A 30-year-old doctor, without comorbidities, presented to the emergency department of our hospital in Rio de Janeiro with a 2-week history of intermittent high fever (reaching 39°C), headache and abdominal pain. A week later the patient developed a dry cough, dyspnoea, and cervical lymphadenopathy. As relevant epidemiological data, the patient had travelled to Canada 15 days before the start of these manifestations. He denied contact with sick people, visits to caves or rural areas, and eating of raw food. Treatment for community-acquired pneumonia with levofloxacin was started. As there was no clinical improvement, he was admitted to the intensive care unit (ICU) of our hospital for investigation and treatment.
Short abstract
Pneumonitis due to primary toxoplasmosis in an immunocompetent subject is rare. Here, the mononucleosis-like syndrome, associated with serological evidence of T. gondii infection and positive PCR for T. gondii in BAL, allowed us to establish the diagnosis. https://bit.ly/3qHE2U7
A 30-year-old doctor, without comorbidities, presented to the emergency department of our hospital in Rio de Janeiro with a 2-week history of intermittent high fever (reaching 39°C), headache and abdominal pain. A week later the patient developed a dry cough, dyspnoea, and cervical lymphadenopathy. As relevant epidemiological data, the patient had travelled to Canada 15 days before the start of these manifestations. He denied contact with sick people, visits to caves or rural areas, and eating of raw food. Treatment for community-acquired pneumonia with levofloxacin was started. As there was no clinical improvement, he was admitted to the intensive care unit (ICU) of our hospital for investigation and treatment.
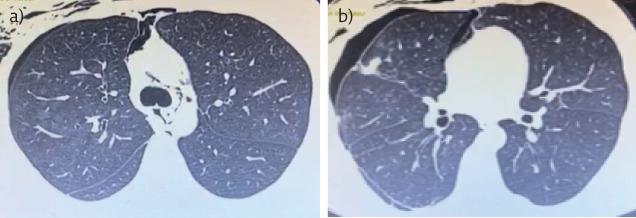
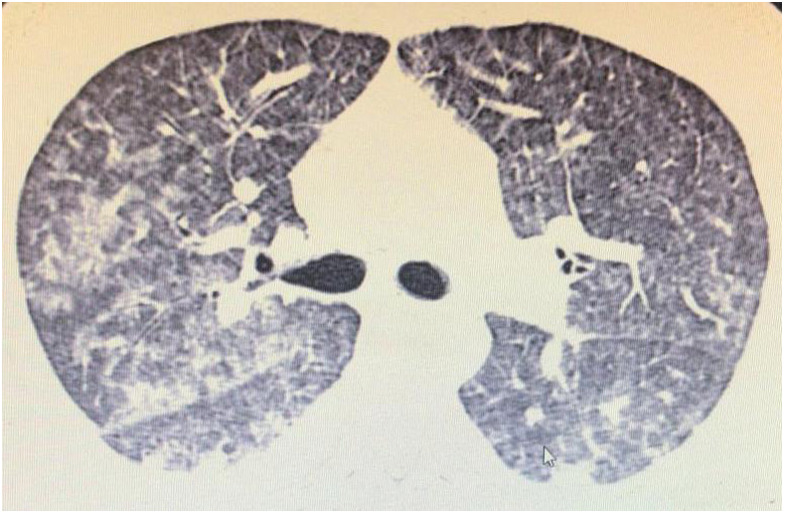
On admission in the ICU, the patient was dyspnoeic and hypoxaemic, depending on high-flow oxygen support and intermittent noninvasive mechanical ventilation. Physical examination revealed cervical bilateral lymphadenopathy, pulmonary auscultation with discrete bilateral pulmonary rales, and abdominal palpation with hepatosplenomegaly. Initial laboratory findings demonstrated mild liver injury and elevated C-reactive protein. Serological panel showed both reactive anti-Toxoplasma gondii IgM and IgG and IgG avidity was low. HIV serology was negative. Chest computed tomography (CT) showed bilateral ground-glass opacities, mediastinal lymphadenopathy, and slight pleural effusion (figures 1 and 2). Abdominal CT revealed hepatosplenomegaly.
Figure 1.
Chest CT showing bilateral ground-glass opacities associated with peripheral septal thickening.
Figure 2.
Chest CT showing bilateral ground-glass opacities associated with slight pleural effusion.
Task 1
Which of the following is the main diagnostic hypothesis?
a) Disseminated tuberculosis
b) Lymphoma
c) Mononucleosis-like syndrome
d) Hantavirosis
e) Disseminated histoplasmosis
Answer 1
All of the diagnostic hypotheses listed may present with a clinical picture of fever, lymphadenopathy and hepatosplenomegaly. Among such hypotheses, mononucleosis-like syndrome would be the most common in a young patient without comorbidities. Lymphoma would be a plausible possibility for the case and cannot be ruled out at this time. However, the rapid clinical evolution seems more acute than expected for cases of lymphoproliferative disease, and the B-symptoms of lymphoma are characterised by lower fever than that presented by the patient and by night sweats, which does not appear in the clinical history. For a severe condition of lymphoma already evolving with respiratory failure, changes in the patient's blood count would be expected, which is not demonstrated in the clinical case. Disseminated tuberculosis would be more commonly associated with immunosuppression and is also generally characterised by a fever that is less high than the fever of the patient in question, in addition to being more common in the evening and associated with night sweats. In the same way as lymphoma, tuberculosis usually has a more insidious evolution. The CT changes evidenced with ground-glass opacities are not typical of disseminated tuberculosis, which is characterised by diffuse micronodular infiltrates, randomly distributed, whose small nodules measure between 2 and 3 mm in diameter with a predominance in the upper lobes. Disseminated histoplasmosis is generally associated with environmental exposure to bat faeces. Hantavirus is related to exposure to urine, faeces, or rodent saliva (not described in the case) and is not usually related to hepatosplenomegaly.
Task 2
What would be the next step?
a) Surgical lung biopsy
b) Sulfadiazine with pyrimethamine
c) Bronchoscopy with bronchoalveolar lavage (BAL) and endobronchial ultrasound
d) Amphotericin B
Answer 2
The serological panel with positive IgM and IgG results for T. gondii and low IgG avidity test indicate the diagnosis of acute toxoplasmosis, an aetiology compatible with the mononucleosis-like syndrome presented by the patient. The recommended treatment for severe cases of disseminated toxoplasmosis is sulfadiazine with pyrimethamine. The use of trimethoprim-sulfamethoxazole is a therapeutic alternative if sulfadiazine with pyrimethamine is not available or if it is not possible to take medication through the digestive tract.
Because of suspected toxoplasmosis and due to the case severity and respiratory impairment we chose to start treatment with intravenous medication (trimethoprim-sulfamethoxazole, 10–50 mg·kg−1·day−1). Despite treatment, he developed respiratory worsening in the next 24 h and it was decided to carry out an open lung biopsy and bronchoscopy. A histopathological study from the lung biopsy demonstrated diffuse alveolar damage. Gram, Ziehl Nielsen and Fontana-Masson stains did not demonstrate specific pathogens. BAL T. gondii PCR was positive.
Task 3
What is the best therapeutic choice?
a) High-dose corticosteroid therapy
b) Empiric therapy with amphotericin B, piperacillin-tazobactam, azithromycin and corticosteroid
c) Keep the treatment for toxoplasmosis
d) Start ganciclovir
e) None of the above
Answer 3
The finding of diffuse alveolar damage on lung biopsy is not specific to a particular disease and can be the result of different inflammatory and/or infectious processes. Diffuse alveolar damage is the histopathological finding found in acute respiratory distress syndrome (ARDS). The absence of common pathogens in the histopathology of lung tissue, associated with positive T. gondii PCR obtained from BAL, led us to establish that the toxoplasmosis was responsible for the pneumonitis aetiology, so the treatment with trimethoprim-sulfamethoxazole should be continued.
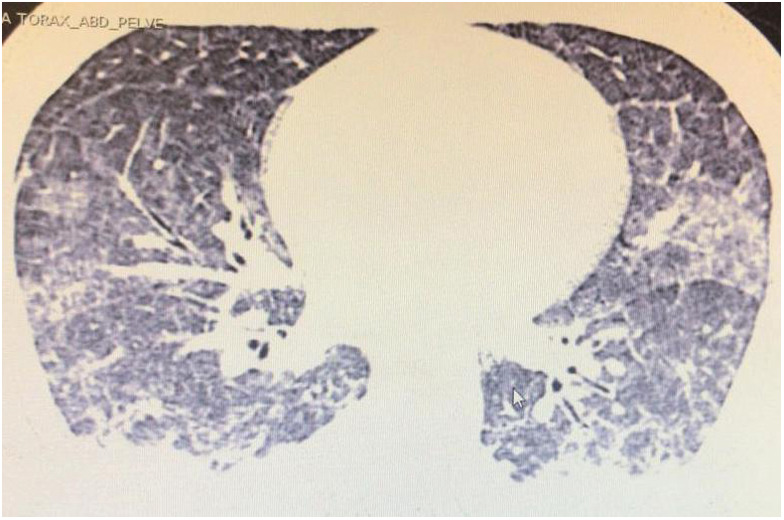
It was decided to keep the treatment for toxoplasmosis and add low-dose corticosteroids as part of the treatment of ARDS. After 3 days, it was possible to wean from mechanical ventilation and switch to oral medication (sulfadiazine 6 g·day−1 and pyrimethamine 75 mg loading dose, followed by 25 mg·day−1). After 10 days of hospitalisation, the patient was discharged with significant clinical and laboratory improvement, and recommendation to complete a 4-week course of anti-Toxoplasma treatment. The control CT performed before hospital discharge showed a slight residual pneumothorax after removal of the chest drain and an important evolutionary improvement of the bilateral pulmonary infiltrate in ground glass (figure 3).
Figure 3.
Chest CT before hospital discharge showing improvement in ground-glass opacities and small residual pneumothorax and pneumomediastinum after surgical biopsy.
Task 4
Which of the following is not correct about the diagnosis of toxoplasmosis?
a) Raw food intake is often related to illness
b) Fever, lymphadenopathy and hepatosplenomegaly are usually present in cases with clinical manifestations
c) The disease is usually symptomatic in immunocompetent patients
d) Infections due to cytomegalovirus (CMV) and Epstein–Barr virus (EBV) viruses can manifest similar symptoms
e) None of the above
Answer 4
Toxoplasmosis is a zoonosis caused by the parasite T. gondii. Felids are infected as definite hosts, and humans as intermediate hosts. T. gondii infection in humans most often occurs through the ingestion of uncooked meat contaminated by cysts, ingestion of food or water contaminated by oocysts, or by mother–child transmission during pregnancy [1]. Toxoplasmosis is an endemic disease in developing countries [2–4]. Usually, toxoplasmosis presents as an asymptomatic disease or a nonspecific infectious syndrome, the most common manifestations are fatigue, fever, headache, lymphadenopathy, and hepatosplenomegaly [2, 3]. Young adults are the most often affected, predominantly men [2, 3]. The disease can be life-threatening in immunocompromised individuals, such as HIV carriers, patients who have undergone haematopoietic stem cell transplant and solid organ transplant recipients [5–7]. In rare situations, the primary infection can manifest as a severe infirmity in otherwise healthy people [8–10]. Infections with the EBV and CMV viruses can manifest as a mononucleosis-like syndrome (fever, lymphadenopathy and hepatosplenomegaly) and, therefore, are part of the differential diagnoses for the case presented.
Discussion
Here, we report a case of acute toxoplasmosis infection with pneumonitis in an immunocompetent patient. The primary infection is supported by documented seroconversion of IgM and IgG antibodies and low IgG avidity test. There are few reports of lung involvement associated with T. gondii infection in immunocompetent patients [8–12]. The absence of common pathogens in the histopathology study of lung tissue, associated with positive T. gondii PCR obtained from BAL, led us to establish the pneumonitis aetiology. Other studies had demonstrated that PCR is an important tool in acute toxoplasmosis diagnosis, and can be detected from different clinical samples, such as BAL, blood, amniotic fluid and cerebrospinal fluid [9, 10, 13, 14].
Although standard toxoplasmosis treatment is sulfadiazine and pyrimethamine, trimethoprim-sulfamethoxazole is supported as an option in the treatment of disseminated infection in immunocompetent people [15–17]. Our initial choice for treatment with trimethoprim-sulfamethoxazole was due to patient respiratory impairment and the difficulty of swallowing pills.
Conclusion
The diagnostic of pneumonitis due to primary toxoplasmosis in an immunocompetent subject is very rare. The severity of the clinical case presented by the patient required rapid and accurate diagnostic and therapeutic approaches. The clinical presentation of mononucleosis-like syndrome, associated with serological evidence of recent T. gondii infection and the finding of positive PCR for T. gondii in BAL allowed us to define the diagnosis. The rapid clinical recovery of the patient after beginning adequate therapy, with hospital discharge after only 10 days, confirms the correct therapeutic decision.
Footnotes
Conflict of interest: J.P. Steinhauser Motta has nothing to disclose.
Conflict of interest: I. Barbosa Cleinmann has nothing to disclose.
Conflict of interest: L.P. Palermo Bruno has nothing to disclose.
References
- 1.Cuomo G, D'Abrosca V, Rizzo V, et al. Severe polymyositis due to Toxoplasma Gondii in an adult immunocompetent patient: a case report and review. Infection 2013; 41: 859–862. doi: 10.1007/s15010-013-0427-x [DOI] [PubMed] [Google Scholar]
- 2.Carme B, Bissuel F, Ajzenberg D, et al. Severe acquired toxoplasmosis in immunocompetent adult patients in French Guiana. J Clin Microbiol 2002; 40: 4037–4044. doi: 10.1128/JCM.40.11.4037-4044.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anand R, Jones CW, Ricks JH, et al. Acute primary toxoplasmosis in travelers returning from endemic countries. J Travel Med 2012; 19: 57–60. doi: 10.1111/j.1708-8305.2011.00564.x [DOI] [PubMed] [Google Scholar]
- 4.Sun X, Lu H, Jia B, et al. A comparative study of Toxoplasma Gondii seroprevalence in three healthy Chinese populations detected using native and recombinant antigens. Parasit Vectors 2013; 6: 241. doi: 10.1186/1756-3305-6-241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schmidt M, Sonneville R, Schnell D, et al. Clinical features and outcomes in patients with disseminated toxoplasmosis admitted to intensive care: a multicenter study. Clin Infect Dis 2013; 57: 1535–1541. doi: 10.1093/cid/cit557 [DOI] [PubMed] [Google Scholar]
- 6.Fernandez-Sabé N, Cervera C, Fariñas MC, et al. Risk factors, clinical features, and outcomes of toxoplasmosis in solid-organ transplant recipients: a matched case-control study. Clin Infect Dis 2012; 54: 355–361. doi: 10.1093/cid/cir806 [DOI] [PubMed] [Google Scholar]
- 7.Balkhair AA, Al Murharrmii ZK, Ganguly S, et al. Spectrum of AIDS-defining opportunistic infections in a series of 77 hospitalized HIV-infected Omani patients. Clin Basic Res 2012; 12: 442–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rodrigues Cal RG, Rodrigues Marra A, Salomão Levy D. Toxoplasmose pulmonar – ocorrência em adulto imunocompetente [Pulmonary toxoplasmosis: occurrence in an immunocompetent adult]. Rev Ass Med Bras 2003; 49: 133–134. doi: 10.1590/S0104-42302003000200027 [DOI] [PubMed] [Google Scholar]
- 9.De Salvador-Guillouet F, Ajzenberg D, Chaillou-Opitz S, et al. Severe pneumonia during primary infection with an atypical strain of Toxoplasma gondii in an immunocompetent man. J Infect 2006; 53: 47–50. doi: 10.1016/j.jinf.2005.10.026 [DOI] [PubMed] [Google Scholar]
- 10.Leal FE, Cavazzana CL, Franco de Andrade H, et al. Toxoplasma gondii pneumonia in immunocompetent subjects: case report and review. Clin Infect Dis 2007; 44: e62–e66. doi: 10.1086/511871 [DOI] [PubMed] [Google Scholar]
- 11.Souza Neves E, Kropf A, Fernandes Bueno W, et al. Disseminated toxoplasmosis: an atypical presentation in an immunocompetent patient. Trop Doct 2011; 41: 59–60. doi: 10.1258/td.2010.100228 [DOI] [PubMed] [Google Scholar]
- 12.Simanaityte D, Le Gouellec N, Ajana F, et al. Primary pulmonary toxoplasmosis in an immunocompetent patient. Med Mal Infect 2010; 40: 713–715. doi: 10.1016/j.medmal.2010.03.013 [DOI] [PubMed] [Google Scholar]
- 13.Smati M, Taillé C, Menotti J, et al. Contribution of Toxoplasma-gondii specific PCR for the diagnosis of disseminated toxoplasmosis in a non-HIV and non-grafted adult patient. Med Mal Infect 2010; 40: 596–599. doi: 10.1016/j.medmal.2010.01.004 [DOI] [PubMed] [Google Scholar]
- 14.Ferreira IMR, Vidal JE, Brandão de Mattos C, et al. Toxoplasma gondii isolates: Multilocus RFLP-PCR genotyping from human patients in São Paulo state, Brazil identified distinct fenotypes. Exp Parasitol 2011; 129: 190–195. doi: 10.1016/j.exppara.2011.06.002 [DOI] [PubMed] [Google Scholar]
- 15.Yan J, Huang B, Liu G, et al. Meta-analysis of prevention and treatment of toxoplasmic encephalitis in HIV-infected patients. Acta Trop 2013; 127: 236–244. doi: 10.1016/j.actatropica.2013.05.006 [DOI] [PubMed] [Google Scholar]
- 16.Béraud G, Pierre-François S, Foltzer A, et al. Cotrimoxazole for treatment of cerebral toxoplasmosis: an observational cohort study during 1994–2006. Am J Trop Med Hyg 2009; 80: 583–587. doi: 10.4269/ajtmh.2009.80.583 [DOI] [PubMed] [Google Scholar]
- 17.Torre D, Casari S, Speranza F, et al. Randomized trial of trimethoprim-sulfamethoxazole versus pyrimethamine-sulfadiazine for therapy of toxoplasmic encephalitis in patients with AIDS. Antimicrob Agents Chemother 1998; 42: 1346–1349. doi: 10.1128/AAC.42.6.1346 [DOI] [PMC free article] [PubMed] [Google Scholar]