks. Following their time on the waitlist, participants received the full 8-week MBSR course. All participants received conventional supportive and medical care as defined by the clinic and physician serving those patients.
2.3 |. Study measures
At baseline, participants completed questions about their previous meditation history using a detailed questionnaire developed by our group27 as well as the Expectancy/Credibility Scale,28 which consists of items based on attitudes and perceived benefits of the therapy being offered. This scale is typically administered once prior to the intervention, however given the makeup of these items we administered and analyzed select items again at the 16-week follow up to determine post-intervention acceptability, using ratings of ≥7 (on a 1–9 scale) as indicative of acceptable. Items included: (a) How logical does the course on mindfulness offered to you seem?; (b) How successful do you think this course will be in raising the quality of your wellbeing?; and (c) How confident would you be in recommending this course to a friend who experiences similar problems?
Common indicators of Health-Related Quality of Life guided the selection of outcomes measures, which included the following three domains and measures below. All scales are scored/interpreted in the direction of the scale name (eg, a high score on perceived stress = higher stress). Score ranges are provided below for each measure, except for PROMIS measures administered via a computer adaptive test, in which case items were adaptively drawn from a full bank of calibrated items and are presented as T-Scores, with a mean of 50 and SD of 10.
2.3.1 |. Disease and treatment related symptoms
Patient Reported Outcomes Measurement Information System (PROMIS) Computer Adaptive Tests (CATs) (see www.healthmeasures.net); of Fatigue, Sleep Disturbance, and Pain Interference.
2.3.2 |. Psychosocial distress
PROMIS CATs of Anxiety and Depression, and Social Isolation; Cancer Survivor Concerns,29 score range = 0–36; Uncertainty Intolerance,30 score range = 0–48; Perceived Stress Scale-4 (PSS-4)31 score range = 0–16.
2.3.3 |. Overall wellbeing
PROMIS CATS of Social Role Satisfaction, Emotional Support, and short form of Positive Affect and Wellbeing, score range = 9–45; Mindfulness Attention Awareness Scale (MAAS),32 score range = 15–90; Self-Kindness and Self-Judgment subscales of the Self-Compassion Scale (SCS),33 score ranges = 5–25 for each; and the Posttraumatic Growth Inventory—Short Form (PTGI-SF), score range = 0–25.34
2.4 |. Statistical analysis and hypotheses
All analyses were conducted using SPSS version 25. Descriptive statistics were used to summarize indicators of feasibility and acceptability, which included the following criteria: (a) access to participants, (b) barriers to participation and clinical delivery of the intervention, (c) suitability of assessment procedures, outcome measures, time and resources required to conduct assessments, (d) willingness of participants to be randomized to proposed study arms, (e) instructor adherence to protocols, (f) acceptability to participants of the treatment, (g) participant adherence to treatment, (h) suitability of recruitment/screening processes, (i) participant retention among the allocation groups, and (j) whether intervention effects are consistent with expectations and previous literature. Based on our previous experience and organizational infrastructure delivering mindfulness interventions to other cancer survivor populations27 and recruiting young adult cancer survivors,35–37 we hypothesized that indicators related to access, recruitment/screening, outcomes assessment, and instructor fidelity would all be in the high range of feasibility. Further, we hypothesized that the intervention would be considered acceptable to ≥70% of attendees (as measured by the three previously described acceptability items); that no more than 2%−3% would attrite once randomized; that between 35% and 45% of those approached would enroll; and that we would not see greater than 10%−15% attrition once enrolled.
To evaluate the aforementioned last indicator, (j) whether intervention effects are consistent with expectations and previous literature, an intent to treat analysis was used. We hypothesized that compared to being on a waitlist, MBSR group participants would experience relatively greater increases in health related quality of life as evidenced by fewer symptoms of psychosocial distress (eg, symptoms of anxiety, depression, stress, social isolation, fear of recurrence, and uncertainty intolerance), fewer disease and treatment-related sequelae (eg, fatigue, sleep disturbance, pain interference), and higher overall wellbeing (eg, social role satisfaction, emotional support, positive affect and wellbeing, mindfulness, self-compassion, and posttraumatic growth). Following bivariate analyses (using chi-square and independent samples t-tests) to examine potential group differences between intervention and control conditions and completers/non-completers, we tested for intervention effects on each outcome variable from baseline to 16-weeks. Longitudinal mixed models were specified using data from week 16 as the dependent variable. Each outcome was tested separately as the dependent variable; intervention arm, and time point were entered as fixed effects. All models were adjusted for meditation history, receipt of follow-up texts or e-mails, and class and retreat attendance. Given the primary focus on feasibilty and acceptabilty outcomes, a power analysis was premature for this phase.
3 |. RESULTS
3.1 |. Enrollment and attrition
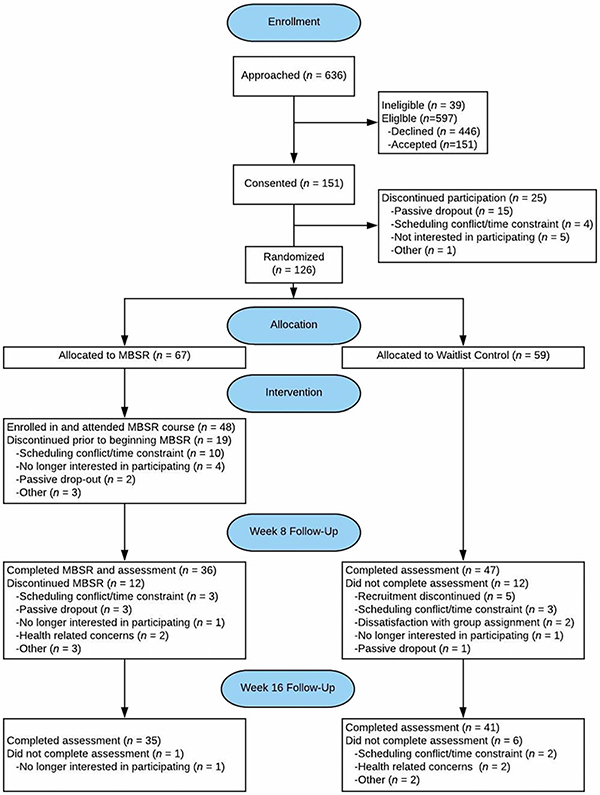
In total, 597 eligible participants were identified, of which 151 (26.5%) consented and 126 (83.4%) completed baseline measures. Sixty-seven participants were randomized to MBSR, and 59 to the waitlist. A marginally significant baseline difference in meditation history between intervention and control conditions was observed (P = .07); therefore meditation history was included as a covariate in subsequent analyses. Following randomization, 48 individuals enrolled in an MBSR course. No statistically significant differences were observed between completers and non-completers. Additional information about enrollment and attrition, including details regarding reasons for dropout, are presented in Figure 1.
FIGURE 1.
Consort diagram
3.2 |. Demographic and clinical characteristics
On average, participants were 32.8 years old (SD = 4.76). The majority of participants were female (78.6%), Caucasian (74.6%), employed full time (61.1%), and had completed at least a college degree (83.3%). Most participants were either married (43.7%) or single and had never been married (41.3%). Participants had been diagnosed on average 2.06 years prior to study enrollment. This breaks down to 48.4% being <1 year since diagnosis; 18.6% being 1–3 years post diagnosis; 11.2% being 4–5 years post diagnosis, and 6.4% being 6–10 years post diagnosis. The majority (58.9%) stated they had completed treatment (38.1% were still in treatment, 3% unsure), which included surgery (62.1%), radiation (41.9%), and chemotherapy (81.5%). Breast cancer and lymphoma were the most common cancer types (34.1% and 25.4%, respectively). 81.7% of the participants had never regularly engaged in a meditation practice (Tables 1 and 2).
Table 1.
Sociodemographic characteristics
| Variable | Mindfulness | Control | Statistic | P |
|---|---|---|---|---|
| Age | 33.01 ± 4.42 | 32.56 ± 5.14 | t(124) = 0.535 | .136 |
| Gender | ||||
| Male | 13 (19.4%) | 14 (23.7%) | Χ2(1) = 0.349 | .555 |
| Female | 54 (80.6%) | 45 (76.3%) | ||
| Race | ||||
| White | 52 (77.6%) | 42 (71.2%) | ||
| Black/African American | 10 (14.9%) | 8 (13.6%) | ||
| Asian | 2 (3.0%) | 8 (13.6%) | Χ2(4) = 6.40 | .171 |
| Other | 1 (1.5%) | 1 (1.7%) | ||
| Not provided | 2 (3.0%) | 0 (0.0%) | ||
| Ethnicity | ||||
| Hispanic | 10 (14.9%) | 9 (15.3%) | Χ2(1) < 0.01 | .959 |
| Non-Hispanic | 57 (85.1%) | 50 (84.7%) | ||
| Marital status | ||||
| Single (never married) | 29 (43.3%) | 23 (39.0%) | ||
| Living with partner | 3 (4.5%) | 5 (8.5%) | ||
| Married | 30 (44.8%) | 25 (42.4%) | Χ2(4) = 1.98 | .739 |
| Separated | 2 (3.0%) | 1 (1.7%) | ||
| Divorced | 3 (4.5%) | 5 (8.5%) | ||
| Education | ||||
| High school | 2 (3.0%) | 2 (3.4%) | ||
| Some college | 10 (14.9%) | 7 (11.9%) | ||
| College degree | 27 (40.3%) | 16 (27.1%) | Χ2(4) = 7.93 | .094 |
| Some graduate school | 7 (10.4%) | 2 (3.4%) | ||
| Graduate degree | 21 (31.3%) | 32 (54.2%) | ||
| Employment | ||||
| Full time | 41 (61.2%) | 36 (61.0%) | ||
| Part time | 5 (7.5%) | 8 (13.6%) | ||
| Self-employed | 3 (4.5%) | 5 (8.5%) | ||
| Not employed (looking for work) | 5 (7.5%) | 2 (3.4%) | Χ2(6) = 3.92 | .687 |
| Not employed (not looking for work) | 5 (7.5%) | 3 (5.1%) | ||
| Student | 5 (7.5%) | 4 (6.8%) | ||
| Homemaker | 3 (4.5%) | 1 (1.7%) | ||
Note:
P < .05
P < .01.
Table 2.
Clinical characteristics, meditation history, and expectancy
| Variable | Mindfulness | Control | Statistic | P |
|---|---|---|---|---|
| Cancer type | Χ2(15) = 12.52 | .639 | ||
| Bone/soft tissue | 4 (6.0%) | 2 (3.4%) | ||
| Brain | 2 (3.0%) | 2 (3.4%) | ||
| Breast | 23 (34.3%) | 20 (34.5%) | ||
| Cervical | 1 (1.5%) | 0 (0.0%) | ||
| Colorectal | 3 (4.5%) | 2 (3.4%) | ||
| Head and neck | 0 (0.0%) | 2 (3.4%) | ||
| Leukemia | 4 (6.0%) | 4 (6.8%) | ||
| Liver | 1 (1.5%) | 0 (0.0%) | ||
| Lung | 1 (1.5%) | 1 (1.7%) | ||
| Lymphoma | 15 (22.4%) | 17 (28.8%) | ||
| Melanoma | 4 (6.0%) | 2 (3.4%) | ||
| Ovarian | 1 (1.5%) | 0 (0.0%) | ||
| Stomach and esophageal | 0 (0.0%) | 1 (1.7%) | ||
| Testicular | 1 (1.5%) | 2 (3.4%) | ||
| Thyroid and endocrine | 0 (0.0%) | 2 (3.4%) | ||
| Other | 7 (10.4%) | 2 (3.4%) | ||
| Meditation history | Χ2(2) = 5.23 | .073 | ||
| Never | 26 (38.8%) | 19 (32.2%) | ||
| Occasionally | 25 (37.3%) | 33 (55.9%) | ||
| Regularly | 16 (23.9%) | 7 (11.9%) | ||
| Expectancy | 0.14 ± 2.91 | −0.15 ± 2.42 | t(123) = 0.60 | .553 |
| Credibility | −0.02 ± 2.57 | 0.03 ± 2.49 | t(123) = −0.12 | .908 |
Note:
P < .05
P < .01.
3.3 |. Feasibility and acceptability of the MBSR intervention
3.3.1 |. Barriers to clinical delivery of the intervention
There were no major barriers to the clinical delivery of the intervention. From time to time an MBSR instructor would be ill or unavailable, however we had a substitute instructor pool in place to accommodate this. Identifying a suitable, large group room within the hospital was also sometimes challenging, however we partnered with a nearby community cancer support center to expand our room options.
3.3.2 |. Willingness of participants to be randomized to proposed study arms
Of the 126 individuals who were randomized to MBSR or a waitlist, three individuals reported dropping out due to dissatisfaction with their group assignment. Randomization was explained in the following way, “You will be randomly assigned to one of two groups (Group A or Group B). If assigned to Group A, you will begin the course at its earliest availability. If assigned to Group B, you will be placed on a waitlist for 16 weeks before beginning the course. Group B participants will partake in the study procedures in the same manner as Group A.”
3.3.3 |. Barriers to participation
Of the 446 individuals who declined interest in participating, the vast majority reported it was due to distance (41.5%) or time constraints (21.7%). Relatively smaller groups reported it was due to a lack of interest in research (6.1%), scheduling challenges (5.6%), health issues (5.2%), or a lack of interest in MBSR (4.9%). Some reported having transportation issues (1.8%) or feeling too overwhelmed by current stressors (1.3%). The remaining group passively refused and gave no information (11.9%).
A subset of individuals who declined (n = 120–126) were asked if they would participate in an MBSR course if it were offered in an alternative locations or formats. Of those asked, 73.8% stated they would enroll in MBSR if it were offered at a location closer to home, and 70.8% stated they would enroll in an online MBSR course. Eighty-six (n = 86) of the individuals who indicated interest in an online MBSR course were queried about specific online course formats: 68.6% stated they would enroll in a live/synchronous video-conference-delivered course taught by an instructor, 70.9% stated they would enroll in a self-directed “educational modules” course, and 73.3% stated they would enroll in a “hybrid” course that contained both synchronous experiences in addition to self-directed educational content. Following randomization to MBSR, 48 individuals of the 68 who were randomized actually enrolled in an MBSR course. Of the 19 individuals who dropped out between consent and the start of a course, the most common reason was scheduling conflict.
3.3.4 |. Participant adherence to treatment/retention among the allocation groups
Of those who enrolled in MBSR, 75% (n = 36) completed the course and the 8-week assessment. This is consistent with previous studies, in which the average MBSR drop-out rate among cancer patients was 23% (13). Fifty-four percent (54%) attended between 6–8 sessions. Similarly 54% attended the half-day retreat. Of the eight possible sessions (2.5 h per session X 8 = 20 h) and half-day retreat (4 h), MBSR attendance ranged from 2.5 to 24 h among individuals who participated in the course. The median MBSR attendance was 18 h, while the average was 15 h. Reasons for drop-out included passive withdrawal (not responding to calls/emails) [25.0%], time constraints (25.0%), and health concerns (feeling too ill to continue) [16.7%]. Individuals randomized to the Mindfulness Group who found MBSR to be less credible at baseline were less likely to complete all study procedures, t(66) = −2.40; P = .019. Similarly, those who expected MBSR to be less effective were also less likely to complete all study procedures t(65) = −2.31; P = .024. See Table 3 for means and standard deviations on outcomes measures across different time points.
Table 3.
A, Mindfulness group means, standard deviations, and within group changes and B, Waitlist control group means, standard deviations, and within group changes
|
Paired Samples t-test (Baseline to Week 16) |
|||||||||||
| Domain Outcome measure |
Baseline (N = 67) |
Week 8 (N = 36) |
Week 16 (N = 35) |
95% CI |
|||||||
| Mean | (SD) | Mean | (SD) | Mean | (SD) | t | df | P | Lower | Upper | |
| Disease and treatment related symptoms | |||||||||||
| Pain interference | 53.70 | (10.58) | 51.61 | (10.32) | 52.35 | (11.51) | 0.58 | 34 | .566 | −3.10 | 5.58 |
| Fatigue | 57.80 | (8.14) | 54.80 | (8.20) | 53.57 | (9.72) | −1.82 | 34 | .078 | −5.36 | 0.30 |
| Sleep disturbance | 54.92 | (8.21) | 51.63 | (9.14) | 51.48 | (7.59) | −1.67 | 34 | .103 | −4.85 | 0.47 |
| Psychosocial distress | |||||||||||
| Anxiety | 59.19 | (7.54) | 57.25 | (6.54) | 56.96 | (8.14) | −1.07 | 34 | .290 | −6.05 | 1.86 |
| Depression | 53.51 | (8.44) | 52.84 | (7.45) | 54.15 | (9.23) | 0.38 | 33 | .706 | −2.91 | 4.25 |
| Social isolation | 49.89 | (8.70) | 49.70 | (9.11) | 48.00 | (10.05) | −0.79 | 34 | .434 | −5.68 | 2.50 |
| Cancer survivor concerns | 16.67 | (7.47) | 16.28 | (7.72) | 16.71 | (8.39) | 0.19 | 33 | .848 | −2.60 | 3.14 |
| Perceived stress | 7.00 | (2.46) | 5.86 | (2.79) | 5.82 | (2.52) | −1.48 | 33 | .147 | −1.81 | 0.28 |
| Self-judgement | 3.28 | (0.91) | 3.18 | (0.93) | 3.06 | (0.81) | −1.95 | 33 | .059 | −0.55 | 0.01 |
| Intolerance of uncertainty | 19.41 | (7.43) | 15.79 | (9.88) | 15.68 | (6.71) | −2.70 | 33 | .011* | −5.57 | −0.78 |
| Overall wellbeing | |||||||||||
| Emotional support | 53.53 | (8.71) | 54.49 | (8.82) | 54.85 | (7.26) | 1.13 | 34 | .267 | −1.10 | 3.84 |
| Role satisfaction | 48.45 | (8.91) | 50.84 | (8.67) | 50.07 | (6.94) | 0.36 | 34 | .719 | −2.66 | 3.81 |
| Positive affect and wellbeing | 50.75 | (6.36) | 52.35 | (6.51) | 53.25 | (5.72) | 1.72 | 34 | .094 | −0.28 | 3.32 |
| Mindful attention and awareness | 3.88 | (0.88) | 3.65 | (0.82) | 3.91 | (0.93) | 0.85 | 33 | .403 | −0.19 | 0.46 |
| Post-traumatic growth | 3.24 | (1.16) | 3.39 | (1.21) | 3.66 | (0.94) | 2.40 | 33 | .022* | 0.06 | 0.78 |
| Self-kindness | 3.17 | (0.72) | 3.18 | (0.74) | 3.51 | (0.58) | 3.95 | 33 | <.001* | 0.22 | 0.69 |
|
Paired Samples t-test (Baseline to Week 16) |
|||||||||||
| Domain Outcome measure |
Baseline (N = 67) |
Week 8 (N = 36) |
Week 16 (N = 35) |
95% CI |
|||||||
| Mean | (SD) | Mean | (SD) | Mean | (SD) | t | df | P | Lower | Upper | |
| Disease and treatment related symptoms | |||||||||||
| Pain interference | 53.13 | (10.32) | 51.37 | (9.09) | 53.08 | (9.63) | −0.50 | 41 | .622 | −4.43 | 2.68 |
| Fatigue | 55.61 | (8.20) | 55.03 | (8.47) | 54.18 | (9.03) | −1.16 | 41 | .254 | −3.47 | 0.94 |
| Sleep disturbance | 51.84 | (9.14) | 51.92 | (8.98) | 51.19 | (7.42) | −1.51 | 41 | .139 | −4.17 | 0.61 |
| Psychosocial distress | |||||||||||
| Anxiety | 59.17 | (6.54) | 58.76 | (6.38) | 57.38 | (7.94) | −1.78 | 41 | .083 | −3.84 | 0.25 |
| Depression | 54.95 | (7.45) | 54.58 | (7.36) | 53.65 | (8.15) | −3.01 | 41 | .004* | −4.73 | −0.94 |
| Social isolation | 50.75 | (9.11) | 51.92 | (7.96) | 52.05 | (8.41) | 0.47 | 41 | .644 | −1.92 | 3.06 |
| Cancer survivor concerns | 16.44 | (7.72) | 17.32 | (8.49) | 17.43 | (7.45) | 0.45 | 41 | .657 | −1.57 | 2.46 |
| Perceived Stress | 7.31 | (2.79) | 6.65 | (2.83) | 6.55 | (2.82) | −2.30 | 41 | .026* | −2.01 | −0.13 |
| Self-judgement | 3.18 | (0.93) | 3.29 | (0.91) | 3.16 | (0.96) | −0.95 | 41 | .350 | −0.32 | 0.12 |
| Intolerance of uncertainty | 19.91 | (9.88) | 18.43 | (9.08) | 16.67 | (8.21) | −2.83 | 41 | .007* | −5.90 | −0.99 |
| Overall wellbeing | |||||||||||
| Emotional support | 52.17 | (8.82) | 51.50 | (8.51) | 51.37 | (9.02) | −0.90 | 41 | .376 | −3.06 | 3.06 |
| Role satisfaction | 47.91 | (8.67) | 49.56 | (8.88) | 49.03 | (10.24) | 0.74 | 41 | .464 | −1.91 | 4.12 |
| Positive affect and wellbeing | 51.11 | (6.51) | 51.59 | (6.44) | 51.96 | (7.05) | 1.48 | 41 | .147 | −0.52 | 3.36 |
| Mindful attention and awareness | 4.12 | (0.82) | 3.98 | (0.76) | 4.00 | (1.04) | −0.60 | 41 | .554 | −0.24 | 0.13 |
| Post-traumatic growth | 3.01 | (1.21) | 3.17 | (1.27) | 3.07 | (1.26) | 0.77 | 41 | .446 | −0.19 | 0.42 |
| Self-kindness | 3.22 | (0.74) | 3.19 | (0.76) | 3.22 | (0.73) | −0.05 | 41 | .962 | −0.20 | 0.19 |
3.3.5 |. Acceptability to participants of the treatment
Following course participation, the majority of participants reported their experience with mindfulness to be very logical (77.6%) and one that would be very useful in raising the quality of their wellbeing (72.4%). Similarly, the majority stated they would recommend this course to a friend with similar problems (71.1%). These reports at 16 weeks were relatively consistent with, and in some cases higher than ratings provided at baseline (75.4%, 73%, and 62.4%, respectively), suggesting exposure to the MBSR intervention was an overall satisfactory experience.
3.3.6 |. Whether intervention effects are consistent with expectations and previous literature
Compared to waitlist participants, MBSR participants reported significantly greater increases in self-kindness (a sub-domain of self-compassion) over time F(2, 79.48) = 3.64, P = .031, Cohen’s d = 0.44. No other interaction effects were statistically significant. Within group changes on outcomes from baseline to each follow-up were examined among control and treatment conditions. The control condition demonstrated statistically significant changes in perceived stress, F (2, 86.84) = 3.51, P = .034, Cohen’s d = 0.26 and intolerance of uncertainty, F(2, 86.18) = 4.64, P = .012, Cohen’s d = 0.42 Pairwise comparisons revealed statistically significant decreases in perceived stress from baseline to 8 weeks (P = .012) and from 8 to 16 weeks (P = .035), as well as decreases in uncertainty intolerance from 8 to 16 weeks (P = .006).
Individuals in the MBSR group reported statistically significant within group improvements in all three domains of disease and treatment related symptoms, psychosocial distress, and overall wellbeing. A statistically significant improvement from baseline was observed on sleep, F(2, 79.75) = 4.39, P = .016, Cohen’s d = 0.47, indicating sleep disturbance decreased from baseline to 8 weeks (P = .012) and from 8 to 16 weeks (P = .010). MBSR participants also reported reduced intolerance of uncertainty F(2, 82.34) = 3.50, P = .035, Cohen’s d = 0.51 with decreases from baseline to 8 weeks (P = .015) and 8 to 16 weeks (P = .006). Finally, improvements were also observed in post-traumatic growth, F(2, 82.95) = 3.41, P = .038, Cohen’s d = 0.41, and self-kindness, F(2, 77.67) = 7.35, P = .001, Cohen’s d = 0.46, with both increasing from week 8 to week 16 (P = .011 and P < .001, respectively).
4 |. DISCUSSION
Overall, our findings indicate that MBSR was an acceptable intervention for study participants who took part in the program. This may be attributed to MBSR, and/or that study completers were simply inclined to view their experience in a positive way. The current in-person format of MBSR does not seem to be very feasible for this population, however interest in an online version of MBSR was expressed by over 70% of those who declined.
MBSR is an intensive, in-person, multi-week, mind-body intervention. Participation requires an active commitment to attend as many sessions as possible, participate in daily home practice, and attend a half-day retreat. While our enrollment rate of 26.5% is on par with other MBSR interventions in oncology, suggesting similar challenges to in-person participation as other groups,22,38 this population may experience unique barriers, including: (a) participating in clinical research significantly less than other age groups; (b) harboring skepticism and mistrust toward researchers; and (c) holding attitudes that research is inaccessible, overwhelming, inconvenient, burdensome, and frustrating.39
Given the pilot nature of this effort, the present study was under-powered for efficacy outcomes. Therefore, the observed group difference in self-kindness or within group improvements in sleep disturbance, uncertainty intolerance and posttraumatic growth should not be used to infer efficacy, but rather as initial evidence that certain outcomes performed consistently with expectations, many of which could have also occurred as a result of the passage of time or expectancy effects.
4.1 |. Study limitations
In addition to the small sample size, this present study was limited by demographic homogeneity. Another limitation was the inclusion of participants who were at all stages of their cancer journey from active treatment to 10 years post diagnosis, some of whom may have been getting worse from treatment and others in the initial recovery stage immediately after treatment. This could have significantly influenced score variability and the likelihood of observing a change in PROs. Notwithstanding, it should be noted that the majority of PROs trended in expected directions, suggesting future studies be conducted that are powered for efficacy designed trials.
4.2 |. Clinical implications
Findings from this study support further clinical mindfulness programs and research with this population. A majority of attendees reported finding it valuable for their wellbeing and would recommend it to a friend facing similar challenges. Considering this population’s struggles with loneliness and social isolation, their need for developmentally appropriate psychosocial support, and their status as “digital natives,”40 future clinical and research efforts should examine the effects of technology-enabled interventions. This would increase our understanding on how moving from an in-person group environment to an online environment might affect intervention delivery dynamics, social support, learning styles, and overall uptake.
5 |. CONCLUSION
The present study was the first randomized-controlled pilot trial of an MBSR intervention with a young adult cancer sample. Overall, this program was feasible to deliver and acceptable to participants who experienced it, yet infeasible for the majority of those to whom it was offered, mostly due to limited time and distance. Given interest and feedback for an online format from those who declined, future iterations of this intervention should consider exploring the impact of online delivery.
Acknowledgments
Funding information
American Cancer Society - Illinois Division; National Cancer Institute-Funded T32 Behavioral and Psychosocial Research Postdoctoral Training Grant in Cancer Prevention and Control; Robert H. Lurie Comprehensive Cancer Center
The authors have no conflicts of interest to report and no commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit upon the authors or upon any organization with which the authors are associated.
DATA AVAILABILITY STATEMENT
Data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1.NCI. Adolescents and Young Adults with Cancer. Reports, Research, and Literature Web site. https://www.cancer.gov/types/aya. Published 2018. Accessed December 5, 2018.
- 2.Mattson MR, Demshar RK, Daly BJ. Quality of life of young adult survivors of hematologic malignancies. Cancer Nurs. 2012;35(1):E34–E41. [DOI] [PubMed] [Google Scholar]
- 3.Benedict C, Thom B, Friedman DN, Pottenger E, Raghunathan N, Kelvin JF. Fertility information needs and concerns post-treatment contribute to lowered quality of life among young adult female cancer survivors. Support Care Cancer MASCC. 2018;26(7):2209–2215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harju E, Roser K, Dehler S, Michel G. Health-related quality of life in adolescent and young adult cancer survivors. Support Care Cancer MASCC. 2018;26(9):3099–3110. [DOI] [PubMed] [Google Scholar]
- 5.Smith AW, Bellizzi KM, Keegan TH, et al. Health-related quality of life of adolescent and young adult patients with cancer in the United States: the adolescent and young adult health outcomes and patient experience study. J Clin Oncol. 2013;31(17):2136–2145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Victorson D, Cella D, Wagner LI, Kramer L, Smith ML. Measuring quality of life in cancer survivors. In: Feuerstein M, ed. Handbook of Cancer Survivorship. New York, NY: Springer; 2007:79–112. [Google Scholar]
- 7.Kwak M, Zebrack BJ, Meeske KA, et al. Prevalence and predictors of post-traumatic stress symptoms in adolescent and young adult cancer survivors: a 1-year follow-up study. Psycho-Oncology. 2012;22(8): 1798–1806. [DOI] [PubMed] [Google Scholar]
- 8.Phillips-Salimi CR, Andrykowski MA. Physical and mental health status of female adolescent/young adult survivors of breast and gynecological cancer: a national, population-based, case-control study. Support Care Cancer. 2013;21:1597–1604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mor V, Malin M, Allen S. Age differences in the psychosocial problems encountered by breast cancer patients. J Natl Cancer Inst Monogr. 1994;16:191–197. [PubMed] [Google Scholar]
- 10.Mor V, Allen S, Malin M. The psychosocial impact of cancer on older versus younger patients and their families. Cancer. 1994;74(7 Suppl): 2118–2127. [DOI] [PubMed] [Google Scholar]
- 11.Coccia PF, Altman J, Bhatia S, et al. Adolescent and young adult oncology. Clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2012;10(9):1112–1150. [DOI] [PubMed] [Google Scholar]
- 12.NCCAM Definition of Mind Body Medicine. In: 2011. [Google Scholar]
- 13.Clarke TC, Black LI, Stussman BJ, Barnes PM, Nahin RL. Trends in the use of complementary health approaches among adults: United States. Natl Health Stat Report. 2002–2012;2015(79):1–16. [PMC free article] [PubMed] [Google Scholar]
- 14.Kabat-Zinn J Full Catastrophe Living: Using the Wisdom of your Mind to Face Stress, Pain and Illness. New York: Dell Publishing; 1990. [Google Scholar]
- 15.Wong SY. Effect of mindfulness-based stress reduction programme on pain and quality of life in chronic pain patients: a randomised controlled clinical trial. HongKong Med J. 2009;15(Suppl 6):13–14. [PubMed] [Google Scholar]
- 16.Chiesa A, Serretti A. Mindfulness-based stress reduction for stress management in healthy people: a review and meta-analysis. J Altern Complement Med. 2009;15(5):593–600. [DOI] [PubMed] [Google Scholar]
- 17.Ledesma D, Kumano H. Mindfulness-based stress reduction and cancer: a meta-analysis. Psycho-Oncology. 2009;18(6):571–579. [DOI] [PubMed] [Google Scholar]
- 18.Bohlmeijer E, Prenger R, Taal E, Cuijpers P. The effects of mindfulness-based stress reduction therapy on mental health of adults with a chronic medical disease: a meta-analysis. J Psychosom Res. 2010;68(6):539–544. [DOI] [PubMed] [Google Scholar]
- 19.Bishop SR, Lau M, Shapiro S, et al. Mindfulness: a proposed ooperational definition. Clin Psychol Sci Pract. 2004;11(3):230–241. [Google Scholar]
- 20.Kabat-Zinn J, Massion AO, Kristeller J, et al. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. Am J Psychiatry. 1992;149(7):936–943. [DOI] [PubMed] [Google Scholar]
- 21.Zhang Q, Zhao H, Zheng Y. Effectiveness of mindfulness-based stress reduction (MBSR) on symptom variables and health-related quality of life in breast cancer patients: a systematic review and meta-analysis. Support Care Cancer. 2018;27(3):771–781. [DOI] [PubMed] [Google Scholar]
- 22.Lengacher CA, Reich RR, Paterson CL, et al. Examination of Broad Symptom Improvement Resulting From Mindfulness-Based Stress Reduction in Breast Cancer Survivors: A Randomized Controlled Trial. J Clin Oncol. 2016;34:2827–2834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Roth A, Nissim R, Elliott M. Mindfulness-based cognitive therapy for young adults with cancer. Univ West Ont Med J. 2018;87(1):11–13. [Google Scholar]
- 24.Van der Gucht K, Takano K, Labarque V, et al. A mindfulness-based intervention for adolescents and young adults after cancer treatment: Effects on quality of life, emotional distress, and cognitive vulnerability. J Adolesc Young Adult Oncol. 2017;6(2):307–317. [DOI] [PubMed] [Google Scholar]
- 25.Campo RA, Bluth K, Santacroce SJ, et al. A mindful self-compassion videoconference intervention for nationally recruited posttreatment young adult cancer survivors: feasibility, acceptability, and psychosocial outcomes. Support Care Cancer. 2017;25(6):1759–1768. [DOI] [PubMed] [Google Scholar]
- 26.Abbott JH. The distinction between randomized clinical trials (RCTs) and preliminary feasibility and pilot studies: what they are and are not. J Orthop Sports Phys Ther. 2014;44(8):555–558. [DOI] [PubMed] [Google Scholar]
- 27.Victorson D, Hankin V, Burns J, et al. Feasibility, acceptability and preliminary psychological benefits of mindfulness meditation training in a sample of men diagnosed with prostate cancer on active surveillance: results from a randomized controlled pilot trial. Psycho-Oncology. 2017;26(8):1155–1163. [DOI] [PubMed] [Google Scholar]
- 28.Devilly GJ, Borkovec TD. Psychometric properties of the credibility/expectancy questionnaire. J Behav Ther Exp Psychiatry. 2000;31(2):73–86. [DOI] [PubMed] [Google Scholar]
- 29.Gotay CC, Pagano IS. Assessment of Survivor Concerns (ASC): a newly proposed brief questionnaire. Health Qual Life Outcomes. 2007;5:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Carleton RN, Norton MA, Asmundson GJ. Fearing the unknown: a short version of the Intolerance of Uncertainty Scale. J Anxiety Disord. 2007;21(1):105–117. [DOI] [PubMed] [Google Scholar]
- 31.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:386–396. [PubMed] [Google Scholar]
- 32.Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84(4):822–848. [DOI] [PubMed] [Google Scholar]
- 33.Neff K. Development and validation of a scale to measure self-compassion. Self Identity. 2003;2:223–250. [Google Scholar]
- 34.Cann A, Calhoun LG, Tedeschi, RG A short form of the posttraumatic growth inventory. Anxiety Stress Coping 2010;23(2):127–137. [DOI] [PubMed] [Google Scholar]
- 35.Salsman JM, Garcia SF, Yanez B, Sanford SD, Snyder MA, Victorson D. Physical, emotional, and social health differences between posttreatment young adults with cancer and matched healthy controls. Cancer. 2014;120(15):2247–2254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Munoz AR, Kaiser K, Yanez B, et al. Cancer experiences and health-related quality of life among racial and ethnic minority survivors of young adult cancer: a mixed methods study. Support Care Cancer. 2016;24(12):4861–4870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Victorson D, Garcia SF, Sanford S, Snyder MA, Lampert S, Salsman JM. A qualitative focus group study to illuminate the lived emotional and social impacts of cancer and its treatment on young adults. J Adolesc Young Adult Oncol. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shaw JM, Sekelja N, Frasca D, Dhillon HM, Price MA. Being mindful of mindfulness interventions in cancer: A systematic review of intervention reporting and study methodology. Psycho-Oncology. 2018;27(4):1162–1171. [DOI] [PubMed] [Google Scholar]
- 39.Benedict C, Victorson D, Love B, et al. The Audacity of Engagement: Hearing Directly from Young Adults with Cancer on Their Attitudes and Perceptions of Cancer Survivorship and Cancer Survivorship Research. J Adolesc Young Adult Oncol. 2018;7(1):103–111. [DOI] [PubMed] [Google Scholar]
- 40.Abrol E, Groszmann M, Pitman A, Hough R, Taylor RM, Aref-Adib G. Exploring the digital technology preferences of teenagers and young adults (TYA) with cancer and survivors: a cross-sectional service evaluation questionnaire. J Cancer Surviv. 2017;11(6):670–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data that support the findings of this study are available from the corresponding author upon reasonable request.