Abstract
Background
Individuals’ knowledge, attitude and practice towards preventive and precautionary measures of COVID-19 are essential to control the spread of the disease. Consequently, the aims of the study were to evaluate knowledge, attitude and practice of pharmacy students towards the pandemic and to assess its psychological impact on them to provide future guidance.
Methods
A cross-sectional, questionnaire-based study was conducted via a web-based survey in May 2020. All pharmacy students enrolled at Unaizah College of Pharmacy, Qassim University, were invited to take part in the study.
Results
A total of 232 out of 460 students took part in the study, giving a response rate of 50.43%. The mean total knowledge score was 9.87 ± 2.04 (maximum attainable score, 12). The majority of the participants (n=163; 70.3%) believed COVID-19 is a health threat to their community in the early months of the pandemic. Moreover, the majority (93%) also believed that the lockdown at the beginning of the pandemic was necessary to contain the pandemic. Encouragingly, 86.6% reported that they did not go to any crowded places during the pandemic with more female students avoiding crowded places compared to male students (91.6% versus 78.7%, respectively, P = 0.005). The majority (91%) also reported that they were following the strategies recommended by the authorities to prevent the spread of the virus. Encouragingly, 54.3% reported that the pandemic either had no effect or just a limited effect on their studies. However, 38.5% reported that they always felt or frequently felt nervous or anxious during the pandemic.
Conclusion
The study showed that pharmacy students had good knowledge as well as positive attitudes and good practices towards COVID-19 and the preventive measures. However, during the early months, the pandemic did have a negative psychological impact on a number of students. Consequently, proactive psychological and social support services to the students should be considered during the current and future pandemics. In addition, it is important to consider and proactively address key issues that could cause stress and anxiety among students when shifting to distance learning and assessments.
Keywords: coronavirus, COVID-19, mental health, pharmacy, Saudi Arabia
Introduction
Coronavirus disease (COVID-19) is an infectious disease caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The virus was first reported to the World Health Organization (WHO) country office in Wuhan, China on 31st December 2019 and on 30th January 2020, it was announced as a health emergency.1–3 On 11th March, the WHO announced this disease as a global pandemic.4 As of 9th January, 2021, there have been more than 87.3 million confirmed cases of COVID-19 with more than 1.89 million deaths globally.5 The SARS-CoV-2 is a contagious virus and spreads from human to human primarily through respiratory droplets and potentially aerosol transmission.6–8 The symptoms of COVID-19 infection include fever, cough, sore throat, fatigue and myalgia. In severe cases, it could lead to pneumonia, respiratory failure, cardiac arrest and death.9 However, it is estimated that 30% and up to 70% of patients in some studies could have the virus without showing symptoms of the disease,10–15 impacting on the control of the pandemic. Currently, preventive measures including social distancing, regular hand sanitization, regularly wiping surfaces, quarantining and the wearing face masks are the most effective methods to reducing the spread of the virus and its subsequent morbidity and mortality.7,16–19 Whilst many treatments have been proposed to treat patients with COVID-19, to date only dexamethasone has been shown to be effective in well-conducted clinical trials including the UK Recovery Trial and the WHO Solidarity trial.20,21 Consequently, many governments and health authorities, including the WHO, have been actively educating people to take preventive measures to reduce the spread of the virus including lockdown measures.22–25
However, we are aware that the COVID-19 pandemic and the instigation of lockdown measures have negatively impacted the management of non-communicable diseases (NCDs).26,27 This includes a considerable impact on the mental health of the population exacerbated by a lack of social interactions and fears with future employment,28–33 with COVID-19 and associated preventative measures increasing levels of anxiety, stress, frustration, depression, and insomnia as well as leading to emotional disturbance/alterations.33–38 Studies have also shown that work-related stress has increased among healthcare professionals (HCPs) during the pandemic.39,40 For example, Akudjedu et al reported that 63.2% of the radiology workforce in the UK have experienced work-related stress during the pandemic.40 In view of this, knowledge, attitude and practices towards the disease and associated preventive measures among the public and HCPs are an integral part to help control the spread of the pandemic and its impact. To date, there have been a number of studies assessing this among the general public,41–47 healthcare professionals,48–50 university students51–54 as well as a mixed sample.55 The findings suggest there was generally good knowledge and attitude towards COVID-19 and its associated preventative measures although room for behavioural improvement still exists.41–45,48–55
The first confirmed case of COVID-19 was reported in Saudi Arabia on 2nd March 2020.56,57 Similar to other countries including South Korea, Taiwan and Vietnam that built on their experiences with other emerging infectious diseases such as Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS),25,58–60 Saudi Arabia was one of the first countries globally to introduce proactive and early precautionary measures to help reduce the spread of the virus once introduced.57,61–64 The proactive measures included travel restrictions, closing shopping malls and enforcing lockdown measures, implementing curfews, suspending schools, universities and prayers at mosques, and limiting the number of employees at workplaces except for essential and critical services.57,61,62,64 As a result of these efforts, as of 9th January 2021, there were only 363,692 confirmed cases and 6286 deaths in Saudi Arabia,65 with preventative measures still in place. Online and distance learning at the schools and universities,66 as well as working from home, has been facilitated by major investments in digitalization, technology and artificial intelligence in Saudi Arabia in line with its 2030 vision.67
As a consequence of the pandemic, universities across countries including Saudi Arabia shifted their teaching to virtual and distance learning. However, we are aware this is likely to pose additional challenges to students at this anxious time, with levels of mental health disorders is already a concern among the population,68–82 and potentially exacerbated in university students. For instance, studies from the United States (US) reported that over 70% of the college students had increased stress and anxiety levels arising from the COVID-19 pandemic, although lower levels have been seen in China.74,83,84 However, we were unaware of any study conducted to date in Saudi Arabia to evaluate the knowledge, attitude and practice (KAP) regarding COVID-19 and its impact on pharmacy students’ mental health status. This is important given the growing role for pharmacists in delivering healthcare, which has become even more critical during the pandemic to give advice on prevention to patients as well as help with availability and advice about medicines for patients with NCDs given the concerns reported in the literature regarding the negative impact of the pandemic on the management of NCDs.23,26,85–87 Pharmacy students are future key HCPs in the community helping to control the spread of future infectious diseases, as well as the impact of any unintended consequences of any future pandemic. Consequently, we believe it is important to ascertain their KAP regarding COVID-19 and its impact on their mental health. The findings can be used to provide guidance to implement future initiatives.
Methodology
Study Design and Settings
A cross-sectional, questionnaire-based study was conducted via a web-based survey. All doctor of pharmacy (PharmD) students (2nd - 6th year) of Unaizah College of Pharmacy, Qassim University, were invited to participate in the study. A universal sampling method was used to collect the data using an online method. Consequently, all the 460 enrolled students in the college were invited to participate.
Development of the Questionnaire
A KAP questionnaire was adopted with permission from the original authors.43 The Cronbach’s alpha coefficient for the KAP questionnaire from our study was 0.728, which was seen as acceptable and shows consistency.88,89 An additional section was subsequently added. This included six questions to assess the psychological impact of COVID-19 on students’ life and studies based on a review of the literature and the authors’ experiences with this topic. The preliminary draft was discussed among the authors and was slightly modified after successive rounds of discussions. The modifications were minor and linguistic in nature to be suitable in the local context. To further ensure applicability, suitability and clarity in our setting, and to establish face and content validity, the draft questionnaire was given to four academicians for their review and comments. In addition, it was sent to ten pharmacy students for their review, comments and suggestions including its clarity, simplicity, and understanding. The questionnaire was subsequently refined and finalized following their comments before distribution. The responses during the pilot testing were not included in the full study.
The final questionnaire was designed and implemented using a Web-based survey platform with security features (Survey Monkey 2020, California). This included 12 statements to examine participants’ knowledge about COVID-19. A correct statement was given as a score of 1, and an incorrect one or do not know given a score of zero. The maximum knowledge score was 12. There were three attitude questions and three practice questions. The last section included six questions to assess the psychological impact of COVID-19 on students’ life and studies. The students were also given a list of choices about potential strategies adopted to improve their mental health status during curfew/lockdown periods based on previous studies and feedback. They were also given free space to write down any additional activities they were practicing.
Administration of the Survey
The final paper questionnaire was converted to an online web-based survey. Before administration, the web-based survey was tested on different web browsers to ensure robustness. In addition, the layout was checked on different devices including laptops, tablets, and smartphones to ensure ease of reading and answering the questions. Other technical and security features were also considered including IP addresses and no more than one response from the same device. A message with a link to the web-based survey was sent to the class leaders to invite all the registered students at Unaizah College of Pharmacy to participate in the study. The invitation message was sent via WhatsApp to all the ten class leaders (one leader for each class; five in male campus and five in female campus for the professional PharmD years 2nd–6th year). Subsequently, the class leaders delivered the invitation to their colleagues via the class WhatsApp groups. The invitation included the aim of the study, the estimated time to answer the questionnaire and statements on the anonymity of responses. The participation in the survey was strictly voluntary. Consent to take part in the study was assumed once participants responded to the online survey. The survey was conducted from 9th to 29th May 2020. After the original/initial invitation, three reminders were subsequently sent to participants to enhance the response rate.
Data Analysis
Statistical analyses (data screening, descriptive and inferential analysis) were performed using IBM SPSS statistics 20.0. Descriptive statistics were used to summarize the students’ responses to the KAP statements. These included frequencies, percentages, means, and standard deviations. Inferential statistics were used to ascertain the association between demographics and KAP level. Chi-square test for independence (χ2 test) and its alternative Fisher’s exact test were used to examine the association for categorical variables while independent-samples t-test and one-way ANOVA were used to examine the difference in the participants’ knowledge score in terms of their demographic characteristics, ie gender, education level, age, and health condition. A p-value of <0.05 was considered statistically significant.
Results
Demographic Characteristics of the Participants
A total of 232 out of 460 registered students took part in the study, giving a response rate of 50.43%. The mean age of the participants was 22.5 ± 1.70, and the majority of the participants were females (n=143; 61.64%). The participants were from all professional PharmD years (2nd–6th year) with the highest proportion from the sixth year (n=64; 27.6%) followed by fourth-year PharmD students (n=55; 23.8%). The vast majority of participants (n=214; 92.2%) did not have any coexisting diseases. Details of the demographics of the participants are given in Table 1.
Table 1.
Demographic Characteristics of Participants (N=232)
| Characteristics | n (%) |
|---|---|
| Age (Mean ± SD) | 22.5 ± 1.70 |
| Gender | |
| Male | 89 (38.36) |
| Female | 143 (61.64) |
| Year of Study | |
| 2nd | 39 (16.8) |
| 3rd | 35 (15) |
| 4th | 55 (23.8) |
| 5th | 39 (16.8) |
| 6th | 64 (27.6) |
| Coexisting disease | |
| Yes | 18 (7.8) |
| No | 214 (92.2) |
Knowledge, Attitude and Practice Regarding COVID-19
Knowledge About COVID-19 Among Participants
The mean total knowledge score was 9.87 ± 2.04 out of the maximum attainable score of 12. Consequently, the overall rate of correct answers for the knowledge statements was 82%. The details are presented in Table 2.
Table 2.
Knowledge About COVID-19 Among Participants (N=232)a
| Questions | Yes n (%) | No n (%) | Do Not Know n (%) |
|---|---|---|---|
| K1. The main clinical symptoms of COVID-19 are fever, fatigue, dry cough, and muscle pain. | 209 (90.1) | 15 (6.5) | 8 (3.4) |
| K2. Unlike the common cold, stuffy nose, runny nose, and sneezing are less common in persons infected with the COVID-19 virus. | 167 (72) | 34 (14.7) | 31 (13.4) |
| K3. Currently there is no effective cure for COVID-19, but early symptomatic and supportive treatment can help most patients to recover from the infection. | 212 (91.4) | 6 (2.6) | 14 (6.0) |
| K4. Not all persons with COVID-19 will develop severe cases. Those who are elderly, have chronic illnesses, and are obese are more likely to be severe cases. | 200 (86.2) | 17 (7.3) | 15 (6.5) |
| K5. Eating or contacting wild animals would result in the infection by the COVID-19 virus. | 50 (21.6) | 121 (52.2) | 61 (26.3) |
| K6. Persons with COVID-19 cannot spread the virus to others when the symptoms of COVID-19 are not present | 12 (5.2) | 204 (87.9) | 16 (6.9) |
| K7. The COVID-19 virus spreads via respiratory droplets of infected individuals. | 210 (90.5) | 8 (3.4) | 14 (6.0) |
| K8. Ordinary individuals can wear general medical masks to prevent the infection by the COVID-19 virus. | 143 (61.6) | 67 (28.9) | 22 (9.5) |
| K9. It is not necessary for children and young adults to take measures to prevent the infection by the COVID-19 virus. | 25 (10.8) | 200 (86.2) | 7 (3.0) |
| K10. To prevent the infection by COVID-19, individuals should avoid going to crowded places and avoid gatherings. | 216 (93.1) | 8 (3.4) | 8 (3.4) |
| K11. Test, Trace and Isolate (TTI) are the effective ways to reduce the spread of COVID-19. | 189 (81.5) | 2 (9) | 41 (17.7) |
| K12. People who have contact with someone infected with the COVID-19 virus should be immediately isolated in a proper place. In general, the observation period is 14 days. | 218 (94) | 4 (1.7) | 10 (4.3) |
Notes: aDue to rounding, percentages may not add up to 100%. Correct answers are presented in bold.
An analysis was performed to examine whether there were any statistically significant differences in the participants’ knowledge score in terms of their demographic characteristics, ie gender, education level, age, and health condition (Table 3). No statistically significant differences were noted (P > 0.05). Consequently, as the univariate analysis showed no statistically significant associations, multivariate regression analysis was not conducted.
Table 3.
The Difference Among Participants in Terms of Total Knowledge Score
| Variables | n | Total Knowledge Score Mean (SD) | p-valuea |
|---|---|---|---|
| Gender | |||
| Male | 89 | 9.71 (2.22) | 0.352 |
| Female | 143 | 9.97 (1.93) | |
| Age | |||
| 19–21 | 64 | 9.88 (2.05) | 0.948 |
| 22–24 | 136 | 9.84 (2.07) | |
| ≥ 25 | 32 | 9.97 (1.99) | |
| Year of study | |||
| 2nd | 39 | 9.77 (2.26) | 0.758 |
| 3rd | 35 | 9.80 (2.21) | |
| 4th | 55 | 9.98 (1.82) | |
| 5th | 39 | 9.54 (2.25) | |
| 6th | 64 | 10.06 (1.89) | |
| Coexisting disease | |||
| Yes | 18 | 10.00 (1.94) | 0.773 |
| No | 214 | 9.86 (2.06) |
Note: aIndependent-samples t-test and one-way ANOVA were used.
Attitude and Practice Towards COVID-19 Among Participants
The majority of the participants (n=165; 71.1%) agreed that COVID-19 will finally be successfully controlled. At the early stages of the pandemic, the majority (n=163; 70.3%) believed that COVID-19 is a health threat to the community. Moreover, the vast majority of participants (n=216; 93%) were of the opinion that the lockdown will improve the situation in Saudi Arabia. Regarding practices towards COVID-19, 201 participants (86.6%) did not go to any crowded places during these days and 155 participants (66%) reported wearing a mask when leaving home. Moreover, the vast majority of participants (n = 211; 91%) reported that they were following the strategies recommended by the authorities, eg the Ministry of Health, to prevent infection and spread of COVID-19. The details of the replies to the attitude and practice questions are summarized in Table 4.
Table 4.
Attitude and Practice Towards COVID-19 Among Participantsa
| Questions | Yes n (%) | No n (%) | Not Sure n (%) |
|---|---|---|---|
| Attitude | |||
| A1. Do you agree that COVID-19 will finally be successfully controlled? | 165 (71.1) | 17 (7.3) | 50 (21.6) |
| A2. Do you think that COVID-19 is a threat for your community? | 163 (70.2) | 25 (10.8) | 44 (19) |
| A3. I think that the lockdown would improve the overall well-being of the society in terms of controlling COVID-19 pandemic situation | 216 (93) | 6 (2.6) | 10 (4.4) |
| Practice | |||
| P1. In recent days, have you gone to any crowded place? | 31 (13.4) | 201 (86.6) | 0 (0) |
| P2. In recent days, have you worn a mask when leaving home? | 155 (66.8) | 77 (33.2) | 0 (0) |
| P3. Are you following the strategies recommended by authorities (eg Ministry of Health) to prevent the infection and spread of COVID-19? | 211 (91) | 7 (3) | 14 (6) |
Note: aDue to rounding, percentages may not add up to 100%.
The subsequent statistical analysis showed that there was no significant association between participants’ characteristics, ie their gender, education level, age, and health condition, and their attitude towards COVID-19 (P > 0.05) (Table S1). Similarly, a statistical analysis was performed to examine whether there were any associations between the sociodemographic characteristics and practices of the participants. As shown in Table S2, there was a statistically significant association between gender and the practice of going out to crowded places during the pandemic (P = 0.005). In this study, 131 (91.6%) of female participants reported avoiding any crowded places compared to 70 (78.7%) male participants.
Psychological Impact of COVID-19 on Participants
Impact of COVID-19 on Mental Status of Participants
More than one third of students (n= 89; 38.5%) reported that they always felt or frequently felt nervous or anxious during the current pandemic. Similarly, one third of students (n= 79; 34%) reported feeling down during the pandemic. However, a lower number (n= 59; 26%) always reported or frequently feeling little interest in doing things during the COVID-19 pandemic. Details of the impact of COVID-19 on the mental status of students are given in Table 5.
Table 5.
Impact of COVID-19 on Mental Status of Participantsa
| Descriptions | Always n (%) | Frequently n (%) | Occasionally n (%) | Rarely n (%) | Never n (%) |
|---|---|---|---|---|---|
| Feeling nervous/anxious | 37 (16) | 52 (22.5) | 75 (32) | 53 (23) | 15 (6.5) |
| Feeling hopeless/down | 33 (14) | 46 (20) | 59 (25) | 55 (24) | 39 (17) |
| Feeling little interest in doing things | 27 (12) | 32 (14) | 53 (23) | 63 (27) | 57 (25) |
Note: aDue to rounding, percentages may not add up to 100%.
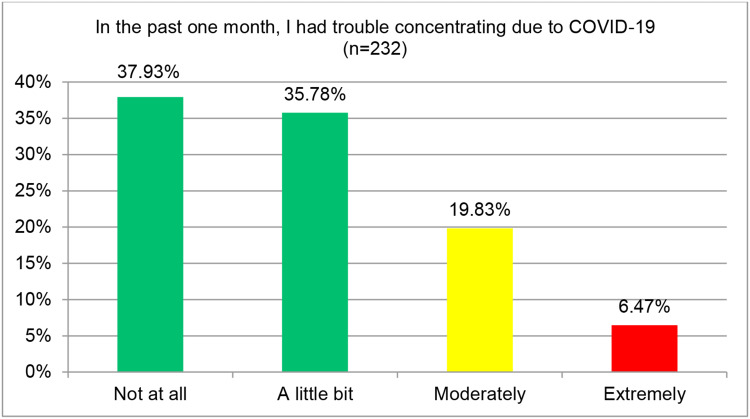
Impact of COVID-19 on Overall Concentration
When asked to what extent this pandemic had caused trouble concentrating, the majority of students (n=171; 73.7%) reported that the COVID-19 pandemic had no or limited impact on their overall concentration. However, approximately one quarter of participants (n=61; 26.3%) were affected. Figure 1 summarizes participant’s responses.
Figure 1.
Impact of COVID-19 on overall concentration of students.
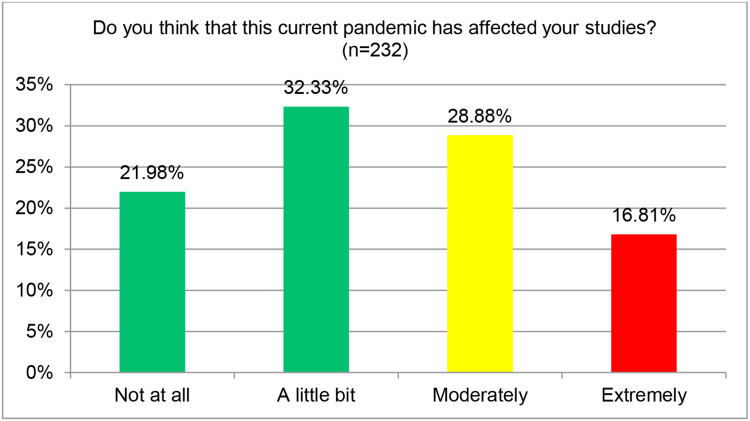
Impact of COVID-19 on Students’ Studies
More than half of the participants (n= 126; 54.3%) reported that the COVID-19 pandemic has either had no effect on their studies or just a limited effect. However, a considerable proportion of participants (n= 106; 45.7%) were affected by this pandemic. Details of the impact of COVID-19 on students’ studies are summarized in Figure 2.
Figure 2.
Impact of COVID-19 on the students’ study during the early stage of the pandemic.
Overall, there was no significant association between participants’ demographic characteristics, ie gender, education level, age, and health condition, and the statements related to the potential impact of COVID-19 on their concentration and studies (P > 0.05) (Table S3).
Strategies Used to Improve Psychological Health During the Lockdown
Maintaining social connections through online communication followed by staying close to normal life activities and eating healthy food/doing exercise were among the most common strategies the participants adopted to improve their mental health during the lockdown (Table 6). Many additional activities were reported in the free space. These included watching movies, reading the Quran (the holy book of Muslims), learning languages, providing families and community with reliable information about COVID-19, learning new things, eg painting and cooking, and playing online games.
Table 6.
Strategies Used to Improve Mental Health During the Lockdown Perioda
| Strategies | n (%) |
|---|---|
| Staying close to your normal life | 152 (65.52) |
| Eating healthy food and doing exercise | 145 (62.50) |
| Maintaining social connection and communication online | 154 (66.38) |
| Viewing the current situation as an opportunity to spend more time with family members | 123 (53.02) |
| Relying on authorities’ information (eg Ministry of Health) to keep updated with the level of risk | 132 (56.90) |
| Avoiding too much exposure to news about COVID-19 | 82 (35.34) |
| Viewing the current situation as an opportunity to improve skills in independent learning | 121 (52.16) |
| Others | 16 (6.90) |
Note: aThis is a multiple response question.
Discussion
To the best of our knowledge, we believe this is the first study to evaluate the KAP regarding COVID-19 and its impact on pharmacy students’ life and their studies in Saudi Arabia. The response rate of 50.43% was comparable to other studies conducted during the pandemic on this topic.54,78 Pharmacy students appeared to have good knowledge about the current pandemic with 82% having appropriate knowledge, and for most knowledge items, the vast majority of students gave correct answers. This is encouraging especially with the survey being conducted in the early stage of the pandemic in Saudi Arabia, and that it is consistent with other studies showing university students had good knowledge of the pandemic.51–53,90 Hamza et al researching senior pharmacy students from Egypt found the mean score of COVID-19 related knowledge was 83%,90 and Peng et al found that 82.3% of students in Shaanxi Province, China, also had good knowledge.52 However, our students had better knowledge than those reported by Singh et al in which the overall level of COVID-19 knowledge among students from India was only 66%.54 One area of concern with our study was the fact that in the statement “eating or contacting wild animals would result in the infection by the COVID-19 virus” only 52.2% of pharmacy students answered it correctly while 26.3% were not sure. However, the students in our study had better knowledge compared to the finding from a Jordanian study in which only 34.8% of medical students stated that transmission from animals is unlikely.53
Encouragingly, the majority of pharmacy students believed COVID-19 is a serious disease and poses a health threat to the community with 93% believing lockdown and curfew during the early stages of the pandemic was required for controlling the pandemic. This is similar to a study in India where 99.1% of students believed lockdown is a good strategy to control the pandemic54 as well as previous studies conducted with the general population in Saudi Arabia,63,91 India,92,93 and Pakistan.94 Perhaps not surprisingly, 91% of the student pharmacists stated they were following the strategies recommended by authorities to prevent the spread of the virus, reflected by 86.6% of participants reporting they did not go to any crowded places during the pandemic, consistent with the findings of Hamza et al.90 In our study, female pharmacy students were more likely to report avoiding crowded places compared to males (91.6% versus 78.7%, respectively), in line with findings among the Saudi public in which females were more likely to follow precautionary and preventive measures compared to males (53.6% versus 40.6%, respectively),63 students from China in which female students had better scores from practice statements towards COVID-19 compared to males63 and in Egypt where female students were 3.6 times more likely to avoid visiting crowded places than male students.90
In our study, 66% of participants reported wearing a mask when leaving home, similar to a study conducted among students in Jordan.51 A recent study in Egypt also reported that approximately 50% of pharmacy students were wearing a mask when leaving home.90 However, another study from Jordan reported that only 9.7% of students from six medical schools often or always wear a mask as a precautionary measure to prevent infection with the virus during the initial stage of the pandemic.53 This difference, despite evidence suggesting that wearing a face mask could reduce the risk of infection,16,95–97 could be explained by the fact that at the beginning of the pandemic, there were inconsistencies regarding the advice for face masks although this changed.96–98 Moreover, there was also a global shortage of masks initially with appreciable price rises in some countries.25,99–103 This was seen initially in Saudi Arabia where approximately 35% of community pharmacies in some areas had face masks for sale from April 20 to May 15 2020.104 Appreciable national efforts were subsequently made to ensure the wide availability of masks to the public. Following this, facemask wearing became mandatory in public in Saudi Arabia enforced by a penalty of 1000 SR on 30th May for violations.105 Consequently, we believe these activities resulted in the response rates seen in our study.
Of concern is that almost one third of students in our study reported being psychologically affected by the pandemic, lower though than studies in the US.74,84 However, similar to a study in Malaysia where 29.8% of surveyed students reported having anxiety,75 in Ethiopia where the prevalence of anxiety and stress among university students was 27.7% and 32.5%, respectively,76 and in Bangladesh where the prevalence of anxiety and stress among students was 33.3% and 28.5%, respectively.79 Consequently, support such as psychological counselling services and other support services are important for students during the pandemic. This could include digital psychological interventions such as digital applications, teleconsultations, and hotlines,75,82 as well as workshops on coping mechanisms and strategies.75 Alongside this, the shift to the emergency online learning should be undertaken in a smooth and careful way as this will be new to students and to avoid overloading students.75 Encouragingly, more than half of the participants in our study (54.3%) reported that the pandemic has either had no or a limited effect, with only 26.3% reporting having difficulty concentrating. These findings are better than studies in the US where 75.3% and 89% of the surveyed students, respectively, reported having difficulties in concentrating on academic work during the pandemic,74,77 and 58.6% had issues with online learning.77 A study with medical students from Australia also showed that 81% of students were concerned about the impact of the pandemic on their studies.78 The high rates could be due to several factors. These include the abrupt shift to online distance learning and assessments, major changes in living environments/conditions, increased social isolation/less interaction at the campus, as well as increased emotional and psychological distress.74,75,77,78,80,106 These are all considerations for the future.
We believe the lower impact of COVID-19 on the psychological health of our students compared to other studies could be due to several factors. These include the Saudi government taking early preventive measures such as reassurance of the public about the current situation and frequent updates and announcements about the ongoing efforts to control the virus through many awareness campaigns conducted by the Ministry of Health (MOH) and other government organizations using a variety of methods.57,64,107 In addition, Saudi government provided adequate resources and funding to help address the impact of the current pandemic. Alongside this, an appreciable investment in technology infrastructure and telehealth in recent years in line with Saudi vision 2030 was made.67,108 This investment resulted in 19 applications and digital platforms in the health care sector being used during the pandemic, facilitating the provision of health services including telemedicine and telecare.67 In addition, Qassim University had good technology infrastructure and e-learning systems even before the pandemic, and it was considered one of the most active e-learning universities in Saudi Arabia.67 In addition, proactive strategies from students were helpful including staying as close to their normal life as possible, eating healthy food and doing exercise, maintaining social connection and communication online, and viewing the current situation as an opportunity to spend more time with family members and improve their skills in independent learning (Table 6).
However, we believe there are several lessons learned that could be useful to enhance the quality of pharmacy education globally during the pandemic and beyond to reassure students and reduce any associated anxiety and stress. We believe having a good e-learning infrastructure including distance learning platforms is essential for the higher education institutions currently and in the future. This includes taking into consideration the appropriate re-structuring and formatting when converting traditional in-person teaching of courses to distance learning courses. We also believe that more investment in having telecommunication technology is necessary where pertinent to facilitate and sustain effective distance communication with students, academic faculty members, and administrative staff. Moreover, the availability of telemedicine and tele-delivery of supports services for pertinent students in a timely manner is also recommended during the pandemic and beyond. Furthermore, effective mechanisms are needed to ensure the early identification and assistance of students from vulnerable groups such as those with pre-existing mental health problems with telemedicine and other services to ensure their mental health is not exacerbated by the pandemic. There is also a need to support students with currently limited access to digital devices or the internet, or having problems with accommodation, during the pandemic to help alleviate the impact of the pandemic on their mental health.82
Limitations
We are aware that the study had a number of limitations. Firstly, it was conducted with pharmacy students from only one University. Consequently, it might not be generalized to other student populations in this and other universities in Saudi Arabia. Secondly, being an online survey, we relied on the responders accurately documenting their understanding and feelings without the ability to check this. However, this typically applies to all online surveys. Despite these limitations, we believe the study does provide useful insights into students’ perspectives and the impact of the pandemic on this population in Saudi Arabia and wider. Consequently, we believe the findings are useful to provide further guidance to education and health policy makers.
Conclusion
Pharmacy students in Saudi Arabia appeared to have good knowledge, positive attitude and good practices towards COVID-19 and the recommended preventive measures. In addition, several strategies were adopted by the students to stay positive and to cope with the situation during this pandemic. However, during the early months of the pandemic, this did have a negative psychological impact on a number of students. Consequently, proactive psychological and social support services to students should be considered essential during the pandemic. Alongside this, considering and proactively addressing key issues that could cause stress and anxiety among students when shifting to distance learning and assessments. More efforts may be needed to ensure that face-to-face courses are subsequently delivered in a suitable online format with pertinent assessments and tasks without overload. In addition, offering telemedicine and other support services to help preserve the mental health of students.
Funding Statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Abbreviations
COVID-19, Coronavirus disease; HCPs, Healthcare professionals; KAP, Knowledge, Attitude and Practice; MERS, Middle East Respiratory Syndrome; MOH, Ministry of Health; NCDs, non-communicable diseases; PharmD, Doctor of Pharmacy; SARS, Severe Acute Respiratory Syndrome; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; SD, Standard deviation; UK, United Kingdom; US, United States; WHO, World Health Organization.
Data Sharing Statement
The data will be available from the corresponding author upon reasonable request.
Ethical Approval
Ethical approval was obtained from the Committee of Health Research Ethics, Deanship of Scientific Research, Qassim University (Approval No. 19-11-01).
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Deng SQ, Peng HJ. Characteristics of and public health responses to the coronavirus disease 2019 outbreak in China. J Clin Med. 2020;9(2):575. doi: 10.3390/jcm9020575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO. COVID-19 Public Health Emergency of International Concern (PHEIC) – Global research and innovation forum; February 12, 2020. Available from: https://www.who.int/publications/m/item/covid-19-public-health-emergency-of-international-concern-(pheic)-global-research-and-innovation-forum. Accessed January11, 2021.
- 3.Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199–1207. doi: 10.1056/NEJMoa2001316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO. Coronavirus disease (COVID-2019). Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Accessed January11, 2021.
- 5.WHO. WHO Coronavirus disease (COVID-19) dashboard; January 10, 2021. Available from: https://covid19.who.int/table. Accessed January11, 2021.
- 6.WHO. Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations. Scientific Brief 29 March 2020. Available from: https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations. Accessed January11, 2021.
- 7.Pradhan D, Biswasroy P, Kumar Naik P, Ghosh G, Rath G. A review of current interventions for COVID-19 prevention. Arch Med Res. 2020;51(5):363–374. doi: 10.1016/j.arcmed.2020.04.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Klompas M, Baker MA, Rhee C. Airborne transmission of SARS-CoV-2: theoretical considerations and available evidence. JAMA. 2020;324(5):441–442. doi: 10.1001/jama.2020.12458 [DOI] [PubMed] [Google Scholar]
- 9.Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wong RSY. The SARS-CoV-2 outbreak: an epidemiological and clinical perspective. SN Compr Clin Med. 2020;2:1983–1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nishiura H, Kobayashi T, Miyama T, et al. Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19). Int J Infect Dis. 2020;94:154–155. doi: 10.1016/j.ijid.2020.03.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mizumoto K, Kagaya K, Zarebski A, Chowell G. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Euro Surveill. 2020;25(10):2000180. doi: 10.2807/1560-7917.ES.2020.25.10.2000180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huff HV, Singh A. Asymptomatic transmission during the COVID-19 pandemic and implications for public health strategies. Clin Infect Dis. 2020;71(10):2752–2756. doi: 10.1093/cid/ciaa654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Day M. Covid-19: identifying and isolating asymptomatic people helped eliminate virus in Italian village. BMJ. 2020;368:m1165. doi: 10.1136/bmj.m1165 [DOI] [PubMed] [Google Scholar]
- 15.Lan FY, Suharlim C, Kales SN, Yang J. Association between SARS-CoV-2 infection, exposure risk and mental health among a cohort of essential retail workers in the USA. Occup Environ Med. 2020;oemed-2020-106774. doi: 10.1136/oemed-2020-106774 [DOI] [PubMed] [Google Scholar]
- 16.Feng S, Shen C, Xia N, Song W, Fan M, Cowling BJ. Rational use of face masks in the COVID-19 pandemic. Lancet Respir Med. 2020;8(5):434–436. doi: 10.1016/S2213-2600(20)30134-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nussbaumer-Streit B, Mayr V, Dobrescu AI, et al. Quarantine alone or in combination with other public health measures to control COVID-19: a rapid review. Cochrane Database Syst Rev. 2020;4(4):Cd013574. doi: 10.1002/14651858.CD013574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Courtemanche C, Garuccio J, Le A, Pinkston J, Yelowitz A. Strong social distancing measures in the United States reduced the COVID-19 growth rate. Health Aff. 2020;39(7):1237–1246. doi: 10.1377/hlthaff.2020.00608 [DOI] [PubMed] [Google Scholar]
- 19.Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395(10242):1973–1987. doi: 10.1016/S0140-6736(20)31142-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abubakar AR, Sani IH, Godman B, et al. Systematic review on the therapeutic options for COVID-19: clinical evidence of drug efficacy and implications. Infect Drug Resist. 2020;13:4673. doi: 10.2147/IDR.S289037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dyer O. Covid-19: remdesivir has little or no impact on survival, WHO trial shows. BMJ. 2020;371:m4057. doi: 10.1136/bmj.m4057 [DOI] [PubMed] [Google Scholar]
- 22.WHO. COVID-19 strategic preparedness and response plan – operational planning guidelines to support country preparedness and response; 2020. Available from: https://www.who.int/docs/default-source/coronaviruse/covid-19-sprp-unct-guidelines.pdf. Accessed January11, 2021.
- 23.Ogunleye OO, Basu D, Mueller D, et al. Response to the novel Corona Virus (COVID-19) pandemic across Africa: successes, challenges, and implications for the future. Front Pharmacol. 2020;11:1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Afriyie DK, Asare GA, Amponsah SK, Godman B. COVID-19 pandemic in resource-poor countries: challenges, experiences and opportunities in Ghana. J Infect Dev Ctries. 2020;14(8):838–843. doi: 10.3855/jidc.12909 [DOI] [PubMed] [Google Scholar]
- 25.Godman B, Haque M, Islam S, et al. Rapid assessment of price instability and paucity of medicines and protection for COVID-19 across Asia: findings and public health implications for the future. Front Public Health. 2020;8. doi: 10.3389/fpubh.2020.585832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kluge HHP, Wickramasinghe K, Rippin HL, et al. Prevention and control of non-communicable diseases in the COVID-19 response. Lancet. 2020;395(10238):1678–1680. doi: 10.1016/S0140-6736(20)31067-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Palmer K, Monaco A, Kivipelto M, et al. The potential long-term impact of the COVID-19 outbreak on patients with non-communicable diseases in Europe: consequences for healthy ageing. Aging Clin Exp Res. 2020;32(7):1189–1194. doi: 10.1007/s40520-020-01601-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.González-Sanguino C, Ausín B, Castellanos M, et al. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun. 2020;87:172–176. doi: 10.1016/j.bbi.2020.05.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rajkumar RP. COVID-19 and mental health: A review of the existing literature. Asian J Psychiatr. 2020;52:102066. doi: 10.1016/j.ajp.2020.102066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Torales J, O’Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. 2020;66(4):317–320. doi: 10.1177/0020764020915212 [DOI] [PubMed] [Google Scholar]
- 32.Xiong J, Lipsitz O, Nasri F, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dubey S, Biswas P, Ghosh R, et al. Psychosocial impact of COVID-19. Diabetes Metab Syndr. 2020;14(5):779–788. doi: 10.1016/j.dsx.2020.05.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Alkhamees AA, Alrashed SA, Alzunaydi AA, Almohimeed AS, Aljohani MS. The psychological impact of COVID-19 pandemic on the general population of Saudi Arabia. Compr Psychiatry. 2020;102:152192. doi: 10.1016/j.comppsych.2020.152192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Burhamah W, AlKhayyat A, Oroszlányová M, et al. The psychological burden of the COVID-19 pandemic and associated lockdown measures: experience from 4000 participants. J Affect Disord. 2020;277:977–985. doi: 10.1016/j.jad.2020.09.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tee ML, Tee CA, Anlacan JP, et al. Psychological impact of COVID-19 pandemic in the Philippines. J Affect Disord. 2020;277:379–391. doi: 10.1016/j.jad.2020.08.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Serafini G, Parmigiani B, Amerio A, Aguglia A, Sher L, Amore M. The psychological impact of COVID-19 on the mental health in the general population. QJM. 2020;113(8):531–537. doi: 10.1093/qjmed/hcaa201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McCracken LM, Badinlou F, Buhrman M, Brocki KC. Psychological impact of COVID-19 in the Swedish population: depression, anxiety, and insomnia and their associations to risk and vulnerability factors. Eur Psychiatry. 2020;63(1):e81. doi: 10.1192/j.eurpsy.2020.81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Elshami W, Akudjedu TN, Abuzaid M, et al. The radiology workforce’s response to the COVID-19 pandemic in the Middle East, North Africa and India. Radiography. 2020. doi: 10.1016/j.radi.2020.09.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Akudjedu TN, Lawal O, Sharma M, et al. Impact of the COVID-19 pandemic on radiography practice: findings from a UK radiography workforce survey. BJR|Open. 2020;2(1):20200023. doi: 10.1259/bjro.20200023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Azlan AA, Hamzah MR, Sern TJ, Ayub SH, Mohamad E. Public knowledge, attitudes and practices towards COVID-19: A cross-sectional study in Malaysia. PLoS One. 2020;15(5):e0233668. doi: 10.1371/journal.pone.0233668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kebede Y, Yitayih Y, Birhanu Z, Mekonen S, Ambelu A. Knowledge, perceptions and preventive practices towards COVID-19 early in the outbreak among Jimma university medical center visitors, Southwest Ethiopia. PLoS One. 2020;15(5):e0233744. doi: 10.1371/journal.pone.0233744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhong B-L, Luo W, Li H-M, et al. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int J Biol Sci. 2020;16(10):1745–1752. doi: 10.7150/ijbs.45221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Reuben RC, Danladi MMA, Saleh DA, Ejembi PE. Knowledge, attitudes and practices towards COVID-19: an epidemiological survey in North-Central Nigeria. J Community Health. 2020. doi: 10.1007/s10900-020-00881-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Al-Hanawi MK, Angawi K, Alshareef N, et al. Knowledge, attitude and practice toward COVID-19 among the public in the Kingdom of Saudi Arabia: a cross-sectional study. Front Public Health. 2020;8:217. doi: 10.3389/fpubh.2020.00217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kasemy ZA, Bahbah WA, Zewain SK, et al. Knowledge, attitude and practice toward COVID-19 among Egyptians. J Epidemiol Glob Health. 2020;10(4):378–385. doi: 10.2991/jegh.k.200909.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bates BR, Moncayo AL, Costales JA, Herrera-Cespedes CA, Grijalva MJ. Knowledge, attitudes, and practices towards COVID-19 among Ecuadorians during the outbreak: an online cross-sectional survey. J Community Health. 2020;45(6):1158–1167. doi: 10.1007/s10900-020-00916-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Huynh G, Nguyen T, Tran V, Vo K, Vo V, Pham L. Knowledge and attitude toward COVID-19 among healthcare workers at District 2 Hospital, Ho Chi Minh City. Asian Pac J Trop Med. 2020;13(6):260–265. doi: 10.4103/1995-7645.280396 [DOI] [Google Scholar]
- 49.Shi Y, Wang J, Yang Y, et al. Knowledge and attitudes of medical staff in Chinese psychiatric hospitals regarding COVID-19. Brain Behav Immun Health. 2020;4:100064. doi: 10.1016/j.bbih.2020.100064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Saqlain M, Munir MM, Rehman SU, et al. Knowledge, attitude, practice and perceived barriers among healthcare workers regarding COVID-19: a cross-sectional survey from Pakistan. J Hosp Infect. 2020;105(3):419–423. doi: 10.1016/j.jhin.2020.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Alzoubi H, Alnawaiseh N, Al-Mnayyis A, Lubad MA, Aqel A, Al-Shagahin H. COVID-19-knowledge, attitude and practice among medical and non-medical University Students in Jordan. J Pure Appl Microbiol. 2020;14:17–24. doi: 10.22207/JPAM.14.1.04 [DOI] [Google Scholar]
- 52.Peng Y, Pei C, Zheng Y, et al. A cross-sectional survey of knowledge, attitude and practice associated with COVID-19 among undergraduate students in China. BMC Public Health. 2020;20:1292. doi: 10.1186/s12889-020-09392-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Khasawneh AI, Humeidan AA, Alsulaiman JW, et al. Medical students and COVID-19: knowledge, Attitudes, and Precautionary Measures. A descriptive study from Jordan. Front Public Health. 2020;8:253. doi: 10.3389/fpubh.2020.00253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Prasad Singh J, Sewda A, Shiv DG. Assessing the knowledge, attitude and practices of students regarding the COVID-19 pandemic. J Health Manag. 2020;22(2):281–290. doi: 10.1177/0972063420935669 [DOI] [Google Scholar]
- 55.Modi PD, Nair G, Uppe A, et al. COVID-19 awareness among healthcare students and professionals in Mumbai metropolitan region: a questionnaire-based survey. Cureus. 2020;12(4):e7514. doi: 10.7759/cureus.7514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.AlHumaid J, Ali S, Farooq I. The psychological effects of the COVID-19 pandemic and coping with them in Saudi Arabia. Psychol Trauma. 2020;12(5):505–507. doi: 10.1037/tra0000623 [DOI] [PubMed] [Google Scholar]
- 57.Algaissi AA, Alharbi NK, Hassanain M, Hashem AM. Preparedness and response to COVID-19 in Saudi Arabia: building on MERS experience. J Infect Public Health. 2020;13(6):834–838. doi: 10.1016/j.jiph.2020.04.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Exemplars in Global Health. Emerging COVID-19 success story: South Korea learned the lessons of MERS; June 30, 2020. Available from: https://ourworldindata.org/covid-exemplar-south-korea. Accessed January11, 2021.
- 59.Pham QT, Rabaa MA, Duong HL, et al. The first 100 days of SARS-CoV-2 control in Vietnam. Clin Infect Dis. 2020;ciaa1130. doi: 10.1093/cid/ciaa1130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wang CJ, Ng CY, Brook RH. Response to COVID-19 in Taiwan: big data analytics, new technology, and proactive testing. JAMA. 2020;323(14):1341–1342. doi: 10.1001/jama.2020.3151 [DOI] [PubMed] [Google Scholar]
- 61.Nurunnabi M. The preventive strategies of COVID-19 pandemic in Saudi Arabia. J Microbiol Immunol Infect. 2020. doi: 10.1016/j.jmii.2020.07.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Alshammari TM, Altebainawi AF, Alenzi KA. Importance of early precautionary actions in avoiding the spread of COVID-19: Saudi Arabia as an Example. Saudi Pharm J. 2020;28(7):898–902. doi: 10.1016/j.jsps.2020.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Almutairi AF, BaniMustafa AA, Alessa YM, Almutairi SB, Almaleh Y. Public trust and compliance with the precautionary measures against COVID-19 employed by authorities in Saudi Arabia. Risk Manag Healthc Policy. 2020;13:753. doi: 10.2147/RMHP.S257287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Obied DA, Alhamlan FS, Al-Qahtani AA, Al-Ahdal MN. Containment of COVID-19: the unprecedented response of Saudi Arabia. J Infect Dev Ctries. 2020;14(7):699–706. doi: 10.3855/jidc.13203 [DOI] [PubMed] [Google Scholar]
- 65.WHO Eastern Mediterranean Office (EMRO). COVID-19 situation in the Region – total reports – Situation as of 9 January 2021. Available from: http://www.emro.who.int/health-topics/corona-virus/index.html. Accessed January 2021.
- 66.Shawaqfeh MS, Al Bekairy AM, Al-Azayzih A, et al. Pharmacy students perceptions of their distance online learning experience during the COVID-19 pandemic: a cross-sectional survey study. J Med Educ Curric Dev. 2020;7:2382120520963039. doi: 10.1177/2382120520963039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hassounah M, Raheel H, Alhefzi M. Digital response during the COVID-19 pandemic in Saudi Arabia. J Med Internet Res. 2020;22(9):e19338. doi: 10.2196/19338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sahu P. Closure of universities due to coronavirus disease 2019 (COVID-19): impact on education and mental health of students and academic staff. Cureus. 2020;12(4):e7541. doi: 10.7759/cureus.7541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Meo SA, Abukhalaf AA, Alomar AA, Sattar K, Klonoff DC. COVID-19 pandemic: impact of quarantine on medical students’ mental wellbeing and learning behaviors. Pak J Med Sci. 2020;36(Covid19–s4):S43–S48. doi: 10.12669/pjms.36.COVID19-S4.2809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Auerbach RP, Mortier P, Bruffaerts R, et al. WHO world mental health surveys International College student project: prevalence and distribution of mental disorders. J Abnorm Psychol. 2018;127(7):623–638. doi: 10.1037/abn0000362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Castaldelli-Maia JM, Lewis T, Marques Dos Santos N, et al. Stressors, psychological distress, and mental health problems amongst Brazilian medical students. Int Rev Psychiatry. 2019;31(7–8):603–607. doi: 10.1080/09540261.2019.1669335 [DOI] [PubMed] [Google Scholar]
- 72.Ibrahim AK, Kelly SJ, Adams CE, Glazebrook C. A systematic review of studies of depression prevalence in university students. J Psychiatr Res. 2013;47(3):391–400. doi: 10.1016/j.jpsychires.2012.11.015 [DOI] [PubMed] [Google Scholar]
- 73.Liang S-W, Chen R-N, Liu -L-L, et al. The Psychological Impact of the COVID-19 epidemic on Guangdong College students: the difference between seeking and not seeking psychological help. Front Psychol. 2020;11:2231. doi: 10.3389/fpsyg.2020.02231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Son C, Hegde S, Smith A, Wang X, Sasangohar F. Effects of COVID-19 on college students’ mental health in the United States: interview survey study. J Med Internet Res. 2020;22(9):e21279. doi: 10.2196/21279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sundarasen S, Chinna K, Kamaludin K, et al. Psychological impact of COVID-19 and lockdown among University Students in Malaysia: implications and policy recommendations. Int J Environ Res Public Health. 2020;17(17):6206. doi: 10.3390/ijerph17176206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Aylie NS, Mekonen MA, Mekuria RM. The psychological impacts of COVID-19 pandemic among University Students in Bench-Sheko Zone, South-west Ethiopia: a community-based cross-sectional study. Psychol Res Behav Manag. 2020;13:813–821. doi: 10.2147/PRBM.S275593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kecojevic A, Basch CH, Sullivan M, Davi NK. The impact of the COVID-19 epidemic on mental health of undergraduate students in New Jersey, cross-sectional study. PLoS One. 2020;15(9):e0239696. doi: 10.1371/journal.pone.0239696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lyons Z, Wilcox H, Leung L, Dearsley O. COVID-19 and the mental well-being of Australian medical students: impact, concerns and coping strategies used. Australas Psychiatry. 2020;28(6):649–652. doi: 10.1177/1039856220947945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Khan AH, Sultana MS, Hossain S, Hasan MT, Ahmed HU, Sikder MT. The impact of COVID-19 pandemic on mental health & wellbeing among home-quarantined Bangladeshi students: a cross-sectional pilot study. J Affect Disord. 2020;277:121–128. doi: 10.1016/j.jad.2020.07.135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kapasia N, Paul P, Roy A, et al. Impact of lockdown on learning status of undergraduate and postgraduate students during COVID-19 pandemic in West Bengal, India. Child Youth Serv Rev. 2020;116:105194. doi: 10.1016/j.childyouth.2020.105194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Rainford LA, Zanardo M, Buissink C, et al. The impact of COVID-19 upon student radiographers and clinical training. Radiography. 2020. doi: 10.1016/j.radi.2020.10.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Sharma D, Bhaskar S. Addressing the Covid-19 burden on medical education and training: the role of telemedicine and tele-education during and beyond the pandemic. Front Public Health. 2020;8:589669. doi: 10.3389/fpubh.2020.589669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Cao W, Fang Z, Hou G, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wang X, Hegde S, Son C, Keller B, Smith A, Sasangohar F. Investigating mental health of US college students during the COVID-19 pandemic: cross-sectional survey study. J Med Internet Res. 2020;22(9):e22817. doi: 10.2196/22817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hedima EW, Adeyemi MS, Ikunaiye NY. Community Pharmacists: on the frontline of health service against COVID-19 in LMICs. Res Social Adm Pharm. 2021;17(1):1964–1966. doi: 10.1016/j.sapharm.2020.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Cadogan CA, Hughes CM. On the frontline against COVID-19: community pharmacists’ contribution during a public health crisis. Res Social Adm Pharm. 2021;17(1):2032–2035. doi: 10.1016/j.sapharm.2020.03.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ung COL. Community pharmacist in public health emergencies: quick to action against the coronavirus 2019-nCoV outbreak. Res Social Adm Pharm. 2020;16(4):583–586. doi: 10.1016/j.sapharm.2020.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Tavakol M, Dennick R. Making sense of Cronbach’s alpha. Int J Med Educ. 2011;2:53–55. doi: 10.5116/ijme.4dfb.8dfd [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Bland JM, Altman DG. Statistics notes: cronbach’s alpha. BMJ. 1997;314(7080):572. doi: 10.1136/bmj.314.7080.572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hamza MS, Badary OA, Elmazar MM. Cross-sectional study on awareness and knowledge of COVID-19 among senior pharmacy students. J Community Health. 2021;46(1):139–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Alahdal H, Basingab F, Alotaibi R. An analytical study on the awareness, attitude and practice during the COVID-19 pandemic in Riyadh, Saudi Arabia. J Infect Public Health. 2020;13(10):1446–1452. doi: 10.1016/j.jiph.2020.06.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Pal R, Yadav U, Grover S, Saboo B, Verma A, Bhadada SK. Knowledge, attitudes and practices towards COVID-19 among young adults with Type 1 diabetes mellitus amid the nationwide lockdown in India: A cross-sectional survey. Diabetes Res Clin Pract. 2020;166:108344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kartheek A, Gara K, Vanamali D. Knowledge, attitude and practices towards COVID-19 among Indian residents during the pandemic: A cross-sectional online survey. J NTR Univ Health Sci. 2020;9(2):107–115. doi: 10.4103/JDRNTRUHS.JDRNTRUHS_75_20 [DOI] [Google Scholar]
- 94.Ali A, Farooq S, Khalid N, Ahmed F. Awareness, attitude and practices related to COVID-19 pandemic in General Public of Province Sindh, Pakistan. Pak J Med Dent. 2020;9(3):90–95. [Google Scholar]
- 95.Liang M, Gao L, Cheng C, et al. Efficacy of face mask in preventing respiratory virus transmission: A systematic review and meta-analysis. Travel Med Infect Dis. 2020;36:101751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lim S, Yoon HI, Song KH, Kim ES, Kim HB. Face masks and containment of COVID-19: experience from South Korea. J Hosp Infect. 2020;106(1):206–207. doi: 10.1016/j.jhin.2020.06.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lyu W, Wehby GL. Community use of face masks and COVID-19: evidence from a natural experiment of state mandates in the US. Health Aff (Millwood). 2020;39(8):1419–1425. doi: 10.1377/hlthaff.2020.00818 [DOI] [PubMed] [Google Scholar]
- 98.Cheng KK, Lam TH, Leung CC. Wearing face masks in the community during the COVID-19 pandemic: altruism and solidarity. Lancet. 2020. doi: 10.1016/S0140-6736(20)30918-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Wu H-L, Huang J, Zhang CJP, He Z, Ming W-K. Facemask shortage and the novel coronavirus disease (COVID-19) outbreak: reflections on public health measures. EClinicalMedicine. 2020;21:100329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Mahase E. Novel coronavirus: Australian GPs raise concerns about shortage of face masks. BMJ. 2020;368:m477. doi: 10.1136/bmj.m477 [DOI] [PubMed] [Google Scholar]
- 101.McMahon DE, Peters GA, Ivers LC, Freeman EE. Global resource shortages during COVID-19: bad news for low-income countries. PLoS Negl Trop Dis. 2020;14(7):e0008412. doi: 10.1371/journal.pntd.0008412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Livingston E, Desai A, Berkwits M. Sourcing personal protective equipment during the COVID-19 pandemic. JAMA. 2020;323(19):1912–1914. doi: 10.1001/jama.2020.5317 [DOI] [PubMed] [Google Scholar]
- 103.Sefah IA, Ogunleye OO, Essah DO, et al. Rapid assessment of the potential paucity and price increases for suggested medicines and protection equipment for COVID-19 across developing countries with a particular focus on Africa and the implications. Front Pharmacol. 2020. doi: 10.3389/fphar.2020.588106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Khojah HMJ. Community pharmacy services and preparedness during COVID-19 outbreak in Madinah, Saudi Arabia. Saudi Pharm J. 2020;28(11):1402–1407. doi: 10.1016/j.jsps.2020.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ministry of interior approves revising regulations on limiting gatherings, updating violations classification schedule. Available from: https://www.spa.gov.sa/viewfullstory.php?lang=en&newsid=2092897. Accessed October23, 2020.
- 106.Aucejo EM, French J, Ugalde Araya MP, Zafar B. The impact of COVID-19 on student experiences and expectations: evidence from a survey. J Public Econ. 2020;191:104271. doi: 10.1016/j.jpubeco.2020.104271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Alumran A. Role of precautionary measures in containing the natural course of novel coronavirus disease. J Multidiscip Healthc. 2020;13:615. doi: 10.2147/JMDH.S261643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Alghamdi S, Alqahtani J, Aldhahir A. Current status of telehealth in Saudi Arabia during COVID-19. J Family Community Med. 2020;27(3):208–211. doi: 10.4103/jfcm.JFCM_295_20 [DOI] [PMC free article] [PubMed] [Google Scholar]