Abstract
Background:
We hypothesized that postoperative delirium is associated with diminished recovery toward baseline preoperative ambulation levels one-month postoperatively.
Methods:
Patients included were ≥60 years old undergoing inpatient operations. Ambulation was measured as steps/day using an accelerometer worn for ≥3-days preoperatively and ≥28- days postoperatively. Primary outcome was the percent recovery of preoperative steps.
Results:
109 patients were included; 17 (16%) developed postoperative delirium. Recovery of ambulation toward preoperative baseline at postoperative day-28 was decreased in delirium group (34% vs. 69%;p<0.01). Immediate postoperative ambulation was similar in the delirium vs. no-delirium groups(p=0.79). Delirium occurred on average on postoperative 3±4 days. Subsequently, ambulation was decreased in the delirium group compared to non-delirium group at postoperative week-1(p=0.01), week-2(p=0.02), week-3(p<0.01) and week-4(p<0.01).
Conclusion:
Patients undergoing inpatient operations who develop delirium recover only one- third of their baseline steps one-month postoperatively. Postoperative delirium results in a decreased recovery towards baseline ambulation for at least 4-weeks following major operations in comparison to non-delirious patients. The decrease in ambulation in the delirium versus no-delirium groups occurred after the occurrence of postoperative delirium.
Keywords: Accelerometer Activity Tracker, Postoperative delirium, Older Adults, Ambulation
Introduction:
Delirium is the most common postoperative complication in older adults.1 Delirium is closely related to adverse healthcare outcomes including major complications, prolonged length of stay, functional decline, impaired cognition and death.2,3 Delirium is a modifiable postoperative complication given that one third of hospitalized delirium is preventable using bedside supportive care interventions.4 With an aging population, understanding the clinical consequences of postoperative delirium is increasingly important.5
An older adult’s ability to ambulate is a vital measure of their well-being. Mobility, or walking, represents a physical health parameter which equates to both independent living and quality of life.6–8 Recent development of wearable activity trackers allows quantification of postoperative recovery and ambulation.9 Currently, a gap in knowledge exists delineating the relationship between postoperative delirium and recovery towards the patient-centered outcome of baseline preoperative ambulation.
The purpose of this study was to determine if postoperative delirium is associated with a delay in recovery of baseline ambulation levels in older adults undergoing major inpatient operations. The specific aims of the study were: (1) to compare the recovery of postoperative ambulation in patients with and without delirium, (2) to determine when the postoperative ambulation recovery trajectories diverge in patients with and without delirium.
Methods:
Participants were enrolled at the Rocky Mountain VA Medical Center between November 2016 to June 2018. Inclusion criteria were patients with advanced age (≥60 years) scheduled for major elective abdominal or thoracic operations with inpatient hospitalizations >48 hours. The reason for selection of age cut-off of 60 years was our prior work which found this population to be at high risk for postoperative delirium.3 Exclusion criteria included emergency/urgent procedures (because baseline preoperative activity levels could not be measured), non-ambulatory patients, and procedures that did not require hospital admission. The research was approved by the Colorado Multi-Institutional Review Board (COMIRB 16–1776) and all participants provided written informed consent prior to participation.
Patients wore an accelerometer activity tracking device (Vivofit3; Garmin Ltd, Schaffhausen, Switzerland) on their non-dominate wrist for a minimum of 3 full calendar days preoperatively and 28 calendar days postoperatively. This activity tracker is validated to track steps according to the gold standard of <1% deviation from a video observation of steps taken.10 The primary outcome was postoperative steps/day reported as a percent of baseline ambulation levels. The primary outcome variable was calculated as the ratio of each participant’s postoperative steps/day divided by that same participants pre-operative average steps per day. This ratio reflects the percent of steps towards preoperative baseline that the patient has recovered. Day of surgery steps per day were not included. Complete data included at least 3 preoperative days of recordings and 28 days of postoperative recordings. Partial data was defined as having at least 14 postoperative days of data. Participants were blinded to the activity tracker recordings. Data collection methodology has been reported by this group previously.9 Steps per day reported as median with inter-quartile range (IQR) because step distribution data was non-parametric. Percent recovery was comparted immediately postoperatively (average postoperative days 1 – 2), postoperative week 1 (average postoperative days 6 – 8), postoperative week 2 (average postoperative days 13 – 15), postoperative week 3 (average postoperative days 20 – 22), and postoperative week 4 (average postoperative days 26 – 28).
The predictor variable was the occurrence of postoperative delirium. Postoperative delirium was assessed twice daily in the ICU using the Confusion Assessment Method-ICU (CAM-ICU).11 The CAM-ICU identifies acute changes in alertness, cognition, and attention. It is the most widely used and validated tool for diagnosis of ICU delirium by nonpsychiatric clinicians.11 The CAM-ICU was validated in that when one or more CAM-ICU tests are positive, delirium is diagnosed as present.11 Additionally, validated chart review was performed identifying key terms or descriptors to suggest an acute change in the patient’s mental status that were indicative of the development of delirium.12 If either the CAM-ICU or chart review identified delirium as present, the patient was considered delirium positive.
Other prospectively recorded information included preoperative, intraoperative, and postoperative clinical variables. Preoperative clinical variables included demographics, the Charlson Comorbidity Index13, the American Society of Anesthesiologists (ASA) physical status class14, cognitive function using the Mini-Cog test (a validated test to screen for the presence of impaired cognition15), and frailty (defined using the frailty score described by Robinson et al and assesses the following seven characteristics; The Timed Up and Go test, the Katz Score, Mini-COG score, Charlson Comorbidity Index, presence of anemia of chronic disease, albumin level to determine nutritional status, presence of the geriatric syndrome of falls16). Preoperative comorbidities reported were defined using variable definitions established by the National Surgical Quality Improvement Program (NSQIP). Intraoperative variables included operation length in minutes, procedure type, and blood loss. Postoperative variables included length of stay, surgical complications (cardiac, pulmonary, renal, infectious and thrombotic using NSQIP established complication definitions17) and readmissions.
Statistical Analysis
The R Project for Statistical Computing Version 3.3.3 (Vienna, Austria) was used for all statistical analysis.18 On univariable analysis, a two-tailed Chi-Square Test was used when comparing proportions, except in cases of small counts where Fisher’s exact test was more appropriate. A student’s t-test was used for comparison of variables with a normal distribution, which are presented as mean ± standard deviation (SD). Wilcoxon rank-sum test was used for comparison of non-parametric continuous variables including percent recovery, presented as median [interquartile range, IQR]. Figure 2 was created using loess non-parameteric smoothed conditional means with a smoothing span of 0.45 to determine trends of percent recovery over time in each of the compared groups. Because univariate analysis found a close association between long operation times and postoperative delirium, the data was analyzed to account for the potential confounding relationship of a longer operations being the reason for decreased ambulation one month postoperatively rather than delirium. This analysis consisted of defining operations of >180 minutes as long operations and plotting the ambulatory recovery trajectory of patients without delirium both with short and long operations in comparison to the recovery trajectory of patients with delirium.
Figure 2. Post-Operative Ambulation Recovery Trajectories in Older Adults With and Without Delirium.

Postoperative recovery trajectories (with 95% confidence intervals) depicted as a percent of pre-operative baseline ambulation levels. Patients with and without delirium had similar ambulation levels immediately after the operation (p=0.79). The average onset of delirium was postoperative day 3. Subsequent to onset of delirium, ambulation recovery trajectories diverged; resulting in patients with delirium having reduced ambulation compared to non-delirious patients.
Results:
Enrollment flow diagram depicted in Figure 1. Included in the study were 109 patients with an average age of 70 ± 5 years who walked a preoperative baseline average of 5,059±2,910 steps/day. Complete data (all 28 postoperative days collected) was available for 94 (86%) patients and partial data (at least 14 postoperative days collected) was available for 15 (14%) patients. Incomplete data (41 or 150) is comparable to the existing literature of the use of outpatient accelerometers to measure step counts.19
Figure 1.
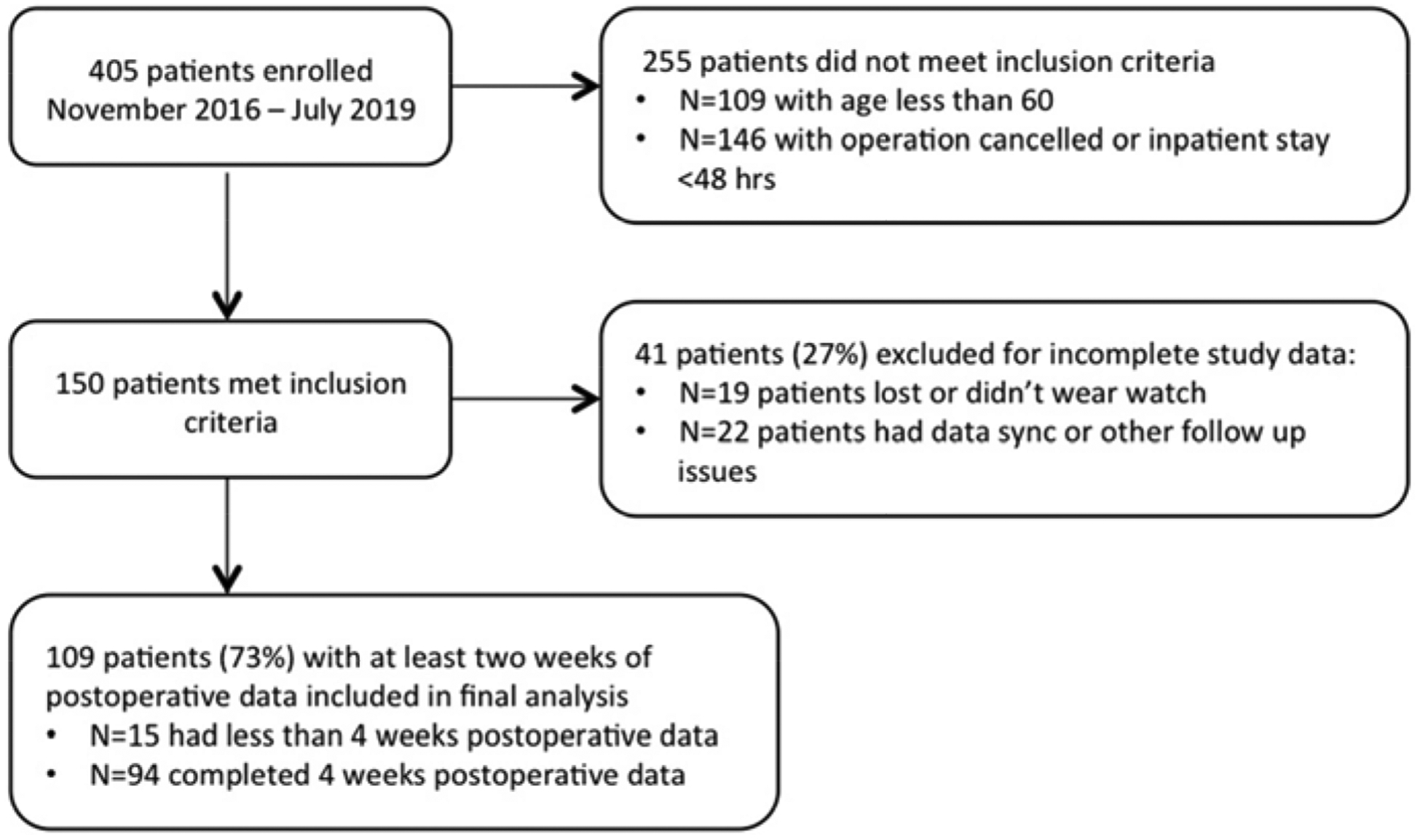
Flow diagram for patient inclusion
Of the 109 patients, 17 (16%) patients developed postoperative delirium. Of the patients diagnosed with delirium, 76% (13) were diagnosed with the CAM-ICU and 24% (4) by validated chart review. Preoperative, intraoperative and postoperative clinical variables compared using univariate analysis in the groups with and without delirium in Table 1. Preoperatively, patients with delirium had higher rates of dementia (18% vs. 2%; p=0.03), higher rates of COPD (29% vs 9%, p=0.04) and decreased cognition by screening with Mini-Cog Test (median score 3 vs 4, p=0.02). Of all participants, 77% (84) had ICU stays. Intraoperatively, patients with delirium had longer operations longer operations (293 vs. 199 minutes; p=0.04). Postoperatively, patients with delirium had longer hospital stays (8 vs. 6 days; p=0.04).
Table 1:
Baseline characteristics, and comparison of patients with and without postoperative
| TOTAL COHORT n=109 | NO DELIRIUM n=92 | YES DELIRIUM n=17 | p-value | |
|---|---|---|---|---|
| PREOPERATIVE CHARACTERISTICS | ||||
| Age (years) (mean ± SD) | 70 ± 5 | 69 ± 6 | 70 ± 4 | 0.66 |
| Male sex (%) | 104 (95%) | 87 (95%) | 17 (100%) | 0.72 |
| BMI (mean ± SD) | 28 ± 5 | 28 ± 5 | 27 ± 6 | 0.30 |
| Diabetes (%) | 34 (31%) | 28 (30%) | 6 (35%) | 0.91 |
| COPD (%) | 13 (12%) | 8 (9%) | 5 (29%) | 0.04 |
| Dementia (%) | 5 (5%) | 2 (2%) | 3 (18%) | 0.03 |
| Charlson Comorbidity Index (median [IQR]) | 2 [1, 3] | 2 [1–3] | 3 [2–4] | 0.05 |
| ASA (median [IQR]) | 3 [3,3] | 3 [3–3] | 3 [3–4] | 0.20 |
| Mini COG Score (median [IQR]) | 4 [3,5] | 4 [3–5] | 3 [2–5] | 0.02 |
| Frail Score (median [IQR]) | 1 [0, 2] | 1 [0–2] | 1 [1–2] | 0.11 |
| INTRAOPERATIVE VARIABLES | ||||
| Operation type | 0.23 | |||
| Cardiothoracic | 26 (24%) | 20 (22%) | 6 (35%) | |
| Abdominal | 83 (76%) | 72 (78%) | 11 (65%) | |
| Operative approach | 0.85 | |||
| Open | 65 (60%) | 53 (58%) | 12 (71%) | |
| Laparoscopic/Robotic | 44 (40%) | 29 (42%) | 5 (29%) | |
| Operative time (minutes) (mean ± SD) | 238±131 | 227±127 | 298 ±142 | 0.04 |
| Blood Loss in mL (median [IQR]) | 68 [35,213] | 50 [32–206] | 196 [91–251] | 0.12 |
| ICU Admission (%) | 84 (77%) | 68 (74%) | 16 (94%) | 0.13 |
| POSTOPERATIVE OUTCOMES | ||||
| Hospital LOS (median [IQR]) | 6 [3, 9] | 6 [3–8] | 8 [4–14] | 0.04 |
| Discharge to Facility (%) | 5 (5%) | 3 (3%) | 2 (12%) | 0.17 |
| Major postoperative complication (%) | 10 (9%) | 9 (7%) | 3 (18%) | 0.15 |
| Hospital Readmission | 14 (13%) | 11 (12%) | 3 (18%) | 0.46 |
delirium
IQR= Interquartile Range, BMI = Body Mass Index, COPD =Chronic Obstructive Pulmonary Disease, ASA = American Society of Anesthesiologists physical status classification system, ICU= Intensive Care Unit, LOS= Length of Stay, POD = Postoperative Day
Operations included in this study were major abdominal 76% (83) and thoracic 24% (26). Abdominal operations included were: 32 colectomies, 10 pancreas resections, 9 liver resections, 8 abdominal wall reconstructions, 6 nephrectomies, and 18 miscellaneous operations. Thoracic operations included were: 17 open heart, 5 lung resections, 3 esophagectomies and 2 miscellaneous operations.
Ambulation
At preoperative baseline, patients with and without delirium walked a similar number of steps per day (4,995 vs. 5,412 steps/day; p=0.59). Postoperative ambulation was similar in the patients with and without delirium immediately following the operation (p=0.79). The average time to onset of initial episode of delirium was 3±4 days; an average time of initial onset of delirium which was two days later than immediate postoperative steps/day comparison. The subsequent percent recovery of baseline ambulation levels was decreased in the delirium group compared to the no delirium group at postoperative week 1 (p=0.01), postoperative week 2 (p=0.02), postoperative week 3 (p<0.01) and postoperative week 4 (p<0.01). Table 2 describes peri-operative ambulation levels. Figure 2 is a graphical representation postoperative ambulation (steps/day) as a percent of baseline ambulation levels over the first 28 postoperative days.
Table 2. Recovery of Postoperative Ambulation as a Percent of Preoperative Baseline.
Percentage values reported represent average percent steps/day compared to baseline preoperative average steps/day. Data reported as average ± standard deviation with comparisons made using a Wilcoxon rank sum test. Abbreviation: Post-Op = Postoperative
| NO DELIRIUM n=92 | YES DELIRIUM n=17 | p-value | |
|---|---|---|---|
| Pre-Op Average Steps/Day | 4,995±2,976 | 5,412±2,582 | 0.59 |
| Immediate Post-Op | 9 ± 13% | 10 ± 22% | 0.79 |
| Post-Op 1 Week | 38 ± 28% | 19 ± 15% | 0.01 |
| Post-Op 2 Weeks | 53 ± 31% | 33 ± 31% | 0.02 |
| Post-Op 3 Weeks | 63 ± 36% | 36 ± 26% | <0.01 |
| Post-Op 4 Weeks | 71 ± 39% | 34 ± 32% | <0.01 |
The average duration of delirium was 2.6 ± 2.0 days (range 1 to 8 days). There was no difference in walking levels four-weeks after surgery in patient with short duration delirium (1 or 2 days) 45±29% of baseline preoperative steps in comparison to patients with long duration delirium (≥3 days) 25±28% of baseline preoperative steps (p=0.18). The average time to initial onset of delirium was postoperative day 3±4 days (range 1 to 18 days). There was no difference in walking levels four-weeks after surgery in patient with who had early initial onset of delirium (on postoperative days 1 and 2) 39±16% of baseline preoperative steps in comparison to patients with developed delirium later in their postoperative course (on postoperative day 3 or later) 33±50% of baseline preoperative steps (p=0.71).
Operation Time and Delirium
To account for a longer operation potentially confounding the relationship between delirium and decrease ambulation one month postoperatively, ambulation recovery trajectories of long (>180 minutes) and short operations in patients without delirium were compared to the recovery trajectory of patients with delirium. Patients with delirium had a decreased percent of preoperative baseline ambulation at 28 days postoperatively compared to non-delirious patient with long (p=0.03) and short (p<0.01) operations. See figure 3 for graphic depiction of ambulation recovery trajectory of non-delirious patients with both long and short operations in comparison to patients with delirium.
Figure 3. Accounting for the Effect of Long Operative Time on Post-Operative Ambulation Recovery Trajectories in Older Adults With and Without Delirium.

Long operative times (>180 minutes) on univariate analysis were closely associated with the occurrence of delirium. The goal of this analysis was to account for a long operative times confounding the relationship between delirium and decreased ambulation. The decreased ambulation resulting from delirium (red line) was greater than the decreased ambulation resulting from long operations in patients without delirium (green line). Patients with delirium had a decreased percent of preoperative baseline ambulation at 28 days postoperatively compared to non-delirious patient with long (p=0.03) and short (p<0.01) operations. This analysis suggests that delirium was the cause of lower ambulation levels independent of the extent of the operation. Recovery trajectories with 95% confidence intervals depicted.
Discussion:
Postoperative delirium is strongly associated with decreased recovery towards preoperative baseline ambulation levels at 28 days postoperatively. At postoperative day 28, patients with delirium have regained only one third of preoperative baseline steps per day in comparison to patients without delirium who had gained two thirds of their baseline steps. Immediate postoperative levels of ambulation are similar in delirious and non-delirious patients. After the immediate postoperative time, on an average of postoperative day 3, delirium occurs. Subsequently, return towards preoperative baseline ambulation levels is decreased in patients who develop delirium in comparison to patients without delirium. Decreased ambulation levels resulting from delirium appeared to be independent of longer operative times. Baseline risk factors for the development of postoperative delirium found in this study were dementia (which has long been recognized as the strongest preoperative risk factor for postoperative delirium with an odd ratio of greater than two-fold3) and COPD (pulmonary disease is a recognized risk factor for postoperative delirium20 but is not consistently found in all studies on risk factors for postoperative delirium).
The cornerstones of patient-centered surgical outcomes are represented by postoperative recovery of mental and physical function. The current study highlights the inter-relationship of compromised mental function (delirium) to subsequent decrements in physical function (ambulation). Increasing the surgical communities’ understanding of mental and physical outcomes is vitally important to improve the consent process of older adults. While traditional surgical preoperative counseling focused on 30-day postoperative morbidity and mortality, recent literature finds that older adults are more interested in understanding the mental and physical consequences of major operations in comparison to the traditional outcomes.21
This study is important because, to our knowledge, it reports the first evidence associating the occurrence of postoperative delirium to quantitative data on the patient centered outcome of decreased postoperative ambulation levels. One prior study found delirium to be a main risk factor for not regaining pre-injury mobility in a study of elderly patients who sustained hip fractures.22 A practical importance of this study’s finding is that the poor mental and physical outcomes reported may be modifiable. One in three cases of delirium are preventable by non- pharmacologic, supportive bedside interventions.23 These data suggest that proactive delirium prevention programs may provide a future avenue to explore with the goal of preserving ambulation as well as preventing delirium.
The main limitations of this study are twofold. First, the study population is predominately male. This proportion represents the demographic of a Veterans Affairs Medical Center and not selection bias. However, the predominately male cohort limits generalizability of the findings to female populations. Second, this study’s postoperative follow-up to 28 days did not allow for full recovery to baseline ambulation levels in both the patients with and without delirium. This limitation does not allow our study to determine if full recovery to preoperative baseline ambulation levels is achieved in both groups.
Conclusion:
Postoperative delirium in older adults is associated with delayed return of preoperative baseline ambulation levels. Patient with delirium recover only one third of their baseline preoperative ambulation level at 28-days following major operations. The finding of decreased baseline preoperative ambulation was not present immediately postoperatively but occurred after the development of postoperative delirium. Given that one third of hospitalized delirium is preventable using non-invasive bedside supportive care protocols, delirium prevention strategies become increasingly important given the potential to not only preserve mental function, but also to preserve physical function. Future studies are necessary to determine if postoperative delirium is causal in the pathway of decreased ambulation and if proactive physical therapy efforts in patient who develop postoperative delirium will mitigate decreased ambulation following major operations.
Highlights.
Older patients with delirium recover only one-third of their baseline preoperative steps one- month postoperatively.
Older adults with postoperative delirium have a decreased recovery towards baseline ambulation for 4 weeks following inpatient operations in comparison to non-delirious patients.
The decrease in ambulation is similar in the delirium and no delirium groups immediately after the operation and the step recovery trajectories begin to differ after the development of delirium occurs.
This study is unique in that it quantifies the patient centered outcome of walking (steps/day) in a large group of older adults undergoing major operations.
This study quantifies the deleterious inter-relationship of two cornerstone patient-centered outcomes (mental and physical function).
Financial Support:
National Institute on Aging Network for Investigation of Delirium: Unifying Scientists (R24AG054259) (Robinson); Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) Education and Research Foundation Grant (Carmichael, Robinson); Eastern Colorado VA Geriatric Research Education and Clinical Center (GRECC) (Jones)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure: The authors have no conflict of interest to report.
References
- 1.Marcantonio ER, Juarez G, Goldman L, et al. The relationship of postoperative delirium with psychoactive medications. JAMA. 1994;272(19):1518–1522. [PubMed] [Google Scholar]
- 2.Marcantonio ER. Postoperative delirium: a 76-year-old woman with delirium following surgery. JAMA. 2012;308(1):73–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Robinson TN, Raeburn CD, Tran ZV, Angles EM, Brenner LA, Moss M. Postoperative delirium in the elderly: risk factors and outcomes. Ann Surg. 2009;249(1):173–178. [DOI] [PubMed] [Google Scholar]
- 4.Inouye SK, Bogardus ST Jr., Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340(9):669–676. [DOI] [PubMed] [Google Scholar]
- 5.Bureau USC. 2017 National Population Projections Tables: Main Series. https://www.census.gov/data/tables/2017/demo/popproj/2017-summary-tables.html. Published 2017. Updated 2/20/2020. Accessed 5/18/2020.
- 6.Appelboom G, Yang AH, Christophe BR, et al. The promise of wearable activity sensors to define patient recovery. J Clin Neurosci. 2014;21(7):1089–1093. [DOI] [PubMed] [Google Scholar]
- 7.Beswick AD, Rees K, Dieppe P, et al. Complex interventions to improve physical function and maintain independent living in elderly people: a systematic review and meta-analysis. Lancet. 2008;371(9614):725–735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Karlsson E, Franzen E, Nygren-Bonnier M, Bergenmar M, Rydwik E. Short-term postoperative physical decline and patient-reported recovery in people aged 70 or older undergoing abdominal cancer resection- A prospective cohort study. J Geriatr Oncol. 2019;10(4):610–617. [DOI] [PubMed] [Google Scholar]
- 9.Carmichael H, Overbey DM, Hosokawa P, et al. Wearable Technology-A Pilot Study to Define “Normal” Postoperative Recovery Trajectories. J Surg Res. 2019;244:368–373. [DOI] [PubMed] [Google Scholar]
- 10.Hochsmann C, Knaier R, Eymann J, Hintermann J, Infanger D, Schmidt-Trucksass A. Validity of activity trackers, smartphones, and phone applications to measure steps in various walking conditions. Scand J Med Sci Sports. 2018;28(7):1818–1827. [DOI] [PubMed] [Google Scholar]
- 11.Ely EW, Margolin R, Francis J, et al. Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit Care Med. 2001;29(7):1370–1379. [DOI] [PubMed] [Google Scholar]
- 12.Pisani MA, Araujo KL, Van Ness PH, Zhang Y, Ely EW, Inouye SK. A research algorithm to improve detection of delirium in the intensive care unit. Crit Care. 2006;10(4):R121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. [DOI] [PubMed] [Google Scholar]
- 14.Doyle DJ, Goyal A, Bansal P, Garmon EH. American Society of Anesthesiologists Classification (ASA Class). In: StatPearls. Treasure Island (FL)2020. [Google Scholar]
- 15.Borson S, Scanlan JM, Chen P, Ganguli M. The Mini-Cog as a screen for dementia: validation in a population-based sample. J Am Geriatr Soc. 2003;51(10):1451–1454. [DOI] [PubMed] [Google Scholar]
- 16.Robinson TN, Wu DS, Pointer L, Dunn CL, Cleveland JC Jr., Moss M. Simple frailty score predicts postoperative complications across surgical specialties. Am J Surg. 2013;206(4):544–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khuri SF, Daley J, Henderson W, et al. The Department of Veterans Affairs’ NSQIP: the first national, validated, outcome-based, risk-adjusted, and peer-controlled program for the measurement and enhancement of the quality of surgical care. National VA Surgical Quality Improvement Program. Ann Surg. 1998;228(4):491–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.R: A language and environment for statistical computing. [computer program]. Vienna, Austria: R Foundation for Statistical Computing; 2017. [Google Scholar]
- 19.Stephens S, Beyene J, Tremblay MS, Faulkner G, Pullnayegum E, Feldman BM. Strategies for Dealing with Missing Accelerometer Data. Rheum Dis Clin North Am. 2018;44(2):317–326. [DOI] [PubMed] [Google Scholar]
- 20.Berian JR, Zhou L, Russell MM, et al. Postoperative Delirium as a Target for Surgical Quality Improvement. Ann Surg. 2018;268(1):93–99. [DOI] [PubMed] [Google Scholar]
- 21.Fried TR, Bradley EH, Towle VR, Allore H. Understanding the treatment preferences of seriously ill patients. N Engl J Med. 2002;346(14):1061–1066. [DOI] [PubMed] [Google Scholar]
- 22.Vochteloo AJ, Moerman S, Tuinebreijer WE, et al. More than half of hip fracture patients do not regain mobility in the first postoperative year. Geriatr Gerontol Int. 2013;13(2):334–341. [DOI] [PubMed] [Google Scholar]
- 23.American Geriatrics Society Expert Panel on Postoperative Delirium in Older A. American Geriatrics Society abstracted clinical practice guideline for postoperative delirium in older adults. J Am Geriatr Soc. 2015;63(1):142–150. [DOI] [PMC free article] [PubMed] [Google Scholar]


