Abstract
Background
Traditional bonesetters (TBS) are still highly patronized by people with fractures in Africa. We sought to investigate factors affecting the utilization of TBS services in the Northern Region of Ghana.
Methods
A mixed-methods study that combined both qualitative and quantitative approaches was conducted among 64 TBS clients in the Northern Region of Ghana. Participants were purposively selected and should have utilized the services of TBSs at the time of the study. In addition, three focus group discussions (FGDs) were conducted to complement the quantitative results. Quantitative analysis was performed by calculating means and proportions. For the qualitative data, content analysis was done manually based on emerging themes in line with the study objectives.
Results
Sixty-four (64) clients were recruited. Twenty-four (37.5%) were female. The modal age group was 19–39 years. The educational status of the clients was dominated by primary/junior secondary education (39.1%), but included the full spectrum from no formal education / illiterate (26.6%) to tertiary (12.5%). Cheaper fees (26.3%), cultural beliefs (17.9%), and quick service (15.9%) were the main reason of patronizing TBSs. Twenty-two (34.3%) would have preferred orthodox care and the reasons cited included availability of X-rays (27.3%) and pain management (25.3%). These themes were reiterated by FGDs with an additional 30 clients. Additional themes identified by the FGDs included a belief that TBSs address both physical and spiritual aspects of the injury and the major role that families (not the injured person alone) make in deciding on type of treatment. Clients were supportive of orthodox providers linking with TBSs for activities such as training to improve pain control.
Conclusion
TBSs have patronage from the full spectrum of society. The decision to opt for TBS treatment was influenced by cheaper fees, cultural belief, and quick service. TBS clients wanted greater linkages between TBSs and orthodox providers.
Keywords: Traditional bonesetters (TBS), Health service utilization, Fracture, Orthopaedics
African relevance
-
•
Many patients with fractures in Africa seek care from traditional bonesetters (TBS) rather than modern health care providers.
-
•
Oftentimes, complications such as infections or gangrene ensue.
-
•
Encouraging fracture patients to seek modern care earlier is important to decrease complications that arise from TBS care.
-
•
Efforts to accomplish the above should be based on an understanding of why people with fractures patronize TBSs.
-
•
The current study provides insights on factors affecting fracture patients' decision to utilize TBSs.
Introduction
Extremity injuries such as fractures are a major cause of disability globally, especially in low- and middle-income countries. Much of the disability caused by fractures could be averted by improvements in emergency care, orthopaedic care, and rehabilitation [1,2]. In many African countries, fracture care is provided not only by formal / orthodox medical practitioners, but also by traditional bonesetters (TBSs) [[3], [4], [5], [6]].
In Ghana, estimates of the proportion of people with fractures who utilize TBSs range from 52% to 78% [7,8]. Orthodox health care providers often need to treat complications ensuing from TBS care [[9], [10], [11], [12], [13], [14]]. The practice of TBS is therefore an issue of public health importance. There have been several approaches advocated to address problems arising from TBS care. These include discouraging people with fractures from utilizing TBS and instead using orthodox care [5,9,10,12,13]. Approaches suggested also include providing training for TBSs so they know their limitations and can recognize cases that need referral to orthodox care [6,15].
Any of these approaches need to be based on an understanding of why people with fractures patronize TBSs. Several researchers have addressed this issue from different perspectives. Several studies in Nigeria interviewed either community members or patients who had first gone to TBSs, but who then came to a hospital [4,[16], [17], [18], [19]]. One study in Nigeria specifically sought out TBS clients and interviewed 88 with a quantitative survey and 4 with an indepth interview [20]. Similarly in Ghana, one study evaluated a mixture of patients at a hospital, some of whom had not utilized TBSs and some of whom had [7]. A second study interviewed a mixture of hospitalized patients and TBS clients with a quantitative survey [8]. A third study interviewed 16 TBS clients in southern Ghana on their perspectives on TBS care [3].
We sought to build on these prior studies in several ways. We sought to identify a large number of people who had sought TBS care, regardless of whether or not they had also used orthodox care. Such people would provide insights that could be different from people identified through hospital-based studies. We also used a mixed-methods approach, providing both quantitative and qualitative data, as such a mixed approach is likely to provide more in-depth insights than either alone.
Methods
This study was set in the Northern Region of Ghana, one of the least economically developed areas of the country. A cross-sectional, mixed-methods (qualitative and quantitative) study was conducted among TBS clients. TBS clients were purposively selected. First, TBSs throughout the Northern Region were identified through a list from the Northern branch of “Ghana Federation of Traditional Medicine” and subsequent snowball sampling of other TBSs. Snowball sampling is a method often used when there are limited or no lists of people whom the researcher is seeking to interview. Once a few suitable people are identified and interviewed, they are asked about whether they know other potential respondents. Hence, the number of potential respondents grows by such contacts as the study proceeds. TBSs who agreed allowed the researchers to contact clients, including those admitted or undergoing active outpatient treatment, or being seen in follow-up. Clients were approached to be involved in either in-person interviews or focus group discussions (FGDs). Written informed consent was obtained from those who agreed to participate, or from their parents if they were under 18 years.
Sixty-four TBS clients participated in one-on-one interviews. A semi-structured interviewer-administered questionnaire was used to obtain quantitative information on demographic characteristics, reasons for TBS patronage, and perceptions of advantages of TBS vs. orthodox care. The principal investigator (PI) or two research officers conducted interviews. Interviews were done mainly in the local languages through interpreters and took around 30 min.
A separate group of TBS clients was involved in FGDs. Three FGDs were conducted to complement the quantitative results. The FGDs consisted of two male groups and one female group, in keeping with local cultural norms. Each group had 10 participants and lasted around 90 min. Standard rigorous FGD methods were utilized [21]. The PI assisted by an assistant who understood the local language moderated the discussion. The FGD audio recordings were primarily in the main local language (Dagbani). Bilingual research assistants transcribed the audio recordings into English, which the PI used to extract the themes from the FGDs. Content analysis of the data was done manually based on emerging themes and sub-themes in line with the study objectives.
Data were gathered during July–October 2018, with the two components of the study performed in parallel. The TBS clients in the study were located in 16 towns and villages that were geographically dispersed across the Northern Region. Quantitative analysis was done using Stata 14.0. Frequencies and percentages were calculated. The results of the two components of the study were triangulated in the development of the study conclusions. The reliability and validity of both components of the study was ensured by several measures including: the PI checked all forms for completeness and accuracy on a daily basis and was present for all FGDs and most individual interviews; FGDs were audio-recorded and transcribed and compared with written notes.
The Committee for Human Research and Publication Ethics of the Kwame Nkrumah University of Science and Technology approved this study.
Results
Socio-demographic characteristics of traditional bonesetter's clients
Sixty-four TBS clients were recruited into the individual interview component of the study. All 64 clients who were approached agreed to participate. The clients were primarily male and young (Table 1). Majority were Muslims and half were Dagomba. Educational status was widely distributed: no formal education (26.6%), primary/junior secondary education (39.1%), secondary education (17.2%), and tertiary / post-secondary education (17.2%), with a wide variety of professions.
Table 1.
Socio-demographic characteristics of bonesetters clients.
| Variable | Responses | Frequency | Percentage (%) |
|---|---|---|---|
| Gender | Male | 40 | 62.5 |
| Female | 24 | 37.5 | |
| Ethnicity | Dagomba | 32 | 50.0 |
| Gonja | 3 | 4.7 | |
| Dagaati | 1 | 1.6 | |
| Mamprusi | 4 | 6.3 | |
| Others | 24 | 37.5 | |
| Educational qualification | No School (Formal Education) | 17 | 26.6 |
| Primary/Junior Secondary School | 25 | 39.1 | |
| Senior Secondary School | 11 | 17.2 | |
| Tertiary | 8 | 12.5 | |
| Post-Secondary | 3 | 4.7 | |
| Age (years) | 0–18 (children and adolescents) | 12 | 18.8 |
| 19–39 (young adults) | 32 | 50.0 | |
| 40–59 (older adults) | 17 | 26.6 | |
| 60 and above (elderly) | 3 | 4.7 | |
| Religion | Christianity | 20 | 31.3 |
| Islam | 42 | 65.6 | |
| Traditional Believer | 2 | 3.1 | |
| Occupation | Civil Servant | 12 | 18.8 |
| Trader | 19 | 29.7 | |
| Farmer | 13 | 20.3 | |
| Unemployment | 16 | 25.0 | |
| Others | 4 | 6.3 |
Reasons for utilizing TBS vs. orthodox treatment
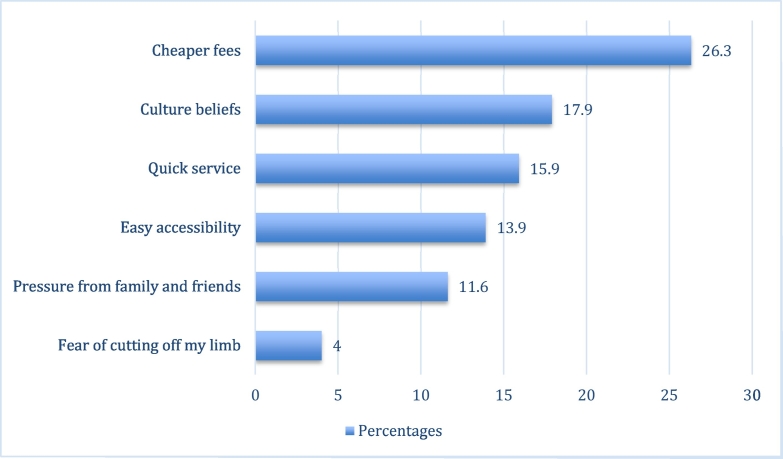
Of the 64 clients interviewed, most (65.7%) preferred TBSs for treatment of their fracture. The main reasons included: cheaper fees, cultural beliefs, quick service, among others (Fig. 1).
Fig. 1.
Reasons for utilizing traditional bonesetter treatment.
Note: Multiple entries allowed. Not all participants listed a reason.
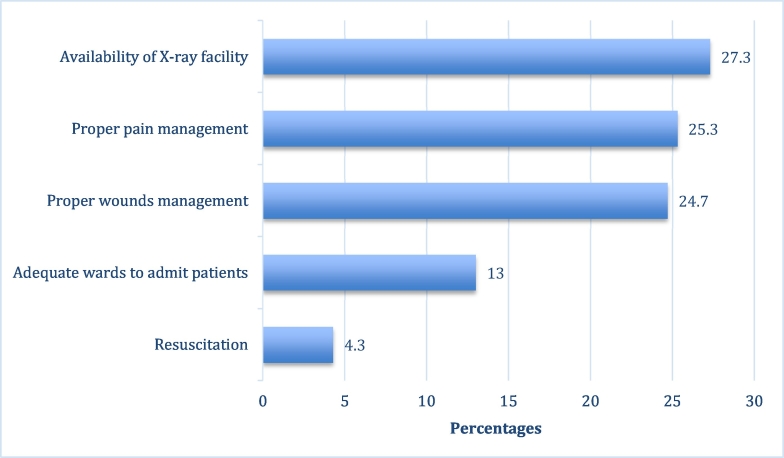
Only 22 (34.3%) of the clients interviewed would have preferred to utilize orthodox care. The main reasons cited included: the availability of X-ray facilities, proper pain management, proper wound management, among others (Fig. 2).
Fig. 2.
Reasons for utilizing orthodox treatment.
Note: Multiple entries allowed. Not all participants listed a reason.
Perceptions of TBS vs. orthodox treatment
The TBS clients were given several statements about their perceptions to agree or disagree with (Table 2). Almost all clients (90.6%) agreed that some fractures are caused by supernatural powers, and most (65.6%) recognized that the perceived strength of TBS lies in the confidence their communities have had in them for years. Findings from the study also show that many of the clients (70.3%) opined that TBS are more skillful than orthodox practitioners. Three in five clients (62.5%) agreed that TBS services were benevolent, economical and effective, and more than three in five (75.0%) agreed that orthodox services are more costly than TBS care. Over half of the clients (59.4%) believed that orthodox services are usually associated with surgery and amputation. However, a large proportion (78.1%) agreed that orthodox medicine is more effective in pain and wound management. Forty-two (65.6%) clients recognized the usefulness of orthodox service when the fracture is complicated.
Table 2.
Perceptions of traditional bone setters (TBS) versus orthodox services.
| Perceptions statements | Agree N (%) | Disagree N (%) | Undecided N (%) |
|---|---|---|---|
| Beliefs that some of the bone injuries are caused by supernatural powers | 58 (90.6%) | 6 (9.4%) | 0 (0%) |
| Perceive belief that TBS are more skillful than orthodox practitioners | 45 (70.3%) | 15 (23.4%) | 4 (6.3%) |
| Consider TBS services as more benevolent, economical and effective than orthodox services | 40 (62.5%) | 17 (26.6%) | 7 (10.9%) |
| Community have more confidence in TBS treatment than orthodox services | 42 (65.6%) | 22 (34.4%) | 0 (0%) |
| Orthodox care is more effective in pain and wound management | 50 (78.1%) | 14 (21.9%) | 0 (0%) |
| Orthodox care is associated with surgery and amputation | 38 (59.4%) | 20 (31.3%) | 6 (9.4%) |
| Orthodox services are associated with high cost of services compared to TBS | 48 (75.0%) | 12 (18.8%) | 4 (6.3%) |
| Orthodox care is only useful when it's a complicated fracture | 42 (65.6%) | 20 (31.3%) | 2 (3.1%) |
Results of focus group discussions
Reasons for utilizing TBS over orthodox services
Participants in the FGDs were of the same general socio-demographic and socio-economic breakdown as for the quantitative interviews, but were all adults. Multiple themes emerged from the FGDs as to why clients utilized TBSs over orthodox services. These included quick service, fear of amputation, and less cost. Another theme was that TBS are special, blessed, and talented people who have been set aside by ‘god’ and if they treat you, you get healed very fast. Participants also considered TBSs as benevolent because clients are often treated and fed for free.
“When your leg breaks and the TBS treats it, it's better. Sometimes your leg can break to the extent that they put metals in it when you take it to the hospital, but TBS just treats it because it is spiritual. Also, someone will go for hospital treatment, comes back and you yourself will realize that, the person has not been treated well, and needs to go to TBS again to become fit.” (Male FGD2)
“I fear seeking treatment from the hospital because I knew I will go through bureaucracy; later doctors will apply POP and few days later they will tell me that my limb is dead so I need amputation. It is very sad but that is what they do for patient with bone injury.” (Male FGD1).
There was a consensus that TBSs spend enough time with patients, unlike doctors who do not have time for the patients, and sometimes ignore them. Participants also believed that TBS treatment heals faster and better than hospital treatment because they give much attention and apply locally-made medicines. There was more faith in such treatments and a corresponding fear of some of the treatments in the hospital, such as metal implants.
“My friend has an accident and fracture the thigh bone. He went to hospital and was operated and metal put inside the thigh. After the healing of the fracture he was always complaining about the implant feeling cold during cold/rainy weather and have to go back and request for removal of metals”. (Female FGD).
The 3 FGD participants also noted the importance of the training that the TBS's receive and recognized that the profession of TBS is an inheritance from their forefathers. They feel that TBS are special people and blessed with their abilities.
“Only specific families can do it, just like royals; if you are not from the royal family, can you become a chief? Even if others try, they cannot heal like those from the family, because it is physical and spiritual and the training start from infancy until the person is mature to be able to treat.” (Male FGD2).
Additional themes emphasized by the FGDs, that were not as apparent in the quantitative part of the study, included a belief that TBSs address both physical and spiritual aspects of the injury and the major role that families (not the injured person alone) make in deciding on treatment. Participants emphasized that persons with fractures have little role to play when it comes to deciding on the treatment choice. Relatives, family, and friends make the decision.
“If the patient proposes to go to the hospital, the parents or relatives will not allow because they think they will spend more money. If patient refuses traditional treatment and goes to the hospital, he will be responsible for the consequences…….If you refuse TBS treatment and they cut your leg off in the hospital, that is what you want and nobody will sympathize with you in the community.” (Male FGD1).
Perceived advantages of orthodox care over TBS
There was a consensus in the FGDs that there were some advantages of orthodox care over TBS care. These advantages include that the hospital has wards for admission, X-rays, and pain management. Many participants indicated that they would want orthodox doctors to help TBSs with pain management because TBS bone setting procedures can be very painful. They also want doctors to help TBSs manage open fractures and to train them to read X-rays. Although some of the fractures are from spiritual attacks, they want orthodox doctors to train TBSs on how to manage fracture complications.
Discussion
This study sought to understand factors affecting utilization of TBSs in Northern Ghana. We found that TBS clients came from the spectrum of society, including a wide range of educational backgrounds and professions. The decision to opt for TBS treatment was influenced by several factors, the most common of which were cheaper fees, cultural belief, quicker service, and the perception that TBSs treatment led to faster healing than orthodox care.
The current study adds to the literature in several ways. Many prior publications were on TBS practices [5,9,10,12,14,15,[22], [23], [24], [25]]. Several other researchers sought to understand why people with fractures patronize TBSs. These include studies that interviewed either community members or patients who had first gone to TBSs, but who then came to a hospital [4,7,[16], [17], [18], [19]]. One study in Nigeria interviewed 88 TBS clients (whether or not they had also sought orthodox care) with a quantitative survey and four with an in-depth interview [20]. Two prior studies in Ghana interviewed TBS clients outside of the hospital setting [3,8].
The current study builds on these prior studies in several ways. It provides viewpoints from a large number of people who had sought TBS care, regardless of whether or not they had also used orthodox care. It is one of the largest studies done of TBS clients outside of the hospital setting, with a total of 94, slightly more than Owumi's study with 92 [20] and considerably more than any of the other studies. It also uses a mixed-methods approach, providing both quantitative and qualitative data. It is also the only study thus far using FGDs. Below we place the findings into the context of the published literature.
The leading reason that TBS clients preferred TBS care in the current study was that it was lower in price than orthodox care, which underscores the issue of poverty. The importance of financial considerations in choosing TBS care is confirmed by other studies in southern Ghana and Nigeria [3,19,23].
The second leading reason for preference for TBS care was cultural belief. TBS clients believe that natural resources used during treatment such as herbs and animal parts have therapeutic principles and supernatural powers. Other authors have documented this finding [19,23]. Similarly, Garba noted that clients felt that TBSs communicate well with their patients and are able to explain fracture signs and symptoms to their patient's satisfaction, as they live in the same community as the patients and share the same cultural beliefs [10].
Other reasons for TBS preference included the feeling that TBSs are located in more readily-available locations and render quick service. Similar results have been found elsewhere in West Africa and globally [19,23,26]. These factors overlap with the high regard communities have for TBSs. In our FGDs, respondents emphasized that TBSs enjoy strong popularity and influence. They were of the opinion that TBSs are reassuring and also offer home treatment and spend more time with their clients. Two studies from Nigeria corroborate these findings [22,24]. Nwachukwu also indicated that many TBS clients are afraid of having metal put in their bodies and of ending up in traction if they seek orthodox care [22].
Prior studies indicated that pressure from friends and family to use TBS were reported by 25% to 75% of respondents [9,17,18]. The quantitative component of the current study found a smaller percent (11.6%) of participants patronizing TBSs because of pressure from family and friends. Nonetheless, the theme of the predominant role of the family in making the decision on where to go for care was emphasized in the FGDs.
Against the backdrop of reasons that people prefer TBS treatment are reasons why people do not like orthodox care. Several authors have reported TBS clients citing apathetic attitude of health workers and delays in care at hospitals due to bureaucracy [12,27]. Other authors have noted fear of amputation in orthodox care as a leading factor in injured people choosing TBSs [16,25]. In the current study, this was only an infrequent reason.
How do the above findings help us to improve care for people with fractures, and so decrease the disability associated with them, in Ghana and Africa more widely? Several strategies have been advanced as ways to decrease the complications associated with TBS care [5,6,9,10,12,13,15]. These include strategies to discourage people with fractures from seeking TBS care in favor of orthodox care [5,9,10,12,13]. Other strategies call for linking of TBSs to orthodox care through such as efforts as training TBSs to recognize their limitations and to refer more complicated cases earlier [6,15]. The results of the current study show that orthodox care could be made more appealing to injured people and their families by making it more user-friendly and by decreasing out-of-pocket costs. Decreasing out-of-pocket costs, especially payments needed before treatment is rendered, can be done through such means as better insurance schemes and is an issue for all types of surgery in low- and middle-income countries. However, these measures are long term and not easy to implement.
Other reasons that injured people prefer TBS care are more deeply ingrained and more difficult to change, such as cultural preferences, the high standing of the TBSs in their communities, and their wide distribution and ready availability. Hence, the results of this study support training TBSs to better recognize their limitations and to link them with orthodox care as a more realistic option. Many TBS clients in this study voiced support for such linkages.
Before drawing conclusions, the study limitations must be addressed. First, data were collected from people who chose TBS care, who might have attitudes that are different from people who chose orthodox care. Second, the need for interpreters may have led to loss of detail. Third, all of the data were gathered from self-report and there is no way to validate the information provided. Despite these limitations, the study offers the advantages of having mixed-methods data gathered on a sizeable sample of TBS clients, who were from multiple ethnic backgrounds and were widely distributed across the Northern Region.
Conclusion
TBSs have patronage from people across the spectrum of society. The decision to opt for TBS treatment was influenced by cheaper fees, cultural belief, and quick service. Other factors were easy accessibility, advice or pressure from family and friends, and fear of operation and amputation in the hospital. The provision of accessible and affordable orthopaedic and trauma services, as well as health education, will reduce TBS patronage. Efforts to link TBSs with the orthodox care system and to train them to recognize their limitations and to refer complicated cases earlier should also be pursued.
Author's contribution
Authors contributed as follows to the conception or design of the work; the acquisition, analysis, or interpretation of data for the work; and drafting the work or revising it critically for important intellectual content:TY contributed 60%; AE, AB, PD, CM contributed 10% each. All authors approved the version to be published and agreed to be accountable for all aspects of the work.
Dissemination of results
The research was based at the Tamale Teaching Hospital. Two of the researchers (including the first author) are orthopaedic surgeons there. Results of the research have been communicated to other medical and nursing staff through informal presentations at the hospital and to the AO Alliance Ghana chapter meeting. Results have also been informally shared with the Northern Branch of the Ghana Federation of Traditional Medicine.
Funding
This study was funded in part by a grant from the United States National Institutes of Health (D43 TW007267). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Declaration of competing interest
The authors declared no conflicts of interest.
Acknowledgements
Special thanks to leaders of Northern branch of Ghana Federation of Traditional Medicine for giving me opportunity to identifier and interview TBS and their clients.
References
- 1.March L.M., Hoy D., Smith E., Buchbinder R., Cross M., Brooks P.M. Global and country specific burden of musculoskeletal disorders: a report from the global burden of diseases musculoskeletal expert group. Arthritis Rheum. 2013;65(10):S34. doi: 10.1002/ART.38216. [DOI] [Google Scholar]
- 2.Mock C., Cherian M.N. The global burden of musculoskeletal injuries: challenges and solutions. Clin Orthop Relat Res. 2008;466(10):2306–2316. doi: 10.1007/s11999-008-0416-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Edusei A.K., Owusu-Ansah F.E., Dogbe J.A., Morgan J., Sarpong K. Perspectives in musculoskeletal injury management by traditional bone setters in Ashanti, Ghana. Afr J Disabil. 2015;4(1):97. doi: 10.4102/ajod.v4i1.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aderibigbe S.A., Agaja S.R., Bamidele J.O. Determinants of utilization of traditional bone setters in Ilorin, north central Nigeria. J Prev Med Hyg. 2013;54(1):35–40. [PMC free article] [PubMed] [Google Scholar]
- 5.Dada A.A., Yinusa W., Giwa S.O. Review of the practice of traditional bone setting in Nigeria. Afr Health Sci. 2011;11(2):262–265. [PMC free article] [PubMed] [Google Scholar]
- 6.Eshete M. The prevention of traditional bone setter’s gangrene. J Bone Joint Surg Br. 2005;87(1):102–103. [PubMed] [Google Scholar]
- 7.Aries M.J., Joosten H., Wegdam H.H., van der Geest S. Fracture treatment by bonesetters in central Ghana: patients explain their choices and experiences. Trop Med Int Health. 2007;12(4):564–574. doi: 10.1111/j.1365-3156.2007.01822.x. [DOI] [PubMed] [Google Scholar]
- 8.Kuubiere C., Abass A., Majeed S. Patients preference for traditional bonesetters in Northern Ghana. Religion. 2015;2:2–5. [Google Scholar]
- 9.Dada A., Giwa S.O., Yinusa W., Ugbeye M., Gbadegesin S. Complications of treatment of musculoskeletal injuries by bone setters. West Afr J Med. 2009;28(1):43–47. doi: 10.4314/wajm.v28i1.48426. [DOI] [PubMed] [Google Scholar]
- 10.Garba E.S., Deshi P.J. Traditional bone setting: a risk factor in limb amputation. East Afr Med J. 1998;75(9):553–555. [PubMed] [Google Scholar]
- 11.OlaOlorun D.A., Oladiran I.O., Adeniran A. Complications of fracture treatment by traditional bonesetters in southwest Nigeria. Fam Pract. 2001;18(6):635–637. doi: 10.1093/fampra/18.6.635. [DOI] [PubMed] [Google Scholar]
- 12.Omololu B., Ogunlade S.O., Alonge T.O. The complications seen from the treatment by traditional bonesetters. West Afr J Med. 2002;21(4):335–337. doi: 10.4314/wajm.v21i4.28014. [DOI] [PubMed] [Google Scholar]
- 13.Onuminya J.E., Onabowale B.O., Obekpa P.O., Ihezue C.H. Traditional bone setter’s gangrene. Int Orthop. 1999;23(2):111–112. doi: 10.1007/s002640050320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Onyemaechi N., Onwuasoigwe O., Nwankwo O.E. Complications of musculoskeletal injuries treated by traditional bonesetters in a developing country. IJAR. 2014;4(3):313–316. doi: 10.15373/2249555X/MAR2014/93. [DOI] [Google Scholar]
- 15.Omololu A.B., Ogunlade S.O., Gopaldasani V.K. The practice of traditional bonesetting: training algorithm. Clin Orthop Relat Res. 2008;466(10):2392–2398. doi: 10.1007/s11999-008-0371-8. (doi:10.1007%2Fs11999-008-0371-8) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ogunlusi J., Okem I., Oginni L. Why patients patronize traditional bone setters. Internet J Orthop Surg. 2007;4(2):1–7. [Google Scholar]
- 17.Onyemaechi N.O., Lasebikan O.A., Elachi I.C., Popoola S.O., Oluwadiya K.S. Patronage of traditional bonesetters in Makurdi, north-central Nigeria. Patient Prefer Adherence. 2015;9:275–279. doi: 10.2147/PPA.S76877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Solagberu B.A. Long bone fractures treated by traditional bonesetters: a study of patients’ behaviour. Trop Doct. 2005;35(2):106–108. doi: 10.1258/0049475054036797. [DOI] [PubMed] [Google Scholar]
- 19.Thanni L.O. Factors influencing patronage of traditional bone setters. West Afr J Med. 2000;19(3):220–224. [PubMed] [Google Scholar]
- 20.Owumi B., Patricia A., Olorunnisola A. Utilization of traditional bone-setters in the treatment of bone fracture in Ibadan North Local Government. Int J Humanit Soc Sci. 2013;2(5):47–57. [Google Scholar]
- 21.Wong L.P. Focus group discussion: a tool for health and medical research. Singapore Med J. 2008;49(3):256–260. [quiz 61] [PubMed] [Google Scholar]
- 22.Nwachukwu B.U., Okwesili I.C., Harris M.B., Katz J.N. Traditional bonesetters and contemporary orthopaedic fracture care in a developing nation: historical aspects, contemporary status and future directions. Open Orthop J. 2011;5:20–26. doi: 10.2174/1874325001105010020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Onuminya J.E. The role of the traditional bonesetter in primary fracture care in Nigeria. S Afr Med J. 2004;94(8):652–658. [PubMed] [Google Scholar]
- 24.Oyebola D.D. Yoruba traditional bonesetters: the practice of orthopaedics in a primitive setting in Nigeria. J Trauma. 1980;20(4):312–322. [PubMed] [Google Scholar]
- 25.Udosen A., Otei O., Onuba O. Role of traditional bone setters in Africa: experience in Calabar, Nigeria. Ann Afr Med. 2006;5(4):170–173. [Google Scholar]
- 26.Panda A.K., Swain K.C. Traditional uses and medicinal potential of Cordyceps sinensis of Sikkim. J Ayurveda Integr Med. 2011;2(1):9–13. doi: 10.4103/0975-9476.78183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Agarwal A., Agarwal R. The practice and tradition of bonesetting. Educ Health (Abingdon) 2010;23(1):225. [PubMed] [Google Scholar]