Abstract
Aim
This study aimed to evaluate the prevalence of carious, restored, and missing teeth among diabetic and non-diabetic patients who visited dental clinics in Dammam, Saudi Arabia.
Method
This retrospective study was conducted between April and November 2018. The data collection procedure was conducted in two steps: (1) review of patient records for the demographic variables and (2) screening of digital panoramic radiographs (OPGs). The patients who visited the restorative and prosthetic clinics in the period of 2016–2017 were included in the study.
Results
A total of 1186 patient records and OPGs were reviewed to extract the data. The average age of the patients in the study sample was 40.96 (±16.29). The sample included 751 (63.3%) female and 435 (36.7%) male patients. Among the patients, 192 (16.2%) had diabetes mellitus and 994 (83.8%) were non-diabetic. The average numbers of fixed partial dentures and missing teeth were significantly high among diabetic patients (P < 0.001). Conversely, the average numbers of carious lesions and restored teeth were higher among the non-diabetic patients. Only the number of restored teeth was found to be significant (P < 0.001).
Conclusion
The diabetic patients were found to be at high risk of losing teeth compared with the non-diabetic patients. The prevalence of fixed partial dentures was also higher among diabetic patients. The oral health status of dental patients with diabetes needs urgent attention to prevent these patients from having teeth loss, and it can be done by improving their oral health.
Keywords: Carious lesions, Restored teeth, Prosthesis, Missing teeth, Diabetic mellitus
1. Introduction
Diabetes mellitus (DM) is a common chronic disease manifested by hyperglycemia resulting from an absolute or relative insulin deficiency (Latti et al., 2018). The disease affects people around the world, as 8.5% of the population worldwide was diagnosed with diabetes in 2014 (Sreedharan and Abdelmalak, 2018). Saudi Arabia is considered one of the countries with a high DM prevalence (Al-Rubeaan, 2015, Naeem, 2015). A recent cross-sectional study examined 6024 Saudi subjects attending the primary health care department at King Fahad Armed Forces Hospital, Jeddah, Saudi Arabia and reported that 30% of the subjects were diagnosed with DM, with 34% of them being male and 27% being female (Alqurashi et al., 2011).
Aside from the relation between periodontal diseases and diabetes (Grossi and Genco, 1998, Nishimura et al., 1998, Kapp et al., 2007, Wiener et al., 2017, Yoo et al., 2019), researchers have also studied the restorative and prosthetic needs of diabetic dental patients. A study detected a strong association between diabetes and teeth loss, with the results indicating that the subjects with diabetes had a 1.46 times higher incident rate of teeth loss than the non-diabetic patients (Kapp et al., 2007). When the researchers stratified the findings by age, they found that diabetes and teeth loss association was significantly higher in the younger subjects (18–44 years) and that the association was not significant for the older age group (65 years or older)(Kapp et al., 2007). A recent cohort study reported that diabetic patients were at a higher risk of teeth loss than the non-diabetic patients. Moreover, the risk of teeth loss increased as the severity of diabetes increased, and the risk decreased as the dental visits increased (Yoo et al., 2019). Consequently, with the increased prevalence of teeth loss among diabetic patients, the prevalence of prosthetic needs also increased (Jung et al., 2013).
Several studies evaluated the effect of diabetes on the incidence of dental caries (Ferizi et al., 2018, Latti et al., 2018). A study exploring the incidence of dental caries and its effect on the salivary flow rate in diabetic children (type 1) compared with non-diabetic patients found that the diabetic children had a higher risk for dental caries and a lower salivary flow than the control group (Ferizi et al., 2018). The mean number of Decayed, missing, and filled teeth (DMFT) among diabetic patients was found to be significantly higher than that of non-diabetic patients (Latti et al., 2018). A retrospective study reported a significant difference in carious lesions between patients with a poor glycemic index and those with controlled diabetes and that patients with controlled diabetes showed less carious lesions than the control group (Buysschaert et al., 2018). Furthermore, reduced salivary flow rates and higher glucose concentrations of the gingival crevicular fluid were observed among diabetic patients (Chhabrani et al., 2013, Velasco-Ortega et al., 2016).
The association between carious lesions and the numbers of restored and missing teeth in diabetic and non-diabetic patients has not been well investigated in a single study. Thus, this research aimed to examine the correlation between the numbers of carious, restored, and missing teeth and DM in diabetic patients compared with non-diabetic patients.
2. Methodology
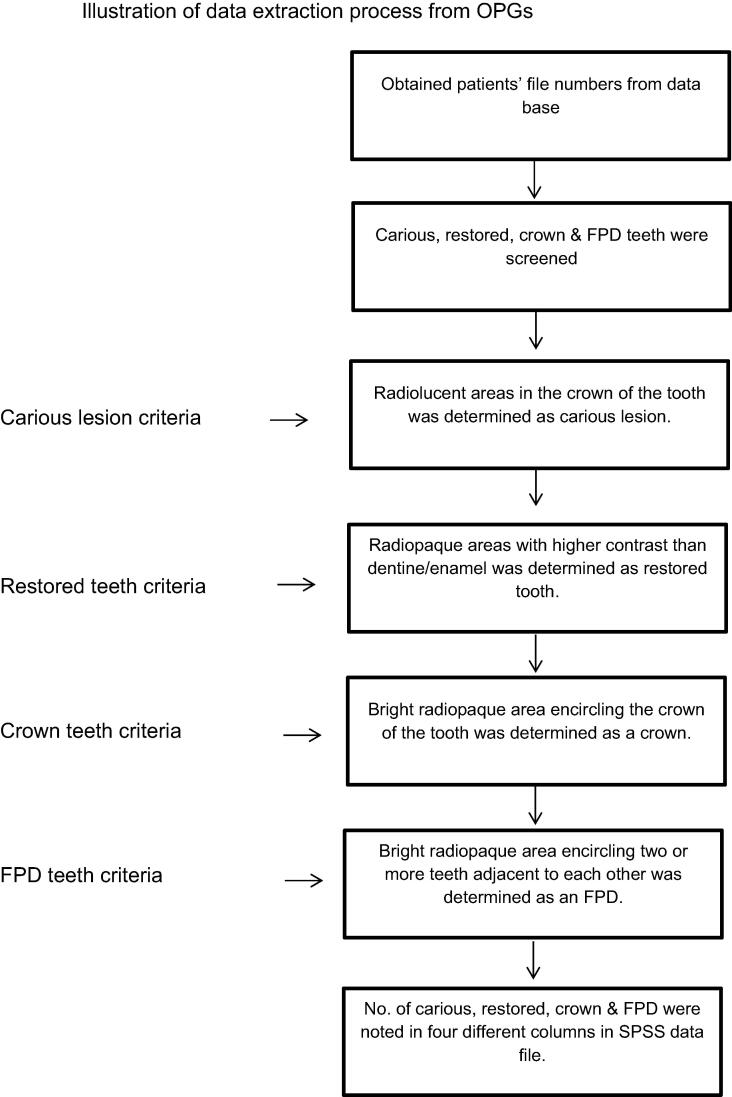
This retrospective study was performed from April to November 2018 after obtaining the ethical approval of the research committee of the College of Dentistry, Imam Abdulrahman bin Faisal University (letter no. 2017019). The patients who visited the restorative and prosthetic clinics in the period of 2016–2017 were included in the study. The study sample was divided into the diabetic and non-diabetic groups. Their health status and demographical data, such as age and gender, were extracted from the patient records. The study variables, including carious lesions and the numbers of restored teeth, prosthesis, and missing teeth, were obtained through a careful examination of the digital panoramic radiographs (OPGs) (Fig. 1) by three calibrated dental interns, and reliability was checked by two radiologists who reviewed the data. The kappa statistics was found to be 0.74.
Fig. 1.
Illustration of data extraction process from OPGs.
The inclusion criteria for the study sample were as follows: (1) all the needed demographical data are available in the records and (2) availability of OPGs. The exclusion criterion was (1) patients visiting the clinics other than for restoration and prosthodontics. The type of DM was not considered, and both types 1 and 2 diabetes were included in the study. The teeth having any of the above findings were noted according to the universal tooth numbering system.
In the first phase, the patient records were reviewed to obtain their health status and demographical data. Afterward, the patients’ OPGs were screened to find the numbers of carious lesions, restored teeth, prosthesis [crowns and fixed partial dentures (FPD)], and missing teeth. Variation in the frequency of restored and missing teeth were analyzed with the demographic variables for the diabetic and non-diabetic patients, respectively. The percentage of the prevalence of the variables among the diabetic and non-diabetic patients was calculated to help assess the oral health status of the sample. Statistical significance was computed by comparing the average numbers of carious lesions, restored teeth, prosthesis, and missing teeth among the diabetic and non-diabetic patients with the gender of the patients using two independent samples T-test to check the hypothesis that diabetic patients have a higher prevalence of dental problems than non-diabetic patients. Analysis of variance was used to assess the significance between the patients’ age and the independent variables. P-value was set to 0.05. An insignificant p-value was obtained when the normality of the data was tested by the Shapiro–Wilk test, which provided the reason to execute all statistics through the parametric tests.
3. Results
A total of 1196 patient records and OPGs were reviewed to extract the data. As 10 (0.8%) patient records did not have the necessary information, the total number of patient records included in the analysis was reduced to 1186. The mean age of the patients was 40.96 (±16.29), and it varied from 13 to 109 years, with the majority being 26–55 years old (57%). The sample comprised of 751 (63.3%) female patients and 435 (36.7%) male patients.
3.1. Prevalence of DM according to gender and age
Among the 1186 patients, 192 (16.2%) had DM and 994 (83.8%) were non-diabetics. A significantly high proportion of male patients (23.6%) suffered from DM compared with the females (12.6%) (P < 0.001). Overall, the prevalence of DM was higher among patients who were 56–70 years old (47.5%; 97 out 204), followed by the age group of above 70 years (31.6%; 12 out of 38).
3.2. Prevalence of missing, carious, and restored teeth according to gender
The study sample groups were compared according to gender with the prevalence of missing teeth, carious lesions, and restored teeth. The male patients had a significantly higher number of missing teeth than the females (P < 0.001) (Table 2). The average number of restored teeth was 3.2 (3.3%) for the female patients and 2.6 (2.96%) for the male patients, with a statistically significant difference (P = 0.002).
Table 2.
Distribution of factors according to patients’ gender.
| Carious Lesion | No. of Restored Teeth | Crowns | FPD | Missing Teeth | |
|---|---|---|---|---|---|
| Mean(SD) | Mean(SD) | Mean(SD) | Mean(SD) | Mean(SD) | |
| Male | 2.6(3.4) | 2.6(2.96) | 0.37(1.1) | 0.97(2.7) | 8.1(9.0) |
| Female | 2.7(3.3) | 3.2(3.3) | 0.5(1.2) | 0.84(2.7) | 5.5(6.8) |
| P-Value | 0.68 | 0.002* | 0.087 | 0.43 | <0.001* |
Significant difference in p-value.
3.3. Prevalence of missing, carious, and restored teeth according to age
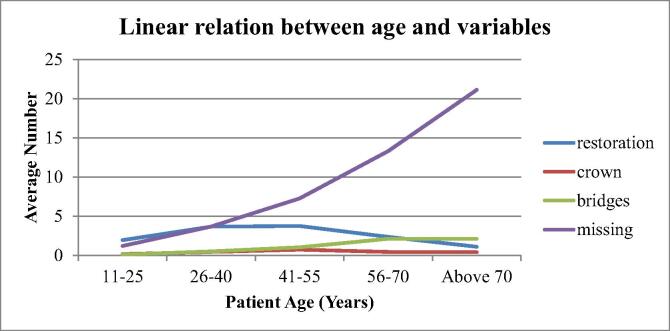
The average number of missing teeth showed an increasing trend with age (Fig. 2) (P < 0.001). Statistically, the number of restored teeth and crowns was significantly higher in the age range of 26–55 years (P < 0.001 and P = 0.003, respectively).
Fig. 2.
Trend of evaluating variables of the study sample according to their age.
3.4. Prevalence of missing, carious, and restored teeth according to diabetic status
On average, the patients had 6.4 (±7.8) missing teeth, 2.68 (±3.4) carious lesions, 2.99 (±3.2) restored teeth, 0.45 (±1.2) crowns, and 0.89 (±2.7) FPDs. The average numbers of FPDs and missing teeth were significantly higher among the diabetic patients than the non-diabetic patients (P < 0.001). Similarly, the average numbers of carious lesions and restored teeth were higher among the non-diabetic patients, but significance was only found in the number of restored teeth (P < 0.001) (Table 1).
Table 1.
Oral health difference among diabetic and non-diabetic patients.
| Carious Lesion | No. of Restored Teeth | Crowns | FPD | Missing Teeth | |
|---|---|---|---|---|---|
| Mean(SD) | Mean(SD) | Mean(SD) | Mean(SD) | Mean(SD) | |
| Diabetic | 2.6(3.4) | 2.2(2.5) | 0.27(0.96) | 1.5(3.5) | 12.04(10.0) |
| Non-Diabetic | 2.8(3.3) | 3.2(3.3) | 0.49(1.2) | 0.77(2.5) | 5.2(6.6) |
| P-value | 0.051 | <0.001* | 0.015* | <0.001* | <0.001* |
Significant difference in p-value.
4. Discussion
The burden of DM is increasing, and its incidence and prevalence are expected to increase from 415 million in 2015 to 642 million in 2040 (Ogurtsova et al., 2017). The disease has two main types, namely type 1 and type 2, with type 2 constituting the majority of the disease prevalence (Forouhi and Wareham, 2010). The results showed a higher prevalence of DM among the male and older age patients compared with the female and younger age patients. Several risk factors contribute to the higher disease prevalence in older age such as menopause (Guo et al., 2019). Oral manifestations, such as periodontal diseases, dental caries, xerostomia, teeth loss, and delayed wound healing, can be observed in diabetic patients (Mauri-Obradors et al., 2015, Neidell et al., 2017). To the best of our knowledge, this study is the first assessing the correlation between DM and multiple oral findings through a retrograde radiographic evaluation.
Teeth loss is a global public health concern (Wiener et al., 2017). Multiple factors, such as race, age, and DM, can lead to teeth loss (Luo et al., 2015). In the present study, a significant difference was found in the number of missing teeth (P < 0.001) between the diabetic and non-diabetic patients. The male patients had significantly more missing teeth (P < 0.001) than the female patients. The results of this study are in agreement with those of other research, indicating that a higher number of missing teeth can be observed in diabetic patients (Wiener et al., 2017, Yoo et al., 2019).
Dental caries and DM have a complex relationship, which is a matter of controversy (Taylor et al., 2004, Latti et al., 2018). In a previous study, diabetic patients showed to have an increased number of Streptococcus mutans, which are the main bacteria responsible for dental caries, thus indicating that patients with DM are at higher risk of developing dental caries (Taylor et al., 2005). However, in the present study, no significant difference was observed in dental caries between the diabetic and non-diabetic patients (P < 0.05). This result can be attributed to the number of missing teeth in diabetic patients compared with the non-diabetic. As the diabetic patients had a higher number of missing teeth, the prevalence of dental caries was not significantly high because the number of remaining teeth to be affected by caries was less in the diabetic patients than in the non-diabetic patients. Many factors may influence dental caries, such as poor oral hygiene practices, diet, and saliva, which are the more significant factors in developing dental caries (BolguÈl et al., 2004). According to BolguÈl et al. (2004), well- or moderately controlled diabetic patients have a significantly lower incidence of caries than poorly controlled diabetic patients.
Conversely, in the present study, the non-diabetic patients had a significantly higher number of restored teeth (P < 0.001) than the diabetic patients. The highest number of restored teeth was found in the female patients. One study compared the DMFT in the female and male patients with their dental visits and found that the females had an average of 2.4 filled teeth compared with 1.7 in the males. In both groups, the patients who came for general treatment clinics showed a higher number of filled teeth, and those who attended emergency treatment clinics had a higher number of root canal treatments and extractions (Abduallah, 2013). Regardless of the number of restored teeth, some researchers compared composite restorations between diabetic and non-diabetic patients and found that composite restorations were biocompatible in both groups (Nassar et al., 2012)
This study did not compare the periodontal problems between the diabetic and non-diabetic patients, and this is one of the study limitations. As this work is a single-center study, the inclusion of various dental colleges can help to generalize the results more effectively.
5. Conclusion
The average tooth loss among diabetic patients demands urgent care and patient guidance, so that patients can maintain adequate oral health. Otherwise, they will have to bear the cost and consequence of extractions. This can lead to a greater need for removable and fixed dental prosthesis, which can be a burden on the patients socially and economically. Based on the results of this study, the following can be concluded:
-
–
DM significantly affected the patients’ oral health status.
-
–
The numbers of missing teeth and fixed dental prostheses were significantly higher in the diabetic patients than in the non-diabetic patients.
-
–
The diabetic patients had significantly lower numbers of restored teeth and carious lesions because of their significant tooth loss.
CRediT authorship contribution statement
Soban Qadir Khan: Conceptualization; Formal analysis; Writing - original draft; Writing - review & editing. Abdul Khabeer: Writing - original draft; Writing - review & editing. Ahmad M. Al-Thobity: Writing - original draft; Writing - review & editing. Mashael Abdullah Benrashed: Data curation. Nujood Ibrahim Alyousef: Data curation. Yara AlMaimouni: Data curation.
Footnotes
Peer review under responsibility of King Saud University.
References
- Abduallah H.A. Experience of dental caries of adult patients in relation to the characteristic of dental visit and brushing behavior in Tikrit City. Mustansiria Dental J. 2013;10:17–27. [Google Scholar]
- Al-Rubeaan K. National surveillance for type 1, type 2 diabetesand prediabetes among children and adolescents:a population-based study (SAUDI-DM) J. Epidemiol. Commun. Health. 2015;69:7. doi: 10.1136/jech-2015-205710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alqurashi K.A., Aljabri K.S., Bokhari S.A. Prevalence of diabetes mellitus in a Saudi community. Ann. Saudi Med. 2011;31:19–23. doi: 10.4103/0256-4947.75773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BolguÈl B.S., Celenk S., Ayna B.E., Atakul F., Uysal E. Evaluation of caries risk factors and effects of a fluoride-releasing adhesive material in children with insulin-dependent diabetes mellitus (IDDM): initial first-year results. Acta Odontologica Scandinavica. 2004;65:289–292. doi: 10.1080/00016350410001766. [DOI] [PubMed] [Google Scholar]
- Chhabrani P.R., Ali S.M., Nigam C., Gahlot R., Chhabrani J.R. Perspective of diabetes mellitus in dentistry. Int. J. Contemporary Dentistry. 2013;4:6. [Google Scholar]
- Ferizi L., Dragidella F., Spahiu L., Begzati A., Kotori V. The influence of type 1 diabetes mellitus on dental caries and salivary composition. Int. J. Dentistry. 2018;2018:1–7. doi: 10.1155/2018/5780916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forouhi N.G., Wareham N.J. Epidemiol. Diabetes Med. 2010;38:602–606. [Google Scholar]
- Grossi S.G., Genco R.J. Periodontal disease and diabetes mellitus: a two way relationship. J. Periodontol. 1998;3:51–61. doi: 10.1902/annals.1998.3.1.51. [DOI] [PubMed] [Google Scholar]
- Guo C., Li Q., Tian G., Liu Y., Sun X., Yin Z., Li H., Chen X., Liu X., Zhang D., Cheng C. Association of age at menopause and type 2 diabetes: a systematic review and dose-response meta-analysis of cohort studies. Primary Care Diabetes. 2019;13:301–309. doi: 10.1016/j.pcd.2019.02.001. [DOI] [PubMed] [Google Scholar]
- Jung H.-Y., Kim Y.-G., Jin M.-U., Cho J.-H., Lee J.-M. Relationship of tooth mortality and implant treatment in Type 2 diabetes mellitus patients in Korean adults. J. Adv. Prosthodont. 2013;5:7. doi: 10.4047/jap.2013.5.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapp J.M., Boren S.A., Yun S., LeMaster J. Diabetes and tooth loss in a national sample of dentate adults reporting annual dental visits. Prevent. Chronic Disease. 2007;4:A59. [PMC free article] [PubMed] [Google Scholar]
- Latti B.R., Kalburge J.V., Birajdar S.B., Latti R.G. Evaluation of relationship between dental caries, diabetes mellitus and oral microbiota in diabetics. J. Oral Maxillofacial Pathol. 2018;22:6. doi: 10.4103/jomfp.JOMFP_163_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo H., Pan W., Sloan F., Feinglos M., Wu B. Forty-year trends in tooth loss among american adults with and without diabetes mellitus: an age-period-cohort analysis. Prevent. Chronic Disease. 2015;12:E211. doi: 10.5888/pcd12.150309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysschaert M., Buysschaert B., Jamart J. Dental caries and diabetes: a Belgian survey of patients with type 1 and type 2 diabetes. Diabetes Metab. 2018 doi: 10.1016/j.diabet.2018.06.002. [DOI] [PubMed] [Google Scholar]
- Mauri-Obradors E., Jané-Salas E., del Mar Sabater-Recolons M., Vinas M., López-López J. Effect of nonsurgical periodontal treatment on glycosylated hemoglobin in diabetic patients: a systematic review. Odontology. 2015;103:301–313. doi: 10.1007/s10266-014-0165-2. [DOI] [PubMed] [Google Scholar]
- Naeem Z. Burden of diabetes mellitus in Saudi Arabia. IJHS. 2015;9(3):V–VI. doi: 10.12816/0024690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nassar C.A., Nassar P.O., Secundes M.B., Ribeiro Busato P.D.M., Camilotti V. Composite resin restorations of non-carious cervical lesions in patients with diabetes mellitus and periodontal disease: pilot study. Acta Odontológica Latinoamericana. 2012;25:279–286. [PubMed] [Google Scholar]
- Neidell M., Lamster I.B., Shearer B. Cost-effectiveness of diabetes screening initiated through a dental visit. Commun. Dent. Oral Epidemiol. 2017;45:275–280. doi: 10.1111/cdoe.12286. [DOI] [PubMed] [Google Scholar]
- Nishimura F.F., Takahashi K., Kurihara M., Takashiba S., Murayama Y. Periodontal disease as a complication of Diabetes Mellitus. J. Periodontol. 1998;3:20–29. doi: 10.1902/annals.1998.3.1.20. [DOI] [PubMed] [Google Scholar]
- Ogurtsova K., da Rocha Fernandes J.D., Huang Y., Linnenkamp U., Guariguata L., Cho N.H., Cavan D., Shaw J.E., Makaroff L.E. IDF Diabetes Atlas: global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res. Clin. Pract. 2017;128:40–50. doi: 10.1016/j.diabres.2017.03.024. [DOI] [PubMed] [Google Scholar]
- Sreedharan R., Abdelmalak B. Diabetes Mellitus: preoperatve concerns and evaluation. Anesthesiol. Clin. 2018;36:581–597. doi: 10.1016/j.anclin.2018.07.007. [DOI] [PubMed] [Google Scholar]
- Taylor G.W., Manz M.C., Borgnakke W.S. Diabetes, periodontal diseases, dental caries and tooth loss: a review of the literature. Compendium. 2004;25:179–188. [PubMed] [Google Scholar]
- Taylor G.W., Manz M.C., Borgnakke W.S. Caries risk assessment as a predictor of metabolic control in young type 1 diabetics. Diabetic Med. 2005;22:312–315. doi: 10.1111/j.1464-5491.2005.01419.x. [DOI] [PubMed] [Google Scholar]
- Velasco-Ortega E., Delgado-Ruiz R.A., López-López J. Dentistry and diabetes: the influence of diabetes in oral diseases and dental treatments. J. Diabetes Res. 2016;2016:6073190. doi: 10.1155/2016/6073190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiener R.C., Shen C., Findley P.A., Sambamoorthi U., Tan X. The association between diabetes mellitus, sugar-sweetened beverages, and tooth loss in adults: evidence from 18 states. J. Am. Dental Assoc. 2017;148:500–509. doi: 10.1016/j.adaj.2017.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoo J.J., Kim D.W., Kim M.Y., Kim Y.T., Yoon J.H. The effect of diabetes on tooth loss due to periodontal disease: a nationwide population-based cohort study in South Korea. J. Periodontol. 2019;90:576–583. doi: 10.1002/JPER.18-0480. [DOI] [PubMed] [Google Scholar]