Abstract
Background & Objective
To identify patient’s factors from their clinical picture and demographics, and recognize their association and influence on frequency of physician visit.
Method
Study was conducted in Karachi from January – December 2019. Primary data was collected from 255 asthmatic patients that visited different hospitals, homeopathic and herbal clinics. Questionnaire included patient’s demographic details, treatment choice for asthma and satisfaction level with different treatments. Collected data was analyzed by SPSS 20.
Result
Among 255 asthmatic patients, 101 visited 5 – 7 times to physician from the past year, 48 visited 8–10 times and 27 went to physician more than 10 times in past 12 months. While 30 patients did not visit the physician even once and only 20 patients visited 1–2 times in the last year. From clinical factors, association of severity (p = 0.0001), limitation (p = 0.0001) and side effects (p = 0.003) with physician visit were found to be statistically significant. In addition, among demographics, age (p = 0.004), education (p = 0.0001), income (p = 0.0001) and having pets (p = 0.007) were found to be significant factors associated with physician visit for asthma in the past year.
Conclusion
Most of the asthmatic patients covered in the study visited the physician more than five times during the last year and chose allopathic treatment for asthma. Age, education, severity and side effects of asthma treatment were some of the significant factors associated with physician visit. Patients with frequent follow up visits to the physician were satisfied with their treatment.
Keywords: Asthma, Physician visits, Treatment satisfaction, Patient demographic, Asthma severity
1. Introduction
For providing a better and quality health care system, patient’s values and preferences can play a major role. Physicians, clinicians, specialists and researchers have also focused on the importance of patient involvement in providing patient centered care. However, it also had brought many challenges for physicians in terms of giving extra time, communication skills and interaction with the patients (Say and Thomson, 2003). Several studies have suggested that patient’s individuality and patient-physician interactions contributes significantly in developing patient value and preference and they have a huge impact on their treatment decisions (Lee et al., 2013, Bastemeijer et al., 2017). For incorporation of patient values in health care system, it’s important to understand the patient factors and provide a better treatment in various long-term ailments.
Asthma has emerged as a worldwide public health problem with approximately 300 million patients and expected to increase by 100 million by 2025 (Dharmage et al., 2019). Various treatments including allopathic and alternative methods are widely used for asthma. However, studies showed that asthma is still poorly controlled in a significant proportion of patients (Society) and concluded that more attention should be given to patient-focused care in asthma. The modifications according to patient needs and requirements may result in improved asthma management and reduced morbidity (van der Molen et al., 2018). With significant worldwide burden of asthma, it is necessary to enhance understanding of patient characteristics that may be related with their needs and to identify different groups of patients who may benefit most from addressing their needs. This can play a major role in development of custom-made patient-adjusted interventions (Kritikos et al., 2019).
Frequent clinical visits might increase the opportunity to increase adherence, compliance and reduces the risk of hospitalization (Park et al., 2018). When patients visit clinics regularly, physicians may provide more consideration to patients, educate patients well, understand patient’s individual needs more properly and suggest appropriate medication for a particular patient. Together, this might result in an improved prognosis (Zeng et al., 2018). Other explanations for frequent physician visit or to emergency department includes asthma severity, poor compliance, the inappropriate use of inhalers, the cost of medication, lack of an asthma controlling action plan, co-morbidities, over reliance on short acting bronchodilators, pollution and changes in the weather, the patient’s level of education and low socioeconomic status (Srivastava, 2017). Additionally, patient individual characteristics such as gender, age and tobacco use can play a significant role (Nunes et al., 2017).
This study had been designed to identify the regularity of physician visits by asthma patients based upon his/her preferences, to recognize association between patients’ individual characteristics such as demographics and clinical picture of asthma with the frequency of physician visits.
2. Method
The study design was cross sectional and observational. The multicenter study was conducted at government hospitals, private hospitals and clinics. Duration of study was from January 2019 to December 2019. The sample size was calculated by precision analysis technique (Aparasu, 2016). The study includes 255 asthmatic patients from different centers all over the city.
2.1. Hypothesis
The hypothesis of the study was that the demographics and clinical presentation of asthmatic patients has impact on frequency of physician visit.
2.2. Ethical Aproval
Ethical approval of study has been taken from Institutional Bioethics Committee, University of Karachi with approval No. IBC-KU-24.
2.3. Data collection
The structured questionnaire was used for primary data collection; the questionnaire was finalized after multiple iterations and pilot testing in the field. The questionnaire was both in English and Urdu language for better understanding. The questionnaire for each respondent was completed through face-to-face interview. All participants of the study provided informed consent before the interview. The questionnaire for this study includes patient’s age, gender, family history of asthma, frequency of visiting physician in last 12 months, and choice of treatment of asthma with conventional and/or alternative medicines. In this study, we interviewed asthmatic patients and asked them about number of visits to physician for asthma treatment in the last 12 months. Asthmatic patients, both male and female of age above 13 were included in the study while asthmatic children under age 13 years were excluded from the study.
2.4. Data analysis
The data for study was analyzed by SPSS (version 20). The responses for different groups were compared using Chi square test. Any result with a p < 0.05 was considered as significant for this study.
3. Results
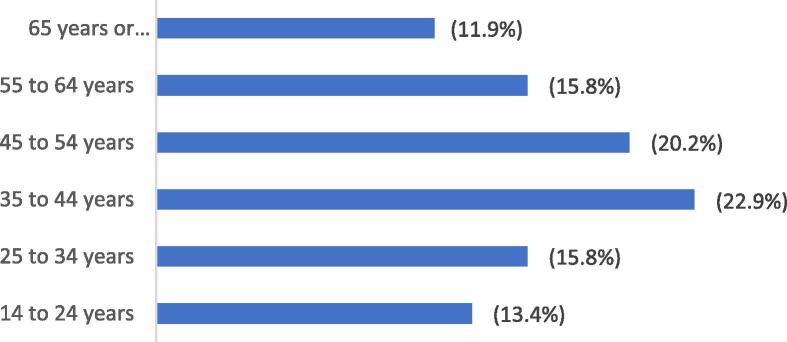
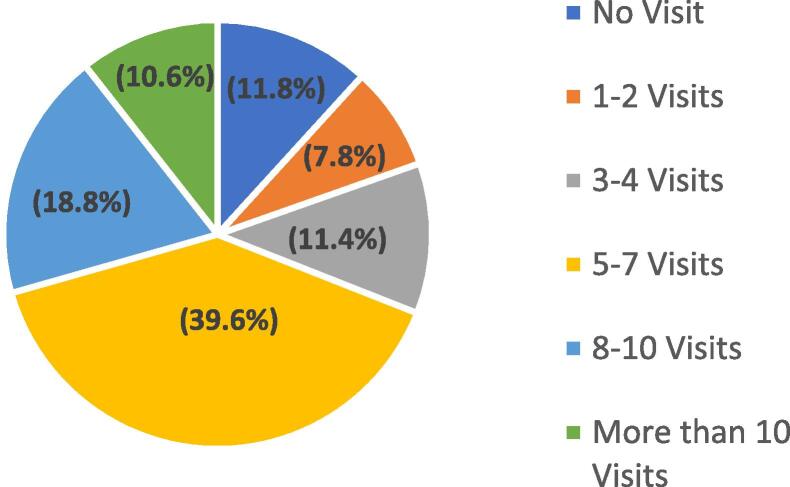
The data for this study was collected from 255 asthmatic patients. Among them 124 (48.70%) are male and 131 (51.30%) are female. Fig. 1 represents that highest visiting frequency i.e. 22.90% was noted in age group of 35 to 44 years and least visiting frequency i.e. 11.90% was noted in age group of 65 years and above, while Fig. 2 presented that in last twelve months, how many asthmatic patients visited how frequently to physicians. It is clear from the Fig. 2 that maximum number of patients i.e. 39.60% visited 5–7 times per year, 11.80% not visited at all in last twelve months, while highest frequency of visits i.e. 8–10 was observed in 18.80% patients.
Fig. 1.
Age groups distribution.
Fig. 2.
Frequency of Physician Visit in last 12 months.
Table 1 represents the association of severity of asthma, functional limitations due to asthmatic attacks, acute attacks, side effects due to treatments, combination treatments and satisfaction of patients with frequency of physician visits in the past 12 months.
Table 1.
Clinical and treatment parameters of asthmatic patients with number of physician visit in past year.
| No Visit | 1–2 Visits | 3–4 Visits | 5–7 Visits | 8–10 Visits | More than 10 Visits | p-Value | |
|---|---|---|---|---|---|---|---|
| Severity (n = 255) | (n = 30) | (n = 20) | (n = 29) | (n = 101) | (n = 48) | (n = 27) | 0.0001 |
| Intermittent (n = 106) | 20(66.7%) | 10(50%) | 20(69%) | 37(36.6%) | 15(31.3%) | 4(14.8%) | |
| Mild(n = 88) | 8(26.7%) | 8(40%) | 6(20.7%) | 44(43.6%) | 20(41,7%) | 2(7.4%) | |
| Moderate(n = 50) | 2(6.7%) | 2(10%) | 3(10.3%) | 20(19.8%) | 11(22.9%) | 12(44.4%) | |
| Severe(n = 11) | 0 | 0 | 0 | 0 | 2(4.2%) | 9(33.3%) | |
| Limitation(n = 251) | (n = 29) | (n = 20) | (n = 28) | (n = 100) | (n = 48) | (n = 26) | 0.0001 |
| No limitation(n = 138) | 22(75.9%) | 9(45%) | 19(67.9%) | 64(64%) | 20(41.7%) | 4(15.4%) | |
| Some limitation(n = 86) | 7(24.1%) | 10(50%) | 8(28.6%) | 31(31%) | 22(45.8%) | 8(30.8%) | |
| Extremely limited(n = 27) | 0 | 1(5%) | 1(3.6%) | 5(5%) | 6(12.5%) | 14(53.8%) | |
| Acute asthma(n = 254) | (n = 30) | (n = 20) | (n = 28) | (n = 101) | (n = 48) | (n = 27) | 0.021 |
| Allopathic(n = 224) | 25(83.3%) | 14(70%) | 21(75%) | 95(94.1%) | 46(95.8%) | 23(85.2%) | |
| Homeopathic(n = 16) | 2(6.7%) | 4(20%) | 3(10.7%) | 4(4%) | 1(2.1%) | 2(7.4%) | |
| Herbal(n = 14) | 3(10%) | 2(10%) | 4(14.3%) | 2(2%) | 1(2.1%) | 2(7.4%) | |
| Treatment side effects (n = 252) | (n = 28) | (n = 20) | (n = 29) | (n = 100) | (n = 48) | (n = 27) | 0.003 |
| No(n = 183) | 24(85.7%) | 16(80%) | 23(79.3%) | 79(79%) | 27(56.3%) | 14(51.9%) | |
| Yes(n = 69) | 4(14.3%) | 4(20%) | 6(20.7%) | 21(21%) | 21(43.8%) | 13(48.1%) | |
| Combination Treatments(n = 253) | (n = 29) | (n = 20) | (n = 28) | (n = 98) | (n = 48) | (n = 26) | 0.01 |
| No(n = 162) | 20(69%) | 14(70%) | 20(71.4%) | 73(74.5%) | 23(47.9%) | 12(46.2%) | |
| Yes(n = 87) | 9(31%) | 6(30%) | 8(28.6%) | 25(25.5%) | 25(52.1%) | 14(53.8%) | |
| Satisfaction level(n = 250) | (n = 28) | (n = 20) | (n = 29) | (n = 100) | (n = 47) | (n = 26) | 0.053 |
| Not Satisfied at all(n = 1) | 1(3.6%) | 0 | 0 | 0 | 0 | 0 | |
| Not Satisfied(n = 14) | 1(3.6%) | 0 | 4(13.8%) | 3(3%) | 5(10.6%) | 1(3.8%) | |
| Neutral(n = 47) | 6(21.4%) | 2(10%) | 4(13.8%) | 12(12%) | 14(29.8%) | 9(34.6%) | |
| Satisfied(n = 160) | 16(57.1%) | 15(75%) | 18(62.1%) | 73(73%) | 24(51.1%) | 14(53.8%) | |
| Extremely Satisfied(n = 28) | 4(14.3%) | 3(15%) | 3(10.3%) | 12(12%) | 4(8.5%) | 2(7.7%) |
Significance at p < 0.05
Table 2 presents the association of age of patient, education level, marital status, income group and pet availability at home to the number of physician visits during past 12 months. All these factors are significantly associated with number of physician visits during past 12 months.
Table 2.
Demographics of asthmatic patients with number of physician visit in past year.
| No Visit | 1–2 Visits | 3–4 Visits | 5–7 Visits | 8–10 Visits | More than 10 Visits | p-Value | |
|---|---|---|---|---|---|---|---|
| Age(n = 253) | (n = 30) | (n = 20) | (n = 28) | (n = 101) | (n = 48) | (n = 26) | 0.004 |
| 14 to 24 years(n = 34) | 11(36.7%) | 2(10%) | 4(13.8%) | 7(7%) | 7(14.9%) | 3(11.1%) | |
| 25 to 34 years(n = 40) | 5(16.7%) | 2(10%) | 11(37.9%) | 12(12%) | 6(12.8%) | 4(14.8%) | |
| 35 to 44 years(n = 58) | 8(26.7%) | 3(15%) | 7(24.1%) | 30(30%) | 5(10.6%) | 5(18.5%) | |
| 45 to 54 years(n = 51) | 1(3.3%) | 6(30%) | 4(13.8%) | 21(21%) | 12(25.5%) | 7(25.9%) | |
| 55 to 64 years(n = 40) | 1(3.3%) | 4(20%) | 2(6.9%) | 19(19%) | 10(21.3%) | 4(14.8%) | |
| 65 years plus (n = 30) | 4(13.3%) | 3(15%) | 1(3.4%) | 11(11%) | 7(14.9%) | 4(14.8%) | |
| Education(n = 253) | (n = 30) | (n = 20) | (n = 28) | (n = 101) | (n = 48) | (n = 26) | 0.0001 |
| No formal education(n = 57) | 1(3.3%) | 6(30%) | 0 | 25(24.8%) | 12(25%) | 13(50%) | |
| Primary(n = 38) | 4(13.3%) | 1(5%) | 3(10.7%) | 17(16.8%) | 9(18.8%) | 4(15.4%) | |
| Secondary(n = 36) | 4(13.3%) | 2(10%) | 3(10.7%) | 18(17.8%) | 6(12.5%) | 3(11.5%) | |
| Intermediate(n = 35) | 3(10%) | 4(20%) | 5(17.9%) | 15(14.9%) | 7(14.6%) | 1(3.8%) | |
| Graduate(n = 56) | 12(40%) | 5(25%) | 11(39.3%) | 19(18.8%) | 7(14.6%) | 2(7.7%) | |
| Masters/Professionals (n = 31) | 6(20%) | 2(10%) | 6(21.4%) | 7(6.9%) | 7(14.6%) | 3(11.5%) | |
| Marital Status(n = 255) | (n = 30) | (n = 20) | (n = 29) | (n = 101) | (n = 48) | (n = 27) | 0.0001 |
| Single(n = 53) | 15(50%) | 1(5%) | 13(44.8%) | 9(8.9%) | 11(22.9%) | 4(14.8%) | |
| Married(n = 186) | 12(40%) | 16(80%) | 15(51.7%) | 89(88.1%) | 33(68.8%) | 21(77.8%) | |
| Widow/Widower(n = 4) | 1(3.3%) | 3(15%) | 1(3.4%) | 3(3%) | 4(8.3%) | 2(7.4%) | |
| Divorced(n = 2) | 2(6.7%) | 0 | 0 | 0 | 0 | 0 | |
| Income (n = 244) | (n = 28) | (n = 20) | (n = 28) | (n = 98) | (n = 45) | (n = 25) | 0.0001 |
| Up to 10,000(n = 55) | 2(7.1%) | 4(20%) | 2(7.1%) | 31(31.6%) | 10(22.2%) | 6(24%) | |
| 10,001–25,000(n = 84) | 5(17.9%) | 6(30%) | 7(25%) | 39(39.8%) | 19(42.2%) | 8(32%) | |
| 25,001–50,000(n = 44) | 3(10.7%) | 3(15%) | 10(35.7%) | 14(14.3%) | 7(15.6%) | 7(28%) | |
| 50,001–75,000(n = 19) | 4(14.3%) | 3(15%) | 4(14.3%) | 6(6.1%) | 0 | 2(8%) | |
| 75,001–100,000(n = 18) | 5(17.9%) | 1(5%) | 3(10.7%) | 2(2%) | 5(11.1%) | 2(8%) | |
| Above 100 k(n = 24) | 9(32.1%) | 3(15%) | 2(7.1%) | 6(6.1%) | 4(8.9%) | 0 | |
| Pets(n = 254) | (n = 30) | (n = 19) | (n = 29) | (n = 101) | (n = 48) | (n = 27) | 0.007 |
| No (n = 140) | 20(66.7%) | 12(63.2%) | 17(58.6%) | 41(40.6%) | 30(62.5%) | 20(74.1%) | |
| Yes(n = 114) | 10(33.3%) | 7(36.8%) | 12(41.4%) | 60(59.4%) | 18(37.5%) | 7(25.9%) |
Significance at p < 0.05
4. Discussion
The current study showed a trend of frequent physician visits, most of the patients visited 5–7 times during the past year which shows a positive response as regular asthma monitoring visits every 1–6 months depending on severity of asthma are suggested by the National Asthma Education and Prevention Program (NAEPP) guidelines (2007). Highest visiting frequency i.e. 22.90% was noted in age group of 35 to 44 years and least visiting frequency i.e. 11.90% was noted in age group of 65 years and above, it may be due to the reason that 35–44 years age bracket is mainly working group of individuals that is why they are concern about their health and visit very frequently, on the other hand old age group has the multiple complications and due to poor cognitive functions it might be difficult for them to recognize the severity of their own diseases as well they are dependent on their care-giver to visit clinicians. It is clear from the results of study (Fig. 2) that maximum number of patients i.e. 39.60% visited 5–7 times per year (35–44 years), 11.80% (greater than65 years) not visited at all in last twelve months, while highest frequency of visits i.e. 8–10 was observed in 18.80% (14–24 years) patients.
Most of the patients in the current study used allopathic treatments for asthma and did not appreciate combination treatments for asthma, however, combination treatment is significantly associated with frequency of visits to clinician (p = 0.01). Altogether, patients visiting physician frequently found to be satisfied with their treatment as literature indicated that physician’s communication with patient results in enhanced treatment satisfaction (Dugdale et al., 1999). However, current study reveals that patient satisfaction is non-significantly associated with number of visits (p = 0.053). These finding and results by different studies recommend that asthma follow-up consultations may have a positive impact on adherence to asthma medication treatment and may result in better asthma control (Axelsson et al., 2015).
Studies suggested that follow-up visits help physicians to regularly evaluate asthma risk and alter treatment if required (Nelson et al., 2014). These visits may also help in solving the issues of poor inhaler technique and failure to proper asthma control. These visits can be used to educate the patients and increase awareness about asthma (Yawn, 2011). Various studies have explored the association of physician and patient individual factors in search of better clinical outcome. In addition to that, significant role of physician and importance of shared decision making has been determined, it was suggested that follow up physician visits leads to a better understanding of patients' preferences and expectations and help in monitoring the symptoms and effects of medications (Dugdale et al., 1999). Study conducted in 2002 presented that asthma clinic visits constantly increased from 1978 to 1990, while remained stable after 1990. During this period, controller drugs use was increased as compared to relievers and was suggested as indirect improved asthma control. However, authors listed that decline in asthma visits might be due to patients going to internists and pediatricians more rather than to allergist for asthma (Stafford et al., 2003). Most of the scientific studies conducted focused on patients visiting to emergency room and hospitalization (Suruki et al., 2017, Bilal et al., 2016). While our study focused on patients visiting for asthma follow-up visit and found that most of the patients had intermittent and mild asthma and did not exhibited any significant (p = 0.003) side effects of treatment or faced too much limitation due to asthma. The previous literature has proved that patients also used complementary and alternative treatment method for asthma (Thomson et al., 2012). However, evidence-based data for efficacy and safety of alternative treatments is still lacking so before starting any alternative methods, its better if patients discuss with their primary physician to avoid any harmful effects (Eisenberg, 1997).
Limited research is available on association of demographic factors of patient with physician visits. Most of the studies concentrated on physician role and on factors that patients considered for choosing physicians (Victoor et al., 2012, Park et al., 2018). Current study data proposed that age of the patients was significantly (p = 0.004) associated with frequency of physician visits and most common age groups were 35–44 years and 44–54 years. Centers for Disease Control (CDC) mentioned the similar age group for frequent asthma visits (Control). Large number of patients visited physicians for asthma had no formal education while the other significant (p = 0.0001) groups were educated till graduate level. Past literature emphases on importance of the of asthma education by physicians or staff during primary care visits (Zeng et al., 2018). The current study trend matches with the result of study suggesting that patients with spouse and kids visit more significantly (p = 0.0001) frequent to physicians (Schafer, 2013). Similarly patients having pets at home tend to visit physician significantly (p = 0.007) more as pets are known to trigger asthma (Simpson and Custovic, 2005). Asthma cost differs in different countries depending upon factors including health system and quality of life (Srivastava, 2017). However, according to current study, most of the patients visiting physician belong to the low-income group. The reason might be that most of patients’ interviews in this study were conducted at hospital and clinics that were free or had minimal consultation fees.
5. Conclusion
The study concluded that most of the asthmatic patients had number of follow up physician visits during the last year. In addition, most of them were satisfied with their treatment. The study discovered that many of patient specific factors (demographic and clinical) have significant association with number of follow up physician visits. These factors should be explored more thoroughly in order to improve asthma control and prognosis. This type of study might help in long-term asthma management by identifying different patients’ factors that need more attention to have better asthma control and make the treatment better and customized according to patient’s needs.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
Not applicable
Footnotes
Peer review under responsibility of King Saud University.
References
- Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma-Summary Report 7. J Allergy Clin Immunol, 120, S94-138. [DOI] [PubMed]
- Aparasu R.R. First ed. Pharmaceutical Press; United Kingdom: 2016. Sampling methods; Chapter 107. Research methods for pharmaceutical practice and policy. [Google Scholar]
- Bastemeijer C.M., Voogt L., van Ewijk J.P., Hazelzet J.A. What do patient values and preferences mean? A taxonomy based on a systematic review of qualitative papers. Patient Education and Counseling. 2017;100:871–881. doi: 10.1016/j.pec.2016.12.019. [DOI] [PubMed] [Google Scholar]
- Bilal M., Haseeb A., Khan M.H., Saad M., Devi S., Arshad M.H., Alam A., Wagley A.M., Javed K.M. Factors associated with patient visits to the emergency department for asthma therapy in Pakistan. Asia Pac Fam Med. 2016;15:1. doi: 10.1186/s12930-016-0026-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Control, C. F. D. Asthma-related physician office visits 2010–2016. https://www.cdc.gov/asthma/asthma_stats/asthma-related-physician-visits_2010-2016.html [Online]. [Accessed 10.9.2020].
- Dharmage S.C., Perret J.L., Custovic A. Epidemiology of Asthma in Children and Adults. Frontiers in pediatrics. 2019;7:246. doi: 10.3389/fped.2019.00246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dugdale D.C., Epstein R., Pantilat S.Z. Time and the patient-physician relationship. Journal of general internal medicine. 1999;14(Suppl 1):S34–S40. doi: 10.1046/j.1525-1497.1999.00263.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg D.M. Advising Patients Who Seek Alternative Medical Therapies. Annals of Internal Medicine. 1997;127:61–69. doi: 10.7326/0003-4819-127-1-199707010-00010. [DOI] [PubMed] [Google Scholar]
- Kritikos V., Price D., Papi A., Infantino A., Ställberg B., Ryan D., Lavorini F., Chrystyn H., Haughney J., Lisspers K., Gruffydd-Jones K. A multinational observational study identifying primary care patients at risk of overestimation of asthma control. npj Primary Care Respiratory Medicine. 2019;29:43. doi: 10.1038/s41533-019-0156-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Y.K., Low W.Y., Ng C.J. Exploring patient values in medical decision making: a qualitative study. PLoS One. 2013;8 doi: 10.1371/journal.pone.0080051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson K.A., Garbutt J.M., Wallendorf M.J., Trinkaus K.M., Strunk R.C. Primary care visits for asthma monitoring over time and association with acute asthma visits for urban Medicaid-insured children. The Journal of asthma : official journal of the Association for the Care of Asthma. 2014;51:907–912. doi: 10.3109/02770903.2014.927483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nunes C., Pereira A.M., Morais-Almeida M. Asthma costs and social impact. Asthma Research and Practice. 2017;3:1. doi: 10.1186/s40733-016-0029-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park H.J., Byun M.K., Kim H.J., Ahn C.M., Rhee C.K., Kim K., Kim B.Y., Bae H.W., Yoo K.H. Regular follow-up visits reduce the risk for asthma exacerbation requiring admission in Korean adults with asthma. Allergy Asthma Clin Immunol. 2018;14:29. doi: 10.1186/s13223-018-0250-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Say R.E., Thomson R. The importance of patient preferences in treatment decisions–challenges for doctors. Bmj. 2003;327:542–545. doi: 10.1136/bmj.327.7414.542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer M.H. Discussion networks, physician visits, and non-conventional medicine: probing the relational correlates of health care utilization. Soc Sci Med. 2013;87:176–184. doi: 10.1016/j.socscimed.2013.03.031. [DOI] [PubMed] [Google Scholar]
- Simpson A., Custovic A. Pets and the development of allergic sensitization. Curr Allergy Asthma Rep. 2005;5:212–220. doi: 10.1007/s11882-005-0040-x. [DOI] [PubMed] [Google Scholar]
- Society, B. T. BTS/SIGN British Guidelines on the Management of Asthma (2019).https://www.brit-thoracic.org.uk/quality-improvement/guidelines/asthma/ [Online]. [Accessed 10.9.2020].
- Srivastava A. Itolizumab in Psoriasis. Indian journal of dermatology. 2017;62:418–421. doi: 10.4103/ijd.IJD_467_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stafford R.S., Ma J., Finkelstein S.N., Haver K., Cockburn I. National trends in asthma visits and asthma pharmacotherapy, 1978–2002. Journal of Allergy and Clinical Immunology. 2003;111:729–735. doi: 10.1067/mai.2003.177. [DOI] [PubMed] [Google Scholar]
- Suruki R.Y., Daugherty J.B., Boudiaf N., Albers F.C. The frequency of asthma exacerbations and healthcare utilization in patients with asthma from the UK and USA. BMC Pulm Med. 2017;17:74. doi: 10.1186/s12890-017-0409-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomson P., Jones J., Evans J.M., Leslie S.L. Factors influencing the use of complementary and alternative medicine and whether patients inform their primary care physician. Complement Ther Med. 2012;20:45–53. doi: 10.1016/j.ctim.2011.10.001. [DOI] [PubMed] [Google Scholar]
- van der Molen T., Fletcher M., Price D. Identifying Patient Attitudinal Clusters Associated with Asthma Control: The European REALISE Survey. J Allergy Clin Immunol Pract. 2018;6:962–971. doi: 10.1016/j.jaip.2017.10.007. [DOI] [PubMed] [Google Scholar]
- Victoor A., Delnoij D.M., Friele R.D., Rademakers J.J. Determinants of patient choice of healthcare providers: a scoping review. BMC Health Serv Res. 2012;12:272. doi: 10.1186/1472-6963-12-272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yawn B.P. The role of the primary care physician in helping adolescent and adult patients improve asthma control. Mayo Clinic proceedings. 2011;86:894–902. doi: 10.4065/mcp.2011.0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng Y.-Q., Au D.H., Cai S., Carey E., Jiang F., Chen Y., Liu Z.-J., Chen P. Effect of a Patient Education Intervention on Asthma Control and Patient-Doctor Relationship. Chinese medical journal. 2018;131:1110–1112. doi: 10.4103/0366-6999.230736. [DOI] [PMC free article] [PubMed] [Google Scholar]