Abstract
Anti-acid drugs, proton pump inhibitor (PPI) and histamine-2 blocker (H2-blocker), are commonly prescribed to treat gastrointestinal disorders. These anti-acid drugs alter gut microbiota in the general population, but their effects are not known in hemodialysis patients. Hence, we investigated the microbiota composition in hemodialysis patients treated with PPIs or H2-blocker. Among 193 hemodialysis patients, we identified 32 H2-blocker users, 23 PPI users, and 138 no anti-acid drug subjects. Fecal samples were obtained to analyze the gut microbiome using 16S RNA amplicon sequencing. Differences in the microbial composition of the H2-blocker users, PPI users, and controls were assessed using linear discriminant analysis effect size and the random forest algorithm. The species richness or evenness (α-diversity) was similar among the three groups, whereas the inter-individual diversity (β-diversity) was different between H2-blocker users, PPI users, and controls. Hemodialysis patients treated with H2-blocker and PPIs had a higher microbial dysbiosis index than the controls, with a significant increase in the genera Provetella 2, Phascolarctobacterium, Christensenellaceae R-7 group, and Eubacterium oxidoreducens group in H2-blocker users, and Streptococcus and Veillonella in PPI users. In addition, compared to the H2-blocker users, there was a significant enrichment of the genera Streptococcus in PPI users, as confirmed by the random forest analysis and the confounder-adjusted regression model. In conclusion, PPIs significantly changed the gut microbiota composition in hemodialysis patients compared to H2-blocker users or controls. Importantly, the Streptococcus genus was significantly increased in PPI treatment. These findings caution against the overuse of PPIs.
Keywords: microbiome, proton pump inhibitor, histamine-2 blocker, hemodialysis
1. Introduction
The gut microbiota is a complex ecosystem in which microbes coexist and interact with the human host. There is a bidirectional causal effect relationship in patients with chronic kidney disease (CKD) and gut microbial changes [1]. Moreover, commonly used medications are associated with distinct gut microbiota signatures [2]. Among the medications, the acid-suppressive agents, such as histamine-2 blockers (H2-blocker) or proton pump inhibitors (PPIs), are generally well tolerated and commonly prescribed in patients with end-stage renal disease (ESRD) [3] as the first-choice treatment for acid-related disorders [4]. However, long-term anti-acid drugs have been found to be associated with several adverse events, such as osteoporosis, fracture, hypomagnesemia, vitamin B12 deficiency, iron deficiency anemia, CKD, dementia, and pneumonia [5,6]. In addition, PPIs have been associated with an increased risk of mortality [7], major adverse cardiovascular events [8], vascular calcification [9], and hip fracture [3] in patients with kidney disease. Furthermore, the long-term reduction of gastric acid secretion by PPIs was suggested to decrease gut microbial richness, alter the composition of both gastric and intestinal microbiota, and increase oral bacteria and potentially pathogenic bacteria [10,11]. Chronic acid suppression by surgical vagotomy or chronic PPI treatment may cause hypochlorhydria and alter the intraluminal environment to promote the growth of the bacterial flora in the small intestine and increase the risk of common community-acquired enteric infections [12].
Although studies have suggested profound changes in PPI users’ gut microbiota in the general population, this has not been investigated in ESRD patients. Nonetheless, conflicting reports of gut microbial diversity change after PPI administration have been observed [10,11,13,14,15]. Therefore, our study aimed to evaluate the influence of two anti-acid drugs (H2-blocker and PPI) on the fecal microbiome in hemodialysis patients.
2. Materials and Methods
2.1. Study Participants
The Ethics Committee approved the study protocols of Kaohsiung Medical University Hospital (KMUHIRB-E(I)-20160095 and KMUHIRB-E(I)-20180118) and Taipei Tzu Chi Hospital (07-X01-002). Hemodialysis (HD) patients from Kaohsiung Medical University Hospital and Taipei Tzu Chi Hospital, Taiwan, were recruited between August 2017 and February 2018. Participants received regular HD three times per week, 3.5–4 h with high-flux dialyzers for each HD section. Patients with active malignancies or prescribed antibiotics within 3 months before enrollment were excluded. In total, 193 HD patients, including 32 H2-blocker users and 23 PPI users, were recruited and collected fecal samples for high throughput 16S ribosomal RNA gene sequencing to compare the microbiome composition between groups, H2-blocker users, PPI users, and controls (without H2-blocker or PPI) (Figure S1). All investigated anti-acid drug users (H2-blocker or PPI) were prescribed for at least one month.
2.2. Comorbidity, Laboratory, and Clinical Variables
Sociodemographic data, age, sex, dialysis vintage, arteriovenous shunt type, medical history, medications, and biochemical data were obtained for all participants from the electronic health care system records. Diabetes was defined as HbA1C 6.5% or higher or the use of oral antidiabetic agents or insulin. Hypertension was defined as 140/90 mmHg or higher or taking blood pressure-lowering drugs. The definition of cardiovascular disease included a history of myocardial infarction or was documented by coronary angiography, chronic heart failure, or a cerebrovascular accident. Blood samples were obtained after overnight fasting from patients through the arteriovenous shunt before their scheduled HD session at a single midweek dialysis session. Biochemical data included hemoglobin, albumin, high sensitivity C-reactive protein, total cholesterol, low-density lipoprotein, triglycerides, ion calcium, and phosphate from routine data within 30 days before stool sample collection. Dietary data were recorded from a modified short-form food frequency questionnaire by a licensed dietitian.
2.3. Fecal Sample Collection and Bacterial 16S rRNA Amplicon Sequencing
All participants provided a stool sample immediately frozen after home collection and delivered to the laboratory (Germark Biotechnology, Taichung, Taiwan) in cooler bags within 24 h via commercial transportation. DNA was extracted using a QIAamp DNA Stool Mini Kit (Qiagen, Germantown, MD, USA).
The amplicon library was constructed by amplifying the variable regions 3 and 4 (V3-V4) of the 16S rRNA gene using barcode-indexed PCR primers (341F and 805R) [16] and the 16S amplicons were sequenced (300 bp paired-end) by an Illumina MiSeq sequencer by Genomics BioScience (Taipei, Taiwan). All samples were simultaneously sequenced in the same laboratory (Germark Biotechnology, Taichung, Taiwan) to minimize batch effects. The detailed methodology of 16S rRNA amplicon sequencing and processing, as described in the supplementary method.
2.4. Statistical and Bioinformatics Analyses
Demographic characteristic differences between H2-blocker users, PPI users, or controls were determined using an ANOVA test or chi-squared test, as appropriate. A rarefaction curve was constructed to prevent methodological artifacts originating from variations in sequencing depth. The α-diversity indices were estimated to evaluate the microbiome richness indices (Chao 1), and the Kruskal–Wallis test calculated evenness (Shannon index, Simpson index, and inverse Simpson index) and the p-value. The β-diversity (i.e., diversity in bacterial composition between samples) was estimated by computing the Bray–Curtis distance, Jensen–Shannon divergence, or Jaccard index and visualized through a principal coordinates analysis (PCoA) to evaluate the difference in bacterial communities between anti-acid drug users and controls [17]. The sample-grouped heterogeneity of β-diversity was examined using an analysis of the similarity (permutational multivariate analysis of variance using distance matrices (PERMANOVA)) with 104 bootstrap replications. The microbial dysbiosis index (MDI) [18] was determined as the log10 of the total abundance in organisms increased in H2-blocker users or PPI users divided by the total abundance of organisms decreased in the controls. Co-correlation analysis was used to determine the relationships within the gut ecosystem. The sparse correlations for compositional data (SparCC) algorithm (19) is described in Supplementary Methods.
The bacterial community difference between H2-blocker users, PPI users, and controls by the linear discriminant analysis (LDA) of effect size (LEfSe) analysis [19], heat tree method [20], hierarchical clustering heat map, and random forest method [21]. The differential abundance analysis was also analyzed using DESeq2 methods [22]. We provide a detailed method described in the Supplementary Materials.
Considering the confounding factors, regression models were used to identify associations between the target microbiota marker and anti-acid drugs used, adjusting for age, sex, and other potential confounders. To reduce the effect of zero-inflation in the microbiome data, the matrix was normalized by dividing each feature by the respective total sample sum and transformed with log10(x + 1), where x is the normalized feature coverage as calculated in the OTUs algorithm.
Co-correlation analysis, heat tree analysis, random forest analysis, and DESeq2 were performed by MicrobiomeAnalyst [23,24]. Other statistical analyses were performed using R statistical software (version 3.5.1) and STATA statistical software (version 14).
2.5. Functional Annotation
Predicted functional genes were aligned with the Kyoto Encyclopedia of Genes and Genomes (KEGG) database and annotated by KEGG orthology (KO) using the R “Tax4Fun” package [25]. The KEGG metabolic modules were retrieved from the KEGG MODULE database, mapped with KOs. The Wilcoxon rank-sum test calculated the differential abundance between the two anti-acid drugs. KEGG modules were deemed present when ≥30% of the enzymes were recovered after the manual removal of overly ‘promiscuous’ enzymes (that is, present in multiple modules) before abundance calculation.
3. Results
3.1. Patient Characteristics
The baseline characteristics are reported in Table 1. The mean age was 65 ± 11.5 years in H2-blocker users, 68.3 ± 12.1 in PPI users, and 64.1 ± 11.0 in controls. The H2-blocker users were more likely to be male than PPI users or controls, with the control group having a higher blood phosphate level and single pool Kt/V than H2-blocker users or PPI users. The indications of PPI and H2-blocker used were also shown (Table 1).
Table 1.
Baseline characteristics of hemodialysis patients using the histamine-2 blocker (H2-blocker), proton pump inhibitor and the controls.
| Baseline Characteristics | Histamine-2 Blocker Users (N = 32) | Proton Pump Inhibitor Users (N = 23) | Control Subjects (N = 138) |
p-Value |
|---|---|---|---|---|
| Age (years) | 65 ± 11.5 | 68.3 ± 12.1 | 64.1 ± 11.0 | 0.309 |
| Male | 17 (73.9%) | 12 (37.5%) | 77 (55.8%) | 0.026 |
| Dialysis vintage (months) | 84.37 ± 52.55 | 98.09 ± 61.51 | 92.02 ± 61.73 | 0.778 |
| Cause of ESRD | ||||
| Hypertension | 1 (4.3%) | 2 (6.3%) | 14 (10.1%) | 0.566 |
| Diabetes mellitus | 11 (47.8%) | 12 (37.5%) | 43 (31.2%) | 0.270 |
| Glomerulonephritis | 6 (26.1%) | 13 (40.6%) | 56 (40.6%) | 0.408 |
| Others * | 5 (21.7%) | 5 (15.6%) | 25 (18.1%) | 0.845 |
| Comorbidities | ||||
| Diabetes mellitus | 13 (56.5%) | 12 (37.5%) | 54 (39.1%) | 0.265 |
| Hypertension | 18 (78.3%) | 27 (84.4%) | 122 (88.4%) | 0.388 |
| Dyslipidemia | 9 (39.1%) | 12 (37.5%) | 34 (24.6%) | 0.169 |
| Medications | ||||
| Anti-hypertensive drugs | 17 (73.9%) | 22 (68.8%) | 79 (57.2%) | 0.198 |
| Diabetes treatment medications | 9 (39.1%) | 9 (28.1%) | 39 (28.3%) | 0.561 |
| Calcium carbonate | 18 (78.3%) | 23 (71.9%) | 120 (87.0%) | 0.092 |
| Clinical laboratory data | ||||
| Hemoglobin (g/dL) | 10.51 ± 1.10 | 10.64 ± 1.09 | 10.7 ± 1.38 | 0.517 |
| Albumin (g/dL) | 3.54 ± 0.71 | 3.52 ± 0.52 | 3.55 ± 0.42 | 0.832 |
| High sensitivity CRP (mg/dL) | 3.4 ± 4.04 | 1.65 ± 4.12 | 2.35 ± 4.50 | 0.574 |
| Total calcium (mg/dL) | 9.27 ± 0.99 | 9.14 ± 1.10 | 9.24 ± 0.85 | 0.901 |
| Phosphate (mg/dL) | 4.63 ± 1.35 | 4.69 ± 1.19 | 5.14 ± 1.20 | 0.020 |
| Single pool Kt/V | 1.55 ± 0.14 | 1.65 ± 0.29 | 1.68 ± 0.28 | 0.046 |
| Dietary intake (serving/day) | ||||
| Meat | 0.86 ± 0.63 | 0.91 ± 0.63 | 0.82 ± 0.51 | 0.695 |
| Vegetable | 1.51 ± 1.20 | 1.8 ± 1.01 | 2.02 ± 1.09 | 0.083 |
| Fruit | 0.8 ± 0.90 | 0.84 ± 0.54 | 0.99 ± 0.72 | 0.399 |
| Bristol stool scale | 3.96 ± 1.77 | 4 ± 1.95 | 3.76 ± 1.78 | 0.745 |
| Anti-acid drugs indication | ||||
| Peptic ulcer disease | 8 (25%) | 11 (47.8%) | ||
| Gastroesophageal reflux disease | 15 (46.9%) | 10 (43.5%) | ||
| Others ** | 9 (28.1%) | 2 (8.7%) |
* Other causes of end-stage renal disease include polycystic kidney disease, tumor, systemic lupus erythematosus, gout, interstitial nephritis. ** Other indications for anti-acid drugs used: gastrointestinal bleed prophylaxis in patients on antiplatelet or anticoagulation therapy or functional dyspepsia. Abbreviation: ESRD, end-stage renal disease; CRP, C-reactive protein
3.2. Differences in the Gut Microbiota Profile in HD Patients
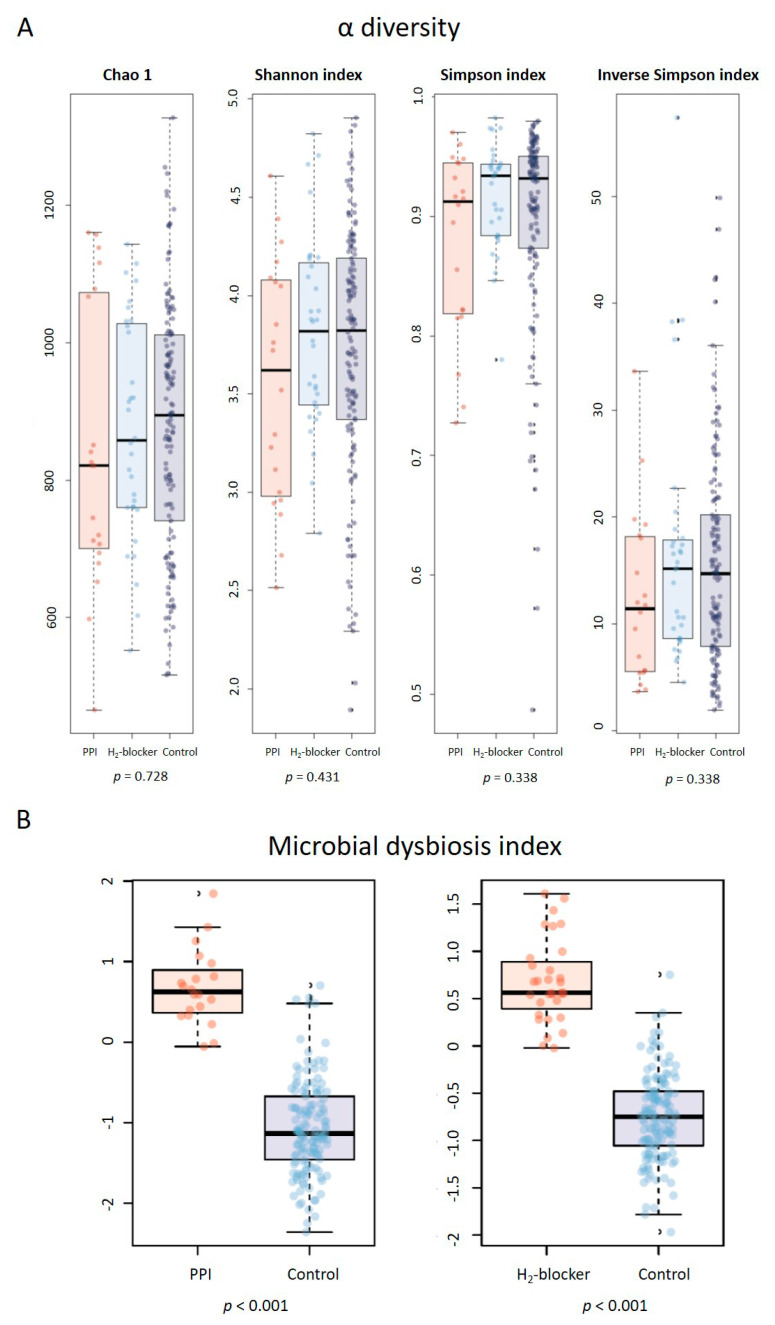
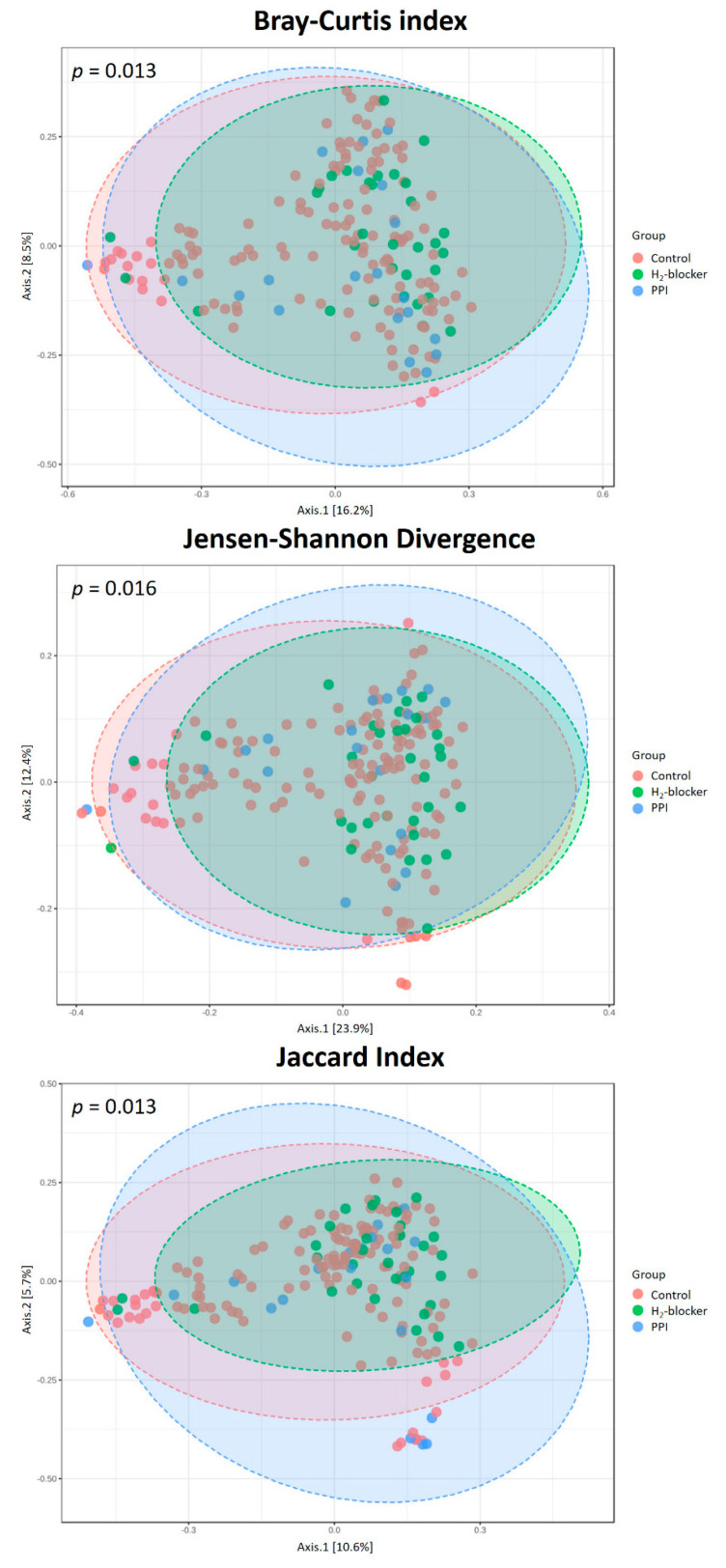
The rarefaction curves, which plot the OTU number as a function of the read number, showed that the three-patient groups’ contours almost overlapped, suggesting no difference in the degree of bacterial species richness (Figure S2). In addition, there was no significant difference between the groups in the relative abundance proportion (Figure S3) and α diversity (Figure 1A). However, HD patients taking H2-blocker or PPI had a higher MDI than controls (Figure 1B), with a significant difference in their microbiota composition (Figure 2). Similar findings were found in a subgroup analysis stratified by diabetes or not. Anti-acid users remained present at a higher MDI than the controls in both diabetic and non-diabetic patients (Figure S4).
Figure 1.
The α-diversity and microbial dysbiosis index in hemodialysis patients with proton pump inhibitor (PPI) users, H2-blocker users, and controls: (A) no difference in richness (Chao 1 index) or evenness (Shannon index, Simpson index, Inverse Simpson index); (B) proton pump inhibitor users or H2-blocker users had a higher microbial dysbiosis index compared to the controls.
Figure 2.
The β-diversity in hemodialysis patients with proton pump inhibitor users, H2-blocker users, and controls (Bray–Curtis index, Jensen–Shannon divergence, and Jaccard index). Differences in β-diversity were tested by permutational multivariate analysis of variance using distance matrices (PERMANOVA).
3.3. Co-Occurrence Pattern Analysis of the Intestinal Ecosystems of HD Patients Treated with H2-Blocker, PPI and Control
Core microbiome analysis was performed at the genus level using MicrobiomeAnalyst and SparCC to calculate the Spearman correlation coefficient with the corresponding p-value between every two taxa (Figure S5A). The core microbiome comprised 13 genera in H2-blocker users, 11 genera in PPI users, and 12 genera in controls, with Bacteroides, which belong to the family Bacteroidaceae, being the most dominant genus (Figure S5B), followed by the core taxa belonging to Parabacteroides and Lachnoclostridium, whereas a unique core taxon, Fusobacterium, linked with hub taxa in the PPI network, was absent from the H2-blocker network.
3.4. Specific Microbial Taxa Are Associated with H2-Blocker and PPI Use
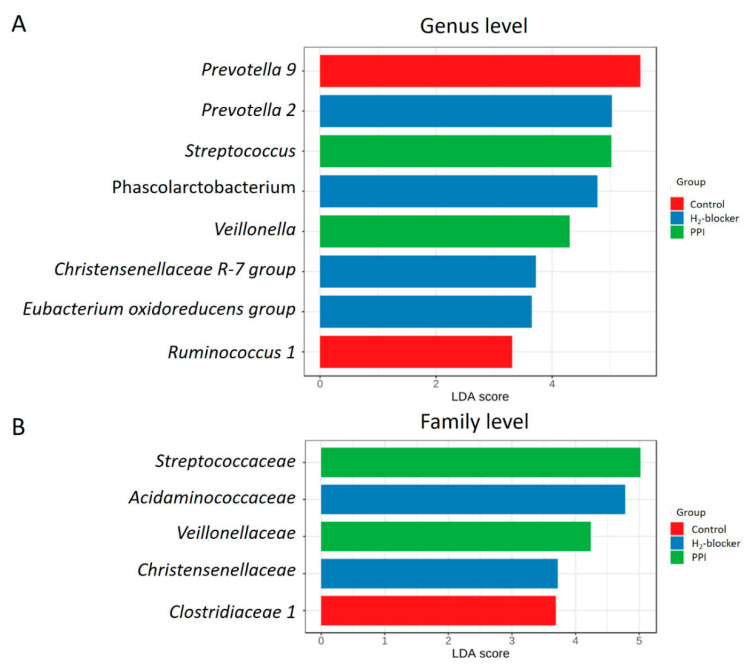
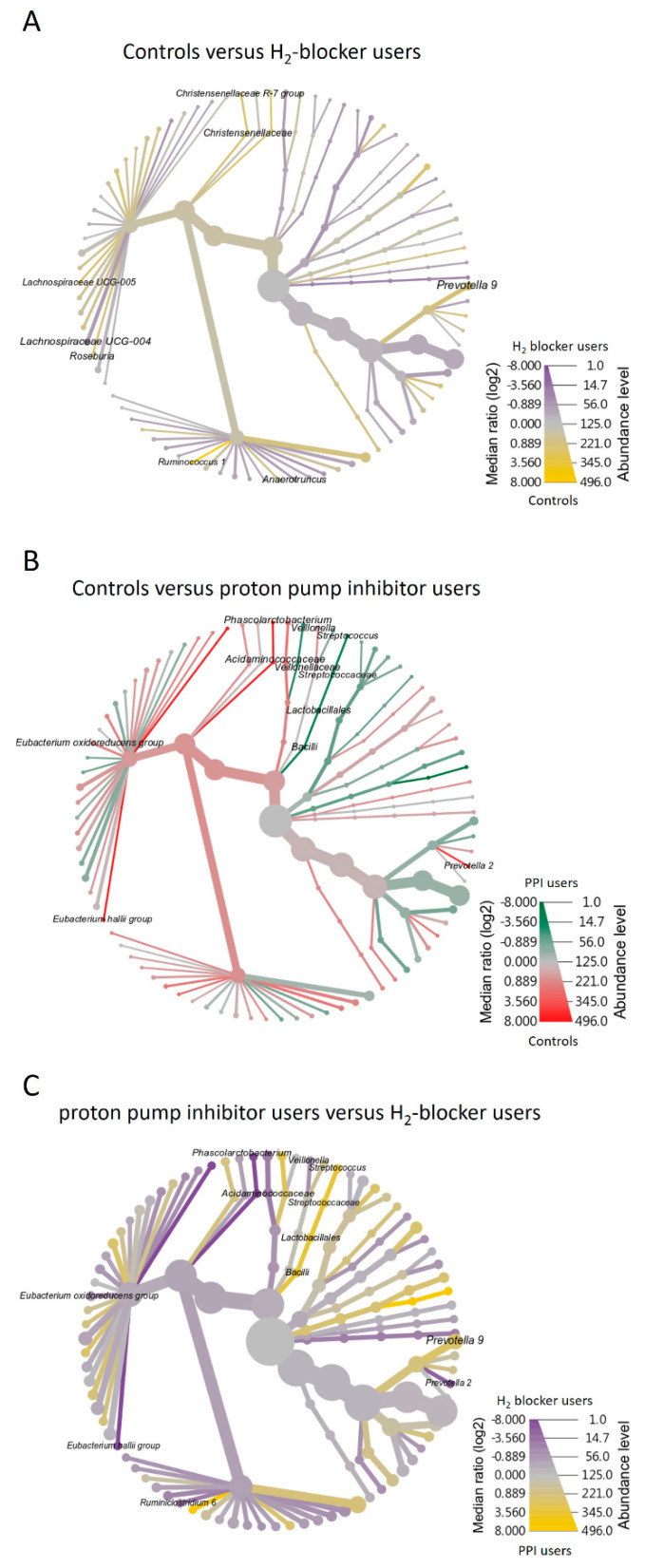
The heat map clustering analysis identified the microbial taxa that varied significantly between H2-blocker users and PPI users (Figure S6). The genera Prevotella 2, Phascolarctobacterium, Christensenellaceae R-7 group, and Eubacterium oxidoreducens group were enriched in H2-blocker users, while Streptococcus and Veillonella were enriched in PPI users and Prevotella 9 and Ruminococcus 1 in the controls (Figure 3A). The family Acidaminococcaceae and Christensenellaceae were enriched in the H2-blocker group, Streptococcaceae and Veillonellaceae in PPI users, and Clostridiaceae 1 in controls (Figure 3B). The heat tree method revealed that compared to the controls or H2-blocker users, the most abundant taxa among PPI users were class Bacilli, order Lactobacillales, family Streptoccaceae, genus Streptococcus, and species Streptococcus salivarius (Figure 4).
Figure 3.
Linear discriminative analysis (LDA) effect size (LEfSe) analysis between H2-blocker users (blue), proton pump inhibitor users (green) and controls (red) at the (A) genus level and (B) family level.
Figure 4.
Heat tree visualization of taxonomic differences. A heat tree illustrates the taxonomic differences between H2-blocker users, proton pump inhibitor users, and controls. The color gradient and the size of the node, edge, and label are based on the log2 ratio of median abundance: (A) controls versus H2-blocker users; (B) controls versus proton pump inhibitor users; (C) H2-blocker users versus proton pump inhibitor users.
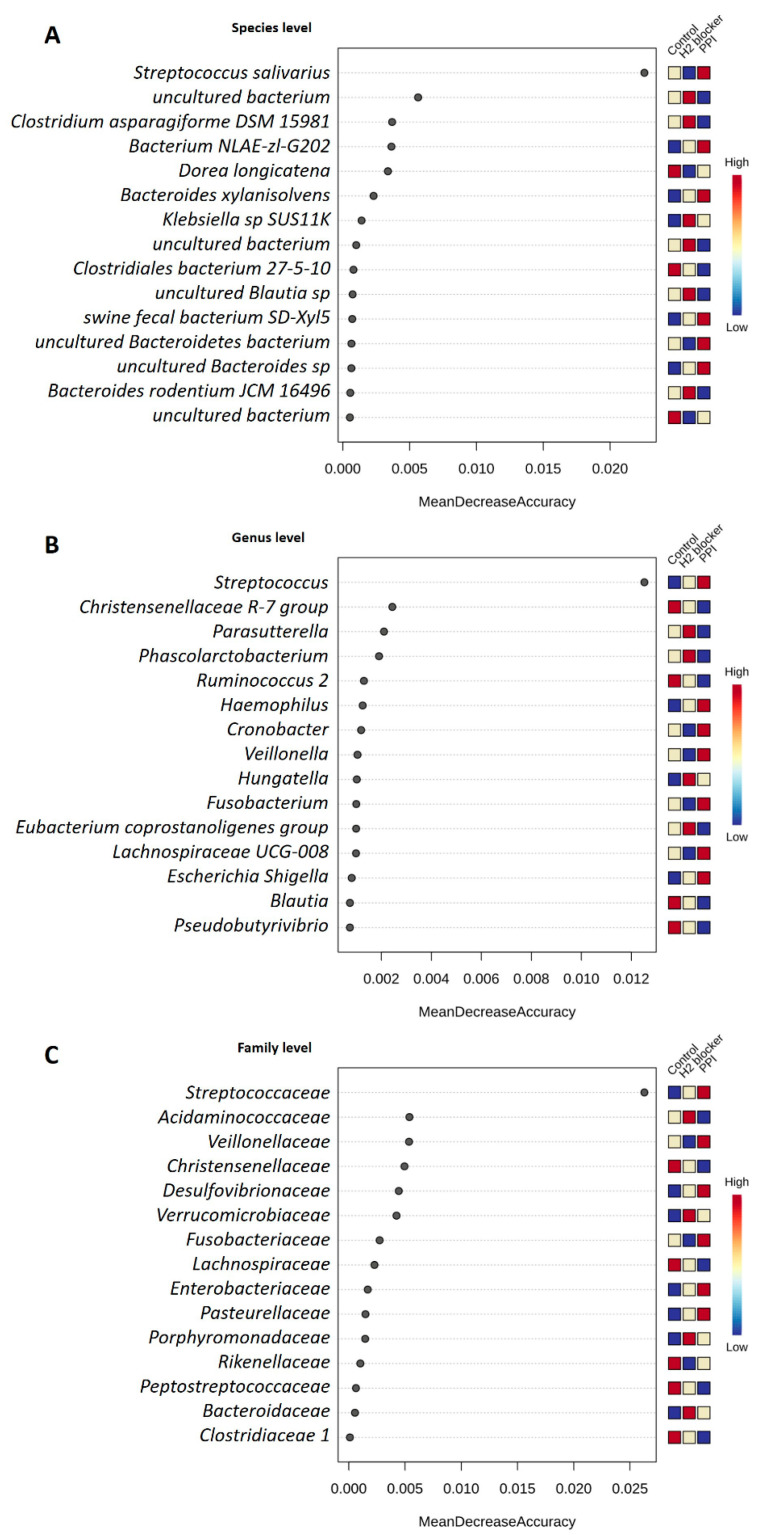
Using all microbiome taxonomy from 193 samples, the machine learning random forest algorithm enabled the prediction of H2-blocker users, PPI users, and controls clusters with 72.6% prediction accuracy (the out-of-bag error is 0.274) in HD patients. The top-ranked bacterial taxa to discriminate between the groups were species S. salivarius, genus Streptococcus, and family Streptococcaceae (Figure 5). Regarding the random forest model predicted specific taxa, there was increased S. salivarius species, genus Streptococcus, and family Streptococcaceae in PPI users compared to H2-blocker users or controls. Other specific top difference taxa included less genus Phascolarctobacterium and family Acidaminococcaceae in PPI users, and more genus Parasutterella in H2-blocker users (Figure S7).
Figure 5.
Determination of bacteria-specificity for discrimination across H2-blocker users, proton pump inhibitor users, and controls in hemodialysis patients. The anti-acid drugs discriminatory taxa were determined by applying random forest analysis using the (A) species-levels abundance; (B) genus-level abundance; and (C) family-level abundance.
Considering confounders may influence the microbiome difference, so a multivariate-adjusted regression model was performed, showing that PPI users had higher 16S RNA levels of Bacilli, Lactobacillales, Streptococcaceae, and Streptococcus than the controls (Table 2), which remained after adjusting for covariates (age, sex, blood phosphate level, and single pool Kt/V level) in the logistic regression models.
Table 2.
Distribution of the Bacilli class and its major subclass between and proton pump inhibitor users and controls.
| Taxonomic Level | Taxon | PPI Users (n = 23) Reads Count, Mean ± SD |
Controls (n = 138) Reads Count, Mean ± SD |
p-Value, Crude | p-Value, Adjusted * |
|---|---|---|---|---|---|
| Class | Bacilli | 1093.1 ± 2121.2 | 34.9 ± 76.9 | <0.001 | <0.001 |
| Order | Lactobacillales | 1092.5 ± 2120.5 | 34.6 ± 76.9 | <0.001 | <0.001 |
| Family | Streptococcaceae | 826.4 ± 2047.8 | 20.5 ± 36.9 | <0.001 | <0.001 |
| Genus | Streptococcus | 826.4 ± 2047.8 | 20.5 ± 36.9 | <0.001 | <0.001 |
SD, standard deviation. * p-value calculated by the logistic regression model adjusted for age, sex, blood phosphate level, and single pool Kt/V level.
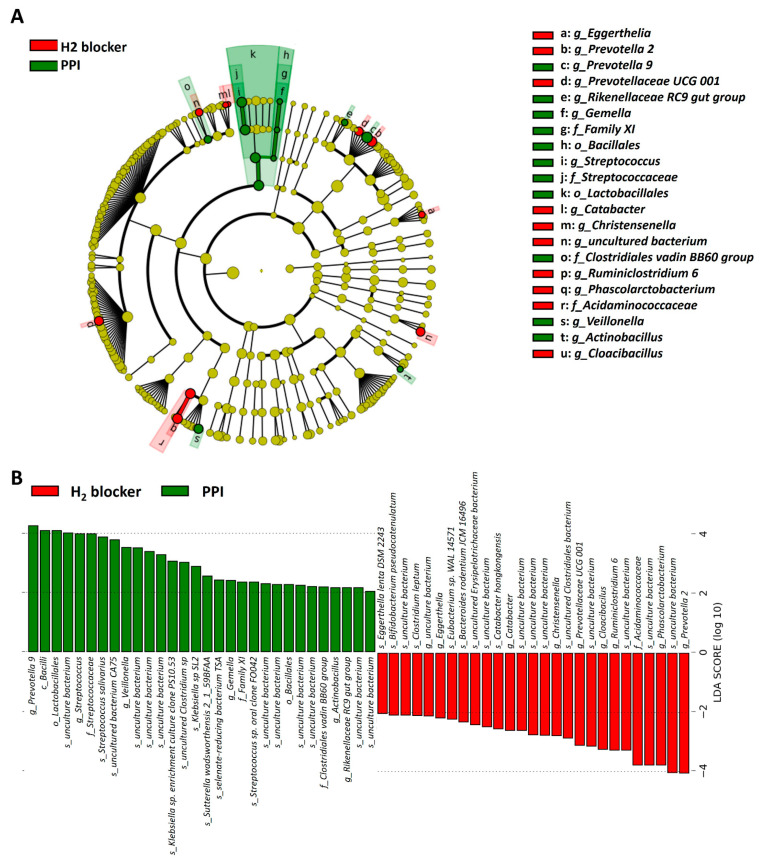
3.5. Comparison of the Microbiome Differences between H2-Blocker Users and PPI Users
Microbiome differences may be related to the anti-acid effect or individual drug effect, so the differences were compared between treatment groups. The cladogram represents these differences at various phylogenic levels starting from the phylum level at the center to subphylum levels toward the periphery (Figure 6A). LDA identified an enriched relative abundance of order Lactobacillales, family Streptococcaceae, genus Streptococcus, and genus Prevotella 9 in PPI users and genus Prevotella 2 in H2-blocker users (Figure 6B). To demonstrate the specific microbial features associated with exposure to the different anti-acid drugs, a single microbiome taxa (genera, families, and orders) comparison was performed (Figures S8–S10). The random forest models to predict the taxonomy classification between two anti-acid drugs demonstrated similar findings (Figure S11). The abundance of the top taxa in the random forest algorithm confirmed that PPI users had higher amounts of species S. salivarius, genera Streptococcus, Prevotella 9, Veillonella, and family Streptococcaceae than H2-blocker users. In contrast, PPI users had lower amounts of species Clostridium leptum, Bacteroides rodentium JCM 16496, genera Ruminiclostridium 6, Phascolarctobacterium, and family Acidaminococcaceae than the H2-blocker users (Figure S12). The negative binomial generalized linear models (DESeq2 method) and a classical univariate method confirmed that PPI users had higher amounts of Streptococcus and Veillonella and lower amounts of Phascolarctobacterium, Prevotella 2, and Ruminiclostridium 6 (Table S1).
Figure 6.
Taxonomic differences were detected between the proton pump inhibitor users and H2-blocker users: (A) cladogram showing differentially abundant taxonomic clades with an LDA score > 4.0 among PPI users and H2-blocker users; (B) linear discriminative analysis (LDA) effect size (LEfSe) analysis between proton pump inhibitor users (green) and H2-blocker users (red).
3.6. Oral Bacterial Translocation in Anti-Acid Users
The 16S RNA amplicon sequencing was assessed against the Human Oral Microbiome Database to confirm the bacterial translocation of oral microbiota in anti-acid drug treatment, showing a different β-diversity (Bray–Curtis index, Jensen–Shannon divergence, and Jaccard index) between the three groups (Figure S13). The heat tree demonstrated an increased abundance of Streptococcus in PPI users than controls or H2-blocker users (Figure S14), specifically, S. vestibularis and S. parasanguinis clade 411 (Figure S15).
3.7. Functional Characterization of the Microbiome of H2-Blocker or PPI Users Compared to Controls
Further analysis of the KEGG modules revealed an alteration in the gut microbiota pathways in response to the H2-blocker or PPI use. In H2-blocker users, most of the mapped genes with KEGG module prediction were involved in carbohydrate metabolism (glyoxylate cycle, methylaspartate cycle), glycan metabolism (N-glycan precursor biosynthesis), and the metabolism of cofactors and vitamins (tetrahydrofolate biosynthesis) (Figure S16). In PPI users, the enriched predicted KEGG modules were involved in amino acid metabolism (serine biosynthesis, glutathione biosynthesis, γ-aminobutyric acid biosynthesis (GABA)), carbohydrate metabolism (ascorbate degradation), energy metabolism (nicotinamide-adenine dinucleotide phosphate (NADPH), cytochrome c oxidase, cytochrome aa3-600 menaquinol oxidase, photosystem 1, nitrogen metabolism), metabolism of cofactors and vitamins (heme biosynthesis), pathogenicity and toxins, drug resistance, and the biosynthesis of other secondary metabolites (pentalenolactone biosynthesis) (Figure S17).
4. Discussion
This study demonstrated that H2-blocker or PPI use is associated with an altered gut microbiota composition, increased MDI, and a distinct β diversity analysis compared to non-users. The microbial communities of HD patients contained higher amounts of Bacteroidetes and lowered Firmicutes levels, similar to CKD rat microbial communities [26]. Co-occurrence analysis revealed no significant difference in keystone taxa Bacteroides between H2-blocker users or PPI users, but there was a difference in the gut microbiota composition. Compared to controls, the genera Provetella 2 was enriched in H2-blocker users and Streptococcus and Veillonella in PPI users. Furthermore, PPI users had abundant class Bacilli taxa, order Lactobacillales, family Streptoccaceae, genus Streptococcus, and species S. salivarius. The random forest algorithm also confirmed family Streptoccaceae, genus Streptococcus, and species S. salivarius as the top taxa to discriminate PPI users. Therefore, in comparison to the controls, PPI use is associated with increases in the order Lactobacillales, particularly the family Streptococcaceae and genus Streptococcus after adjusting for confounders.
The α-diversity analysis revealed no significant differences between H2-blocker users, PPI users, and controls, similar to the results reported by Clooney et al. [13], Freedberg et al. [14], and Takagi et al. [15], but not in line with Jackson et al. [11], Imhann et al. [10], and a systematic review [27]. Our HD patients had been exposed to H2-blocker or PPI for at least one month, similar to the drug exposure time in Freedberg et al. [14], but less than the median of 1.5 years in Jackson et al. [11]. Furthermore, the sample size was larger in Jackson et al. [11] and Imhann et al. [10]; thus, this discrepancy in results may be related to sample size and PPI treatment duration.
The distinct microbial composition in H2-blocker users, PPI users, and controls was demonstrated, showing that, like in previous reports [10,14,15], PPI use was associated with an increased abundance of the genera Streptococcus and Veillonella. A meta-analysis found that PPI induced a shift in the Gram-positive bacteria Streptococcus and Enterococcus [28]. As previously reported, there was also an increased abundance of Streptococcaceae in PPI users at the bacterial family level [11,14]. Other PPI-associated taxa reported from a systematic review [27], such as the order Bacillales (e.g., Staphylococcaceae) and Actinomycetales (e.g., Actinomycetaceae, Micrococcaceae), the family Enterobacteriaceae, Pasteurellaceae, Enterococcaceae, and Lactobacillaceae were not significantly different between the groups in our study; however, the role of these bacterial taxa in HD patients should be further investigated.
Several potential mechanisms may explain the change in the proximal intestinal pH that alters the gut microbiota. First, the increase in gastric pH due to anti-acid therapy may increase bacterial migration from the oral cavity to the intestinal lumen through decreased gastric acid-related bacterial killing [29], as observed by the increased oral microbiome in the fecal microbiota of PPI users, including genus Rothia and Streptococcus spp. [10,11]. In our study, members of the genus Streptococcus, commensals of the human oral cavity, nasopharynx, and esophagus [30], in particular, S. salivarius, were observed in PPI users compared to H2-blocker users or controls. A different β diversity and increased Streptococcus taxa were found using the Human Oral Microbiome Database as a reference, such as S. vestibularis and S. parasanguinis clade 411. Taken together, these findings show that bacteria present in the human oral cavity increased in the intestine, implying that bacterial translocation may have occurred. PPIs reduce gastric acidity; hence the barrier function becomes weakened, potentially accounting for the increased Streptococcus in our study.
Second, the diminished gastric acid secretion and small intestinal dysmotility cause the small intestinal bacterial overgrowth of microaerophilic microorganisms such as Streptococcus, Staphylococcus, Escherichia, and Klebsiella and anaerobic bacteria such as Bacteroides, Lactobacillus, Veillonella, and Clostridium [31], similar to that observed in the PPI group in our study.
Third, PPIs induce hormonal changes, including hypergastrinemia and hyperparathyroidism, which can alter the gastrointestinal bacterial milieu [32]. They can modify the luminal contents, interfering with nutrient absorption, and changing the amount or location of bacterial food substrates [33]. These potential mechanisms may explain the microbiota differences in anti-acid users compared to non-users.
The functional prediction of the microbiome between H2-blocker or PPI users compared to controls demonstrated several essential pathways. PPI was associated with a lower function of GABA biosynthesis compared to controls. As we know, the environmental decreasing pH is fundamental stress for cell growth during GABA production. The proton pump is also included in the acid-resistance system of lactic acid bacteria [34]. GABA biosynthesis is archived through the decarboxylation of glutamate in the cytoplasm, of which this process needs to consume intracellular protons. Therefore, PPI’s effect on GABA biosynthesis may link bacteria’s intracellular pH value [35]. In addition, PPIs could markedly reduce the proportion of vitamin C in its biologically active antioxidant form of ascorbic acid [36] because of a marked and sustained rise in intragastric pH. We also found a difference in ascorbate degradation between PPI users and controls in our study. Furthermore, PPI was associated with a lower function of heme biosynthesis compared to controls. Studies reported that the PPI-mediated reduction of gastric acid causes a reduction in the absorption of dietary iron [37,38].
This study has several limitations. First, cross-sectional studies only evaluated microbiota at a single time point, so it is impossible to capture the complex dynamics of the microbial ecosystems overtime or the microbiome alternation after the initiation of anti-acid drugs. Second, residual confounding cannot be fully excluded and statistical correlations between PPI or H2-blocker treatment and gut microbiota profiles do not implicate a causal relationship. Thus, studies comparing microbiota composition between anti-acid drugs naïve treatment are needed to elucidate the causal inference. Third, the sequencing of the 16S rRNA gene is limited in the analysis at the genera level. Metagenomic shotgun sequencing would permit the strain and more accurate functional analysis. Finally, the study was performed in Asian HD patients whose diet may differ from other populations, so the results should be interpreted cautiously.
Gut microbes have key roles in metabolic, nutritional, and physiological processes in the human body [39]. Changes in this microbial equilibrium, that is, dysbiosis, can promote many intestinal and extra-intestinal diseases [40,41]. In patients with kidney disease, the dysbiotic gut microbiome produced various uremic toxins and inflammation contributing to the complications [42,43]. Thus, therapeutic interventions to restore intestinal dysbiosis was recognized as a potential therapeutic target in patients with kidney disease [42,44].
Although anti-acid drugs (H2-blockers or PPIs) induce changes in the gut microbiota composition with unknown health-related consequences in HD patients, further consideration is the potential for the gastrointestinal tract to become a reservoir for pathogens. A significantly increased risk of community-acquired pneumonia has been observed with PPIs [45], specifically for Streptococcus-derived pneumonia [46]. In addition, PPI also increases sepsis risk, spontaneous bacterial peritonitis, and enteric infections [47,48]. Our study confirmed an association between PPI use and bacterial translocation using the Human Oral Microbiome Database. Given the widespread use of PPIs, healthcare providers should recognize the effects of long-term anti-acid therapy on patients’ health and avoid gut microbiota alternation-related adverse effects.
In conclusion, this study demonstrated that the use of anti-acid drugs changes the composition of gut microbiota in HD patients, with notably increased Streptococcus genus, Streptococcaceae family, and Lactobacillales order in PPI users.
Acknowledgments
We acknowledge Germark Biotechnology Lab for the stool sample analysis of gut microbiota.
Supplementary Materials
The following are available online at https://www.mdpi.com/2076-2607/9/2/286/s1, Supplementary methods, Figure S1: Enrollment of study participants; Figure S2: Rarefaction curves based on gene count in H2-blocker users, proton pump inhibitor users, and controls; Figure S3: The relative percentage abundance of intestinal microbiota at the phylum level between H2-blocker users, proton pump inhibitor users, and controls: (A) phylum, (B) class, and (C) order level; Figure S4: Subgroup analysis of α-diversity and microbial dysbiosis index in hemodialysis patients with proton pump inhibitor users, H2-blocker users, and controls stratified by with and without diabetes mellitus: (A) diabetic patients and (B) non-diabetic patients; Figure S5: Core microbiome analysis in H2-blocker users, proton pump inhibitor users, and controls; (A) SparCC correlation analysis (genus level using 100 SparCC permutations, 0.4 correlation threshold, and 0.05 p-value threshold); (B) relative abundance and sample prevalence of bacterial genus in H2-blocker users, proton pump inhibitor users, and controls; Figure S6: Hierarchical clustering heat map of bacterial genera (A) and families (B) between H2-blocker users, proton pump inhibitor users, and controls generated by MicrobiomeAnalyst using Euclidean distance measure and Ward clustering algorithm; Figure S7: The abundance of the top taxa in random forest algorithm and their enriched difference between H2-blocker users, proton pump inhibitor users, and controls: (A) species level, (B) genus level, and (C) family level; Figure S8: The relative abundance of the specific microbiome genus differentially enriched in the clinical settings after linear discriminant analysis between the H2-blocker and proton pump inhibitor users; Figure S9: The relative abundance of the specific microbiome family differentially enriched in the clinical settings after linear discriminant analysis; Figure S10: The relative abundance of the specific microbiome order differentially enriched in the clinical settings after linear discriminant analysis; Figure S11: Determination of bacteria-specific for discriminatory across H2-blocker and proton pump inhibitor users in hemodialysis patients. The anti-acid drugs discriminatory taxa were determined by applying random forest analysis using the (A) species-levels abundance, (B) genus-level abundance, and (C) family-level; Figure S12: The abundance of the top taxa in the random forest algorithm and their enriched difference between H2-blocker and proton pump inhibitor users: (A) species level, (B) genus level, and (C) family level; Figure S13: The β-diversity in hemodialysis patients with proton pump inhibitor users, H2-blocker users, and controls using Human Oral Microbiome Database as the reference database (Bray–Curtis index, Jensen–Shannon divergence, and Jaccard index). Differences in β-diversity were tested by PERMANOVA; Figure S14: Heat tree visualization of taxonomic differences based on human oral microbiome database. A heat tree illustrates the taxonomic differences between H2-blocker users, proton pump inhibitor users, and controls. The color gradient and the size of the node, edge, and label are based on the log2 ratio of median abundance: (A) proton pump inhibitor users versus controls and (B) proton pump inhibitor users versus H2-blocker users; Figure S15: The abundance of the streptococcus taxa (species level, genus level, and family level) difference between H2-blocker users, proton pump inhibitor users, and controls based on human oral microbiome database; Figure S16: Selected significant functional classification of the predicted metagenome content of the microbiota of H2-blocker users and controls by KO modules. The relative abundances of modules were compared among hemodialysis patients with and without H2-blocker used. Significance was considered for p < 0.05; Figure S17: Selected significant functional classification of the predicted metagenome content of the microbiota of proton pump inhibitor users and controls by KO modules. The relative abundances of modules were compared among hemodialysis patients with and without proton pump inhibitors used. Significance was considered for p < 0.05; Table S1: Summary table of significant genus difference between the H2-blocker and proton pump inhibitor users in negative binomial generalized linear models (DESeq2 method) and classical univariate method.
Author Contributions
Conceptualization, Y.-T.L., P.-H.W., Y.-W.C. and M.-C.K.; data curation, Y.-T.L., P.-Y.L. and P.-H.W.; funding acquisition, Y.-T.L. and P.-H.W.; investigation, Y.-T.L., P.-Y.L., P.-H.W. and C.-Y.W.; methodology, Y.-T.L., P.-Y.L., P.-H.W., Y.-W.C., M.-C.K. and C.-Y.W.; software, Y.-T.L., P.-Y.L. and P.-H.W.; writing—original draft, Y.-T.L., P.-Y.L. and P.-H.W.; writing—review and editing, T.-Y.L., S.-C.H., Y.-S.C., W.-C.H., Y.-W.C., M.-C.K. and C.-Y.W. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by grants from the Ministry of Science and Technology, Taiwan (MOST 106-2314-B-037-054, MOST 107-2314-B-037-104, and MOST 107-2314-B-037-098-MY3), Kaohsiung Medical University Hospital, Taiwan (KMUH106-6R17, KMUH106-6T03, KMUH107-7R16, KMUH107-7R78, KMUH108-8M11, KMUH108-8R70, KMUH109-9R16, and KMUH109-9R81), Kaohsiung Medical University, Taiwan (KMU-Q108024 and KMU-Q108027), and NSYSU-KMU JOINT RESEARCH PROJECT (NSYSUKMU 105-I005 and NSYSUKMU 106-I005).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of Kaohsiung Medical University Hospital (KMUHIRB-E(I)-20160095 and KMUHIRB-E(I)-20180118) and Taipei Tzu Chi Hospital (07-X01-002).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data (sequenced reads) presented in this study are publicly available on National Center for Biotechnology Information’s (NCBI) Sequence Read Archive (SRA) under BioProject accession number PRJNA648014.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Vaziri N.D., Wong J., Pahl M., Piceno Y.M., Yuan J., DeSantis T.Z., Ni Z., Nguyen T.H., Andersen G.L. Chronic kidney disease alters intestinal microbial flora. Kidney Int. 2013;83:308–315. doi: 10.1038/ki.2012.345. [DOI] [PubMed] [Google Scholar]
- 2.Jackson M.A., Verdi S., Maxan M.E., Shin C.M., Zierer J., Bowyer R.C.E., Martin T., Williams F.M.K., Menni C., Bell J.T., et al. Gut microbiota associations with common diseases and prescription medications in a population-based cohort. Nat. Commun. 2018;9:2655. doi: 10.1038/s41467-018-05184-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vangala C., Niu J., Lenihan C.R., Mitch W.E., Navaneethan S.D., Winkelmayer W.C. Proton Pump Inhibitors, Histamine-2 Receptor Antagonists, and Hip Fracture Risk among Patients on Hemodialysis. Clin. J. Am. Soc. Nephrol. 2018;13:1534–1541. doi: 10.2215/CJN.02190218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nehra A.K., Alexander J.A., Loftus C.G., Nehra V. Proton Pump Inhibitors: Review of Emerging Concerns. Mayo Clin. Proc. 2018;93:240–246. doi: 10.1016/j.mayocp.2017.10.022. [DOI] [PubMed] [Google Scholar]
- 5.Freedberg D.E., Kim L.S., Yang Y.X. The Risks and Benefits of Long-term Use of Proton Pump Inhibitors: Expert Review and Best Practice Advice From the American Gastroenterological Association. Gastroenterology. 2017;152:706–715. doi: 10.1053/j.gastro.2017.01.031. [DOI] [PubMed] [Google Scholar]
- 6.Vaezi M.F., Yang Y.X., Howden C.W. Complications of Proton Pump Inhibitor Therapy. Gastroenterology. 2017;153:35–48. doi: 10.1053/j.gastro.2017.04.047. [DOI] [PubMed] [Google Scholar]
- 7.De Francisco A.L.M., Varas J., Ramos R., Merello J.I., Canaud B., Stuard S., Pascual J., Aljama P., Optimizing Results in Dialysis (ORD) Group Proton Pump Inhibitor Usage and the Risk of Mortality in Hemodialysis Patients. Kidney Int. Rep. 2018;3:374–384. doi: 10.1016/j.ekir.2017.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tsai I.J., Lai T.S., Shiao C.C., Huang T.M., Wang C.H., Chen L.W., Lin Y.H., Chen L., Wu V.C., Chu T.S., et al. Proton-Pump Inhibitors Augment the Risk of Major Adverse Cardiovascular Events and End-Stage Renal Disease in Patients with Acute Kidney Injury After Temporary Dialysis. Clin. Pharmacol. Ther. 2020:10.1002/cpt.1762. doi: 10.1002/cpt.1762. [DOI] [PubMed] [Google Scholar]
- 9.Okamoto T., Hatakeyama S., Hosogoe S., Tanaka Y., Imanishi K., Takashima T., Saitoh F., Suzuki T., Ohyama C. Proton pump inhibitor as an independent factor of progression of abdominal aortic calcification in patients on maintenance hemodialysis. PLoS ONE. 2018;13:e0199160. doi: 10.1371/journal.pone.0199160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Imhann F., Bonder M.J., Vich Vila A., Fu J., Mujagic Z., Vork L., Tigchelaar E.F., Jankipersadsing S.A., Cenit M.C., Harmsen H.J., et al. Proton pump inhibitors affect the gut microbiome. Gut. 2016;65:740–748. doi: 10.1136/gutjnl-2015-310376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jackson M.A., Goodrich J.K., Maxan M.E., Freedberg D.E., Abrams J.A., Poole A.C., Sutter J.L., Welter D., Ley R.E., Bell J.T., et al. Proton pump inhibitors alter the composition of the gut microbiota. Gut. 2016;65:749–756. doi: 10.1136/gutjnl-2015-310861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bavishi C., Dupont H.L. Systematic review: The use of proton pump inhibitors and increased susceptibility to enteric infection. Aliment. Pharmacol. Ther. 2011;34:1269–1281. doi: 10.1111/j.1365-2036.2011.04874.x. [DOI] [PubMed] [Google Scholar]
- 13.Clooney A.G., Bernstein C.N., Leslie W.D., Vagianos K., Sargent M., Laserna-Mendieta E.J., Claesson M.J., Targownik L.E. A comparison of the gut microbiome between long-term users and non-users of proton pump inhibitors. Aliment. Pharmacol. Ther. 2016;43:974–984. doi: 10.1111/apt.13568. [DOI] [PubMed] [Google Scholar]
- 14.Freedberg D.E., Toussaint N.C., Chen S.P., Ratner A.J., Whittier S., Wang T.C., Wang H.H., Abrams J.A. Proton Pump Inhibitors Alter Specific Taxa in the Human Gastrointestinal Microbiome: A Crossover Trial. Gastroenterology. 2015;149:883–885.e889. doi: 10.1053/j.gastro.2015.06.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Takagi T., Naito Y., Inoue R., Kashiwagi S., Uchiyama K., Mizushima K., Tsuchiya S., Okayama T., Dohi O., Yoshida N., et al. The influence of long-term use of proton pump inhibitors on the gut microbiota: An age-sex-matched case-control study. J. Clin. Biochem. Nutr. 2018;62:100–105. doi: 10.3164/jcbn.17-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Herlemann D.P., Labrenz M., Jurgens K., Bertilsson S., Waniek J.J., Andersson A.F. Transitions in bacterial communities along the 2000 km salinity gradient of the Baltic Sea. ISME J. 2011;5:1571–1579. doi: 10.1038/ismej.2011.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lozupone C.A., Hamady M., Kelley S.T., Knight R. Quantitative and qualitative beta diversity measures lead to different insights into factors that structure microbial communities. Appl. Environ. Microbiol. 2007;73:1576–1585. doi: 10.1128/AEM.01996-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gevers D., Kugathasan S., Denson L.A., Vazquez-Baeza Y., Van Treuren W., Ren B., Schwager E., Knights D., Song S.J., Yassour M., et al. The treatment-naive microbiome in new-onset Crohn’s disease. Cell Host Microbe. 2014;15:382–392. doi: 10.1016/j.chom.2014.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Segata N., Izard J., Waldron L., Gevers D., Miropolsky L., Garrett W.S., Huttenhower C. Metagenomic biomarker discovery and explanation. Genome Biol. 2011;12:R60. doi: 10.1186/gb-2011-12-6-r60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Foster Z.S., Sharpton T.J., Grunwald N.J. Metacoder: An R package for visualization and manipulation of community taxonomic diversity data. PLoS Comput. Biol. 2017;13:e1005404. doi: 10.1371/journal.pcbi.1005404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Svetnik V., Liaw A., Tong C., Culberson J.C., Sheridan R.P., Feuston B.P. Random forest: A classification and regression tool for compound classification and QSAR modeling. J. Chem. Inf. Comput. Sci. 2003;43:1947–1958. doi: 10.1021/ci034160g. [DOI] [PubMed] [Google Scholar]
- 22.Love M.I., Huber W., Anders S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 2014;15:550. doi: 10.1186/s13059-014-0550-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dhariwal A., Chong J., Habib S., King I.L., Agellon L.B., Xia J. MicrobiomeAnalyst: A web-based tool for comprehensive statistical, visual and meta-analysis of microbiome data. Nucleic Acids Res. 2017;45:W180–W188. doi: 10.1093/nar/gkx295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chong J., Liu P., Zhou G., Xia J. Using MicrobiomeAnalyst for comprehensive statistical, functional, and meta-analysis of microbiome data. Nat. Protoc. 2020:10.1038/s41596-019-0264-1. doi: 10.1038/s41596-019-0264-1. [DOI] [PubMed] [Google Scholar]
- 25.Asshauer K.P., Wemheuer B., Daniel R., Meinicke P. Tax4Fun: Predicting functional profiles from metagenomic 16S rRNA data. Bioinformatics. 2015;31:2882–2884. doi: 10.1093/bioinformatics/btv287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lau W.L., Vaziri N.D., Nunes A.C.F., Comeau A.M., Langille M.G.I., England W., Khazaeli M., Suematsu Y., Phan J., Whiteson K. The Phosphate Binder Ferric Citrate Alters the Gut Microbiome in Rats with Chronic Kidney Disease. J. Pharmacol. Exp. Ther. 2018;367:452–460. doi: 10.1124/jpet.118.251389. [DOI] [PubMed] [Google Scholar]
- 27.Macke L., Schulz C., Koletzko L., Malfertheiner P. Systematic review: The effects of proton pump inhibitors on the microbiome of the digestive tract-evidence from next-generation sequencing studies. Aliment. Pharmacol. Ther. 2020 doi: 10.1111/apt.15604. [DOI] [PubMed] [Google Scholar]
- 28.Naito Y., Kashiwagi K., Takagi T., Andoh A., Inoue R. Intestinal Dysbiosis Secondary to Proton-Pump Inhibitor Use. Digestion. 2018;97:195–204. doi: 10.1159/000481813. [DOI] [PubMed] [Google Scholar]
- 29.Dong T., Pisegna J. Passing the “Acid Test”: Do Proton Pump Inhibitors Affect the Composition of the Microbiome? Dig. Dis. Sci. 2018;63:2817–2819. doi: 10.1007/s10620-018-5273-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Andersson A.F., Lindberg M., Jakobsson H., Backhed F., Nyren P., Engstrand L. Comparative analysis of human gut microbiota by barcoded pyrosequencing. PLoS ONE. 2008;3:e2836. doi: 10.1371/journal.pone.0002836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fujimori S. What are the effects of proton pump inhibitors on the small intestine? World J. Gastroenterol. 2015;21:6817–6819. doi: 10.3748/wjg.v21.i22.6817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yang Y.X., Metz D.C. Safety of proton pump inhibitor exposure. Gastroenterology. 2010;139:1115–1127. doi: 10.1053/j.gastro.2010.08.023. [DOI] [PubMed] [Google Scholar]
- 33.Markovits N., Loebstein R., Halkin H., Bialik M., Landes-Westerman J., Lomnicky J., Kurnik D. The association of proton pump inhibitors and hypomagnesemia in the community setting. J. Clin. Pharmacol. 2014;54:889–895. doi: 10.1002/jcph.316. [DOI] [PubMed] [Google Scholar]
- 34.Wang C., Cui Y., Qu X. Mechanisms and improvement of acid resistance in lactic acid bacteria. Arch. Microbiol. 2018;200:195–201. doi: 10.1007/s00203-017-1446-2. [DOI] [PubMed] [Google Scholar]
- 35.Cui Y., Miao K., Niyaphorn S., Qu X. Production of Gamma-Aminobutyric Acid from Lactic Acid Bacteria: A Systematic Review. Int. J. Mol. Sci. 2020;21:995. doi: 10.3390/ijms21030995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Van der Loo B., Bachschmid M., Spitzer V., Brey L., Ullrich V., Luscher T.F. Decreased plasma and tissue levels of vitamin C in a rat model of aging: Implications for antioxidative defense. Biochem. Biophys. Res. Commun. 2003;303:483–487. doi: 10.1016/S0006-291X(03)00360-7. [DOI] [PubMed] [Google Scholar]
- 37.Hutchinson C., Geissler C.A., Powell J.J., Bomford A. Proton pump inhibitors suppress absorption of dietary non-haem iron in hereditary haemochromatosis. Gut. 2007;56:1291–1295. doi: 10.1136/gut.2006.108613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Handa P., Kowdley K.V. A Proton Pump Inhibitor a Day Keeps the Iron Away. Clin. Gastroenterol. Hepatol. 2016;14:153–155. doi: 10.1016/j.cgh.2015.09.007. [DOI] [PubMed] [Google Scholar]
- 39.Lynch S.V., Pedersen O. The Human Intestinal Microbiome in Health and Disease. N. Engl. J. Med. 2016;375:2369–2379. doi: 10.1056/NEJMra1600266. [DOI] [PubMed] [Google Scholar]
- 40.Belizario J.E., Faintuch J., Garay-Malpartida M. Gut Microbiome Dysbiosis and Immunometabolism: New Frontiers for Treatment of Metabolic Diseases. Mediators Inflamm. 2018;2018:2037838. doi: 10.1155/2018/2037838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.DeGruttola A.K., Low D., Mizoguchi A., Mizoguchi E. Current Understanding of Dysbiosis in Disease in Human and Animal Models. Inflamm. Bowel Dis. 2016;22:1137–1150. doi: 10.1097/MIB.0000000000000750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nallu A., Sharma S., Ramezani A., Muralidharan J., Raj D. Gut microbiome in chronic kidney disease: Challenges and opportunities. Transl. Res. 2017;179:24–37. doi: 10.1016/j.trsl.2016.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stadlbauer V., Horvath A., Ribitsch W., Schmerbock B., Schilcher G., Lemesch S., Stiegler P., Rosenkranz A.R., Fickert P., Leber B. Structural and functional differences in gut microbiome composition in patients undergoing haemodialysis or peritoneal dialysis. Sci. Rep. 2017;7:15601. doi: 10.1038/s41598-017-15650-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cigarran Guldris S., Gonzalez Parra E., Cases Amenos A. Gut microbiota in chronic kidney disease. Nefrologia. 2017;37:9–19. doi: 10.1016/j.nefro.2016.05.008. [DOI] [PubMed] [Google Scholar]
- 45.Eom C.S., Jeon C.Y., Lim J.W., Cho E.G., Park S.M., Lee K.S. Use of acid-suppressive drugs and risk of pneumonia: A systematic review and meta-analysis. CMAJ. 2011;183:310–319. doi: 10.1503/cmaj.092129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.De Jager C.P., Wever P.C., Gemen E.F., van Oijen M.G., van Gageldonk-Lafeber A.B., Siersema P.D., Kusters G.C., Laheij R.J. Proton pump inhibitor therapy predisposes to community-acquired Streptococcus pneumoniae pneumonia. Aliment. Pharmacol. Ther. 2012;36:941–949. doi: 10.1111/apt.12069. [DOI] [PubMed] [Google Scholar]
- 47.Xu H.B., Wang H.D., Li C.H., Ye S., Dong M.S., Xia Q.J., Zhang A.Q., Pan K., Ge X.L., Dong J.H. Proton pump inhibitor use and risk of spontaneous bacterial peritonitis in cirrhotic patients: A systematic review and meta-analysis. Genet. Mol. Res. 2015;14:7490–7501. doi: 10.4238/2015.July.3.25. [DOI] [PubMed] [Google Scholar]
- 48.Zhou S.J., Wang S.Q., Ma Y.Y., Tang L.Y., Shi Y.F., Liang B., Chen Y., Yu K. Association of proton pump inhibitors with the occurrence of gut-derived bacteraemia in patients with haematological malignancy after chemotherapy. Hematology. 2016;21:332–337. doi: 10.1080/10245332.2016.1142711. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data (sequenced reads) presented in this study are publicly available on National Center for Biotechnology Information’s (NCBI) Sequence Read Archive (SRA) under BioProject accession number PRJNA648014.