Abstract
Background
Medial elbow pain is a common complaint in overhead throwing athletes. The throwing motion places repetitive tensile and compressive forces on the elbow resulting in significant stress across the ulnohumeral joint. This stress can result in soft-tissue, ligamentous, and ulnar nerve injury. The purpose of this study was to retrospectively investigate the clinical findings and outcomes, including return to play rates, of patients who underwent ulnar nerve transposition surgery for isolated ulnar neuritis.
Methods
Throwing athletes who underwent isolated, primary ulnar nerve transposition surgery over an eight-year period, 2009 to 2017, were identified and included in our analysis. Nonthrowing athletes, those who underwent revision ulnar nerve transposition surgery, and those who underwent concomitant ulnar collateral ligament reconstruction or repair were excluded. Patients were contacted to complete the Kerlan-Jobe Orthopaedic Clinic Shoulder and Elbow Score as well as a return to play rate questionnaire. The minimum follow-up was 2 years.
Results
Fifteen patients met the inclusion criteria: 13 (86.7%) men and 2 (13.3%) women. The average age at the time of surgery was 19.2 years old (range, 15.6-28.0). Preoperatively, 13 (86.7%) patients played baseball and 2 (13.3%) patients played softball. Two patients (13.3%) underwent a previous ulnar collateral ligament reconstruction. There were no complications. The average final follow-up was 65.26 (range, 24.44-113.29) months with an average Kerlan-Jobe Orthopaedic Clinic Score of 64.51 (range, 28.60-100.00). Thirteen (86.7%) patients were able to return to their preinjury sport, 2 to a higher level of competition, 8 to the same level, and 3 to a lower level. Seven of the 13 (53.8%) patients sustained a postoperative ipsilateral shoulder or elbow injury at an average of 19.57 (range, 7.00-36.00) months postoperatively. All patients reported sustaining the injury as a result of throwing.
Conclusion
The results of our study indicate that ulnar nerve transposition surgery in throwing athletes allows athletes to return to throwing with low reoperation rates. However, more than half of the athletes in our analysis sustained a subsequent ipsilateral shoulder or elbow injury. Further investigation regarding outcomes in throwing athletes after ulnar nerve transposition surgery is warranted.
Keywords: Elbow, baseball/softball, return to play, ulnar nerve transposition, ulnar nerve decompression, throwing athlete
Medial elbow pain is a common complaint in overhead throwing athletes, regardless of the level of competition.7 The throwing motion places repetitive tensile and compressive forces across the elbow joint resulting in significant stress. Although most of stress is absorbed by the bony articulations at high and low flexion, much of the pressure during the throwing motion takes place between these extremes and is placed on the soft tissues about the elbow.3,10 As a result, the trauma placed on the elbow during the throwing motion can lead to soft-tissue, ligamentous, and/or nerve injury.5,10 The valgus stress during the throwing motion can cause repetitive traction across the medial structures, including the ulnar nerve.10
Tears of the ulnar collateral ligament (UCL) have increased significantly in incidence over the past several decades and the treatment options and outcomes are well documented.9 The ulnar nerve lies adjacent to the ulnar collateral ligament at the elbow as it courses through and distal to the cubital tunnel. The space within the cubital tunnel through which the nerve passes decreases through the arc of flexion.13,17 This can result in an increased risk of injury, particularly in repetitive throwing athletes.10 Accordingly, isolated ulnar neuropathy in overhead throwing athletes without varus/valgus instability has been documented.12,16 However, there has been little research in throwing athletes documenting return to play rates and performance after surgical decompression and/or transposition of the ulnar nerve.2,14
Recently, professional baseball pitchers undergoing ulnar nerve decompression and anterior transposition were noted to have a 62% return to sport rate.8 Among those players who returned to sport after surgical intervention, it was found that increased walks per nine innings were the only performance measure that suffered compared with controls. However, to date there has been limited clinical research assessing return to play rates in nonprofessional throwing athletes of all levels after isolated ulnar nerve decompression/transposition.
The purpose of this study was to retrospectively investigate the clinical findings and clinical outcomes, including return to play rates, of throwing athletes who underwent ulnar nerve transposition surgery for ulnar neuropathy in the stable elbow. We hypothesized that ulnar nerve transposition surgery for the treatment of a symptomatic elbow ulnar nerve would not result in significant improvement in elbow function.
Materials and methods
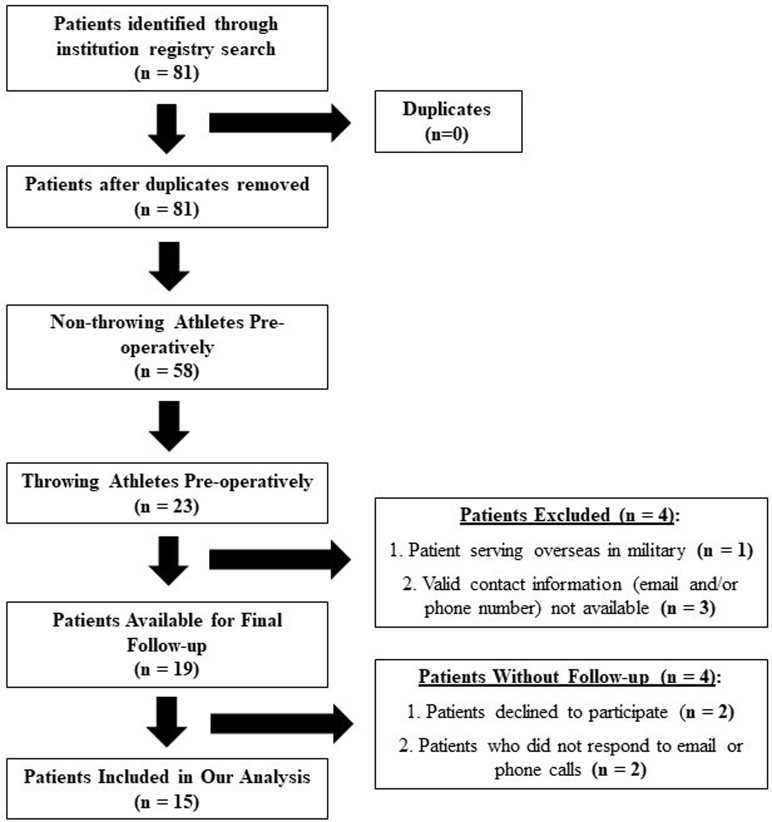
Between 2009 and 2017, eighty-one patients underwent isolated, primary ulnar nerve transposition (CPT Code 64722) or decompression (CPT Code 64718) surgery for ulnar neuropathy in an otherwise stable elbow. Surgeries were performed by one of three, fellowship trained surgeons (MGC, SBC, CCD) experienced in the care of throwing athletes. Cubital tunnel decompression was performed in standard fashion, with concomitant transposition of the ulnar nerve to prevent subluxation during the throwing motion. Twenty-three patients were identified as throwing athletes (baseball or softball players) preoperatively. Nonthrowing athletes, those who underwent revision ulnar nerve transposition surgery, and those who underwent other concomitant elbow surgery, including UCL reconstruction or repair, were excluded from this analysis. All patients had undergone prior activity modification, anti-inflammatory use, and a period of rest from throwing before surgical intervention. Identical, standard surgical technique was performed in all patients that consisted of cubital tunnel decompression and subcutaneous transposition of the nerve. Four patients were not available for follow-up leaving nineteen athletes eligible for follow-up and inclusion in our analysis (Fig. 1).
Figure 1.
Patient inclusion/exclusion criteria.
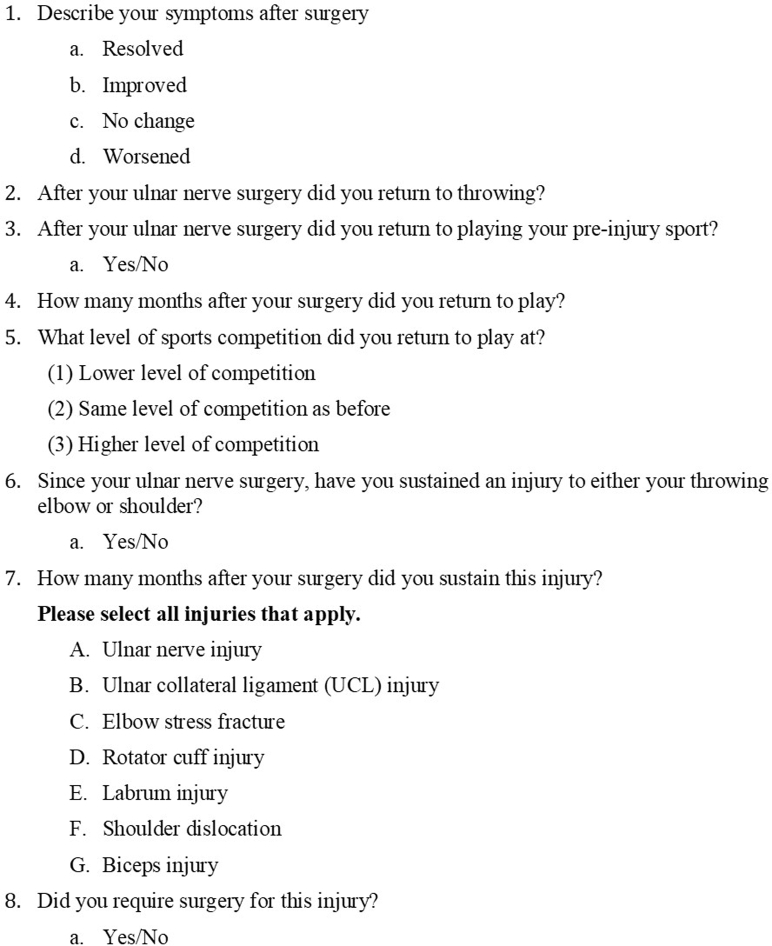
Institutional review board approval was obtained for this study. Patients were contacted via email or over the phone to complete the Kerlan-Jobe Orthopaedic Clinic (KJOC) Shoulder and Elbow Score outcome measure as well as a return to play/reinjury questionnaire (Fig. 2). The final scores were tallied by a single researcher and patients were only included if they had achieved a minimum follow-up interval of two years.
Figure 2.
Return to play and reinjury questionnaire.
Results
During the period studied, 15 (78.9%) patients who underwent isolated, primary ulnar nerve transposition surgery for ulnar neuropathy in an otherwise stable elbow, were identified as throwing athletes preoperatively and completed postoperative outcome scores a minimum of 2 years after their surgery. All patients underwent ulnar nerve transposition (CPT Code 64718) surgery. There were 13 (86.7%) men and 2 (13.3%) women with an average BMI of 26.3 (range, 22.3-33.1). The average age at the time of surgery was 19.2 years old (range, 15.6-28.0). Preoperatively, 13 (86.7%) patients played baseball and 2 (13.3%) patients played softball. Two patients (13.3%) underwent a previous ulnar collateral ligament reconstruction.
The average final follow-up was 65.26 (range, 24.44-113.29) months with an average KJOC score of 64.51 (range, 28.60-100.00). Five (33.3%) patients reported resolved symptoms, 8 (61.5%) patients reported improved symptoms, 1 (6.7%) patient noted no change in symptoms, and 1 (6.7%) patient reported worsened symptoms at final follow-up. After surgery, all 15 (100.0%) patients were able to return to throwing. Thirteen (86.7%) patients were able to return to their sport: 2 (13.3%) patient returned to a higher level of competition, 8 (53.3%) to the same level, 3 (20.0%) to a lower level, and 2 (13.3%) were unable to return to their preinjury sport (Table I). The average time to return to play was 6.3 (range, 2.0-12.0) months.
Table I.
Return to play results
| Patient # | Sex | Symptoms after surgery | Return to throwing (Y/N) | Return to preinjury sport (Y/N) | Months RTP | Level of competition |
|---|---|---|---|---|---|---|
| 1 | M | Improved | Yes | Yes | 6 | Same level of competition |
| 2 | M | Resolved | Yes | Yes | 4 | Same level of competition |
| 3 | F | Improved | Yes | No | ||
| 4 | M | Improved | Yes | Yes | 3 | Same level of competition |
| 5 | M | Resolved | Yes | Yes | 3 | Same level of competition |
| 6 | M | Worsened | Yes | Yes | 7 | Same level of competition |
| 7 | M | No change | Yes | Yes | 12 | Lower level of competition |
| 8 | M | Resolved | Yes | Yes | 8 | Same level of competition |
| 9 | F | Improved | Yes | Yes | 8 | Lower level of competition |
| 10 | M | Improved | Yes | Yes | 12 | Same level of competition |
| 11 | M | Improved | Yes | No | ||
| 12 | M | Improved | Yes | Yes | 2 | Lower level of competition |
| 13 | M | Resolved | Yes | Yes | 5 | Higher level of competition |
| 14 | M | Resolved | Yes | Yes | 6 | Higher level of competition |
| 15 | M | Improved | Yes | Yes | 6 | Same level of competition |
There were no complications. Of the patients who did not return to their sport, one (6.7%) patient did require a second surgery: the patient was bench pressing a heavy weight 6 weeks after surgery and required a flexor/pronator repair and ulnar neurolysis. After the second surgery, the patient attempted to return to baseball; however, at final follow-up, 29 months after the initial surgery, the patient was no longer able to play baseball without recurrent ulnar nerve symptoms. The other patient (6.7%) decided to no longer play before a loss of interest in the sport/graduation. Of the 13 patients who returned to play, 7 (53.8%) patients sustained a postoperative ipsilateral shoulder or elbow injury at an average of 19.57 (range, 7.00-36.00) months after their surgery (Table II). Players who reported a postoperative ipsilateral elbow or shoulder injury had a lower average KJOC score of 57.44 compared with 70.69 for players who did not report a postoperative injury; however, this difference was not significant (P = .28).
Table II.
Postsurgery ipsilateral elbow and shoulder injury results
| Patient # | Sex | Ipsilateral injury (Y/N) | Months after surgery injury | Was this injury the result of throwing? | Surgery for injury (Y/N) |
|---|---|---|---|---|---|
| 1 | M | Yes | 10 | Yes | No |
| 2 | M | No | |||
| 3 | F | No | |||
| 4 | M | Yes | 24 | Yes | No |
| 5 | M | No | |||
| 6 | M | Yes | 7 | Yes | No |
| 7 | M | Yes | 24 | Yes | No |
| 8 | M | Yes | 12 | Yes | Yes |
| 9 | F | Yes | 24 | Yes | No |
| 10 | M | Yes | 36 | Yes | Yes |
| 11 | M | No | |||
| 12 | M | No | |||
| 13 | M | No | |||
| 14 | M | No | |||
| 15 | M | No |
All 7 patients reported sustaining the injury as a result of throwing. One (6.7%) patient sustained a UCL injury but did not require surgery. Three (20.0%) patients sustained a concomitant rotator cuff and labrum injury but did not require surgery for this injury. Three (20.0%) patients sustained an isolated labrum injury for which 2 (13.3%) patients elected to undergo anterior labral débridement and superior labral repair while the other (6.7%) patient did not require surgery for their injury.
Discussion
Medial elbow pain is a common complaint among throwing athletes; however, isolated ulnar nerve decompression/transposition is a relatively uncommon surgical procedure performed for throwing athletes with ulnar neuropathy at the elbow who fail nonoperative treatment.7,8 Our hypothesis that ulnar nerve transposition surgery for the treatment of a symptomatic elbow ulnar nerve will not result in significant improvement in elbow function was not confirmed: most patients (86.7%) were able to return to their preinjury sport. However, only 66.7% of patients were able to return to their prior level of play.
The ulnar nerve is responsible for the innervation of several key muscles in the arm and hand. In instances where the ulnar nerve becomes compressed or inflamed, pain, numbness, and on occasion, severe dysfunction can occur.15 In most cases, nonoperative treatment aimed at decreasing both compression and traction on the ulnar nerve about the elbow, is successful, particularly in cases of mild nerve dysfunction.15 However, when nonoperative management fails, surgical intervention is offered in one of two forms: in situ ulnar nerve decompression for cases where the nerve does not subluxate, or transposition for cases where the nerve does subluxate.8 Transposition has also been advocated in throwing athletes even when the nerve does not subluxate.8
To date, there remains little investigation into the outcomes of throwing athletes undergoing ulnar nerve transposition. The largest investigation performed was by Erickson et al in their retrospective review of 52 professional baseball players undergoing ulnar nerve decompression/transposition.8 The authors found that 62% of players were able to return to sport and 56% returned to the same or higher preinjury level. Furthermore, Aoki et al retrospectively investigated outcomes on 6 adolescent baseball players who underwent anterior subcutaneous transposition of the ulnar nerve for cubital tunnel syndrome.1 Of the 6 players, 5 (83.3%) returned to full throwing within 5 months of surgery. One patient stopped throwing after their surgery.1 The findings of our study reported a higher return to sport rate than both of these studies, with 86.7% of the athletes in our series returning to their sport.
In situ ulnar nerve decompression has been promoted by the American Society for Surgery of the Hand to address cubital tunnel syndrome in nonoverhead athletes.18 However, postoperative instability of the ulnar nerve leading to recurrence is of particular concern in the overhead throwing athlete because of the speed and force the throwing motion places on the ulnar nerve.18 Therefore, ulnar nerve decompression followed by subcutaneous transposition is often performed in the overhead throwing athlete to address this concern. In our analysis, all patients underwent ulnar nerve transposition. As noted by Dowdle and Chalmers, a simple decompression may lead to increased failure rates and recurrence of preoperative symptoms. The authors also noted that subcutaneous transposition results in less surgical morbidity to the flexor–pronator mass.6 In our series, the nerve was transposed in all cases as opposed to isolated decompression to decrease recurrence and snapping after RTP. These findings are consistent with the prior studies by Erickson et al in professional baseball players and Aoki et al in adolescent throwing athletes undergoing treatment for ulnar neuropathy in the stable elbow. In the series by Erickson et al evaluating professional baseball players, 96% of patients underwent ulnar nerve decompression followed by subcutaneous transposition, whereas just 4% underwent in situ decompression.1,8 In the Aoki et al series, all patients underwent anterior subcutaneous transposition of the ulnar nerve.
In our study, there were 2 patients with a history of prior ulnar collateral ligament reconstruction (UCLR). Both patients were able to return to sport after surgery: 1 patient returned to prior level of competition and 1 patient returned to a lower level of competition. After the ulnar nerve transposition surgery, one of the two aforementioned players sustained an injury to the ipsilateral shoulder labrum 24 months after surgery. The patient did not require surgery for this injury. The other player did not sustain an ipsilateral elbow or ipsilateral shoulder injury. In the series by Erickson et al, similar results were shown in patients with a history of prior UCLR as 10 (73.4%) patients were able to return to their sport and 9 (64.3%) patients returned to the same or higher level of competition. Clain et al in their systematic review of 17 papers and 1518 cases demonstrated a mean prevalence of postoperative ulnar neuropathy of 12.0%.4 However, only 0.8% required a second operation to address the ulnar neuropathy. The authors also noted that patients who underwent concomitant ulnar nerve transposition with their UCLR had a higher incidence of ulnar neuropathy (16.1%) than patients who underwent isolated UCLR (3.9%). Although limited, our results indicate that a prior history of UCLR does not lead to poorer outcomes after ulnar nerve transposition.
In our series, the return to sports rate was high (86.7%); however, the return to prior performance was lower at only 66.7%. In addition, a large percentage (53.8%) of patients who returned to sport did sustain an injury to either their ipsilateral elbow or ipsilateral shoulder. In most patients, nonoperative treatment was performed; however, 2 (13.3%) patients required further surgery for their additional injuries. Therefore, the potential risk of reinjury to the athlete's throwing arm as well as the possibility of decreased return to play level should be paramount during the preoperative ulnar nerve surgery discussion.
Kraeutler et al in their series of 44 healthy, professional baseball pitchers from a single organization noted an average KJOC score of 94.82%.11 The authors discussed that throwers reporting KJOC scores below 90 may be an indicator that the thrower is playing through an injury or is at the very least, not functioning at full capacity. In our analysis, the average KJOC score at final follow-up was much lower at 64.51. Players who reported a postoperative ipsilateral elbow or shoulder injury had a lower average KJOC score of 57.44 compared with 70.69 for players who did not report a postoperative injury (P = .28). Further analysis, with baseline KJOC scores before returning to play after surgery, is necessary to determine how frequently patients are playing below the normal KJOC after ulnar nerve transposition surgery.
Limitations
This study does have several limitations. Owing to the retrospective design, minimizing selection bias can be difficult; however, we note that the bias was minimal. The retrospective nature of the analysis as well as the lack of preoperative data makes it difficult to draw definitive conclusions regarding the effectiveness of the treatment. Players were excluded if they had undergone an additional elbow procedure at the time of surgery. Therefore, the results of this study may not be generalizable to a player undergoing ulnar nerve transposition with a concomitant UCL reconstruction or other elbow procedure. In addition, outcomes were limited to functional recall from patients as well as patient response rate. Furthermore, there were no cases of ulnar nerve decompression surgery; therefore, we could not compare performance and draw conclusions on the optimal surgical technique (transposition vs. decompression) for throwing athletes. Overall, four patients could not be contacted and four patients did not respond to our follow-up leaving less than 100% follow-up in a more limited patient population. However, given the migratory nature of this population (young age, relocation and new contact information) full follow-up can be difficult to achieve. Therefore, we feel our results well represent this patient population.
Conclusion
The results of our study indicate that ulnar nerve transposition surgery in throwing athletes allows athletes to return to throwing with low reoperation rates. However, more than half of the athletes in our analysis sustained an ipsilateral shoulder or elbow injury. Further investigation regarding outcomes in throwing athletes after ulnar nerve transposition surgery is warranted.
Disclosures
Michael G. Ciccotti: American Orthopaedic Society for Sports Medicine: Board or committee member; Arthrex, Inc.: Research support; Herodicus Sports Research Society: Board or committee member; Major League Baseball Team Physicians Association: Board or committee member; Orthopaedic Learning Center: Board or committee member Steven B. Cohen: American Orthopaedic Society for Sports Medicine: Board or committee member; Arthrex, Inc., Major League Baseball: Research support; CONMED Linvatec: Paid consultant; International Society of Arthroscopy, Knee Surgery, and Orthopaedic Sports Medicine: Board or committee member; Slack, INC.: Publishing royalties, financial or material support; Zimmer: IP royalties; Paid consultant; Paid presenter or speaker Christopher C. Dodson: Arthrex, Inc.: Paid consultant.
The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional review board approval was received from Thomas Jefferson University (control no. 18D.762).
References
- 1.Aoki M., Kanaya K., Aiki H., Wada T., Yamashita T., Ogiwara N. Cubital tunnel syndrome in adolescent baseball players: a report of six cases with 3- to 5-year follow-up. Arthroscopy. 2005;21:758. doi: 10.1016/j.arthro.2005.03.030. [DOI] [PubMed] [Google Scholar]
- 2.Black B.T., Barron O.A., Townsend P.F., Glickel S.Z., Eaton R.G. Stabilized subcutaneous ulnar nerve transposition with immediate range of motion. Long-term follow-up. J Bone Joint Surg Am. 2000;82:1544–1551. doi: 10.2106/00004623-200011000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Bruce J.R., Andrews J.R. Ulnar collateral ligament injuries in the throwing athlete. J Am Acad Orthop Surg. 2014;22:315–325. doi: 10.5435/JAAOS-22-05-315. [DOI] [PubMed] [Google Scholar]
- 4.Clain J.B., Vitale M.A., Ahmad C.S., Ruchelsman D.E. Ulnar nerve complications after ulnar collateral ligament reconstruction of the elbow: a systematic review. Am J Sports Med. 2019;47:1263–1269. doi: 10.1177/0363546518765139. [DOI] [PubMed] [Google Scholar]
- 5.Conti M.S., Camp C.L., Elattrache N.S., Altchek D.W., Dines J.S. Treatment of the ulnar nerve for overhead throwing athletes undergoing ulnar collateral ligament reconstruction. World J Orthop. 2016;7:650–656. doi: 10.5312/wjo.v7.i10.650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dowdle S.B., Chalmers P.N. Management of the ulnar nerve in throwing athletes. Curr Rev Musculoskelet Med. 2020;13:449–456. doi: 10.1007/s12178-020-09639-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dugas J., Chronister J., Cain E.L., Andrews J.R. Ulnar collateral ligament in the overhead athlete: a current review. Sports Med Arthrosc Rev. 2014;22:169–182. doi: 10.1097/JSA.0000000000000033. [DOI] [PubMed] [Google Scholar]
- 8.Erickson B.J., Chalmers P.N., D'Angelo J., Ma K., Romeo A.A. Performance and return to sport after ulnar nerve decompression/transposition among professional baseball players. Am J Sports Med. 2019;47:1124–1129. doi: 10.1177/0363546519829159. [DOI] [PubMed] [Google Scholar]
- 9.Erickson B.J., Harris J.D., Chalmers P.N., Bach B.R., Verma N.N., Bush-Joseph C.A. Ulnar collateral ligament reconstruction: anatomy, indications, techniques, and outcomes. Sports Health. 2015;7:511–517. doi: 10.1177/1941738115607208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harris J.D., Lintner D.M. Nerve injuries about the elbow in the athlete. Sports Med Arthrosc Rev. 2014;22:e7–e15. doi: 10.1097/JSA.0000000000000038. [DOI] [PubMed] [Google Scholar]
- 11.Kraeutler M.J., Ciccotti M.G., Dodson C.C., Frederick R.W., Cammarota B., Cohen S.B. Kerlan-Jobe Orthopaedic Clinic overhead athlete scores in asymptomatic professional baseball pitchers. J Shoulder Elbow Surg. 2013;22:329–332. doi: 10.1016/j.jse.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 12.Lyman S., Fleisig G.S., Waterbor J.W., Funkhouser E.M., Pulley L., Andrews J.R. Longitudinal study of elbow and shoulder pain in youth baseball pitchers. Med Sci Sports Exerc. 2001;33:1803–1810. doi: 10.1097/00005768-200111000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Pechan J., Julis I. The pressure measurement in the ulnar nerve. A contribution to the pathophysiology of the cubital tunnel syndrome. J Biomech. 1975;8:75–79. doi: 10.1016/0021-9290(75)90045-7. [DOI] [PubMed] [Google Scholar]
- 14.Shuai C., Hede Y., Shen L., Yuanming O., Hongjiang R., Cunyi F. Is routine ulnar nerve transposition necessary in open release of stiff elbows? Our experience and a literature review. Int Orthop. 2014;38:2289–2294. doi: 10.1007/s00264-014-2465-0. [DOI] [PubMed] [Google Scholar]
- 15.Staples J.R., Calfee R. Cubital tunnel syndrome: current concepts. J Am Acad Orthop Surg. 2017;25:e215–e224. doi: 10.5435/JAAOS-D-15-00261. [DOI] [PubMed] [Google Scholar]
- 16.Torg J.S., Pollack H., Sweterlitsch P. The effect of competitive pitching on the shoulders and elbows of preadolescent baseball players. Pediatrics. 1972;49:267–272. [PubMed] [Google Scholar]
- 17.Werner C.O., Ohlin P., Elmqvist D. Pressures recorded in ulnar neuropathy. Acta Orthop Scand. 1985;56:404–406. doi: 10.3109/17453678508994358. [DOI] [PubMed] [Google Scholar]
- 18.Yahya A., Malarkey A.R., Eschbaugh R.L., Bamberger H.B. Trends in the surgical treatment for cubital tunnel syndrome: a survey of members of the American Society for Surgery of the Hand. Hand (N Y) 2018;13:516–521. doi: 10.1177/1558944717725377. [DOI] [PMC free article] [PubMed] [Google Scholar]