Abstract
Background
Polytrauma can lead to multi-organ dysfunction in addition to the local injuries. Acute kidney injury (AKI) is one of the most common causes and contributors to the high morbidity and mortality. Prevalence of acute kidney injury in trauma patients is as reported to be as high as 40.3%. Early detection and management leads to better outcomes. The prevalence of AKI among polytrauma patients remains unknown in our setting.
Methodology
A cross-sectional study involving all adults with polytrauma who presented at the emergency department at Muhimbili Orthopedic Institute (MOI) was designed. A score of ≥18 on the New Injury Severity Score (NISS) screening tool was used to identify polytrauma patients. The Kidney Disease Improving Global Outcomes (KDIGO) criteria was used to identify patient with polytrauma who developed acute kidney injury. Descriptive statistics were then obtained followed by hypothesis testing between variables with the chi squared test. Logistic regression models were used to determine factors associated with acute kidney injury.
Results
More than half (56.4%) of the patients were between 26 and 40 years and 92.3% of the polytrauma patients were males. Almost 2/5th (38.5%) of the polytrauma patients had acute kidney injury – half of these had stage 1 AKI, 33.3% had stage 2 AKI and the remaining 16.7% had stage 3 AKI. On multivariate logistic regression, it was found that patients who were older than 45 years (OR 8.53, CI 1.65–43.89, p = 0.01) and those patients with Systemic Inflammatory Response Syndrome (SIRS) (OR 21.83, CI 1.66–286.2, p = 0.019) had higher risk of acute kidney injury.
Conclusion
There is high prevalence of AKI among polytrauma patients. Elderly patients and those with SIRS were seen to have higher likelihood of AKI.
Keywords: Polytrauma, Acute kidney injury, Muhimbili Orthopedic Institute, Tanzania
African relevance
-
•
There is a rising number of motor traffic crashes in Africa.
-
•
Polytrauma is responsible for significant morbidity and mortality on the continent.
-
•
Knowledge of the prevalence of acute kidney injury and its risk factors can guide appropriate care and treatment.
Introduction
Trauma causes significant morbidity and mortality in all age groups but particularly for those below 60 years and is one of the top 5 causes of death [1,2]. Most deaths occur in adults who are between 15 and 44 years [3]. Polytrauma originates from the Greek words poly which means multiple and trauma which means wounds. The term polytrauma is defined as a New Injury Severity Score of ≥18 [4]. There are complex pathophysiological changes that happen in a polyrauma patient which requires effective treatment for improving morbidity and mortality outcomes. Hemorrhage, systemic inflammatory response syndrome (SIRS) and multiple organ dysfunction syndrome (MODS) are some of the complications of trauma whose effects are not only local but also systemic. There are mechanisms and triggers which result in cardiovascular shock, hemostasis, apoptosis, organ dysfunctions and immune suppression (CHAOS) [5]. These local and systemic pathophysiological changes that occur in polytrauma (CHAOS) eventually lead to Acute Kidney Injury (AKI) which further worsens their outcomes [6,7].
Acute kidney injury is a clinical syndrome characterized by serum urea and creatinine changes that reflects decrease in glomerular filtration rate and electrolyte imbalances [8]. A higher risk of AKI has been identified among patients with pre-existing chronic kidney disease and pre-existing comorbidities, males, elderly patients and those with higher trauma Injury Severity Score [9,10]. Discontinuation of all nephrotoxic drugs (like NSAID's and antibiotics like gentamycin), ensuring adequate volume status, correction of sepsis, monitoring serum creatinine and urine output, avoiding hyperglycemia and seeking alternatives to investigations with contrast are all used to prevent AKI [11]. A timely diagnosis and management of AKI in polytrauma patients would likely improve their outcomes.
Tanzania is one of the countries that is affected greatly by motor traffic crashes with an almost 50% increase from 1990 to 2000. The risk of mortality in Tanzania for those involved in motor traffic crash is more than 20 times that in the United states of America [12]. A recent study showed that almost 10% of patients attending the hospital presented with trauma-related complaints among which 56.3% were male and had a median age of 30 years. [13] Pre hospital care is almost non-existent in Tanzania for those having suffered trauma and there is quite a delay for trauma patient being brought to the emergency department [14]. This is also true for many countries in Africa such as Malawi [15] and Nigeria [16].
The prevalence of AKI in polytrauma patients in Tanzanian setup is unknown. We have tried to identify the local prevalence of this complication and the factors that are associated with it.
Methods
Study Design and setting
Cross-sectional study was conducted between July 2018 to October 2018 at Muhimbili Orthopedic Institute which is the largest orthopedic and trauma referral center based in Dar-es-salaam. A total of 78 consenting adults over 18 years who presented at MOI with polytrauma were included in the study in consecutive manner. The proposal was ethically cleared by MUHAS ethical clearance board (Ref. No. DA.287/298/01A/) and the MOI administration.
Data collection
Patients who attended MOI emergency department were assessed at the casualty/emergency department according to the NISS and once they fulfilled the criteria of polytrauma (NISS score ≥ 18), standard structured questionnaire was used. Mechanism of injury and time of the injury was recorded. Temperature, oxygen saturation and hemodynamic data including blood pressure (BP), pulse rate (PR), urine output (UO) and fluid management for the first 6 h of arrival at the hospital and whether patient received blood or not was recorded. Glasgow Coma Score (GCS) was scored and recorded. Blood tests for full blood picture, blood group, random blood glucose, serum creatinine were taken and determined. Serum creatinine was also repeated at day 7 to establish diagnosis of AKI from the baseline according to standard KDIGO criteria [17]. Informed consent was obtained from the patient or next of kin after being explained the objectives of the study, ensuring confidentiality. Refusal to participate did not affect patient management. For those who were not able to give their consent (for example due to brain trauma) consent was sought from the next of kin.
Statistical analysis
The data obtained were entered, processed and analyzed by Statistical Package for Social Sciences (SPSS) version 25. Frequency distribution tables and appropriate two by two tables were generated. Means and proportions were calculated for numerical and categorical data respectively. Hypothesis testing between variables was done using the χ2 test and the student's t-test.
Logistic regression models were used to determine factors associated with acute kidney injury. The dependent variable (acute kidney injury) was reported as present or absent. Independent variables which were tested included age, sex, body mass index (BMI), SIRS, the New Injury Severity Score, Glasgow coma score, hypotension, open fracture, use of nephrotoxic drugs, use of contrast CT (computed tomography) scan, blood product requirement, type of surgical intervention, type of anesthesia and duration of surgery. Those variables which had p value of <0.2 in univariate analysis were run in multivariate analysis. Finally multiple logistic regression analysis were done and variables with p < 0.05 were considered statistically significant.
Results
A total of 78 participants were recruited in this study. More than half (56.4%) of the patients were between 26 and 45 years. Among the subjects, 72 (92.3%) were males. (Table 1).
Table 1.
Socio-demographic characteristics of polytrauma patients (N = 78).
| Frequency | Proportion | |
|---|---|---|
|
Age group (years) Mean ± SD; 35.37 ± 12.5 | ||
| 18–25 26–45 46–64 ≥65 |
19 44 13 2 |
24.4% 56.4% 16.7% 2.6% |
| Sex | ||
| Male Female |
72 6 |
92.3% 7.7% |
| Occupation | ||
| Motorcyclist Businessman Peasant Others |
39 13 7 19 |
50% 16.7% 9% 24.4% |
In this study, AKI was seen in 38.5% of the patients who had polytrauma (Fig. 1). Half of the patients with AKI had stage 1 AKI, 10 patients (33.3%) had stage 2 AKI and the remaining 5 patients (16.7%) had stage 3 AKI (Fig. 2).
Fig. 1.
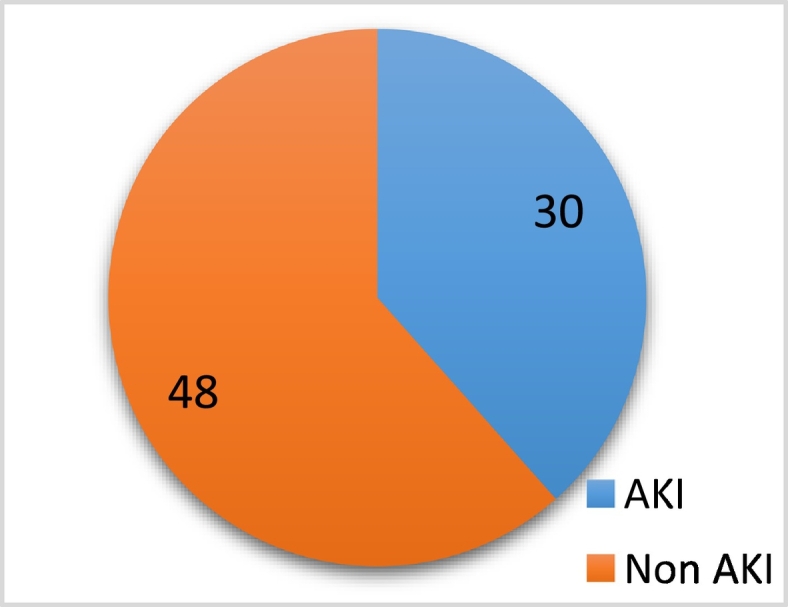
Prevalence of AKI in polytrauma patients (N = 78).
Fig. 2.
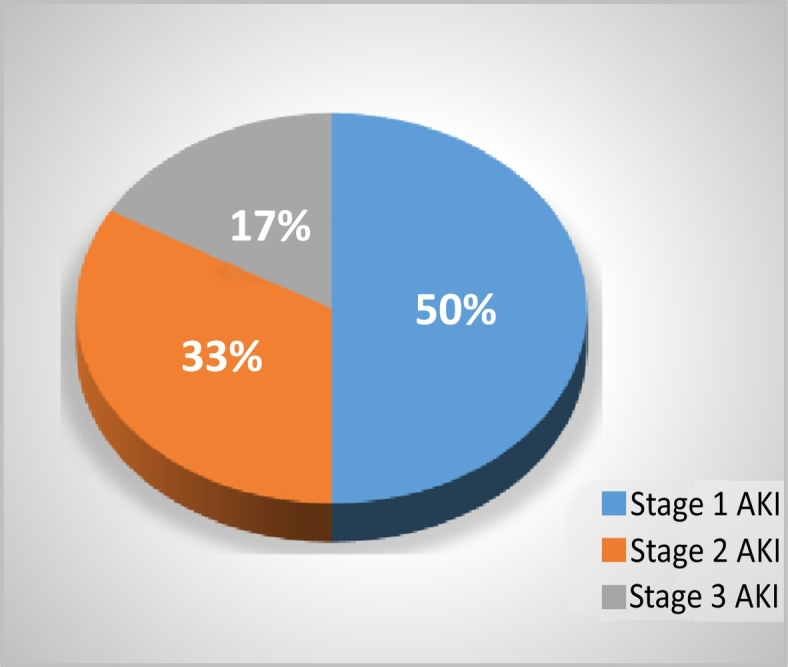
Severity (KDIGO stages) of acute kidney injury (N = 30).
Acute kidney injury was seen in 27 (37.5%) of the male patients with polytrauma (p = 0.545). Prevalence of AKI in age group 18–25 years was 26.4% of patients, compared to 34.1% in ages 26–45 and 61.5% among age group 46–65 years (p = 0.05). Patients who had been injured for <12 h (42.2%) were more likely to develop AKI (p = 0.148). More than 4/5(81.8%) of the patients who had SIRS developed AKI compared to less than 1/3 who did not have (p = 0.001). Seventy five percent of the patients with hypotension on admission had AKI (p = 0.123). All patients with NISS of more than 25 had AKI compared to less than a quarter of the patients with NISS between 18 and 25. This was statistically very significant (p < 0.001). A third of the patients with GCS between 13 and 15 had AKI whilst three quarter of patients with GCS below 13 had AKI (p = 0.081) (Table 2).
Table 2.
Socio-demographic and clinical characteristics against AKI among polytrauma patients.
| Characteristics | Non - AKI | AKI | p-Value |
|---|---|---|---|
| Gender | |||
| Male | 45(62.5%) | 27(37.5%) | 0.545 |
| Female | 3(50%) | 3(50%) | |
| Age | |||
| 18–25 | 14(73.6%) | 5(26.4%) | 0.05 |
| 26–45 | 29(65.9%) | 15(34.1%) | |
| 46–65 | 5(38.5%) | 8(61.5%) | |
| >65 | 0(0%) | 2(100%) | |
| Time of injury | |||
| <12 h | 37(57.8%) | 27(42.2%) | 0.148 |
| >12 h | 11(78.6%) | 3(21.4%) | |
| BMI | |||
| Underweight | 1(100%) | 0(0%) | 0.092 |
| Normal | 26(74.3%) | 9(25.7%) | |
| Overweight | 16(55.2%) | 13(44.8) | |
| Obese | 5(38.5%) | 8(61.5%) | |
| SIRS | |||
| Yes | 2(18.2%) | 9(81.8%) | 0.001 |
| No | 46(68.7%) | 21(31.3%) | |
| MAP | |||
| <60 mmHg | 1(25%) | 3(75%) | 0.123 |
| ≥60 mmHg | 47(63.5%) | 27(36.5%) | |
| NISS | |||
| 18–25 | 48(77.4%) | 14(22.6%) | <0.001 |
| ≥25 | 0(0%) | 16(100%) | |
| GCS | |||
| 13–15 | 46(65.7%) | 24(34.3%) | 0.081 |
| 9–12 | 1(25%) | 3(75%) | |
| ≤8 | 1(25%) | 3(75%) | |
| CT Scan | |||
| Yes | 23(57.5%) | 17(42.5%) | 0.452 |
| No | 25(65.8%) | 13(34.2%) | |
| Fractures | |||
| Closed | 24(88.9%) | 3(11.1%) | <0.001 |
| Open | 24(47.1%) | 27(52.9%) | |
| Diclofenac use | |||
| Yes | 40(58%) | 29(42%) | 0.073 |
| No | 8(88.9%) | 1(11.1%) | |
| Gentamycin use | |||
| Yes | 8(34.8%) | 15(65.2%) | 0.002 |
| No | 40(72.7%) | 15(27.3%) | |
| Blood transfusion | |||
| Yes | 32(51.6%) | 30(48.4%) | <0.001 |
| No | 16(100%) | 0(0%) | |
| Surgery done | |||
| Yes | 28(50%) | 28(50%) | 0.001 |
| No | 20(90.9%) | 2(9.1%) | |
| Type of surgery | |||
| Damage control | 17(50%) | 17(50%) | 0.011 |
| Definitive orthopedics | 3(50%) | 3(50%) | |
| Neurosurgery | 8(50%) | 8(50%) | |
| Duration of surgery | |||
| <2 h | 10(52.6%) | 9(47.4%) | 0.778 |
| ≥ 2 h | 18(48.6%) | 19(51.4%) | |
| Anesthesia used | |||
| GA | 14(40%) | 21(60%) | 0.001 |
| Spinal | 14(66.7%) | 7(33.3%) | |
Among the polytrauma patients with open fractures, AKI was seen in more than half (52.9%) as compared to only 11.1% of those with closed fracture/s (p < 0.001). Gentamycin use was associated with AKI (65.2%, p = 0.002) but not associated with diclofenac use (42%, p = 0.073). Blood transfusion was also associated with AKI (48.4%, p < 0.001) (Table 2).
Half of the patients who underwent surgery developed (AKI 50%, p = 0.001). The type of surgery also determined the severity of AKI, definitive orthopedic surgery in a polytrauma patient had twice the risk of stage 3 AKI compared to damage control surgery. This relationship was also shown to be statistically significant with p-value of 0.01. (sub analysis not shown). However, the duration of surgery was not significant to the development of AKI. Patients who underwent general anesthesia (GA) (60%) were more likely to develop AKI compared to those who underwent spinal anesthesia (SA) (33.3%) (p = 0.001) (Table 2).
Acute kidney injury was found to be 8 fold higher in patients older than 45 years (OR 8.53 (CI 1.658–43.893), p 0.01) and 21 fold higher in those with Systemic Inflammatory Response Syndrome (OR 21.83 (CI 1.66–286.2), p = 0.019) (Table 3).
Table 3.
Logistic regression analysis.
| Characteristic | Comparison | Adj OR(*) | CI | p-Value |
|---|---|---|---|---|
| Age: ≥45 | <45 | 8.53 | 1.658–43.893 | 0.01 |
| Fracture: open | closed | 7.047 | 0.258–192.8 | 0.247 |
| SIRS | No SIRS | 21.83 | 1.66–286.2 | 0.019 |
| MAP < 60 mmHg | MAP > 60 mmHg | 5.22 | 0.517–52.72 | 0.161 |
| GCS ≤ 12 | >13 | 4.589 | 0.458–45.98 | 0.195 |
| Diclofenac use | No diclofenac use | 3.189 | 0.226–45.019 | 0.391 |
| Gentamycin use | No gentamycin use | 2.12 | 0.599–7.51 | 0.244 |
| BMI >25 | ≤25 | 2.45 | 0.724–8.3 | 0.149 |
| Blood transfusion | No blood transfusion | 6.2 | 0.51–4.55 | 0.779 |
| Surgery | No surgery done | 1.37 | 0.017–114.2 | 0.888 |
| General anesthesia | Spinal anesthesia | 1.8 | 0.388–8.372 | 0.452 |
* Adjusted odds ratio.
Discussion
We report a 38.5% prevalence of AKI among polytrauma patients. Half of the patients with AKI had stage 1 AKI, 10 patients (33.3%) had stage 2 AKI and the remaining 5 patients (16.7%) had stage 3 AKI. Most of the polytrauma patients (80.8%) were between the ages of 18–45 years. These findings indicate a huge and as yet unrecognized burden of AKI among polytrauma patients in Dar-es-salaam. Previous studies have shown a similar prevalence and socio-demographic distribution in different parts of the world [[18], [19], [20], [21], [22]].
Acute kidney injury was 8.53 times more likely to occur in patients more than 45 years compared to patients less than or equal to 45 years. This has been the trend in other parts of the world as well with higher renal insults from trauma in the elderly of up to 3 to 6 fold [23,24] Age-related changes including structural and physiological changes are greatly responsible for this. Changes which occur in the kidneys include decrease in renal mass with aging [25,26], loss of cortico-glumeruli due to ischemic changes, subclinical injury to kidney from co morbid conditions, reduction in number and size of tubules, increasing tubulo-interstitial fibrosis and a decrease in glomerular filtering surface [24,[27], [28], [29]]. Age related accumulation of co morbidities that need procedures, medicines which are nephrotoxic and other kidney stressors causes increased risk of acute kidney injury [30]. At the microscopic level, studies have found that stressors such as acute infection or trauma in the setting of co-morbid conditions leads to exacerbated ischemic changes and injury to the nephrons [31]. Although AKI is reversible, it is implicated in the development of chronic kidney disease especially in the elderly population [29]. This further confounds the problem of ‘this acute injury’ having ‘chronic consequences’.
The systemic inflammatory response syndrome (SIRS) criteria represents a series of objective physical and laboratory findings indicative of an infectious or non-infectious insult [32]. It is simple and can be done at the bedside and can be an invaluable tool in resource constrained settings like ours. Using this simple tool, we found that patients with SIRS were 21 times more likely to develop AKI than those without SIRS in this study. In comparison, more complex tools like the APACHE II tool (acute physiology score + age points + chronic health points) [33] are harder to adapt to this setting and were not used in this study.
Majority of patients (82.1%) presented to the facility within 12 h of the injury. This is quite significant because pre-hospital care is almost non-existent in Tanzania. Delays in reaching the emergency department following trauma has been reported before [14] and may be a significant contributor to post trauma morbidity and mortality. However, we found that more patients (42.8%) who presented to the facility within 12 h had AKI compared to those with delayed presentation (21.4%). One possible explanations to this finding includes our unique subset of ‘polytrauma’ patients rather than just ‘trauma’ patients, in the sense that the seriousness of these patients may have prompted rapid referrals to this tertiary trauma center, compared to the delays that have previously been shown in literature [14]. Further, the ‘time to treatment vs outcome’ relationship shown in this sense applies only to the development of AKI. Non AKI morbidities (e.g. mortality, amputation rates etc.) that could also potentially be influenced by delays have not been addressed by this study.
Half of the patients who underwent emergency surgery had AKI. However this very strong association disappeared on multivariate modeling. While surgery may at first glance appear to cause a strong renal insult due to the second hit phenomenon [34,35] the mere fact that there is trauma with significant physiological disruption (as noted by the abnormal SIRS criteria) may be enough to push polytrauma patients into AKI. Attention to the ‘kidneys’ of polytrauma victims must thus be paid from the beginning of their admission, rather than to offer ‘exaggerated treatment’ for surgical candidates alone.
The use of drugs like diclofenac (commonly used for pain) and gentamycin (commonly used for infections) cannot be undermined in polytrauma patients in terms of their nephrotoxic potential. We saw that 65% and 42% of gentamycin and diclofenac users respectively developed AKI. While statistically not significant in our multivariate analysis, we feel that in a larger cohort of patients, the relationship between such nephrotoxic drugs and AKI may be more evident. As such the standard of care for nephro-protective treatment must include avoidance of unnecessary nephrotoxic drugs and renal dosing of antibiotics where appropriate (especially for open fractures), as would be the case in any other (non-traumatic) severe medical illness.
This study was limited in the following ways. First, the setting of the study (in a national level speciality trauma centre) may have meant that any patients with polytrauma who could not make it to MOI from within the referral zone, could not be captured in this study. The weakness of the emergency response system in Dar es salaam is well known [14] and beyond the control of the investigators. Secondly, the KDIGO criteria for acute kidney injury that was used in the study includes serum creatinine changes within 48 h and 7 days. For this study the control serum creatinine was done only at day 7 and not taken 48 h after the 1st sample. Some cases of acute kidney injury which may have resolved before day 7 but present within 48 h might have missed. We feel this shortcoming may have self-mitigated given that those whom we might have missed in the first 48h may actually represent very mild and transient forms of AKI.
With the findings of this study, we hope to improve awareness on the reality of renal insults in polytrauma patients in the county. We hope the findings of this study will alter our local practice into the engagement of physicians and nephrologists into the co management of such patients. We hope to improve our choices of medicines given to these patients. And whilst there were no incidences of any of our AKI patients requiring organ support in this study, in a larger more national perspective, organ support services like dialysis and ventilation may be required.
Conclusion
There is high prevalence (38.5%) of AKI among polytrauma patients at MOI. Elderly patients and those with SIRS were seen to have higher likelihood of AKI.
A high index of suspicion is necessary to identify patients with AKI. Special attention needs to be given to high risk groups for example elderly patients and those with SIRS. More studies can be done to look at short and long-term outcomes and potential interventions for AKI in polytrauma patients.
Dissemination of results
The findings of this research were initially presented at the departmental level after which were presented at the annual university scientific conference (7th MUHAS scientific conference). The results were also presented as an oral presentation at the 6th NESOT (Nephrology Society of Tanzania) annual scientific conference and the 20th annual COSECSA (College of surgeons, East, central and Southern African) conference.
Funding
The research was self-funded by the authors.
Authors’ contribution
Authors contributed as follow to the conception or design of the work; the acquisition, analysis, or interpretation of data for the work; and drafting the work or revising it critically for important intellectual content: MSMH contributed 50%; MM contributed 20%; KSN contributed 15%; PR contributed 10%; and KK contributed 5%. All authors approved the version to be published and agreed to be accountable for all aspects of the work.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declaration of competing interest
The authors declare that they have no conflicts of interest.
Acknowledgements
We would like to thank Dr. Billy Haonga, Head of Orthopedics and Trauma department at MUHAS for his assistance with the entire project. We would also like to thank Dr. Candida Moshiro who helped during analysis and interpretation of the results. We would also like to show appreciation to Prof. Karim Manji, Dr. Zahra Nagri, Dr. Sibtain Moledina and Dr. Hussein Karim for their help during the study. Thanks goes to entire MOI staff and most importantly the patients without whom the study wouldn't have been possible.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.afjem.2020.08.004.
Appendix A. Supplementary data
Supplementary material
References
- 1.Păun S., Beuran M., Negoi I. Trauma--epidemiology: where are we today? Chir (Bucharest, Rom 1990) 2011;106:439–443. [PubMed] [Google Scholar]
- 2.El Mestoui Z., Jalalzadeh H., Giannakopoulos G.F., Zuidema W.P. Incidence and etiology of mortality in polytrauma patients in a Dutch level I trauma center. Eur J Emerg Med. 2017;24:49–54. doi: 10.1097/MEJ.0000000000000293. [DOI] [PubMed] [Google Scholar]
- 3.Byun C.S., Park I.H., Oh J.H. Epidemiology of trauma patients and analysis of 268 mortality cases: trends of a single center in Korea. Yonsei Med J. 2015;56:220–226. doi: 10.3349/ymj.2015.56.1.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gebhard F., Huber-Lang M. Polytrauma—pathophysiology and management principles. Langenbecks Arch Surg. 2008;393:825. doi: 10.1007/s00423-008-0334-2. [DOI] [PubMed] [Google Scholar]
- 5.Keel M. Trentz o. Pathophysiol polytrauma Inj. 2005;36:691–709. doi: 10.1016/j.injury.2004.12.037. [DOI] [PubMed] [Google Scholar]
- 6.Ricci Z., Cruz D., Ronco C. The RIFLE criteria and mortality in acute kidney injury: a systematic review. Kidney Int. 2008;73:538–546. doi: 10.1038/sj.ki.5002743. [DOI] [PubMed] [Google Scholar]
- 7.Thakar C.V., Christianson A., Freyberg R. Incidence and outcomes of acute kidney injury in intensive care units: a veterans administration study*. Crit Care Med. 2009;37:2552–2558. doi: 10.1097/CCM.0b013e3181a5906f. [DOI] [PubMed] [Google Scholar]
- 8.Rewa O., Bagshaw S.M. Acute kidney injury—epidemiology, outcomes and economics. Nat Rev Nephrol. 2014;10:193. doi: 10.1038/nrneph.2013.282. [DOI] [PubMed] [Google Scholar]
- 9.Daher E.D.F., Maria R., Mota S., Menezes F.A. vol. 124. 2006. Risk factors for death among critically ill patients with; pp. 257–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cury F., Baitello A.L., Echeverria R.F. Rates of thoracic trauma and mortality due to accidents in Brazil. Ann Thorac Med. 2009;4:25. doi: 10.4103/1817-1737.44782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kellum J.A., Lameire N., Aspelin P. Kidney Disease: Improving Global Outcomes (KDIGO) acute kidney injury work group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int. 2012;2:1. doi: 10.1038/kisup.2012.6. [DOI] [Google Scholar]
- 12.Museru L.M., Mcharo C.N.L.M.T. Road traffic accidents in Tanzania: a ten year epidemiological appraisal. East Cent African J Surg. 2002;7:23–26. doi: 10.1017/CBO9781107415324.004. [DOI] [Google Scholar]
- 13.Sawe H.R., Mfinanga J.A., Mbaya K.R. Trauma burden in Tanzania: a one-day survey of all district and regional public hospitals. BMC Emerg Med. 2017;17:30. doi: 10.1186/s12873-017-0141-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boniface R., Museru L., Kiloloma O., Munthali V. Factors associated with road traffic injuries in Tanzania. Pan Afr Med J. 2016 doi: 10.11604/pamj.2016.23.46.7487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chokotho L., Mulwafu W., Singini I. First responders and prehospital care for road traffic injuries in Malawi. Prehosp Disaster Med. 2017;32:14–19. doi: 10.1017/S1049023X16001175. [DOI] [PubMed] [Google Scholar]
- 16.Ibrahim N.A., Ajani A.W.O., Mustafa I.A. Road traffic injury in Lagos, Nigeria: assessing prehospital care. Prehosp Disaster Med. 2017:1–7. doi: 10.1017/S1049023X17006410. [DOI] [PubMed] [Google Scholar]
- 17.Ülger F., Küçük M.P., Küçük A.O. Evaluation of acute kidney injury (AKI) with RIFLE, AKIN, CK, and KDIGO in critically ill trauma patients. Eur J Trauma Emerg Surg. 2018;44:597–605. doi: 10.1007/s00068-017-0820-8. [DOI] [PubMed] [Google Scholar]
- 18.Kalsotra N., Mahajan V., Kalsotra G. Epidemiology of polytrauma in a tertiary care centre. J Evol Med Dent Sci. 2016;5:3021–3025. doi: 10.14260/jemds/2016/703. [DOI] [Google Scholar]
- 19.de Abreu K.L.S., Silva Júnior G.B., Barreto A.G.C. Acute kidney injury after trauma: prevalence, clinical characteristics and RIFLE classification. Indian J Crit Care Med. 2010;14:121–128. doi: 10.4103/0972-5229.74170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Haines R.W., Lin S.P., Hewson R. Acute kidney injury in trauma patients admitted to critical care: development and validation of a diagnostic prediction model. Sci Rep. 2018 doi: 10.1038/s41598-018-21929-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harrois A., Libert N., Duranteau J. Acute kidney injury in trauma patients. Curr Opin Crit Care. 2017;23(6):447–456. doi: 10.1097/MCC.0000000000000463. [DOI] [PubMed] [Google Scholar]
- 22.Lecky F., Bouamra O., Woodford M. Damage Control Management in the Polytrauma Patient. 2017. Changing epidemiology of polytrauma; pp. 27–32. [Google Scholar]
- 23.Rosner M.H. Acute kidney injury in the elderly. Clin Geriatr Med. 2013;29:565–578. doi: 10.1016/j.cger.2013.05.001. [DOI] [PubMed] [Google Scholar]
- 24.Coca S.G. Acute kidney injury in elderly persons. Am J Kidney Dis. 2010;56:122–131. doi: 10.1053/j.ajkd.2009.12.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lindeman R.D. Overview: renal physiology and pathophysiology of aging. Am J Kidney Dis. 1990;16:275–282. doi: 10.1016/S0272-6386(12)80002-3. [DOI] [PubMed] [Google Scholar]
- 26.Lindeman R.D., Preuss H.G. Renal physiology and pathophysiology of aging. Geriatr Nephrol Urol. 1994;4:113–120. [Google Scholar]
- 27.Frocht A., Fillit H. Renal disease in the geriatric patient. J Am Geriatr Soc. 1984;32:28–43. doi: 10.1111/j.1532-5415.1984.tb05148.x. [DOI] [PubMed] [Google Scholar]
- 28.Kaplan C., Pasternack B., Shah H., Gallo G. Age-related incidence of sclerotic glomeruli in human kidneys. Am J Pathol. 1975;80:227–234. [PMC free article] [PubMed] [Google Scholar]
- 29.YIlmaz R., Erdem Y. Acute kidney injury in the elderly population. Int Urol Nephrol. 2010;42:259–271. doi: 10.1007/s11255-009-9629-7. [DOI] [PubMed] [Google Scholar]
- 30.Farooqi S., Dickhout J.G. Major comorbid disease processes associated with increased incidence of acute kidney injury. World J Nephrol. 2016 doi: 10.5527/wjn.v5.i2.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Basile D.P., Anderson M.D., Sutton T.A. Pathophysiology of acute kidney injury. Compr Physiol. 2012;2:1303–1353. doi: 10.1002/cphy.c110041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Klouwenberg P.M.C.K., David D.S., Bonten M.J.M., Cremer O.L. Classification of sepsis, severe sepsis and septic shock: the impact of minor variations in data capture and definition of SIRS criteria. Intensive Care Med. 2012 doi: 10.1007/s00134-012-2549-5. [DOI] [PubMed] [Google Scholar]
- 33.Raith E.P., Udy A.A., Bailey M. Prognostic accuracy of the SOFA score, SIRS criteria, and qSOFA score for in-hospital mortality among adults with suspected infection admitted to the intensive care unit. JAMA-J Am Med Assoc. 2017 doi: 10.1001/jama.2016.20328. [DOI] [PubMed] [Google Scholar]
- 34.Giannoudis P V Surgical priorities in damage control in polytrauma. doi: 10.1302/0301-620X.85B4.14217. [DOI] [PubMed]
- 35.Pape H.C., Halvachizadeh S., Leenen L. Timing of major fracture care in polytrauma patients – an update on principles, parameters and strategies for 2020. Injury. 2019 doi: 10.1016/j.injury.2019.09.021. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.


