Abstract
Background
Altered scapular motion is thought to be one of the factors associated with the development of symptomatic rotator cuff tears. However, the differences in kinematics and muscle activities of scapular upward/downward rotation between patients with symptomatic and asymptomatic tears are unclear. The purpose of this study was to compare the differences in kinematics and muscle activities of scapular rotation among patients with symptomatic and asymptomatic tears, and healthy individuals.
Methods
Twenty-three patients with rotator cuff tears and 9 healthy individuals (healthy group) participated in this study. Based on a visual analog scale (VAS, 0-100 mm), the patients were divided into symptomatic (13 patients; VAS ≥20 mm) and asymptomatic (10 patients; VAS <20 mm) groups. Scapular upward rotation was measured with a digital inclinometer. Elasticities of the upper trapezius, levator scapulae, and rhomboid major were assessed by using ultrasound real-time tissue elastography to quantify their muscle activities. All measurements were performed at 0°, 60°, 90°, and 120° of active arm elevation in the scapular plane.
Results
Scapular upward rotation was significantly less in the symptomatic group (9.4° ± 5.6°) compared with the asymptomatic group (15.7° ± 6.0°; P = .022) at 90° of arm elevation. The activity of the levator scapulae was significantly higher in the symptomatic group compared with the asymptomatic and healthy groups (P = .013 and P = .005, respectively) at 90° of arm elevation. The activity of the upper trapezius was significantly higher in the symptomatic group compared with the healthy group (P = .015) at 120° of arm elevation.
Conclusion
Patients with symptomatic rotator cuff tears showed less scapular upward rotation and higher activity of the levator scapulae at 90° of arm elevation compared to patients with asymptomatic rotator cuff tears.
Keywords: Rotator cuff tear, asymptomatic, scapular kinematics, muscle activity, upper trapezius, levator scapulae, rhomboid major, ultrasound elastography
Rotator cuff tear is a common shoulder disease among middle-aged and elderly people. The prevalence of tears has been reported to be at least 10% in the 50s and increase to over 30% in the 80s.41,63 Most of the patients with rotator cuff tears who come to a clinic suffer from severe shoulder pain, particularly during arm elevation. On the other hand, some rotator cuff tears are known to be asymptomatic in the general population.41,57,63 This indicates that the existence of rotator cuff tear itself is not necessarily a cause of pain. Patients with symptomatic rotator cuff tears often become asymptomatic with nonoperative treatment in the clinical setting.2,5,6,22,34,65 Nevertheless, factors associated with the development of pain is still unclear.
Alterations in scapular motion during arm elevation have been considered a potential mechanism for shoulder pain.29,45,52,55 Several previous studies reported that the altered scapular motion reduced subacromial space29,52,55 and increased subacromial contact pressure.45 These anatomical changes may contribute to development or progression of subacromial impingement, leading to shoulder pain during arm elevation. In patients with shoulder impingement, decreased scapular upward rotation has often been observed.16,37,56 A few studies have attempted to clarify the difference in scapular upward rotation between patients with symptomatic and asymptomatic rotator cuff tears by using x-ray images62 and 3D/2D registration techniques with biplane fluoroscopic images.32 However, these studies showed no statistically significant difference in scapular upward rotation between patients with symptomatic and asymptomatic tears. One of the reasons may be because these studies had small sample size.
Scapular upward rotation during arm elevation is coordinated by activities of the scapular upward rotators (ie, the upper trapezius and serratus anterior) and downward rotators (ie, the levator scapulae and rhomboid major).10,14,26,61 Any changes in the muscular coordination among the scapular upward and downward rotators may be considered to cause abnormalities in scapular upward rotation. For the scapular upward rotators, there is a consensus that patients with symptomatic tears show higher activity of the upper trapezius during arm elevation than those with asymptomatic tears.31,54 However, little information is available on the activities of the scapular downward rotators in patients with symptomatic and asymptomatic tears.54 The main reason for the lack of information may be that the scapular downward rotators are too deeply located to be investigated by surface electromyography, which is the gold standard methodology for assessing muscle activities.
Recently, another method for assessment of activities of the deeper-lying muscles using ultrasound real-time tissue elastography (RTE) has been established.21,44,53,64 RTE is capable of noninvasively estimating the elasticity of deeper-lying tissues from the strain of the tissue. Some previous studies reported that the elasticity of muscles in the shoulder girdle assessed by RTE increased with an increase in muscle contraction intensity and positively correlated with the EMG activities (r = 0.55-0.66).21,44
The purpose of this study was to compare the differences in scapular motion and parascapular muscle activities assessed by RTE during static arm elevation among patients with symptomatic and asymptomatic tear, and healthy individuals. We hypothesized that (1) symptomatic patients would demonstrate less scapular upward rotation and higher activities of the scapular upward and downward rotators as compared with asymptomatic patients and healthy individuals, and (2) no significant differences in scapular motion and parascapular muscle activities would be demonstrated between asymptomatic patients and healthy individuals.
Materials and methods
Subjects
Subjects were recruited from a convenience sample of patients with rotator cuff tears who visited the authors’ institution. The diagnosis of partial-thickness or full-thickness rotator cuff tears was established with magnetic resonance imaging. The size of full-thickness tear was classified into the following categories11: small <10 mm, medium 10-30 mm, large 30-50 mm, and massive >50 mm in width or length. Active and passive range of motion (ROM) measurements for shoulder flexion and external rotation with the arm adducted were performed with a goniometer.1 The inclusion criteria were patients with a partial- or full-thickness rotator cuff tears that involve only the supraspinatus tendon or multiple tendons. Patients with less than 120° of active shoulder flexion and a previous history of shoulder surgery, cervical radiculopathy, rheumatoid arthritis, or neuromuscular disease were excluded.
Twenty-three patients with rotator cuff tears who fulfill the criteria agreed to participate in this study. These patients were divided into symptomatic and asymptomatic groups based on the result of pain evaluation.31,54 Self-reported pain at rest and during shoulder motion were reported on a 100-mm visual analog scale (VAS) ranging from 0 (no pain) to 100 (worst imaginable pain).30 The symptomatic group consisted of 13 subjects was defined as the subject with the highest VAS score of ≥20 mm. The asymptomatic group consisted of 10 subjects was defined as the subject with the highest VAS score of <20 mm.
In addition, 12 healthy volunteers who were recruited through advertising in our institution participated in this study. The healthy group was defined as the subject without rotator cuff tear, any shoulder pain, and history of neck or shoulder injuries, cervical radiculopathy, rheumatoid arthritis, or neuromuscular disease. The absence of rotator cuff tear was confirmed with a combination of 5 physical examination including the full and empty can, external rotation resistance, lift-off, and belly-press tests and ultrasonography23,24. For the ultrasonography, the shoulder was scanned to display longitudinal images of the supraspinatus and infraspinatus tendons in B-mode imaging. The ultrasound scanning for the supraspinatus tendon was performed at the anterior edge of the superior facet of the greater tuberosity, and the ultrasound scanning for the infraspinatus tendon was performed at the middle facet of the greater tuberosity. The diagnosis of rotator cuff tear was established on the basis of the following criteria as described in a previous study: (1) flattening of peribursal fat, (2) loss of actual rotator cuff tendon, (3) surface irregularity of the greater tuberosity, and (4) effusion of the subacromial bursa.33 Subjects without any of the positive results for the 5 physical examinations and the 4 ultrasound findings was selected as the healthy group.
Approval for this study was obtained from the authors’ institutional review board. All participants received a verbal explanation of the testing procedure and signed an informed consent form to protect their rights.
Procedures for data collection
Subjects were seated in a height-adjustable chair without a backrest or armrests. The height of the chair was adjusted so that they can place their feet flat on the floor with bilateral hips and knees flexed at approximately 90°. Subjects were instructed to keep their eyes straight ahead in a relaxed position with their arms at the side of the body and then elevate the involved arm with the thumb pointing up in the scapular plane until reaching each target angle of arm elevation: 60°, 90°, and 120°. At each elevation angle, the subjects held their arms in the position for approximately 10 seconds and then returned to the rest position to minimize fatigue. The subjects adequately practiced before the task, and the examiner carefully confirmed that the subjects elevated their arms without lateral bending of trunk during a series of trials. The scapular plane was defined as 30° anterior to the frontal plane. The plane of elevation and arm elevation angle were verified with a goniometer, and a marked pole was used as a guide to maintain the arm position.
Data for scapular upward rotation and elasticities of the scapular upward and downward rotators were collected separately at each angle of arm elevation in the scapular plane: 0° (rest position), 60°, 90°, and 120°, with the order of the arm elevation angle randomized by using a random number generator (Microsoft Office Excel version 16; Microsoft, Redmond, WA, USA). The data collection was conducted on the side of rotator cuff tear in the symptomatic and asymptomatic groups and on the dominant side in the healthy group. All measurements were performed by a licensed physical therapist with 12 years of clinical experience, who was blinded to the patient’s group allocation.
Measurement of scapular upward rotation
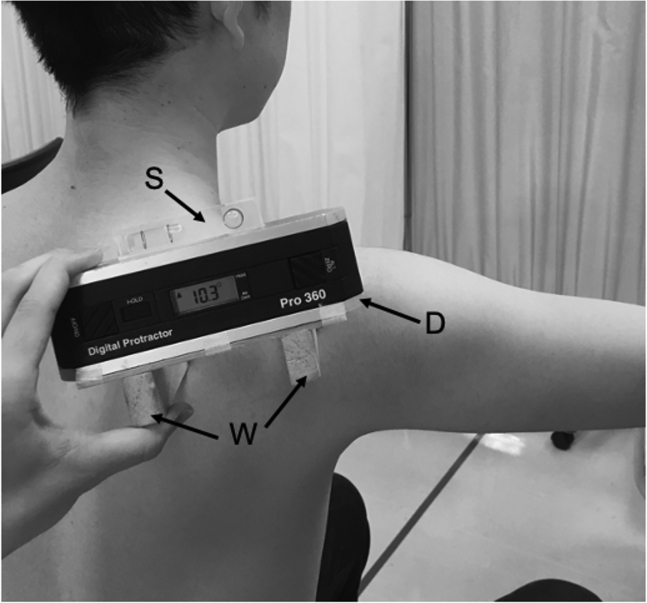
A digital inclinometer (Pro 360 Digital Protractor; M-D Building Products, Oklahoma City, OK, USA) was used for the measurement of scapular upward rotation. The inclinometer provides a real-time reading of angles from a horizontal reference and is designed to be accurate within 0.1° as reported by the manufacturer.35 Two wooden square rods were attached to the bottom of the inclinometer. Each rod is approximately 10 cm in length and one end of the rod is shaped in the form of Y. A spirit level was also attached to the top of the inclinometer (Fig. 1).
Figure 1.
Measurement of scapular upward rotation. A digital inclinometer with wooden square rods was placed along the medial and lateral aspect of the scapular spine. The inclination angle of the scapular spine with respect to the horizontal plane was measured to determine the amount of scapular upward rotation. S, spirit level; D, digital inclinometer; W, wooden square rods.
The examiner placed the inclinometer over the scapula with the subjects seated. The wooden square rods were located along the medial and lateral aspect of the scapular spine. The spirit level was used to avoid an anterior/posterior rotation of the body of the inclinometer about an axis parallel to the scapular spine. The inclination angle of the scapular spine with respect to the horizontal plane was measured to determine the amount of scapular upward rotation.27,35,60 The measurement was performed twice at each arm position, and the mean value of the two trials was used for the data analysis.
The clinical measurement of scapular upward rotation with a digital inclinometer has been validated by comparing with angular data using an electromagnetic tracking device (r = 0.74-0.92).27 In addition, many previous researches have demonstrated that this clinical measurement is a reliable procedure.27,35,58,60 In our pilot study of 20 healthy participants, the intraexaminer reliability for the measurement of scapular upward rotation was assessed using the intraclass correlation coefficient (ICC1,2), the standard error of the measure (SEM), and the minimal detectable change with 95% confidence (MDC95). The SEM was defined as the standard deviation multiplied by the square root of the ICC subtracted from 1. The ICC1,2 (SEM, MDC95) values of the scapular upward rotation with the arm at 0°, 60°, 90°, and 120° of arm elevation were 0.990 (0.4°, 1.1°), 0.994 (0.3°, 1.0°), 0.996 (0.3°, 0.8°), and 0.986 (0.6°, 1.6°), respectively.
Ultrasound RTE examination
A diagnostic ultrasound system (HI VISION Avius; Hitachi Aloka Medical Japan, Tokyo, Japan), with a linear array transducer (14–6 MHz EUP-L65; Hitachi Aloka Medical Japan), was used for the measurement of muscle elasticity. An acoustic coupler (EZU-TECPL1; Hitachi Aloka Medical, Japan) was attached to the head of the transducer with a plastic attachment (EZU-TEATC; Hitachi Aloka Medical Japan) as a reference material. The acoustic coupler (60 × 50 × 8 mm) is made of elastomer resin and has an elastic modulus of 22.6 ± 2.2 kPa. The ultrasound system is equipped with RTE, being capable of estimating elasticity of a target tissue from the strain of the tissue.
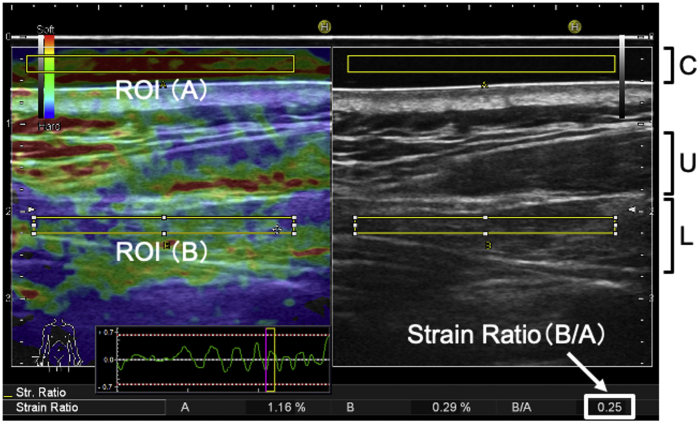
The elasticities of the upper trapezius, levator scapulae, and rhomboid major were measured with the subjects in a seated position. First, the examiner scanned the shoulder girdle to obtain a longitudinal axial B-mode image of each muscle. For scanning of the upper trapezius, the ultrasound transducer was placed at the area approximately 2 cm distal to the midpoint between the spinous process of C7 and the lateral edge of the acromion.21 For scanning of the levator scapulae, the ultrasound transducer was placed at the area approximately 2 cm distal to the midpoint between the superior angle of the scapula and the midpoint between the transverse processes of C1 and C4.21 For scanning of the rhomboid major, the ultrasound transducer was placed at the intermediate area between the midpoint from the inferior angle of the scapula to the spine triangle and the spinous process of T3.21 Then, the examiner applied repeated manual compression on the muscle with the ultrasound transducer. The frequency of the compression was adjusted from approximately 2 to 4 Hz by monitoring the strain graph which indicates time variation of the average strain. While applying the compression repeatedly, the color-coded RTE images were superimposed on the entire B-mode image, which automatically stored in the built-in memory with a frame rate of 15 frames per second (Fig. 2).
Figure 2.
The real-time tissue elastographic (RTE) image (left image) and the B-mode image (right image) for the measurement of the levator scapulae. The color code indicates the relative strain of the tissues, ranging from red (soft) to blue (hard). The region of interests (ROIs), which is represented as yellow rectangle, were individually set on the acoustic coupler (A) and the muscle (B). The depth of the ROIs was defined as approximately the middle two-thirds of the acoustic coupler and the muscle to avoid the boundary condition effect. The width of the ROI on the muscle was adjusted to coincide with that on the acoustic coupler. The strain ratio (B/A) was automatically calculated from the strains of the acoustic coupler (A) and the muscle (B) in the ROIs. C, coupler; U, the upper trapezius; L, the levator scapulae.
After the ultrasound scanning, the examiner randomly selected two RTE images and then individually set the rectangular region of interests on the acoustic coupler and the muscle in each RTE image. The strain values of the acoustic coupler (A) and the muscle (B) in the region of interests were measured by the built-in software. To quantitatively estimate the muscle elasticity, the “strain ratio (B/A)” was calculated from the ratio of the strain of the muscle (B) to that of the acoustic coupler (A). Lower value of the strain ratio indicated stiffer muscle because the strain of muscle with high elasticity is smaller than that with low elasticity when a stress is applied to the muscle.20,21,44 The mean value of two RTE images at each arm position was used for the data analysis.
Good to fair validity for the RTE measurement has been demonstrated by comparing between the strain ratios and EMG activities for the middle deltoid (r = −0.659) and upper trapezius (r = −0.554).21 These results suggest that the RTE is capable of noninvasively assessing the activities of the shoulder girdle muscles. In addition, our pilot study of 20 healthy participants showed the excellent intraexaminer reliability for the RTE measurements of the upper trapezius (ICC1,2 = 0.988-0.998, SEM = 0.05-0.15, MDC95 = 0.13-0.43), levator scapulae (ICC1,2 = 0.983-0.994, SEM = 0.04-0.10, MDC95 = 0.12-0.28), and rhomboid major (ICC1,2 = 0.959-0.989, SEM = 0.03-0.12, MDC95 = 0.08-0.34) at each angle of arm elevation.
Statistical analysis
The qualitative (ie, gender) and quantitative (ie, age, body mass index, and ROM) demographic data were compared among the 3 groups using a chi-square test and 1-way analysis of variance (ANOVA), respectively. When a statistically significant main effect was showed on ANOVA, post hoc testing was conducted with a Bonferroni correction. Side and type of rotator cuff tear and VAS score were compared between the symptomatic and asymptomatic groups using a chi-square test and an independent t test, respectively. Scapular upward rotation and the strain ratios of the scapular upward and downward rotators at each angle of arm elevation were compared among the 3 groups using 1-way ANOVA, and a Bonferroni correction was used as post hoc testing. All statistical analyses were performed with a statistical analysis software package (SPSS version 25; IBM, Armonk, NY, USA). The statistical significance level was set at 0.05.
To determine the appropriate sample size, a post hoc power analysis for the 1-way ANOVA was performed using a statistical analysis software package (G∗Power version 3.1; Heinrich Hein University, Düsseldorf, Germany). The power (1-β) was calculated using the sample size of 35, the α level of .05, and the effect size (d) which was established from mean and standard deviation values of each group.
Results
The demographic data of each group are summarized in Table I. The mean age in the asymptomatic group was significantly higher than that in the healthy group (P = .013). The mean ROM for active and passive flexion in the healthy group were significantly greater than those in the other 2 groups (symptomatic, P = .003; asymptomatic, P = .038) for active motion and in the symptomatic group (P = .007) for passive motion. The mean VAS score for motion in the symptomatic group was significantly higher than that in the asymptomatic group (P < .001).
Table I.
Demographic data of each group
| Symptomatic group | Asymptomatic group | Healthy group | P value | |
|---|---|---|---|---|
| Number of subjects, n | 13 | 10 | 12 | |
| Dominant side, right/left, n | 13/0 | 10/0 | 12/0 | |
| Gender, male/female, n | 10/3 | 3/7 | 5/7 | .058 |
| Age, mean ± SD, y | 66 ± 7 | 72 ± 8∗ | 62 ± 8 | .016 |
| BMI, mean ± SD, kg/m2 | 24.9 ± 4.1 | 23.7 ± 2.9 | 23.0 ± 2.2 | .337 |
| ROM, mean ± SD, degree | ||||
| Active flexion | 144 ± 16∗ | 147 ± 18∗ | 164 ± 8 | .004 |
| Passive flexion | 152 ± 15∗ | 156 ± 16 | 168 ± 8 | .011 |
| Passive external rotation | 53 ± 9 | 53 ± 9 | 60 ± 4 | .067 |
| Side of rotator cuff tear, right/left, n | 9/4 | 8/2 | .463 | |
| Type of rotator cuff tear, n | .417 | |||
| Partial thickness | 6 | 2 | ||
| Full thickness | ||||
| Small (<10 mm) | 0 | 0 | ||
| Medium (10-30 mm) | 4 | 5 | ||
| Large (30-50 mm) | 3 | 3 | ||
| Massive (>50 mm) | 0 | 0 | ||
| Involved tendon, n | .299 | |||
| SSP | 9 | 3 | ||
| SSP + ISP | 1 | 2 | ||
| SSP + SSC | 1 | 1 | ||
| SSP + ISP + SSC | 2 | 4 | ||
| VAS score, mean ± SD, mm | ||||
| Rest | 12 ± 25 | 1 ± 3 | .120 | |
| Motion | 55 ± 20† | 9 ± 8 | <.001 |
SD, standard deviation; BMI, body mass index; ROM, range of motion; SSP, supraspinatus; ISP, infraspinatus; SSC, subscapularis; VAS, visual analog scale.
Significant difference compared with healthy group.
Significant difference compared with asymptomatic group.
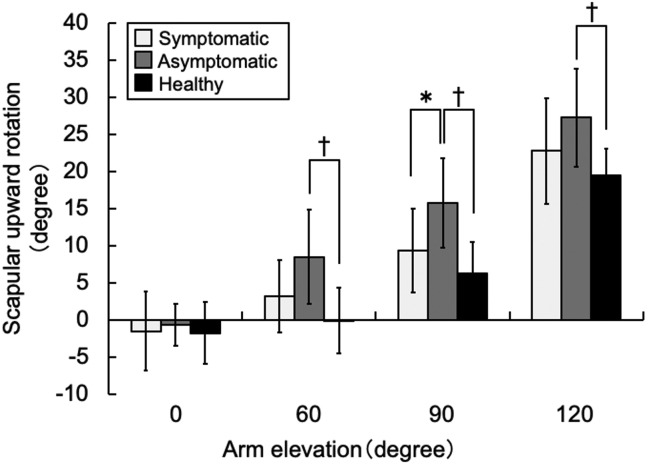
The mean and standard deviation values of scapular upward rotation and the strain ratio of 3 muscles at each angle of arm elevation are shown in Table II. For scapular upward rotation, 1-way ANOVA showed a statistically significant main effect at 60° (F2,32 = 7.43; P = .002), 90° (F2,32 = 8.99; P = .001), and 120° (F2,32 = 4.68; P = .017) of arm elevation, but no main effect was found at rest (F2,32 = 0.17; P = .842). The scapular upward rotation in the asymptomatic group was significantly greater than that in the healthy group at 60° (8.5 ± 6.4° vs. −0.1 ± 4.4°; P = .002), 90° (15.7 ± 6.0° vs. 6.3 ± 4.2°; P = .001), and 120° (27.2 ± 6.6° vs. 19.4 ± 3.6°; P = .013) of arm elevation (Fig. 3). At 90° of arm elevation, the scapular upward rotation in the symptomatic group was significantly less than that in the asymptomatic group (9.4 ± 5.6°; P = .022) (Fig. 3).
Table II.
Mean and standard deviation values of scapular upward rotation and the strain ratio of 3 muscles
| Variables | Group | Arm elevation |
|||
|---|---|---|---|---|---|
| 0° | 60° | 90° | 120° | ||
| Scapular upward rotation, degree | Symptomatic | −1.5 ± 5.3 | 3.2 ± 4.9 | 9.4 ± 5.6 | 22.8 ± 7.1 |
| Asymptomatic | −0.7 ± 2.8 | 8.5 ± 6.4 | 15.7 ± 6.0 | 27.2 ± 6.6 | |
| Healthy | −1.8 ± 4.1 | −0.1 ± 4.4 | 6.3 ± 4.2 | 19.4 ± 3.6 | |
| Upper trapezius, strain ratio | Symptomatic | 4.83 ± 2.85 | 2.49 ± 1.31 | 1.77 ± 0.99 | 0.90 ± 0.58 |
| Asymptomatic | 4.26 ± 2.03 | 2.44 ± 1.44 | 1.62 ± 0.67 | 1.68 ± 1.03 | |
| Healthy | 3.67 ± 1.23 | 2.34 ± 1.21 | 1.93 ± 1.27 | 1.93 ± 0.95 | |
| Levator scapulae, strain ratio | Symptomatic | 3.01 ± 1.66 | 1.08 ± 0.97 | 0.45 ± 0.26 | 0.52 ± 0.44 |
| Asymptomatic | 2.61 ± 1.81 | 1.41 ± 0.74 | 1.05 ± 0.34 | 1.05 ± 0.80 | |
| Healthy | 1.66 ± 0.81 | 0.95 ± 0.47 | 1.08 ± 0.67 | 1.02 ± 0.37 | |
| Rhomboid major, strain ratio | Symptomatic | 3.57 ± 1.01 | 1.12 ± 0.59 | 0.59 ± 0.28 | 0.42 ± 0.26 |
| Asymptomatic | 2.80 ± 1.52 | 1.41 ± 1.74 | 0.82 ± 0.62 | 0.49 ± 0.16 | |
| Healthy | 3.11 ± 1.15 | 1.51 ± 0.74 | 0.67 ± 0.29 | 0.56 ± 0.30 | |
Values represent mean ± standard deviation.
Figure 3.
Comparison of scapular upward rotation among the 3 groups. The bars and error bars indicate the mean value and standard deviation, respectively. Asterisk (∗) indicates a significant difference between the symptomatic and asymptomatic groups (P < .05). Dagger (†) indicates a significant difference between the asymptomatic and healthy groups (P < .05).
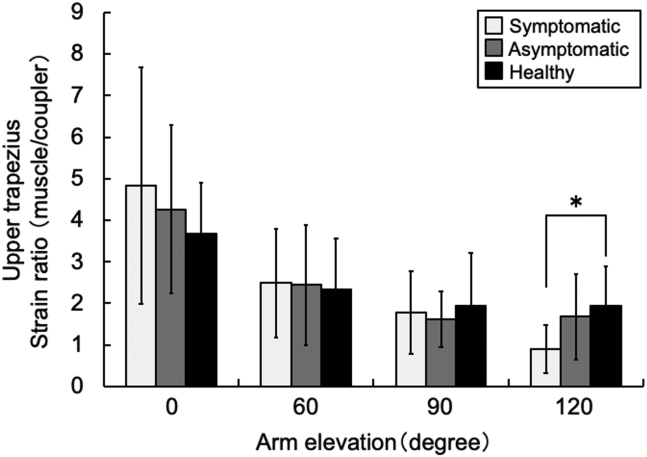
For the strain ratio of the upper trapezius, 1-way ANOVA showed a statistically significant main effect at 120° of arm elevation (F2,32 = 4.90; P = .014), but no main effects were found at rest (F2,32 = 0.89; P = .419), 60° (F2,32 = 0.41; P = .960) and 90° of arm elevation (F2,32 = 0.25; P = .779). The strain ratio of the upper trapezius in the symptomatic group (0.90 ± 0.58) was significantly lower than that in the healthy group (1.93 ± 0.95) at 120° of arm elevation (P = .015) (Fig. 4).
Figure 4.
Comparison of the strain ratio of the upper trapezius among the 3 groups. The bars and error bars indicate the mean value and standard deviation, respectively. Asterisk (∗) indicates a significant difference between the symptomatic and healthy groups (P < .05).
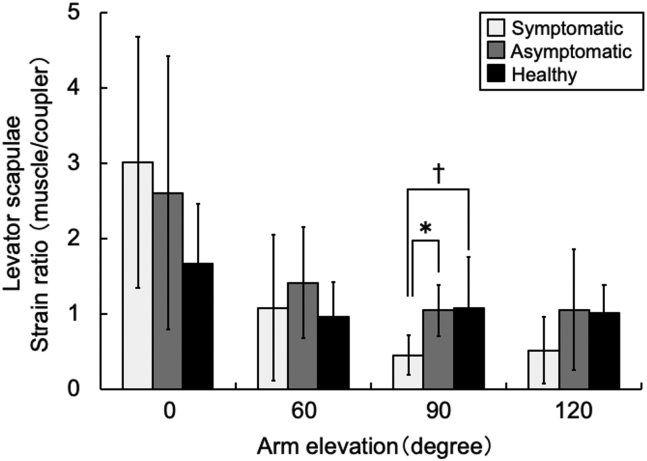
For the strain ratio of the levator scapulae, 1-way ANOVA showed a statistically significant main effect at 90° (F2,32 = 7.24; P = .003) and 120° (F2,32 = 3.68; P = .036) of arm elevation, but no main effects were found at rest (F2,32 = 2.69; P = .083), 60° of arm elevation (F2,32 = 1.04; P = .364). The strain ratio of the levator scapulae in the symptomatic group (0.45 ± 0.26) was significantly lower than that in the asymptomatic (1.05 ± 0.34) and healthy (1.08 ± 0.67) groups at 90° of arm elevation (P = .013 and P = .005, respectively) (Fig. 5).
Figure 5.
Comparison of the strain ratio of the levator scapulae among the 3 groups. The bars and error bars indicate the mean value and standard deviation, respectively. Asterisk (∗) indicates a significant difference between the symptomatic and asymptomatic groups (P < .05). Dagger (†) indicates a significant difference between the symptomatic and healthy groups (P < .05).
For the strain ratio of the rhomboid major, there was no statistically significant main effect at all elevation angles (Fig. 6).
Figure 6.
Comparison of the strain ratio of the rhomboid major among the 3 groups. There were no significant differences among the 3 groups.
The post hoc power analysis indicated that the power were 0.97 and 0.93 to detect significant differences in scapular upward rotation (effect size, 0.75) and the strain ratio of the levator scapulae (effect size, 0.67) at 90°, respectively.
Discussion
Alterations in scapular motion during arm elevation have been commonly observed in patients with various shoulder diseases.17,37,38,46,56 However, it remains unclear whether the altered scapular motion is associated with pain in patients with symptomatic rotator cuff tears. Based on our findings, the patterns of scapular upward rotation and activities of the scapular upward and downward rotators during static arm elevation are different among patients with symptomatic and asymptomatic rotator cuff tears, and healthy individuals. These changes in scapular motion are likely to be related to symptoms. However, we cannot tell from this study whether these changes are the cause or the result of symptomatic cuff tears.
The present study demonstrated that the scapular upward rotation in the asymptomatic group was significantly greater than that in the healthy group at 60°, 90°, and 120° of arm elevation. This result suggests that the increased scapular upward rotation might be caused by the dysfunction in rotator cuff-deficient shoulders. Several cadaveric studies reported that defects of the supraspinatus and infraspinatus tendons resulted in a reduction in glenohumeral abduction torque.19,43 In vivo, some investigations demonstrated that scapular upward rotation during arm elevation significantly increased after a suprascapular nerve block39,51 and muscle fatigue task,15,28 which produce experimental dysfunction of the rotator cuff muscles. Therefore, scapular upward rotation seemed to have increased group at 60°, 90°, and 120° of arm elevation to compensate for the loss of glenohumeral motion in patients with asymptomatic rotator cuff tears.
On the other hand, there were no statistically significant differences in scapular upward rotation between the symptomatic and healthy groups at all elevation angles. Previous studies showed increased scapular upward rotation in patients with rotator cuff tears as compared with healthy individuals by using x-ray images,12 electromagnetic tracking system,40 and biplane images.59 One of the reasons for the discrepancy between our result and previous findings may be that different devices were used for measurement of scapular motion. The other reason may be the heterogeneity of subjects. In the previous studies, the pain level of the patients was unclear. Therefore, both symptomatic and asymptomatic rotator cuff tears may be included in the patient group.
The present study also demonstrated that the symptomatic group presented with significantly less scapular upward rotation at 90° of arm elevation as compared with the asymptomatic group. It has been found that the minimum distance between the coracoacromial arch and the rotator cuff insertion occurs near or below 90° of arm elevation.3,18,36,50 Some previous studies reported that scapular upward rotation could change subacromial contact pressure45 and space52 at a certain angle of arm elevation. Seitz et al52 demonstrated that the acromiohumeral distance at 90° of arm elevation increased with manual assistance for scapular upward rotation and posterior tilt. An increase in scapular upward rotation at 90° of arm elevation could important for avoiding subacromial impingement. Decreased scapular upward rotation at 90° of arm elevation in patients with symptomatic rotator cuff tears might be related to the development of pain by mechanical compression of the rotator cuff.
We also attempted to compare the differences in activities of the scapular upward and downward rotators among patients with symptomatic and asymptomatic rotator cuff tears, and healthy individuals by using ultrasound RTE. The strain ratio of the upper trapezius in the symptomatic group was significantly lower than that in the healthy group at 120° of arm elevation. This finding means that the symptomatic group showed higher activity of the upper trapezius, although there was no statistically significant difference between the symptomatic and asymptomatic groups. Consistent with our result, previous studies reported that higher activity31,54 and longer duration of activity13 for the upper trapezius during shoulder motion were presented in patients with symptomatic rotator cuff tears. The higher activity of the upper trapezius would increase upward rotation of the scapula. Nevertheless, no statistically significant increase in scapular upward rotation was showed in symptomatic group. This might be because the function of the upper trapezius as an upward rotator was diminished by increased activity of the levator scapulae in the middle range of elevation (90° to 120° of arm elevation). Furthermore, the upper trapezius is speculated to elevate the scapula by working together with the levator scapulae. The abnormal motion elevating the scapula during arm elevation, which is known as the “shrug sign”, is a clinical finding commonly observed in patients with symptomatic rotator cuff tears.4,25 The coactivation of the upper trapezius and levator scapulae could cause the “shrug sign” in patients with symptomatic rotator cuff tears.
The strain ratio of the levator scapulae in the symptomatic group was significantly lower than that in the asymptomatic group at 90° of arm elevation. This finding means that the symptomatic group showed higher activity of the levator scapulae at 90° of arm elevation, which is the same angle as the angle where significantly less scapular upward rotation was observed. The levator scapulae is generally believed to rotate the scapula downwardly on the basis of anatomical location. Therefore, excessive activation of the levator scapulae can impede normal scapular upward rotation during arm elevation. In the present study, decreased scapular upward rotation at 90° of arm elevation in patients with symptomatic tears might be influenced by increased activity of the levator scapulae.
We assume that decrease in scapular upward rotation may be associated with the pain in patients with symptomatic rotator cuff tears. Further studies should determine the effect of interventions to improve the decreased scapular upward rotation during arm elevation. In addition, a highlight of this study is to compare the different activation patterns of the scapular downward rotators between patients with symptomatic and asymptomatic rotator cuff tears while there is a lack of research evaluating these muscle activities. In clinical practice, exercises to facilitate the activation of the scapular upward rotators have been widely recommended with the aim of improving decreased scapular upward rotation.9,47, 48, 49 Our findings suggest the need to focus more on minimizing the activity of the levator scapulae to improve decreased scapular upward rotation.
There were several limitations in the present study. First, the asymptomatic group was not age-matched to the healthy group. The age difference may have been a potential confounding factor related to scapular kinematics. However, a previous study demonstrated that there were no statistically significant differences in activities of the scapular upward rotators between young and elderly adults.42 Second, the sample size was small. Although post hoc power analysis indicated sufficient statistical power to detect significant differences in scapular upward rotation and the strain ratio of the levator scapulae at 90°, a study in large size of subjects might reveal the difference which was not found in this study. Third, the measurements in this study were conducted during static arm elevation. A previous study reported that the static measures favorably compared with dynamic measures using an electromagnetic tracking device.27 However, the findings of this study may be different if data are collected during dynamic arm elevation. Fourth, scapular upward rotation might include other joint motions such as the thoracic and lumber motions because the inclination angle of the scapular spine relative to the horizontal plane was measured. However, it has been validated that the scapular measurement using this technique is comparable with dynamic measurement using an electromagnetic tracking device in a three-dimensional setting.27 Therefore, the influence of other joint motions would be minimal. Fifth, other biomechanical factors related to altered scapular kinematics such as pectoralis minor length8 and posterior shoulder tightness7 were not considered in this study. These confounding factors might affect the outcome of this study. Sixth, the RTE measurement in the present study analyzed only a limited area of the muscle on the B-mode image. It may not completely represent the state of the entire muscle. However, the EMG measurement, which is the gold standard methodology for assessing muscle activities, has the same disadvantage as the RTE measurement. Finally, we did not investigate the activity of the serratus anterior. The serratus anterior is one of the important muscles that upwardly rotate the scapula during arm elevation.14 However, it was difficult to do an ultrasound scan to accurately identify the location of the serratus anterior at each angle of arm elevation in the RTE measurement.
Conclusion
In patients with symptomatic rotator cuff tears, scapular upward rotation was significantly less at 90° of arm elevation as compared with patients with asymptomatic rotator cuff tears. The decreased scapular upward rotation might be influenced by increased activity of the levator scapulae. These findings suggest that the alterations in scapular upward rotation and activity of the levator scapulae may be related to the development of pain in patients with rotator cuff tears.
Disclaimer
The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Acknowledgments
This work was supported by JSPS KAKENHI (grant no. JP19K19786). The authors would like to thank Hitachi Aloka Medical Japan for technical advice.
Footnotes
This study was approved by the Ethical Committee of Tohoku University Graduate School of Medicine (study no. 2014-1-93).
References
- 1.Barnes C.J., Van Steyn S.J., Fischer R.A. The effects of age, sex, and shoulder dominance on range of motion of the shoulder. J Shoulder Elbow Surg. 2001;10:242–246. doi: 10.1067/mse.2001.115270. [DOI] [PubMed] [Google Scholar]
- 2.Baydar M., Akalin E., El O., Gulbahar S., Bircan C., Akgul O. The efficacy of conservative treatment in patients with full-thickness rotator cuff tears. Rheumatol Int. 2009;29:623–628. doi: 10.1007/s00296-008-0733-2. [DOI] [PubMed] [Google Scholar]
- 3.Bey M.J., Brock S.K., Beierwaltes W.N., Zauel R., Kolowich P.A., Lock T.R. In vivo measurement of subacromial space width during shoulder elevation: technique and preliminary results in patients following unilateral rotator cuff repair. Clin Biomech (Bristol, Avon) 2007;22:767–773. doi: 10.1016/j.clinbiomech.2007.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blevins F.T., Hayes W.M., Warren R.F. Rotator cuff injury in contact athletes. Am J Sports Med. 1996;24:263–267. doi: 10.1177/036354659602400303. [DOI] [PubMed] [Google Scholar]
- 5.Boorman R.S., More K.D., Hollinshead R.M., Wiley J.P., Brett K., Mohtadi N.G. The rotator cuff quality-of-life index predicts the outcome of nonoperative treatment of patients with a chronic rotator cuff tear. J Bone Joint Surg Am. 2014;96:1883–1888. doi: 10.2106/JBJS.M.01457. [DOI] [PubMed] [Google Scholar]
- 6.Boorman R.S., More K.D., Hollinshead R.M., Wiley J.P., Mohtadi N.G., Lo I.K.Y. What happens to patients when we do not repair their cuff tears? Five-year rotator cuff quality-of-life index outcomes following nonoperative treatment of patients with full-thickness rotator cuff tears. J Shoulder Elbow Surg. 2018;27:444–448. doi: 10.1016/j.jse.2017.10.009. [DOI] [PubMed] [Google Scholar]
- 7.Borich M.R., Bright J.M., Lorello D.J., Cieminski C.J., Buisman T., Ludewig P.M. Scapular angular positioning at end range internal rotation in cases of glenohumeral internal rotation deficit. J Orthop Sports Phys Ther. 2006;36:926–934. doi: 10.2519/jospt.2006.2241. [DOI] [PubMed] [Google Scholar]
- 8.Borstad J.D., Ludewig P.M. The effect of long versus short pectoralis minor resting length on scapular kinematics in healthy individuals. J Orthop Sports Phys Ther. 2005;35:227–238. doi: 10.2519/jospt.2005.35.4.227. [DOI] [PubMed] [Google Scholar]
- 9.Castelein B., Cagnie B., Parlevliet T., Cools A. Serratus anterior or pectoralis minor: Which muscle has the upper hand during protraction exercises? Man Ther. 2016;22:158–164. doi: 10.1016/j.math.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 10.Castelein B., Cagnie B., Parlevliet T., Cools A. Superficial and Deep Scapulothoracic Muscle Electromyographic Activity During Elevation Exercises in the Scapular Plane. J Orthop Sports Phys Ther. 2016;46:184–193. doi: 10.2519/jospt.2016.5927. [DOI] [PubMed] [Google Scholar]
- 11.Cofield R.H. Rotator cuff disease of the shoulder. J Bone Joint Surg Am. 1985;67:974–979. [PubMed] [Google Scholar]
- 12.Deutsch A., Altchek D.W., Schwartz E., Otis J.C., Warren R.F. Radiologic measurement of superior displacement of the humeral head in the impingement syndrome. J Shoulder Elbow Surg. 1996;5:186–193. doi: 10.1016/s1058-2746(05)80004-7. [DOI] [PubMed] [Google Scholar]
- 13.Duc C., Pichonnaz C., Bassin J.P., Farron A., Jolles B.M., Aminian K. Evaluation of muscular activity duration in shoulders with rotator cuff tears using inertial sensors and electromyography. Physiol Meas. 2014;35:2389–2400. doi: 10.1088/0967-3334/35/12/2389. [DOI] [PubMed] [Google Scholar]
- 14.Dvir Z., Berme N. The shoulder complex in elevation of the arm: a mechanism approach. J Biomech. 1978;11:219–225. doi: 10.1016/0021-9290(78)90047-7. [DOI] [PubMed] [Google Scholar]
- 15.Ebaugh D.D., McClure P.W., Karduna A.R. Scapulothoracic and glenohumeral kinematics following an external rotation fatigue protocol. J Orthop Sports Phys Ther. 2006;36:557–571. doi: 10.2519/jospt.2006.2189. [DOI] [PubMed] [Google Scholar]
- 16.Endo K., Ikata T., Katoh S., Takeda Y. Radiographic assessment of scapular rotational tilt in chronic shoulder impingement syndrome. J Orthop Sci. 2001;6:3–10. doi: 10.1007/s007760170017. [DOI] [PubMed] [Google Scholar]
- 17.Fayad F., Roby-Brami A., Yazbeck C., Hanneton S., Lefevre-Colau M.M., Gautheron V. Three-dimensional scapular kinematics and scapulohumeral rhythm in patients with glenohumeral osteoarthritis or frozen shoulder. J Biomech. 2008;41:326–332. doi: 10.1016/j.jbiomech.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 18.Giphart J.E., van der Meijden O.A., Millett P.J. The effects of arm elevation on the 3-dimensional acromiohumeral distance: a biplane fluoroscopy study with normative data. J Shoulder Elbow Surg. 2012;21:1593–1600. doi: 10.1016/j.jse.2011.11.023. [DOI] [PubMed] [Google Scholar]
- 19.Halder A.M., O'Driscoll S.W., Heers G., Mura N., Zobitz M.E., An K.N. Biomechanical comparison of effects of supraspinatus tendon detachments, tendon defects, and muscle retractions. J Bone Joint Surg Am. 2002;84-A:780–785. doi: 10.2106/00004623-200205000-00013. [DOI] [PubMed] [Google Scholar]
- 20.Ishikawa H., Muraki T., Morise S., Sekiguchi Y., Yamamoto N., Itoi E. Changes in stiffness of the dorsal scapular muscles before and after computer work: a comparison between individuals with and without neck and shoulder complaints. Eur J Appl Physiol. 2017;117:179–187. doi: 10.1007/s00421-016-3510-z. [DOI] [PubMed] [Google Scholar]
- 21.Ishikawa H., Muraki T., Sekiguchi Y., Ishijima T., Morise S., Yamamoto N. Noninvasive assessment of the activity of the shoulder girdle muscles using ultrasound real-time tissue elastography. J Electromyogr Kinesiol. 2015;25:723–730. doi: 10.1016/j.jelekin.2015.07.010. [DOI] [PubMed] [Google Scholar]
- 22.Itoi E., Tabata S. Conservative treatment of rotator cuff tears. Clin Orthop Relat Res. 1992:165–173. [PubMed] [Google Scholar]
- 23.Jain N.B., Fan R., Higgins L.D., Kuhn J.E., Ayers G.D. Does My Patient With Shoulder Pain Have a Rotator Cuff Tear?: A Predictive Model From the ROW Cohort. Orthop J Sports Med. 2018;6 doi: 10.1177/2325967118784897. 2325967118784897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jain N.B., Luz J., Higgins L.D., Dong Y., Warner J.J., Matzkin E. The Diagnostic Accuracy of Special Tests for Rotator Cuff Tear: The ROW Cohort Study. Am J Phys Med Rehabil. 2017;96:176–183. doi: 10.1097/PHM.0000000000000566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jia X., Ji J.H., Petersen S.A., Keefer J., McFarland E.G. Clinical evaluation of the shoulder shrug sign. Clin Orthop Relat Res. 2008;466:2813–2819. doi: 10.1007/s11999-008-0331-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Johnson G., Bogduk N., Nowitzke A., House D. Anatomy and actions of the trapezius muscle. Clin Biomech (Bristol, Avon) 1994;9:44–50. doi: 10.1016/0268-0033(94)90057-4. [DOI] [PubMed] [Google Scholar]
- 27.Johnson M.P., McClure P.W., Karduna A.R. New method to assess scapular upward rotation in subjects with shoulder pathology. J Orthop Sports Phys Ther. 2001;31:81–89. doi: 10.2519/jospt.2001.31.2.81. [DOI] [PubMed] [Google Scholar]
- 28.Joshi M., Thigpen C.A., Bunn K., Karas S.G., Padua D.A. Shoulder external rotation fatigue and scapular muscle activation and kinematics in overhead athletes. J Athl Train. 2011;46:349–357. doi: 10.4085/1062-6050-46.4.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Karduna A.R., Kerner P.J., Lazarus M.D. Contact forces in the subacromial space: effects of scapular orientation. J Shoulder Elbow Surg. 2005;14:393–399. doi: 10.1016/j.jse.2004.09.001. [DOI] [PubMed] [Google Scholar]
- 30.Kelly A.M. Does the clinically significant difference in visual analog scale pain scores vary with gender, age, or cause of pain? Acad Emerg Med. 1998;5:1086–1090. doi: 10.1111/j.1553-2712.1998.tb02667.x. [DOI] [PubMed] [Google Scholar]
- 31.Kelly B.T., Williams R.J., Cordasco F.A., Backus S.I., Otis J.C., Weiland D.E. Differential patterns of muscle activation in patients with symptomatic and asymptomatic rotator cuff tears. J Shoulder Elbow Surg. 2005;14:165–171. doi: 10.1016/j.jse.2004.06.010. [DOI] [PubMed] [Google Scholar]
- 32.Kijima T., Matsuki K., Ochiai N., Yamaguchi T., Sasaki Y., Hashimoto E. In vivo 3-dimensional analysis of scapular and glenohumeral kinematics: comparison of symptomatic or asymptomatic shoulders with rotator cuff tears and healthy shoulders. J Shoulder Elbow Surg. 2015;24:1817–1826. doi: 10.1016/j.jse.2015.06.003. [DOI] [PubMed] [Google Scholar]
- 33.Koike Y., Sano H., Kita A., Itoi E. Symptomatic rotator cuff tears show higher radioisotope uptake on bone scintigraphy compared with asymptomatic tears. Am J Sports Med. 2013;41:2028–2033. doi: 10.1177/0363546513494741. [DOI] [PubMed] [Google Scholar]
- 34.Kuhn J.E., Dunn W.R., Sanders R., An Q., Baumgarten K.M., Bishop J.Y. Effectiveness of physical therapy in treating atraumatic full-thickness rotator cuff tears: a multicenter prospective cohort study. J Shoulder Elbow Surg. 2013;22:1371–1379. doi: 10.1016/j.jse.2013.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Laudner K.G., Stanek J.M., Meister K. Differences in scapular upward rotation between baseball pitchers and position players. Am J Sports Med. 2007;35:2091–2095. doi: 10.1177/0363546507305098. [DOI] [PubMed] [Google Scholar]
- 36.Lawrence R.L., Schlangen D.M., Schneider K.A., Schoenecker J., Senger A.L., Starr W.C. Effect of glenohumeral elevation on subacromial supraspinatus compression risk during simulated reaching. J Orthop Res. 2017;35:2329–2337. doi: 10.1002/jor.23515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ludewig P.M., Cook T.M. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys Ther. 2000;80:276–291. [PubMed] [Google Scholar]
- 38.McClure P.W., Michener L.A., Karduna A.R. Shoulder function and 3-dimensional scapular kinematics in people with and without shoulder impingement syndrome. Phys Ther. 2006;86:1075–1090. [PubMed] [Google Scholar]
- 39.McCully S.P., Suprak D.N., Kosek P., Karduna A.R. Suprascapular nerve block disrupts the normal pattern of scapular kinematics. Clin Biomech (Bristol, Avon) 2006;21:545–553. doi: 10.1016/j.clinbiomech.2006.02.001. [DOI] [PubMed] [Google Scholar]
- 40.Mell A.G., LaScalza S., Guffey P., Ray J., Maciejewski M., Carpenter J.E. Effect of rotator cuff pathology on shoulder rhythm. J Shoulder Elbow Surg. 2005;14:58S–64S. doi: 10.1016/j.jse.2004.09.018. [DOI] [PubMed] [Google Scholar]
- 41.Minagawa H., Yamamoto N., Abe H., Fukuda M., Seki N., Kikuchi K. Prevalence of symptomatic and asymptomatic rotator cuff tears in the general population: From mass-screening in one village. J Orthop. 2013;10:8–12. doi: 10.1016/j.jor.2013.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Morise S., Muraki T., Ishikawa H., Izumi S.I. Age-Related Changes in Morphology and Function of Scapular Muscles in Asymptomatic People. PM R. 2017;9:892–900. doi: 10.1016/j.pmrj.2017.01.006. [DOI] [PubMed] [Google Scholar]
- 43.Mura N., O'Driscoll S.W., Zobitz M.E., Heers G., Jenkyn T.R., Chou S.M. The effect of infraspinatus disruption on glenohumeral torque and superior migration of the humeral head: a biomechanical study. J Shoulder Elbow Surg. 2003;12:179–184. doi: 10.1067/mse.2003.9. [DOI] [PubMed] [Google Scholar]
- 44.Muraki T., Ishikawa H., Morise S., Yamamoto N., Sano H., Itoi E. Ultrasound elastography-based assessment of the elasticity of the supraspinatus muscle and tendon during muscle contraction. J Shoulder Elbow Surg. 2015;24:120–126. doi: 10.1016/j.jse.2014.04.012. [DOI] [PubMed] [Google Scholar]
- 45.Muraki T., Yamamoto N., Sperling J.W., Steinmann S.P., Cofield R.H., An K.N. The effect of scapular position on subacromial contact behavior: a cadaver study. J Shoulder Elbow Surg. 2017;26:861–869. doi: 10.1016/j.jse.2016.10.009. [DOI] [PubMed] [Google Scholar]
- 46.Ogston J.B., Ludewig P.M. Differences in 3-dimensional shoulder kinematics between persons with multidirectional instability and asymptomatic controls. Am J Sports Med. 2007;35:1361–1370. doi: 10.1177/0363546507300820. [DOI] [PubMed] [Google Scholar]
- 47.Park K.M., Cynn H.S., Yi C.H., Kwon O.Y. Effect of isometric horizontal abduction on pectoralis major and serratus anterior EMG activity during three exercises in subjects with scapular winging. J Electromyogr Kinesiol. 2013;23:462–468. doi: 10.1016/j.jelekin.2012.11.013. [DOI] [PubMed] [Google Scholar]
- 48.Piraua A.L., Pitangui A.C., Silva J.P., Pereira dos Passos M.H., Alves de Oliveira V.M., Batista Lda S. Electromyographic analysis of the serratus anterior and trapezius muscles during push-ups on stable and unstable bases in subjects with scapular dyskinesis. J Electromyogr Kinesiol. 2014;24:675–681. doi: 10.1016/j.jelekin.2014.05.009. [DOI] [PubMed] [Google Scholar]
- 49.Pizzari T., Wickham J., Balster S., Ganderton C., Watson L. Modifying a shrug exercise can facilitate the upward rotator muscles of the scapula. Clin Biomech (Bristol, Avon) 2014;29:201–205. doi: 10.1016/j.clinbiomech.2013.11.011. [DOI] [PubMed] [Google Scholar]
- 50.Roberts C.S., Davila J.N., Hushek S.G., Tillett E.D., Corrigan T.M. Magnetic resonance imaging analysis of the subacromial space in the impingement sign positions. J Shoulder Elbow Surg. 2002;11:595–599. doi: 10.1067/mse.2002.127095. [DOI] [PubMed] [Google Scholar]
- 51.San Juan J.G., Kosek P., Karduna A.R. Humeral head translation after a suprascapular nerve block. J Appl Biomech. 2013;29:371–379. doi: 10.1123/jab.29.4.371. [DOI] [PubMed] [Google Scholar]
- 52.Seitz A.L., McClure P.W., Finucane S., Ketchum J.M., Walsworth M.K., Boardman N.D. The scapular assistance test results in changes in scapular position and subacromial space but not rotator cuff strength in subacromial impingement. J Orthop Sports Phys Ther. 2012;42:400–412. doi: 10.2519/jospt.2012.3579. [DOI] [PubMed] [Google Scholar]
- 53.Shinohara M., Sabra K., Gennisson J.L., Fink M., Tanter M. Real-time visualization of muscle stiffness distribution with ultrasound shear wave imaging during muscle contraction. Muscle Nerve. 2010;42:438–441. doi: 10.1002/mus.21723. [DOI] [PubMed] [Google Scholar]
- 54.Shinozaki N., Sano H., Omi R., Kishimoto K.N., Yamamoto N., Tashiro M. Differences in muscle activities during shoulder elevation in patients with symptomatic and asymptomatic rotator cuff tears: analysis by positron emission tomography. J Shoulder Elbow Surg. 2014;23:e61–e67. doi: 10.1016/j.jse.2013.06.009. [DOI] [PubMed] [Google Scholar]
- 55.Solem-Bertoft E., Thuomas K.A., Westerberg C.E. The influence of scapular retraction and protraction on the width of the subacromial space. An MRI study. Clin Orthop Relat Res. 1993:99–103. [PubMed] [Google Scholar]
- 56.Su K.P.E., Johnson M.P., Gracely E.J., Karduna A.R. Scapular rotation in swimmers with and without impingement syndrome: Practice effects. Medicine and Science in Sports and Exercise. 2004;36:1117–1123. doi: 10.1249/01.Mss.0000131955.55786.1a. [DOI] [PubMed] [Google Scholar]
- 57.Tempelhof S., Rupp S., Seil R. Age-related prevalence of rotator cuff tears in asymptomatic shoulders. J Shoulder Elbow Surg. 1999;8:296–299. doi: 10.1016/s1058-2746(99)90148-9. [DOI] [PubMed] [Google Scholar]
- 58.Thomas S.J., Swanik C.B., Higginson J.S., Kaminski T.W., Swanik K.A., Bartolozzi A.R. A bilateral comparison of posterior capsule thickness and its correlation with glenohumeral range of motion and scapular upward rotation in collegiate baseball players. J Shoulder Elbow Surg. 2011;20:708–716. doi: 10.1016/j.jse.2010.08.031. [DOI] [PubMed] [Google Scholar]
- 59.Ueda Y., Tanaka H., Morioka S., Tachibana T., Hayashi T., Ichihashi N. Comparison of scapular upward rotation during arm elevation in the scapular plane in healthy volunteers and patients with rotator cuff tears pre- and post-surgery. Clin Biomech (Bristol, Avon) 2019;63:207–213. doi: 10.1016/j.clinbiomech.2019.03.012. [DOI] [PubMed] [Google Scholar]
- 60.Wassinger C.A., Sole G., Osborne H. Clinical measurement of scapular upward rotation in response to acute subacromial pain. J Orthop Sports Phys Ther. 2013;43:199–203. doi: 10.2519/jospt.2013.4276. [DOI] [PubMed] [Google Scholar]
- 61.Wickham J., Pizzari T., Stansfeld K., Burnside A., Watson L. Quantifying 'normal' shoulder muscle activity during abduction. J Electromyogr Kinesiol. 2010;20:212–222. doi: 10.1016/j.jelekin.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 62.Yamaguchi K., Sher J.S., Andersen W.K., Garretson R., Uribe J.W., Hechtman K. Glenohumeral motion in patients with rotator cuff tears: a comparison of asymptomatic and symptomatic shoulders. J Shoulder Elbow Surg. 2000;9:6–11. doi: 10.1016/s1058-2746(00)90002-8. [DOI] [PubMed] [Google Scholar]
- 63.Yamamoto A., Takagishi K., Osawa T., Yanagawa T., Nakajima D., Shitara H. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg. 2010;19:116–120. doi: 10.1016/j.jse.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 64.Yuri T., Mura N., Yuki I., Fujii H., Kiyoshige Y. Contractile property measurement of the torn supraspinatus muscle using real-time tissue elastography. J Shoulder Elbow Surg. 2018;27:1700–1704. doi: 10.1016/j.jse.2018.02.065. [DOI] [PubMed] [Google Scholar]
- 65.Zingg P.O., Jost B., Sukthankar A., Buhler M., Pfirrmann C.W., Gerber C. Clinical and structural outcomes of nonoperative management of massive rotator cuff tears. J Bone Joint Surg Am. 2007;89:1928–1934. doi: 10.2106/JBJS.F.01073. [DOI] [PubMed] [Google Scholar]