Abstract
Objectives
The objective of this study was to assess the performance of models of primary healthcare (PHC) delivered in First Nation and adjacent communities in Manitoba, using hospitalization rates for ambulatory care sensitive conditions (ACSC) as the primary outcome.
Methods
We used generalized estimating equation logistic regression on administrative claims data for 63 First Nations communities from Manitoba (1986–2016) comprising 140,111 people, housed at the Manitoba Centre for Health Policy. We controlled for age, sex, and socio-economic status to describe the relationship between hospitalization rates for ACSC and models of PHC in First Nation communities.
Results
Hospitalization rates for acute, chronic, vaccine-preventable, and mental health-related ACSCs have decreased over time in First Nation communities, yet remain significantly higher in First Nations and remote non-First Nations communities as compared with other Manitobans. When comparing different models of care, hospitalization rates were historically higher in communities served by health centres/offices, whether or not supplemented by itinerant medical services. These rates have significantly declined over the past two decades.
Conclusion
Local access to a broader complement of PHC services is associated with lower rates of avoidable hospitalization in First Nation communities. The lack of these services in many First Nation communities demonstrates the failure of the current Canadian healthcare system to meet the need of First Nation peoples. Improving access to PHC in all 63 First Nation communities can be expected to result in a reduction in ACSC hospitalization rates and reduce healthcare cost.
Keywords: Indigenous health, Primary care, Avoidable hospitalization, Nursing stations, Rural and remote communities
Résumé
Objectifs
L’objectif de cette étude était d’évaluer le rendement des modèles de soins de santé primaires (SSP) dispensés dans les Premières Nations et les communautés adjacentes du Manitoba, en utilisant les taux d’hospitalisation pour les conditions propices aux soins ambulatoires (CPSA) comme résultat principal.
Méthodes
Nous avons utilisé une régression logistique par équation d’estimation généralisée sur les données de réclamations administratives pour 63 communautés des Premières Nations du Manitoba (1986-2016) comprenant 140 111 personnes, hébergées au Manitoba Centre for Health Policy. Nous avons contrôlé l’âge, le sexe et le statut socioéconomique afin de décrire la relation entre les taux d’hospitalisation pour les CPSA et les modèles de soins de santé primaires dans les communautés des Premières Nations.
Résultats
Les taux d’hospitalisation pour les CPSA aigus, chroniques, évitables par la vaccination et liés à la santé mentale ont diminué au fil du temps dans les communautés des Premières Nations, mais demeurent considérablement plus élevés dans les communautés des Premières Nations et éloignées non des Premières Nations par rapport aux autres Manitobains. Lorsque l’on compare différents modèles de soins, les taux d’hospitalisation étaient historiquement plus élevés dans les communautés desservies par les centres/bureaux de santé, qu’ils soient ou non complétés par des services médicaux itinérants. Ces taux ont considérablement diminué au cours des deux dernières décennies.
Conclusion
L’accès local à un éventail plus large de services de SSP est associé à des taux plus faibles d’hospitalisation évitable dans les collectivités des Premières Nations. Le manque de ces services dans de nombreuses collectivités des Premières nations démontre l’incapacité du système de santé canadien actuel à répondre aux besoins des peuples des Premières nations. On peut s’attendre à ce que l’amélioration de l’accès aux soins de santé primaires dans les 63 collectivités des Premières nations se traduise par une réduction des taux d’hospitalisation et des coûts des soins de santé.
Mots-clés: Santé autochtone, santé primaire, hospitalisation évitable, postes de soins infirmiers, collectivités rurales et éloignées
Introduction
Primary healthcare (PHC) is a fundamental part of any country’s healthcare system (Starfield et al. 2005). The ideal goals of PHC are to preserve and protect people’s health; prevent the spread of infectious diseases; treat acute episodes of illness in a timely manner; and manage chronic conditions (Health Council of Canada 2005). In the context of First Nation peoples, these goals can only be achieved by: addressing the legacy of colonialism, residential schools, segregated hospitals, and destructive policies (Duff et al. 2014; Lux 2016; Truth and Reconciliation Commission of Canada 2015) which resulted in the disruption of social cohesion and intergenerational knowledge transmission (Wesley-Esquimaux and Smolewski 2004); addressing racism (Browne and Varcoe 2006; Provincial Court of Manitoba 2014); reducing social exclusion; and ensuring access to responsive, respectful and effective healthcare services (Ford-Gilboe et al. 2018; Lavoie et al. 2019). Manitoba First Nations have clearly stated that mental health and well-being must be an integral part of all care, including PHC (Kyoon-Achan et al. 2018).
This is a monumental task: federal and provincial governments engaged with distinct parts of the complex multi-jurisdictional system funding and delivering community-based PHC in First Nation communities have to date failed to clearly outline the explicit responsibility of each level of government in ensuring equitable and responsive access to adequate healthcare services (Lavoie 2013). What exists today, despite 50 years of discussions (Booz•Allen and Hamilton Canada Ltd. 1969), is a patchwork approach to service delivery, where debates over responsibility remain ever present, undermining timeliness, comprehensiveness, and continuity of care (Lavoie et al. 2015; Provincial Court of Manitoba 2014; The Jordan’s Principle Working Group 2015). This results in premature mortality and preventable loss of quality of life.
Indigenous peoples represent approximately 5% of the total Canadian population (Statistics Canada 2016). Overall, 60% of the total Indigenous population identify as First Nation peoples. Compared with other provinces, Manitoba has the largest proportion of Indigenous peoples (18%). Manitoba and Saskatchewan are home to the highest percentage of First Nation peoples living on reserve (Turner et al. 2013). Previous studies have reported higher rates of potentially avoidable hospitalizations, poorer health outcomes and shorter life expectancy among First Nation peoples as compared with other Canadians (Green et al. 2013; Lavoie et al. 2010; Lyons et al. 2014; Ospina et al. 2015; Riediger et al. 2015), indicating a strong need for health system transformation (Lavoie 2013). Nevertheless, little progress has been made in closing the health equity gap that exists between First Nation peoples and other residents of Canada. The profound negative effects of colonization, residential schools, racism, and other social determinants of ill health have played a very important role in the poor health status of this population, and continue to undermine efforts to improve the health status of First Nation peoples (Hackett et al. 2016; Martens et al. 2005). This inequity in health is of huge concern (Lavoie 2013; Lavoie et al. 2007).
Tinkering with the current system is however unlikely to produce significant health improvements for Indigenous peoples. The past decades of conceptual work and research on determinants of health have shown that healthcare’s contribution to health, while important, is limited (Lalonde 1974; Marmot and Wilkinson 2006). While healthcare can contribute to the restoration of health in individuals, and to the prevention of disease through population-level interventions, it can only mitigate the negative impact of poverty, stress related to a lack of control over one’s life, social exclusion, challenging circumstances in early life, unemployment, stressed and stretched social supports, food insecurities, and sedentary lifestyle (Wilkinson and Marmot 2003). To this list, Indigenous scholars have added the continued devastating impact of colonialism on economic and food systems, access to land and medicines, and the transmission of health and wellness-promoting knowledge and practices through teachings and ceremonies, and the undermining of social cohesion and kinship systems (Greenwood et al. 2015). Thus, a fundamental, wellness-oriented shift is needed, one that addresses Indigenous determinants of health, including:
The provision of PHC to include traditional healing modalities, wellness and mental health programs (Kyoon-Achan et al. 2018), and behavioural health consultants (Dale and Lee 2016; Gottlieb 2013; Southcentral Foundation 2019);
Better continuity of care throughout the system, and across jurisdictions (Katz et al. 2017; Lavoie 2013);
Guarantees a right to equitable access to responsive and culturally appropriate care that honours individual and community self-determination (United Nations 2007; United Nations Human Right Council 2007).
While recognizing the limited role of healthcare service provision in determining the health of the population, it is still important to understand the relative merits of models of care delivery. The objective of this study was to assess the performance and shortcomings of existing models of PHC currently delivered in First Nation communities in Manitoba, using hospital admission rates (hereafter hospitalization) for ambulatory care sensitive conditions (ACSC, which include acute, chronic, vaccine-preventable, and mental health ACSC) as the primary outcome indicator. We have shown elsewhere that hospitalization for ACSC, when used in conjunction with premature mortality rates (PMR), can provide a more dependable measure of the performance of the PHC models in rural and remote communities (Lavoie et al. 2019).
Hospitalization rates for ambulatory care sensitive conditions (hACSC) have been widely used as a measure of PHC performance and as an indicator of access to PHC (Ansari et al. 2006; Campbell et al. 2014; Correa-Velez et al. 2007; Erny-Albrecht et al. 2016; Gibson et al. 2013; Lavoie et al. 2010, 2011, 2018, 2019). ACSC are conditions for which hospital admissions could potentially be reduced or avoided with timely, effective, and accessible PHC (Billings et al. 1993; Erny-Albrecht et al. 2016). For example, admissions for asthma are potentially preventable with effective and timely management, which can be provided through PHC. While not all hospitalizations might be preventable, a disproportionate rate of hospitalization for asthma would suggest a need to strengthen outpatient asthma management. In Australia, hospitalization for these conditions is higher for Indigenous peoples, for rural and remote residents, and for socio-economically disadvantaged people (Erny-Albrecht et al. 2016). In Canada, we have demonstrated that communities with better local access to PHC have lower rates of hACSC (Lavoie et al. 2011; Lavoie et al. 2010; Lavoie et al. 2018; Lavoie et al. 2019). Nevertheless, more research on the performance of different models of PHC in Manitoba First Nation communities is needed.
Models of service delivery in First Nation communities
The communities compared in this paper are 63 First Nation communities whose population ranges from 38 residents to 6120 (2017 figures), with an average of 1457 residents. As shown in Table 1, these communities are served through a number of different models and arrangements. Existing models of PHC in First Nation, rural, and remote communities vary considerably, predominantly based on historical decisions grounded in convenience and the circumstances of the time (as is the case for the 1964 Agreement, which made three First Nation communities the responsibility of the provincial government, without consultations; see Lavoie et al. 2010 for more details), pragmatic considerations often gauged from a southern-urban perspective, ability to recruit and retain professionals, and other contextual factors.
Table 1.
Model of PHC available on-reserve
| Model of PHC available on-reserve | Number of communities | Population (2017) |
|---|---|---|
| Federally funded nursing station, supplemented by primary care provided by Ongomiizwin Health Services | 9 | 2083 |
| Federally funded nursing station only | 13 | 22,952 |
| Federally funded health centre or health office, supplemented by primary care provided by Ongomiizwin Health Services | 3 | 511 |
| Federally funded health centre or health office only | 38 | 64,815 |
| Total | 63 | 90,361 |
Ongomiizwin Health Services (OHS, formerly known as the J.A. Hildes Northern Medical Unit) has been delivering services to Manitoba First Nations and Inuit communities of Nunavut’s Kivalliq region for nearly 50 years. Historically, services focused primarily on visiting family physicians and specialists. In the past decade, OHS’ services have expanded to include nursing, occupational and physiotherapy, footcare, and dialysis nursing (in certain communities). Considerable work has been done to ensure that the models of care are responsive to local Indigenous cultures. In 2017, OHS became part of the University of Manitoba’s Indigenous Institute of Health and Healing.
OHS services are delivered primarily on-reserve in partnership with local services. Some First Nation communities (those larger and more isolated) have local access to services through a federally funded Nursing Station, where federally employed nurses working with an expanded scope of practice provide some level of primary care, and where other community-based services (primary prevention, health promotion) are provided by community-employed staff (community health nurses, community-based and defined roles such as Elders workers, community health representatives, addiction prevention workers, etc.). In those communities, OHS supports and supplements the local primary care services.
OHS also offers services in communities served by a health centre or health office. These communities are generally non- or semi-isolated (located within 50 km or 150 km of the nearest community with a family practice, respectively). These communities do not have local primary care capacity, and focus entirely on primary and secondary prevention activities. Primary care is provided by OHS’ visiting family physicians.
In communities OHS providers do not visit, residents must travel to the nearest provincial point of care to access a family physician. There, providers funded through the provincial government and serving the general Manitoba population provide primary care services at no charge to the patient. While theoretically seamless, this expectation is far from ideal. A number of communities not served by OHS are fly-in and fly-out only. Others depend on seasonal roads, open through the winter only. Others still are located at a 2–5-h drive from the nearest point of care, with a considerable portion of the travel being on gravel roads and no access to public transportation. We acknowledge that traveling family physician services are also provided by two other organizations. The approach is however more akin to services provided by family physicians in the rest of the province, with a focus on one-on-one patient care without a similar commitment to the development of alternative models of care, developed in partnership with the community.
OHS’ model of service delivery reflects financial, organizational, and systemic constraints imposed by the funder of these services (Health Canada). Although innovations are happening, the scope of these innovations remains within the jurisdictionally fragmented existing system. Human resources remain insufficient to meet healthcare needs, resulting in high rates of referrals to services outside the community. The context described above is not unique to Manitoba: this reflects the complexities of delivering care to rural and remote communities across Canada, where relatively small communities are distributed across vast largely unpopulated territories. Similar circumstances exist in Australia, Greenland, Norway, Alaska, and other higher income countries as well. This paper purposely focuses on models of care delivery in smaller Indigenous rural and remote communities. To date, the literature on models of PHC delivery has been informed by urban-centric research. This is therefore an important gap which we intend to address.
In this paper, we propose that the currently available models of healthcare in First Nations and in rural and remote communities in Manitoba are not yet able to meet the need of First Nations living in these communities, and a fundamental restructuring of community-based PHC services in First Nation communities is needed to produce equitable health outcomes in these communities.
Methods
The Innovation in Community-based Primary Health Care (CBPHC) Supporting Transformation in the Health of First Nation and rural/remote communities in Manitoba (iPHIT) project is a 5-year partnership between university-based researchers from the University of Manitoba, the First Nations Health and Social Secretariat of Manitoba (hereafter, FNHSSM), and eight First Nation communities in Manitoba, from non-isolated to remote communities, and served by health offices, health centres, or nursing stations. The overall objective of this innovative, strength-based program of research is to expand our knowledge of various models of PHC in rural, remote, and First Nation communities, and to learn from First Nation and rural and remote communities who have developed effective community-based PHC. The project was pursued following ethical principles outlined in the Manitoba First Nations Education Resource Centre Inc.’s guiding document outlining its ethical principles (Manitoba First Nations Education Resource Centre Inc. 2014), which includes OCAP principles (National Aboriginal Health Organization 2007) and goes beyond minimal provisions outlined in the Tri-Council guidelines (Canadian Institutes of Health Research, Natural Sciences and Engineering Research Council of Canada, and Social Sciences and Humanities Research Council of Canada 2014).
Source of data
We used administrative health data (1986–2016) from the Manitoba Population Research Data Repository housed at the Manitoba Centre for Health Policy, University of Manitoba. The Repository is a comprehensive collection of administrative, registry, survey, and other data that includes the vast majority of residents of Manitoba, including residents of First Nations’ communities. The data used for this study included vital statistics files, the population health registry file, the hospital discharge abstracts, and census data files. The study included all Manitoba residents eligible to receive health benefits under the Manitoba Health Services Insurance Plan and living on 63 First Nation reserves, rural and remote communities, or urban Manitoba (Winnipeg and Brandon). Six-digit postal codes were used to identify the population served in each community. Registered members of First Nations represent 96.6% of the overall on-reserve population, others are non-status, Métis, or non-Indigenous individuals who depend on the same services (Lavoie et al. 2010).
Our main dependent variables include premature mortality rates (PMR) and hospitalization for ACSC (hACSC). We used our previously created definition for ACSC (Lavoie et al. 2010), based on the definition created by the Canadian Institute for Health Information (2007, 2008) and by the Victorian Government Department of Human Resources division (Ansari et al. 2006). Following input from First Nations communities who see addressing mental health needs as an integral part of PHC services (Kyoon-Achan et al. 2019), we added two mental health-related conditions. Our final definition included a total of 29 ACSC defined using 3-, 4-, and 5-digit International Statistical Classification of Disease codes (ICD-9-CM and ICD-10-CM) (Table 2). We used hACSC adjusted by age, sex, and socio-economic status (SES) to allow cross-sectional and longitudinal comparisons of hospitalization rates among communities. Our main independent variables were community types and models of care as defined in Table 1. We classified First Nation communities in Manitoba based on the level of care outlined in the same table.
Table 2.
Categories of ACSC explored in this study
| Categories of ACSC | Conditions |
|---|---|
| Chronic conditions | Asthma; angina; diabetes with complications; hypertension; acute bronchitis; chronic obstructive pulmonary disease (COPD); pneumonia; epilepsy; heart failure and pulmonary edema; iron deficiency anemia |
| Acute conditions | Dental conditions; cellulitis; severe ear, nose, and throat infections (ENT) |
| Vaccine-preventable conditions | Hepatitis A and B; influenza; hemophilic influenza; measles; mumps; rubella; meningitis; tuberculosis; tetanus; rubella; poliomyelitis; pertussis |
| Mental health-related conditions | Mood disorders; schizophrenia |
| All ACSC | All conditions combined |
*ICD codes are provided in Appendix 1 for reproducibility
In this study, we defined First Nation communities as those recognized as Indian Reserves under the Indian Act (Government of Canada 1985). While narrow, we justify using this definition because we are concerned with researching models of PHC that emerge as a result of federal policies, and First Nation advocacy and innovations. Rural and remote communities proved somewhat more difficult to define. There is no single, universally accepted definition of concepts such as rural and remote. Most definitions generally focus on geography, population density, or access to services such as healthcare. The “right” definition is context dependent. For the purpose of this study, we included under the rubric “rural and remote communities” all Manitoba communities with a population of less than 8000 (n = 183), as all Manitoba First Nation communities have fewer than 8000 residents. We are less concerned with attributing a “rural” or “remote” label to specific communities and instead focused on exploring local access to community-based PHC and community characteristics that can be linked to better outcomes. The study population included all individuals living in First Nation communities.
The study received ethics approval from the University of Manitoba Health Research Ethics Board and data access approval from the Government of Manitoba Health Information Privacy Committee and the Health Information Research Governance Committee of First Nations Health Social Secretariat of Manitoba.
Data analysis
Data were analyzed using generalized estimating equation (GEE) models, controlling for age, sex, and SES (income quantiles, weighted average using postal codes as an ecological measure using the census data), to identify trends (change over time from 1986 to 2016) and differences in hACSC. GEE models were also used to determine the relationship between hospitalization rates for ACSC and models of PHC in First Nation communities to explore whether the rate of hospitalization for ACSC differed by the model of care available in the community. We analyzed the data using 5-year rolling average rates to attenuate the impact of yearly variations often found in small sample sizes, and highlight trends.
Results
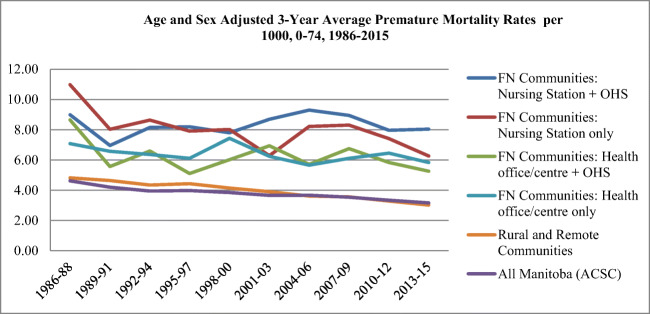
Our analysis (Table 3 and Fig. 1) shows that the PMR was historically highest in communities serviced by nursing stations (with and without OHS). We were able to detect a statistically significant decline in PMR only in communities served by nursing stations (% change 3.47, p = 0.002) and by health offices/health centres (HO/HC; % change 1.50, p = 0.009). The PMR in all First Nation communities under study remains considerably higher than that of Manitoba communities, whether rural, remote, or urban.
Table 3.
Age- and sex-adjusted premature mortality rates per models of care, 1986–2014, per 1000, ages 0–74, 5-year rolling averages
| PHC services serving these communities | PMR 1986–1988 (Adj lower and upper CI) | PMR 2012–15 (Adj lower and upper CI) | % change and direction, 1986–2014 | P value |
|---|---|---|---|---|
| FN NS + OHS | 8.99 (7.13–11.34) | 8.04 (6.96–9.29) | 0.39, ↑ | 0.6627 |
| FN NS | 10.97 (8.61–13.99) | 6.26 (5.21–7.53) | 3.47, ↓ | 0.0002* |
| FN HO/HC + OHS | 8.64 (5.96–12.53) | 5.26 (3.87–7.13) | 2.27, ↓ | 0.3293 |
| FN HO/HC | 7.07 (5.91–8.46) | 5.83 (5.08–6.69) | 1.50, ↓ | 0.0093* |
| Rural and remote | 4.82 (4.20–5.53) | 3.01(2.72–3.34) | 4.88, ↓ | < 0.0001* |
| All Manitoba (ACSC) | 4.62 (4.06–5.25) | 3.16 (3.11–3.22) | 3.49, ↓ | < 0.0001* |
PHC primary health care, PMR premature mortality rate, CI confidence interval, FN First Nations, NS nursing station, OHS Ongomiizwin Health Services, HO/HC health office/health centre
Fig. 1.
Age- and sex-adjusted 3-year average premature mortality rates per 1000, 0–74, 1986–2015
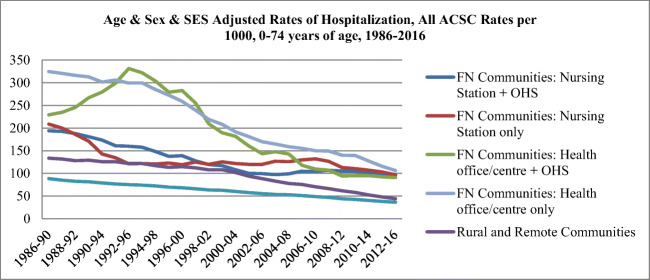
As shown in Table 4 and Fig. 2, the hospitalization rates for all ACSC have been declining over time in First Nation and other communities across Manitoba. The rate of decline was higher in communities where rates were historically higher (First Nations communities served by health centres and health offices with or without OHS). First Nation communities had significantly higher rates of hospitalization for all ACSC compared with rural communities that are also considered rural and remote, and all Manitoba (p < 0.000). While the gap has narrowed, it remains significant.
Table 4.
5-year rolling rates of hospitalization for ACSC adjusted by age, sex, and SES, 1986–2016
| PHC services serving these communities | Ambulatory care sensitive conditions, by categories, % change between 1986 and 2016 (P value) | |||||
|---|---|---|---|---|---|---|
| ALL ACSC | Acute | Chronic | Vaccine-preventable | Mental health | ||
| First Nation communities | Nursing stations, supplemented by OHS services | − 2.85 (< 0.0001) | − 6.15 (< 0.0001) | − 2.48 (< 0.0001) | − 3.53 (0.0002) | 5.34 (< 0.0001) |
| Nursing stations only | − 1.82 (0.0008) | − 5.49 (< 0.0001) | − 2.50 (0.0011) | 0.82 (0.3252) | 5.97 (< 0.0001) | |
| Health centres or health offices, supplemented by OHS services | − 5.15 (< 0.0001) | − 7.14 (< 0.0001) | − 3.71 (< 0.0001) | − 11.78 (< 0.0001) | − 0.73 (0.6146) | |
| Health centres or health offices only | − 4.37 (< 0.0001) | − 6.28 (< 0.0001) | − 2.86 (< 0.0001) | − 7.62 (< 0.0001) | 1.48 (0.0204) | |
| Rural and remote communities | − 3.90 (< 0.0001) | − 4.85 (< 0.0001) | − 3.61 (< 0.0001) | − 7.97 (< 0.0001) | − 0.74 (0.0171) | |
| All Manitoba (ACSC) | − 3.18 (< 0.0001) | − 4.34 (< 0.0001) | − 3.86 (< 0.0001) | − 6.48 (< 0.0001) | − 0.33 (0.7499) | |
* show statistically significant results
Fig. 2.
Age- and sex- and SES-adjusted rates of hospitalization, all ACSC rates per 1000, 0–74 years of age, 1986–2016
Hospitalization rates for chronic, acute, and vaccine-preventable ACSC have been declining over time in all communities (p < 0.000). Nevertheless, First Nation peoples living in First Nation communities had significantly higher hospitalization rates for acute, chronic, and vaccine-preventable ACSC (p < 0.000). Communities served by OHS (nursing stations with and without OHS; health centres/offices with and without OHS) showed a high rate of decline in hospitalizations for all ACSC, acute, chronic, and vaccine-preventable conditions. The difference in the slope was not sufficiently pronounced to be statistically significant (see Table 5).
Table 5.
Comparison of adjusted rates hACSC between on-reserve models of care
| FN communities served by | Is the slope significantly different from FN communities served by | P-value | |||
|---|---|---|---|---|---|
| All ACSC | Nursing station | OHS | Nursing station | 0.1748** | |
| Health centre/office | OHS | Health centre/office | 0.2398** | ||
| Nursing station | OHS | Health centre/office | OHS | 0.0030* | |
| Nursing station | Health centre/office | OHS | < 0.0001* | ||
| Nursing station | Health centre/office | < 0.0001* | |||
| Chronic ACSC | Nursing station | OHS | Nursing station | 0.9838** | |
| Health centre/office | OHS | Health centre/office | 0.3011** | ||
| Nursing station | OHS | Health centre/office | OHS | 0.1882** | |
| Nursing station | Health centre/office | OHS | 0.2532** | ||
| Nursing station | Health centre/office | 0.6603** | |||
| Acute ACSC | Nursing station | OHS | Nursing station | 0.3903** | |
| Health centre/office | OHS | Health centre/office | 0.3037** | ||
| Nursing station | OHS | Health centre/office | OHS | 0.2811** | |
| Nursing station | Health centre/office | OHS | 0.0523** | ||
| Nursing station | Health centre/office | 0.2404** | |||
| Vaccine-preventable ACSC | Nursing station | OHS | Nursing station | 0.0004* | |
| Health centre/office | OHS | Health centre/office | 0.0004* | ||
| Nursing station | OHS | Health centre/office | OHS | < 0.0001* | |
| Nursing station | Health centre/office | OHS | < 0.0001* | ||
| Nursing station | Health centre/office | < 0.0001* | |||
| Mental health ACSC | Nursing station | OHS | Nursing station | 0.6410** | |
| Health centre/office | OHS | Health centre/office | 0.1646** | ||
| Nursing station | OHS | Health centre/office | OHS | 0.0005* | |
| Nursing station | Health centre/office | OHS | 0.0001* | ||
| Nursing station | Health centre/office | < 0.0001* | |||
* show statistically significant results
hACSC Hospitalization rates for ambulatory care sensitive conditions
In contrast, we note that hospitalizations for mental health ACSC are increasing in all First Nation communities, with the exception of those served by health centres or health offices, supplemented by OHS services, where results were not statistically significant. For those communities, we surmise that the small sample size is likely a factor, making the trend undetectable.
In addition, we looked more closely at the impact of additional primary care resources as provided by OHS on First Nations’ health outcomes. As shown in Table 5, nursing stations and health centres/offices accessing supplemental services from OHS showed no statistically significant difference in hACSC (all ACSC) when compared with communities served by nursing stations and health centres/offices alone. Differences were however significant when comparing nursing stations to health centres/offices whether served by OHS (p = 0.03) or not (p < 0.000). We noted no statistically significant differences for chronic or acute hACSC. We did find that communities with a more comprehensive model of care consistently showed lower vaccine-preventable hACSC. Patterns were somewhat less clear for mental health ACSC.
Discussion
The objective of this study was to describe the trends in hospitalization rates for ACSC in First Nation communities and in rural and remote communities compared with those in all Manitoba, to inform health system transformation. We also explored the relationship between models of care in First Nation communities and the hospitalization rates for ACSC (acute, chronic, vaccine-preventable, mental health, and all combined) in these communities.
Our results show that the addition of services provided by OHS has not yet resulted in a detectable decline in PMR. It has however resulted in slight differences in rates of hACSC, suggesting that the addition of primary healthcare resources in First Nations has a positive impact on outcomes (preventable hospitalizations) and that causes of mortality may primarily be non-ACSC related (Martens et al. 2002). It is crucial not to ignore the role of Indigenous determinants of health in relation to PMR. Our results suggest that there is a positive impact to enhancing the PHC system in First Nation communities, and a need to also address other factors, including self-determination, social justice, poverty, housing, food insecurity, smoking, and other social determinants of health.
The remaining gap that exists between First Nations and other Manitoba communities, as evidenced by rates of hospitalizations for ACSC, also suggests that the current level of care remains insufficient compared to need, a finding consistent with previous studies (Martens et al. 2002). We argue that a wellness-oriented model of care is required, and that the implementation of this model requires addressing systemic barriers to the provision of primary healthcare to address determinants of wellness (behavioural and mental health programs and continuity of care throughout the system, and across jurisdictions). Our results echo the findings from our previous Manitoba study in which we demonstrated that “for First Nations communities, local access to a broader complement of PHC services was associated with lower hospitalization rates for ACSC” (Lavoie et al. 2010, p. 721). The current study is more comprehensive, and included other models of PHC (OHS).
This study has many strengths; first, the use of administrative data allows us to study the whole population rather than a sample which may introduce bias. This allowed us to run several GEE models and to run separate analyses on acute, chronic, and vaccine-preventable ACSCs, and detect variations between different types of communities served by different models of care. We acknowledge that the current study has some limitations. First, the administrative data in the Repository do not provide information on factors such as the quality of care in the community, delays in diagnosis, and medical transportation issues in the communities that are likely to impact ACSC hospitalization rates. However, there is no reason to suggest that there is a systematic bias in the distribution of these factors between models of PHC delivery. Second, the models of care stated in the analysis do not fully reflect that some First Nation communities have adapted the models of care provided to meet their own needs. For example, our analyses do not include community-based programs that are developed locally and available in any of the First Nation communities and whether there are more, or more effective, local programs in First Nations served by nursing stations. Third, a lack of consistency in the definition and use of ACSC across studies might affect the comparability of our results with those of other studies. Fourth, we identified First Nations’ community of residence using 6-digit postal codes, and included all residents as if all were First Nations. We are aware that our approach includes Metis, non-registered First Nations, and non-Indigenous people, but approximately 96% of the total on-reserve population are registered First Nations. Furthermore, the focus of this study is on local access to care, and all who live on-reserve depend on the same services (Lavoie et al. 2010). Finally, we acknowledge that the communities included in this study are small, and that this impacts statistically detectable results. We mitigated this by aggregating communities by models of care, and by using 5-year rolling average rates with data that span 30 years. This is the best evidence available to date, and our analyses produced important results. These nevertheless are associations, and should be interpreted with caution.
Conclusion
This study has confirmed the previously described relationship between PHC services in First Nation communities and the poor health outcomes in these communities. The use of ACSC hospital admission rates has supported a population-based assessment of the different models of PHC provision demonstrating the benefit of the more comprehensive PHC services. Not unexpectedly, even communities served by nursing stations have hospitalization rates that are higher than the rates in Manitoba, likely associated with Indigenous determinants of health. The currently available healthcare services are not meeting the needs of the First Nations people and a review of the current approach to the health of First Nations communities is urgently needed.
Appendix
Table 6.
ICD codes used to define ambulatory care sensitive conditions
| Category | Condition | ICD-9-Codes |
|---|---|---|
| Chronic conditions | Asthma | ICD-9-CM 493; ICD-10-CA J45 |
| Angina | ICD-9-CM 411, 413; ICD-10-CA 120, 123.82, 124.0, 124.8,124.9 Excluding cases with the following surgical procedures**: ICD-9 01.01 – 86.99; CCI 1.^,2.^,5.^ (i.e., any procedure from CCI section 1, 2, 5) | |
| Heart failure and pulmonary edema | ICD-9-CM 428, 518.4; ICD-10-CA 150, J81, I11.0Excluding cases with the following surgical procedures**: ICD-9 36.01, 36.02, 36.05, 36.1, 37.5, 37.7; CCI 1.IJ.50, 1.IJ.57.GQ, 1.HZ.85, 1.IJ.76, 1.HB.53; 1.HD.53, 1.HZ.53, 1.HB.55, 1.HD.55, 1.HZ.55, 1.HB.54, 1.HD.54 | |
| Diabetes with complications | ICD-9-CM 250; ICD-10-CA E10, E11, E13, E14 | |
| Hypertension | ICD-9-CM 401, 402; ICD-10-CA I10.0, I10.1, I11 Excluding cases with the following surgical procedures**: ICD-9 36.01, 36.02, 36.05, 36.1, 37.5, 37.7; CCI 1.IJ.50, 1.IJ.57.GQ, 1.HZ.85, 1.IJ.76, 1HB.53; 1.HD.53, 1.HZ.53, 1.HB.55, 1.HD.55, 1.HZ.55, 1.HB.54, 1.HD.54 | |
| COPD | ICD-9-CM 491, 492, 494, 496; ICD-10-CA J41, J42, J43, J44, J47 | |
| Pneumonia | Pneumonia (only when a secondary diagnosis of COPD is present): ICD-9-CM 480, 481, 482, 483, 484, 485, 486; ICD-10-CA J12, J13, J14, J15, J16, J18*Exclude if secondary diagnosis of sickle cell anemia is present | |
| Bronchitis | Acute bronchitis (only when a secondary diagnosis of COPD is present): ICD-9-CM 466.0 ICD-10-CA J20 | |
| Vaccine-preventable conditions | Diphtheria | ICD-9-CM 032; ICD-10-CA A36 |
| Hemophilus influenza type B | ICD-9-CM 320.0; ICD-10-CA G00.0 | |
| Hepatitis A | ICD-9-CM 070.0, 070.1; ICD-10-CA B15 | |
| Hepatitis B | ICD-9-CM 070.2, 070.3; ICD-10-CA B16 | |
| Influenza | ICD-9-CM 487; ICD-10-CA J10, J11 | |
| Measles | ICD-9-CM 055; ICD-10-CA B05 | |
| Meningococcal disease (meningitis) | ICD-9-CM 036; ICD-10-CA A39 | |
| Mumps | ICD-9-CM 072; ICD-10-CA B26 | |
| Pertussis | ICD-9-CM 033; ICD-10-CA A37 | |
| Pneumococcal | ICD-9-CM 038.2, 041.2, 320.1, 567.1, 711.0, 481; ICD-10-CA G00.1, A40.3, J13 Note: “Chronic conditions” are given the priority in the hierarchy for code 481 or J13 (see Pneumonia, only when a secondary diagnosis of COPD is present). | |
| Poliomyelitis | ICD-9-CM 045; ICD-10-CA A80 | |
| Tuberculosis | ICD-9-CM 011 – 018; ICD-10-CA A15 – A19 | |
| Rubella | ICD-9-CM 056; ICD-10-CA B06 | |
| Tetanus | ICD-9-CM 037; ICD-10-CA A34, A35 | |
| Acute Conditions | Dental Conditions | ICD-9-CM 521, 522, 523, 525, 528; ICD-10-CA K02.0, K02.1, K02.2, K02.3, K02.4, K02.8, K02.9, K03.0, K03.1, K03.2, K03.3, K03.4, K03.5, K03.6, K03.7, K03.8, K03.9, K04.0, K04.1, K04.2, K04.3, K04.4, K04.5, K04.6, K04.7, K04.8, K04.9, K05.0, K05.1, K05.2, K05.3, K05.4, K05.5, K05.6, K06.0, K06.1, K06.2, K06.8, K06.9, K08.0, K08.1, K08.2, K08.3, K08.80, K08.81, K08.82, K08.83, K08.87, K08.88, K08.9, K09.8, K09.9, K12.0, K12.1, K12.2, K13.0, K13.1, K13.2, K13.3, K13.4, K13.5, K13.6, K13.7 |
| Cellulitis | ICD-9-CM 681, 682, 683, 686; ICD-10-CA, L03, L04, L08, L44.4, L88, L92.2, L98.0, L98.3 Excluding cases with the following surgical procedures except incision of skin and subcutaneous tissue where it is the only listed: ICD-9 01.01 – 86.99 (except 86.0 – 86.09) CCI 1.^,2.^,5.^ (i.e. any procedure from CCI section 1, 2, 5) (except 1.AX.53.LA-QK, 1.IS.53.HN-LF, 1.IS.53.LA-LF, 1.JU.53.GP-LG, 1.KR.53.LA-LF, 1.OA.53.LA-QK, 1.SY.53.LA-QK, 1.YA.35.HA-W1, 1.YA.35.HA-X4, 1.YA.52.HA, 1.YA.52.LA, 1.YA.55.DA-TP, 1.YA.55.LA-TP, 1.YA.56.LA, 1.YB.52.HA, 1.YB.52.LA, 1.YB.55.DA-TP, 1.YB.55.LA-TP, 1.YB.56.LA, 1.YF.35.HA-W1, 1.YF.35.HA-X4, 1.YF.52.HA, 1.YF.55.DA-TP, 1.YF.55.LA-TP, 1.YF.56.LA, 1.YG.52.HA, 1.YG.52.LA, 1.YG.55.DA-TP, 1.YG.55.LA-TP, 1.YG.56.LA, 1.YR.52.HA, 1.YR.52.LA, 1.YR.56.LA, 1.YS.35.HA-W1, 1.YS.35.HA-X4, 1.YS.52.HA, 1.YS.52.LA, 1.YS.55.DA-TP, 1.YS.55.LA-TP, 1.YS.56.LA, 1.YT.35.HA-W1, 1.YT.35.HA-X4, 1.YT.52.HA, 1.YT.52.LA, 1.YT.55.DA-TP, 1.YT.55.LA-TP, 1.YT.56.LA, 1.YU.52.HA, 1.YU.52.LA, 1.YU.55.DA-TP, 1.YU.55.LA-TP, 1.YU.56.LA, 1.YV.35.HA-W1, 1.YV.35.HA-X4, 1.YV.52.HA, 1.YV.52.LA, 1.YV.55.DA-TP, 1.YV.55.LA-TP, 1.YV.56.LA, 1.YW.52.HA, 1.YW.52.LA, 1.YW.55.DA-TP, 1.YW.55.LA-TP, 1.YW.56.LA, 1.YX.52.HA, 1.YX.52.HA-AV 1.YX.52.LA, 1.YX.56.LA, 1.YZ.35.HA-W1, 1.YZ.35.HA-X4, 1.YZ.52.HA, 1.YZ.52.LA, 1.YZ.55.DA-TP, 1.YZ.55.LA-TP, 1.YZ.56.LA | |
| Pelvic Inflammatory Disease | ICD-9-CM 614, ICD-10-CA, N70, N73, N99.4 Exclude males or cases with a hysterectomy procedures: ICD-9 68.3 – 68.89, CCI 1.RM.87, 1.RM.89, 1.RM.91, 5.CA.89.CK, 5.CA.89.DA, 5.CA.89.GB, 5.CA.89.WJ, 5.CA.89.WK | |
| Gastroenteritis & Dehydration | ICD-9-CM 558, 276.5; ICD-10-CA K52.2, K52.8, K52.9, E86 | |
| Severe Ear, Nose and Thoat (ENT) infections | ICD-9-CM 382, 462, 463, 465, 472.1; ICD-10-CA H66, J02, J03, J06, J31.2, H67 Exclude otitis media cases with a myringotomy procedure: ICD-9 20.01; CCI 1.DF.53.JA-TS | |
| Mental health | Mood disorders | ICD-9-CM 296.1-296.8, 300, 309 or 311; ICD-10-CA F31, F32, F33, F34.1, F38.0, F38.1, F41.2, F43.1, F43.2, F43.8, F53.0, F93.0 or with a diagnosis for an anxiety state, phobic disorders or obsessive-compulsive disorders: ICD-9-CM 300.0, 300.2, 300.3, 300.7; ICD-10-CA F40, F : ICD-9-CM 300; ICD-10-CA F32, F34.1, F40, F41, F42, F44, F45.0, F45.1, F45.2, F48, F68.0, or F99, F41.0, F41.1, F41.3, F41.8, F41.9, F42, F45.2 |
| Schizophrenia | ICD-9-CM 295 ICD-10-CA F20, F21, F23.2, F25 |
* “Secondary diagnosis” refers to a diagnosis other than most responsible; ** Code may be recorded in any position. Procedures coded as cancelled, previous and “abandoned after onset” are excluded
Compliance with ethical standards
The study received ethics approval from the University of Manitoba Health Research Ethics Board and data access approval from the Government of Manitoba Health Information Privacy Committee and the Health Information Research Governance Committee of First Nations Health Social Secretariat of Manitoba.
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Ansari Z, Laditka JN, Laditka SB. Access to health care and hospitalization for ambulatory care sensitive conditions. Med Care Res Rev. 2006;63(6):719–741. doi: 10.1177/1077558706293637. [DOI] [PubMed] [Google Scholar]
- Billings J, Zeitel L, Lukomnik J, Carey TS, Blank AE, Newman L. Impact of socioeconomic status on hospital use in New York City. Health Aff. 1993;12(1):162–173. doi: 10.1377/hlthaff.12.1.162. [DOI] [PubMed] [Google Scholar]
- Booz•Allen & Hamilton Canada Ltd. (1969). Study of health services for Canadian Indians. Ottawa: Booz•Allen & Hamilton Canada Ltd.
- Browne, A. J., & Varcoe, C. (2006). Critical cultural perspectives and health care involving aboriginal peoples. Contemp Nurse, 22(2), 155–167. [DOI] [PubMed]
- Campbell DJ, Lacny SL, Weaver RG, Manns BJ, Tonelli M, Barnabe C, Hemmelgarn BR. Age modification of diabetes-related hospitalization among First Nations adults in Alberta, Canada. Diabetol Metab Syndr. 2014;6(1):108. doi: 10.1186/1758-5996-6-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canadian Institute for Health Information. (2007). Health Indicators 2007. Ottawa. Available at http://secure.cihi.ca/cihiweb/dispPage.jsp?cw_page=indicators_definitions_health_system_e.
- Canadian Institute for Health Information. (2008). Health Indicators 2008. Ottawa. Available at http://secure.cihi.ca/cihiweb/products/HealthIndicators2008_ENGweb.pdf.
- Canadian Institutes of Health Research, Natural Sciences and Engineering Research Council of Canada, & Social Sciences and Humanities Research Council of Canada. (2014). Research involving the First Nations, Inuit and Métis peoples of Canada. In Tri-Council policy statement, ethical conduct for research involving humans. Ottawa: Government of Canada.
- Correa-Velez I, Ansari Z, Sundararajan V, Brown K, Gifford SM. A six-year descriptive analysis of hospitalisations for ambulatory care sensitive conditions among people born in refugee-source countries. Popul Health Metrics. 2007;5:9. doi: 10.1186/1478-7954-5-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dale H, Lee A. Behavioural health consultants in integrated primary care teams: a model for future care. BMC Fam Pract. 2016;17:97. doi: 10.1186/s12875-016-0485-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duff P, Bingham B, Simo A, Jury D, Reading C, Shannon K. The ‘stolen generations’ of mothers and daughters: child apprehension and enhanced HIV vulnerabilities for sex workers of aboriginal ancestry. PLoS One. 2014;9(6):e99664. doi: 10.1371/journal.pone.0099664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erny-Albrecht, K., Oliver-Baxter, J., & Bywood, P. (2016). Primary health care-based programmes targeting potentially avoidable hospitalisations in vulnerable groups with chronic disease. Adelaide: Adelaide Primary Health Care Research and Information Service. Retrieved from https://dspace.flinders.edu.au/xmlui/bitstream/handle/2328/36227/PIR_Potentially%20avoidable%20hospitalisations.pdf?sequence=1&isAllowed=y.
- Ford-Gilboe M, Wathen CN, Varcoe C, Herbert C, Jackson BE, Lavoie JG, et al. How equity-oriented health care affects health: key mechanisms and implications for primary health care practice and policy. Milbank Q. 2018;96(4):635–671. doi: 10.1111/1468-0009.12349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson OR, Segal L, McDermott RA. A systematic review of evidence on the association between hospitalisation for chronic disease related ambulatory care sensitive conditions and primary health care resourcing. BMC Health Serv Res. 2013;13:336. doi: 10.1186/1472-6963-13-336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottlieb, K. (2013). The Nuka System of Care: improving health through ownership and relationships. International Journal of Circumpolar Health, 72(1), 21118. 10.3402/ijch.v72i0.21118. [DOI] [PMC free article] [PubMed]
- Government of Canada. (1985). Indian Act (R.S.C., 1985, c. I-5). Ottawa: Government of Canada. Retrieved from https://laws-lois.justice.gc.ca/eng/acts/I-5/FullText.html.
- Green ME, Wong ST, Lavoie JG, Kwong J, MacWilliam L, Peterson S, et al. Admission to hospital for pneumonia and influenza attributable to 2009 pandemic A/H1N1 influenza in First Nations communities in three provinces of Canada. BMC Public Health. 2013;13:1029. doi: 10.1186/1471-2458-13-1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwood M, de Leeuw S, Lindsay NM, Reading C. Determinants of indigenous peoples’ health in Canada: beyond the social. Toronto: Canadian Scholars' Press; 2015. [Google Scholar]
- Hackett C, Feeny D, Tompa E. Canada’s residential school system: measuring the intergenerational impact of familial attendance on health and mental health outcomes. J Epidemiol Community Health. 2016;70(11):1096–1105. doi: 10.1136/jech-2016-207380. [DOI] [PubMed] [Google Scholar]
- Health Council of Canada. (2005). Health care renewal in Canada: accelerating change. Toronto: Health Council of Canada.
- Katz, A., Enns, J., & Kinew, K. (2017). Canada needs a holistic First Nations health strategy. Canadian Medical Association Journal, 189(31), E1006–E1007. [DOI] [PMC free article] [PubMed]
- Kyoon-Achan G, Lavoie JG, Phillips-Beck W, Kinew KA, Ibrahim N, Sinclair S, Katz A. What changes would Manitoba FN like to see in the primary healthcare they receive? A qualitative investigation. Healthcare Policy. 2019;15(2):85–99. doi: 10.12927/hcpol.2019.26069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kyoon-Achan G, Philips-Beck W, Lavoie JG, Eni R, Sinclair S, Avery Kinew K, et al. Looking back, moving forward: a First Nations framework for mental wellness. Int J Cult Ment Health. 2018;11(4):679–692. doi: 10.1080/17542863.2018.1556714. [DOI] [Google Scholar]
- Lalonde M. A new perspective on the health of Canadians (Lalonde report) Ottawa: Department of National Health and Welfare; 1974. [Google Scholar]
- Lavoie JG. Policy silences: Why Canada needs a National First Nations, Inuit and Metis health policy. Int J Circumpolar Health. 2013;72:22690. doi: 10.3402/ijch.v72i0.22690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavoie JG, Forget E, O'Neil JD. Why equity in financing First Nation on-reserve health services matters: findings from the 2005 National Evaluation of the Health Transfer Policy. Healthcare Policy. 2007;2(4):79–98. [PMC free article] [PubMed] [Google Scholar]
- Lavoie JG, Forget EL, Dahl M, Martens PJ, O'Neil JD. Is it worthwhile to invest in home care? Healthc Policy. 2011;6(4):35–48. [PMC free article] [PubMed] [Google Scholar]
- Lavoie, J. G., Forget, E. L., Prakash, T., Dahl, M., Martens, P. J., & O’Neil, J. D. (2010). Have investments in on-reserve health services and initiatives promoting community control improved First Nations’ health in Manitoba? Social Science & Medicine, 71(4), 717–724. http://dx.doi.org.proxy2.lib.umanitoba.ca/10.1016/j.socscimed.2010.04.037. [DOI] [PubMed]
- Lavoie JG, Kaufert JM, Browne AJ, Mah S, O'Neil JD. Negotiating barriers, navigating the maze: First Nation peoples’ experience of medical relocation. Canadian Public Administration. 2015;58(2):295–314. doi: 10.1111/capa.12111. [DOI] [Google Scholar]
- Lavoie JG, Wong S, Ibrahim N, Green M, O'Neil J, Ward A. Hospitalization for mental health related ambulatory care sensitive conditions: what are the trends for First Nations peoples living on-reserve in British Columbia? International Journal of Health Equity. 2018;17:156–170. doi: 10.1186/s12939-018-0860-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavoie JG, Wong ST, Ibrahim N, O’Neil JD, Green M, Ward A. Underutilized and undertheorized: the use of hospitalization for ambulatory care sensitive conditions for assessing the extent to which primary healthcare services are meeting needs in British Columbia First Nation communities. BMC Health Serv Res. 2019;19(1):50. doi: 10.1186/s12913-018-3850-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lux, M. K. (2016). Separate beds: a history of Indian hospitals in Canada, 1920s-1980s. Toronto: University of Toronto Press.
- Lyons KJ, Ezekowitz JA, Liu W, McAlister FA, Kaul P. Mortality outcomes among status Aboriginals and whites with heart failure. Can J Cardiol. 2014;30(6):619–626. doi: 10.1016/j.cjca.2014.03.004. [DOI] [PubMed] [Google Scholar]
- Manitoba First Nations Education Resource Centre Inc. (2014). Guidelines for Ethical Research in Manitoba First Nations: Principles, practices, and templates. Winnipeg. Retrieved from https://peke.fnhssm.com/wpcontent/uploads/2017/08/tool_fnerc_2014_guide_ethical_research_in_manitoba_first_nations.pdf.
- Marmot, M., & Wilkinson, R. G. (2006). Social determinants of health (Oxford University Press Ed.). Oxford, UK: Oxford University Press.
- Martens, P. J., Bond, R., Jebamani, L., Burchill, C., Roos, N., Derksen, S., . . . O'Neil, J. D. (2002). The health and health care use of registered First Nations people living in Manitoba: a population-based study. Winnipeg: Manitoba Centre for Health Policy, Faculty of Medicine, & University of Manitoba. Retrieved from http://www.umanitoba.ca/centres/mchp/reports/rfn_pdfs.htm.
- Martens PJ, Sanderson D, Jebamani L. Health services use of Manitoba First Nations people: is it related to underlying need? Canadian Journal of Public Health. 2005;96(Suppl. 1):S39–S44. doi: 10.1007/BF03405315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Aboriginal Health Organization . OCAP, ownership, control, access and promotion: sanctioned by the First Nations information governance committee. Ottawa: NAHO First Nations Centre; 2007. [Google Scholar]
- Ospina MB, Voaklander D, Senthilselvan A, Stickland MK, King M, Harris AW, Rowe BH. Incidence and prevalence of chronic obstructive pulmonary disease among aboriginal peoples in Alberta, Canada. PLoS One. 2015;10(4):e0123204. doi: 10.1371/journal.pone.0123204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Provincial Court of Manitoba . Report of the Brian Sinclair Inquest. Winnipeg: Report of the Brian Sinclair Inquest; 2014. [Google Scholar]
- Riediger ND, Lukianchuk V, Bruce SG. Incident diabetes, hypertension and dyslipidemia in a Manitoba First Nation. Int J Circumpolar Health. 2015;74:27712. doi: 10.3402/ijch.v74.27712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Southcentral Foundation. (2019). Nuka system of care. Anchorage, Alaska: Southcentral Foundation. Retrieved from https://www.southcentralfoundation.com/nuka-system-of-care/.
- Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. The Milbank Quarterly. 2005;83(3):457–502. doi: 10.1111/j.1468-0009.2005.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistics Canada. (2016). Aboriginal peoples highlight tables, 2016 census: Aboriginal identity population by both sexes, total - age, 2016 counts, Canada, provinces and territories, 2016 census – 25% sample data. Ottawa: Statistics Canada. Retrieved from http://www12.statcan.gc.ca/census-recensement/2016/dp-pd/hlt-fst/abo-aut/Table.cfm?Lang=Eng&T=101&S=99&O=A.
- The Jordan’s Principle Working Group . Without denial, delay, or disruption: ensuring First Nations children’s access to equitable services through Jordan’s principle. Ottawa: Assembly of First Nations; 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Truth and Reconciliation Commission of Canada. (2015). Honouring the truth, reconciling for the future summary of the final report of the Truth and Reconciliation Commission of Canada. Ottawa: Truth and Reconciliation Commission of Canada. Retrieved from http://www.myrobust.com/websites/trcinstitution/File/Reports/Executive_Summary_English_Web.pdf.
- Turner, A., Crompton, S., & Langlois, S. P. (2013). Aboriginal peoples in Canada - First Nations people, Métis and Inuit national household survey, 2011. Ottawa, Ont. Statistics Canada, Canadian Electronic Library.
- United Nations. (2007). United Nations declaration on the rights of Indigenous peoples. Geneva: United Nations. Retrieved from https://www.cwis.org/drft9329.html/.
- United Nations Human Rights Council. (2007). Implementation of General Assembly Resolution 60/251 of 15 March 2006 entitled “Human Rights Council”: Report of the Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health, Paul Hunt, Addendum, Mission to Sweden*. Geneva: United Nations. Retrieved from https://www.hr-dp.org/files/2015/06/05/UN_Special_Rapporteur_on_the_right_of_health,_Sweden.pdf.
- Wesley-Esquimaux CC, Smolewski M. Historic trauma and Aboriginal healing. Ottawa: Aboriginal Healing Foundation; 2004. [Google Scholar]
- Wilkinson R, Marmot M. Social determinants of health: the solid facts. Copenhagen: World Health Organization; 2003. [Google Scholar]