Abstract
Background
The COVID-19 pandemic has resulted in significant changes to healthcare systems which impact the delivery of surgical training. This study aimed to investigate the qualitative impact of COVID-19 on surgical training in the United Kingdom (UK) & Republic of Ireland (ROI)
Methods
This national, collaborative, cross-sectional study involving 13 surgical trainee associations distributed a pan-surgical specialty questionnaire on the impact of COVID-19 on surgical training over 4 weeks in May 2020. Various aspects of training were assessed.
Results
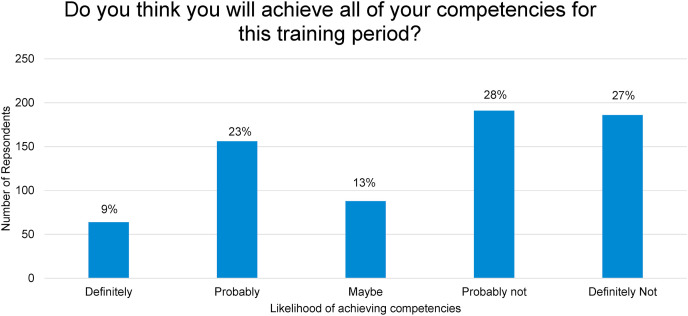
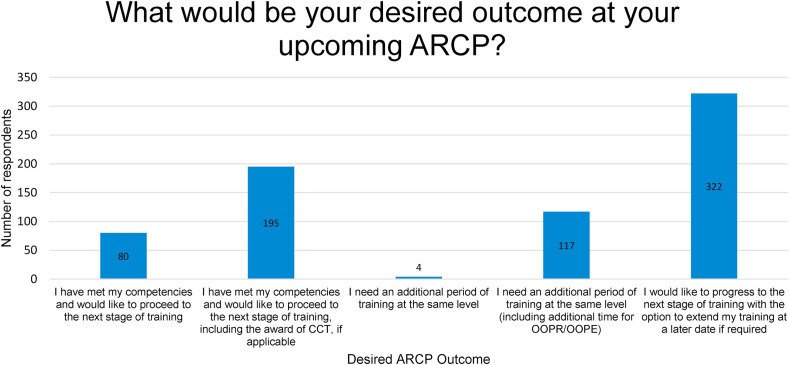
810 completed responses were analysed (males = 401, females = 390) from all deaneries and training grades. The perceived negative overall impact of the pandemic on surgical training experience was significant. (Weighted average = 8.66). 41% of respondents (n = 301) were redeployed with 74% redeployed for >4 weeks. Complete loss of training was reported in elective operating (69.5%), outpatient activity (67.3%) and endoscopy (69.5%). A reduction of >50% was reported in emergency operating (48%) and completion of work-based assessments (WBAs) (46%). 3.3% (n = 17) of respondents reported plans to leave medicine altogether. Cancellations in study leave and regional teaching programmes without rescheduling were reported in 72% and 60% of the cohort respectively. Elective operative exposure and WBAs completion were the primary reported factors affecting potential trainee progression. Only 9% of trainees reported that they would definitely meet all required competencies.
Conclusion
COVID-19 has had a negative impact on surgical training across all grades and specialties, with implications for trainee progression, recruitment and retention of the surgical workforce. Further investigation of the long-term impact at a national level is required.
Keywords: Surgical training, Impact, COVID-19, Pandemic
1. Introduction
The coronavirus (COVID-19) pandemic has had an unprecedented effect on the delivery of healthcare in the United Kingdom (UK) and Republic of Ireland (ROI). Reconfiguration of health services started nationally in early March 2020 in preparation for a potential surge in COVID-19 cases beyond critical care capacity as observed in other countries [1].
Surgical services have been particularly affected, with government and ministerial requests for mandatory cancellation of non-urgent appointments, investigations and procedures [[2], [3], [4], [5], [6]]. In response, the Royal Colleges and surgical associations have advised on adapting local services to continue surgical investigations or interventions amidst the global crisis [7].
Early avoidance of laparoscopic practices, adoption of conservative approaches to certain pathologies, changes to multidisciplinary management (MDM), dual-consultant operating and prioritisation of procedures across specialties have created a new landscape for surgeons and patients [8]. The introduction of COVID-19 clean sites, utilisation of virtual consultations and private-sector hubs have aimed to provide continued care in surgery [9].
The ongoing impact of the COVID-19 pandemic on surgical trainees has been difficult to assess [10,11]. A joint letter from the Association of Surgeons in Training (ASiT) and surgical trainee associations at the start of the pandemic vowed to closely monitor this impact on surgical trainees [12]. Prior to the COVID-19 pandemic the General Medical Council (GMC) identified the negative impact of system pressures that continue to affect training environments and trainee health and wellbeing [13,14]. With the initial postponement of the 2020 national GMC survey due to anticipated pressures on frontline doctors, it was essential to capture large-scale information on the experiences of surgical trainees during the first wave of COVID-19.
The COVID-19 impact on Surgical Training and Recovery Planning (COVID-STAR) collaborative study group was formed in recognition of this. The aim of this study was to qualitatively assess the impact of COVID-19 on surgical trainees in the UK and ROI.
2. Methods
2.1. Survey and study period
A prospective cross-sectional observational study was performed. A novel survey with item numbers ranging from (1–128) depending on grade, specialty and level of training was developed and included binomial, variable-scale, likert-scale and free-text response options. The survey was designed on the online platform SurveyMonkey (SurveyMonkey Inc, San Mateo, California, USA) in accordance with previously published guidelines on conducting survey-based research [[15], [16], [17]]. The survey was peer-reviewed and piloted by the ASiT Executive Committee, collaborating surgical trainee association presidents and ASiT specialty representatives prior to dissemination. No individually identifiable information was collected. Consecutive responses were collected over a 4-week period (11th May-8th June 2020). This timeline fell in conjunction with the point at which the UK lockdown restrictions were reduced (11th May) [18] and incorporated the release of guidance by the Royal College of Surgeons of England (RCSEng) on the recovery of surgical services (14th May) [19].
2.2. Inclusion and exclusion Criteria
Completion was voluntary and open to surgical trainees of all grades and specialties, foundation doctors and medical students. Specialty and Associate Specialist (SAS) doctors were included, and data was captured on less-than-full-time (LTFT), pregnant and out-of-programme (OOP) trainees and those in recognised academic training pathways (Academic Foundation Programme, Academic Clinical Fellowship and Academic Clinical Lectureship). Consultant grades or trainees in a non-surgical speciality were excluded from the analysis.
2.3. collaborative Network
A collaborative authorship model was adopted [20] (Appendix 1). The COVID-STAR Collaborative comprised of ASiT, the Association of Otolaryngologists in Training (AOT), Oral & Maxillofacial Surgery Fellows in Training (OMFS FiT), the trainee section of the Society for Cardiothoracic Surgery (SCTS), the British Neurosurgical Trainees' Association (BNTA), the British Association of Urological Surgeons section of Trainees (BSoT), Trainees in Paediatric Surgery (TriPS), Plastic Surgery Trainees Association (PLASTA) and the Dukes’ Club, Herrick Society, Mammary Fold, Rouleaux Club and Roux Group. All associations represent trainees in different surgical specialties at a national level with the aim of promoting excellence in training. The survey was disseminated through the relevant ASiT and trainee association social media streams as well as through local and national electronic mailing lists. The study was also placed on the RCSEng COVID-19 research portfolio.
2.4. Outcome measures
The primary outcome measure was the perceived overall impact of the COVID-19 pandemic on surgical training experience. Secondary outcomes, as a direct result of COVID-19, were incidence of redeployment to other specialties, perceived loss of training, rate of attrition and the impact on extracurricular surgical activities, health and wellbeing, teaching activity and confidence to progress to the next training stage.
2.5. Statistical analysis
Only fully completed questionnaires were included in the analysis. Significance testing was conducted using the Fisher's exact test for categorical data, Mann–Whitney U test for non-parametric continuous data comparing two groups (male vs female trainees), and one-way analysis of variance (ANOVA) test for non-parametric continuous data comparing more than two groups (specialties). A p-value of <0.05 was considered statistically significant.
Where subgroup analysis resulted in low numbers with the potential for individuals to be identified, these data were excluded from the final synthesis of results. This was communicated to potential participants in advance. For these reasons, non-responding participants could not be identified for follow-up. Participants consented to the use of the analysis, distribution and publication of anonymised grouped results. This study did not require ethical approval due to the anonymous, observational nature of the study and no incentives were offered for participation. This study was conducted in line with the Strengthening the reporting of cohort studies in surgery (STROCSS) criteria [21].
3. Results
3.1. Response rate and subgroups
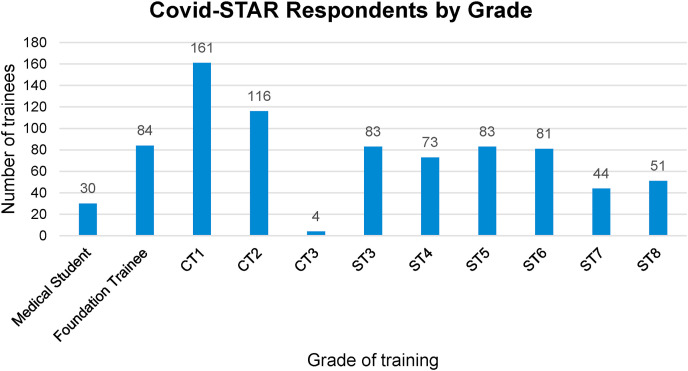
The total number of survey responses was 1042, with 810 responses included in the final analysis. Exclusions are highlighted in Appendix 2. There were 401 (49.5%) male and 390 (48%) female respondents, with 19 (2.5%) choosing not to specify gender. All training grades (Fig. 1 ) and deaneries were represented. Intended certification specialties by training grade are outlined in Table 1 . There were 51 (6%) less than full time trainees (LTFT) and 21 (3%) pregnant trainees.
Fig. 1.
COVID-STAR respondents by grade.
Table 1.
Respondents intended CCT speciality by training grade.
|
Intended CCT Speciality |
Current Grade |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Medical Student | Foundation Trainee | CT1 | CT2 | CT3 | ST3 | ST4 | ST5 | ST6 | ST7 | ST8 | Grand Total | |
| Breast | 4 | 5 | 4 | 5 | 6 | 6 | 5 | 7 | 42 | |||
| Cardiothoracic Surgery | 3 | 4 | 1 | 3 | 2 | 1 | 14 | |||||
| Colorectal | 17 | 10 | 9 | 10 | 11 | 6 | 8 | 10 | 81 | |||
| Emergency General Surgery | 5 | 4 | 2 | 11 | ||||||||
| Endocrine | 2 | 1 | 1 | 4 | ||||||||
| Hepatobiliary (HPB) | 1 | 2 | 1 | 2 | 2 | 1 | 2 | 11 | ||||
| Neurosurgery | 9 | 7 | 3 | 2 | 4 | 4 | 2 | 2 | 33 | |||
| Oesophagogastric (UGI including Bariatrics) | 5 | 4 | 4 | 9 | 6 | 6 | 4 | 4 | 42 | |||
| Oral and Maxillofacial Surgery | 5 | 1 | 2 | 4 | 1 | 4 | 2 | 1 | 20 | |||
| Otolaryngology | 19 | 15 | 1 | 11 | 12 | 11 | 9 | 8 | 4 | 90 | ||
| Paediatric Surgery | 5 | 3 | 1 | 2 | 5 | 1 | 1 | 18 | ||||
| Plastic Surgery | 22 | 12 | 2 | 10 | 8 | 6 | 13 | 5 | 6 | 84 | ||
| Transplant | 3 | 2 | 1 | 2 | 1 | 1 | 10 | |||||
| Trauma & Orthopaedics | 27 | 26 | 13 | 5 | 7 | 5 | 2 | 1 | 86 | |||
| Undecided | 15 | 13 | 4 | 4 | 2 | 1 | 1 | 39 | ||||
| Urology | 12 | 5 | 7 | 4 | 7 | 13 | 4 | 52 | ||||
| Vascular Surgery | 7 | 5 | 8 | 6 | 12 | 8 | 1 | 11 | 58 | |||
| Speciality Not Provided | 30 | 84 | 114 | |||||||||
| Total | 30 | 84 | 161 | 116 | 4 | 83 | 73 | 83 | 81 | 44 | 51 | 810 |
3.2. Impact on services and training
The reported overall impact of COVID-19 on surgical training experience addressed as Likert scale (1 = no impact, 10 = very significant impact) was very significant (Weighted average = 8.66) There was no difference between training grades or specialities. Changes in the delivery of surgical services due to COVID-19 are outlined in Table 2 . Elective non-cancer surgery and elective endoscopy volumes were the most affected, with complete suspension reported by 87% and 84% of respondents respectively. The effect of the pandemic on various aspects of surgical training is highlighted in Table 3 . Course cancellations were reported in 80% of cases, whilst a complete loss of training activity in elective operations (69.5%), outpatient clinics (67.3%), endoscopy (69.5%), specialty-specific accreditations (72%) and simulation training (68%) were reported. Training in emergency operations and completion of Work-based Assessments (WBAs) were reported as significantly reduced (>50% reduction) in 48% and 46% of responses respectively.
Table 2.
Percentage of respondents reporting changes to the delivery of surgical services (n) = number.
| Red Flag/2-week wait Outpatient referrals | Routine Outpatient clinic referrals | Elective Non-cancer surgery | Elective cancer Surgery | Emergency Surgery | Multidisciplinary meetings | Elective Endoscopy | Emergency Endoscopy | Interventional procedures | |
|---|---|---|---|---|---|---|---|---|---|
| Continued Face to Face review/meeting | 19.2 (107) | 0.8 (5) | 0.7 (4) | 9.1 (47) | 31.4 (201) | 12.1 (72) | 3.9 (12) | 24.7 (74) | 19.9 (81) |
| Cases performed at COVID site | 2.9 (16) | 0.6 (4) | 2.9 (18) | 27.3 (141) | 59.9 (384) | 2.9 (17) | 5.2 (16) | 57.0 (171) | 54.8 (223) |
| Review/Meeting switched to another format (e.g. virtual/telephone) | 64.7 (360) | 56.5 (357) | 5.2 (32) | 11.0 (57) | 1.9 (12) | 71.0 (421) | 2.0 (6) | 3.7 (11) | 4.4 (18) |
| Cases performed at COVID freesite | 5.0 (28) | 0.8 (5) | 4.4 (27) | 36.4 (188) | 5.0 (32) | 1.0 (6) | 4.9 (15) | 4.3 (13) | 6.1 (25) |
| Service Suspended | 8.1(45) | 41.3 (261) | 86.8 (534) | 16.2 (84) | 1.9 (12) | 13.0 (77) | 84.0 (258) | 10.3 (31) | 14.7 (60) |
Table 3.
Percentage of respondents reporting degrees of impact of varying aspects of surgical training. (n) = number.
| Complete loss of training activity (Cancellation of services) | Significant reduction in training activity (>50%) | Reduction in my training activity (<50%) | No change to my training activity | Increase in my training activity (<50%) | Significant increase in my training activity (>50%) | |
|---|---|---|---|---|---|---|
| Indicative operative numbers - Elective | 69.5 (474) | 24.0 (164) | 4.3 (29) | 1.9 (13) | 0.3 (2) | 0.0 (0) |
| Indicative operative numbers - Emergency | 28.0 (191) | 47.8 (326) | 17.2 (117) | 5.0 (34) | 1.8 (12) | 0.3 (2) |
| Outpatient clinical activity | 67.3 (457) | 21.8 (148) | 4.3 (29) | 4.3 (29) | 1.5 (10) | 0.9 (6) |
| Ward round activity | 15.9 (109) | 25.7 (176) | 19.3 (132) | 26.3 (180) | 6.0 (41) | 6.7 (46) |
| Multidisciplinary meeting (MDM) attendance | 52.8 (347) | 19.0 (125) | 9.1 (60) | 16.7 (110) | 1.5 (10) | 0.8 (5) |
| Contribution to MDM meeting | 57.2 (369) | 14.3 (92) | 7.1 (46) | 19.5 (126) | 1.2 (8) | 0.6 (4) |
| Endoscopy training | 69.5 (246) | 13.6 (48) | 5.1 (18) | 11.6 (41) | 0.0 (0) | 0.3 (1) |
| Research Outputs | 17.2 (115) | 17.7 (118) | 12.0 (80) | 30.1 (201) | 17.4 (116) | 5.5 (37) |
| Completion of Workplace-based Assessments (WBAs) | 18.7 (127) | 45.5 (309) | 20.5 (139) | 12.4 (84) | 2.2 (15) | 0.7 (5) |
| Audit and Quality Improvement | 17.5 (120) | 25.7 (176) | 14.2 (97) | 26.9 (184) | 12.0 (82) | 3.7 (25) |
| Medical Education and teaching | 34.8 (239) | 25.2 (173) | 11.6 (80) | 12.5 (86) | 10.6 (73) | 5.2 (36) |
| Course Attendance (including mandatory courses) | 80.6 (551) | 9.2 (63) | 4.8 (33) | 3.2 (22) | 1.5 (10) | 0.7 (5) |
| Management and Leadership Activity | 34.6 (230) | 18.7 (124) | 9.5 (63) | 23.6 (157) | 10.4 (69) | 3.2 (21) |
| Specialty specific accreditations e.g. (JAG endoscopy | 72.4 (247) | 6.2 (21) | 3.2 (11) | 17.6 (60) | 0.6 (2) | 0.0 (0) |
| Simulation training | 67.6 (395) | 8.2 (48) | 4.3 (25) | 17.1 (100) | 1.9 (11) | 0.9 (5) |
3.3. Redeployment
41% (n = 301) trainees were redeployed of which only 18.4% were on a voluntary basis. Junior trainees reported a greater rate of redeployment. (Foundation (FY) 53% vs Core training (CT) 44% vs Specialist Training (ST) 21%). 73% were redeployed for more than 4 weeks. 82% felt supported during their period of redeployment. However, 63% reported their overall training experience during redeployment as very bad, bad, or neutral.
3.4. Trainee progression
73% of all respondents above foundation grade anticipated that lack of opportunities for indicative elective numbers may impact their annual review of competency progression (ARCP), while 58% reported the same for emergency operative numbers, 63% for WBAs and 47% for outpatient clinics. 19% of trainees intended to progress to the next stage of training at ARCP having gained all training opportunities. As a result of their experiences during COVID-19, 84% of all respondents reported they plan to stay on their current training path. 3.3% (n = 17) of the cohort reported plans to leave medicine altogether (CT = 8, 3.6%; ST = 11, 3.2%) and an additional 7.7% (n = 53) preferred not to say.
3.5. Health and wellbeing
99 (15%) trainees reported the necessity to shield as per government guidance, 60% (n = 59) were male. 25% (n = 173) of trainees required testing for COVID-19 as per government guidance. 40% of participants (n = 326) reported they had to self-isolate. 81% of trainees reported some negative impact of COVID-19 on their mental health with 10% reporting being affected to a great or very great extent. 48% (n = 474) of trainees reported an inability to take annual leave as a direct result of COVID – 19 (Leave cancelled (27%) or due to rota changes (21%))
3.6. Support for trainees
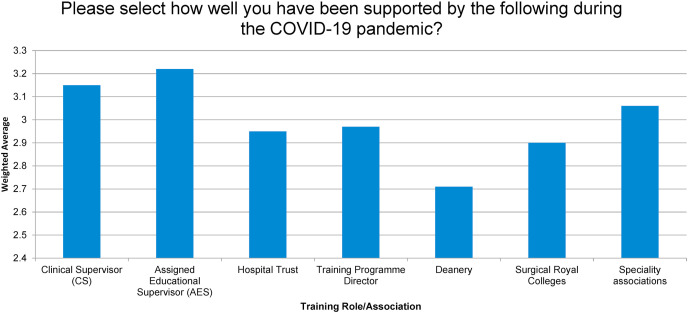
32% felt that they were not provided with enough information and support on the new changes to the ARCP process and 13% were unaware of the new changes. Participants reported variable levels of support from educational supervisors, Training Programme Directors (TPD), deaneries, Royal Colleges, and specialty associations (Fig. 2). Deaneries were rated lowest whilst Clinical and Educational supervisors were the most supportive training role.
Fig. 2.
Perception of support shown by various training roles/Associations.
3.7. Educational opportunities
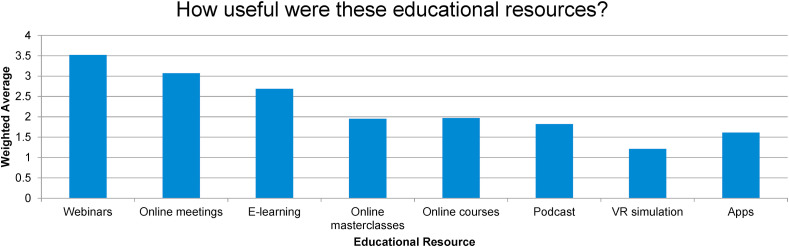
Cancelled study leave was reported by 72% (n = 539) of respondents with 58%, 60%, and 59% of all hospital, regional, and national scheduled teaching programmes reported being cancelled without rescheduling. The most commonly used learning resources were the speciality association and Surgical Royal College webinars followed by online group discussions and E-learning modules. The feedback regarding the usefulness of different educational resources used by trainees was positive (Fig. 3 ).
Fig. 3.
Usefulness of virtual learning modalities.
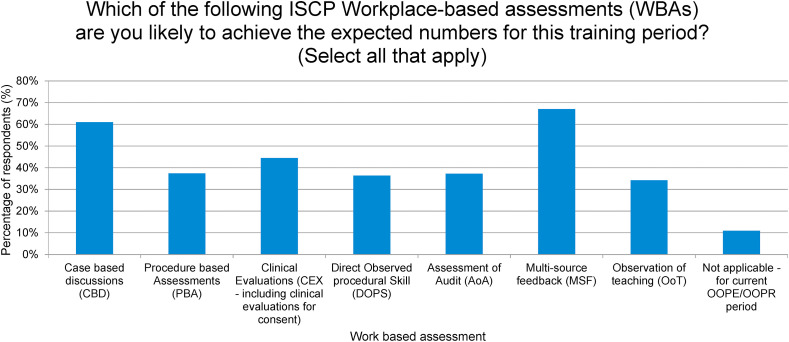
3.8. Training competencies
Fig. 4 outlines the perception of trainees on the WBAs they are likely to achieve during the COVID training period. The most achievable WBAs described by trainees for their current training period was their Multi-source feedback and Case based discussions. Fig. 5 shows the perception of trainees’ likelihood of achieving all competencies for the training period. Only 9% (n = 64) were confident that they would definitely achieve all required competencies. 55% (n = 377) recognised that they would probably (28%) or definitely (27%) not achieve all competencies needed for their current training period. This feeling was more common amongst speciality registrars (61%) and non-trainees (72%). There was no difference observed between males and females. However, 65% (n = 472, 65%) of trainees reported confidence to progress to the next stage of training (60% females and 71% males). More junior trainees reported greater confidence to progress (85% FY vs 65% of CT vs 60% of ST). Fig. 6 defines the desired ARCP outcomes. 45% of the trainees reported that their desired next ARCP outcome would be to progress to the next stage with an option to extend their training at a later stage if needed. 38% reported that they had met their competencies and would like to proceed to the next stage of training. Only 17% stated that they felt they needed an additional period of training at the same level.
Fig. 4.
Percentage (%) of respondents reporting likelihood of achieving specific work-based assessments (WBAs).
Fig. 5.
Likert response of the trainee perception of the Likelihood of achieving all competencies in this training period.
Fig. 6.
Trainee reported desired ARCP outcome.
3.9. Recovery planning
Finally, participants were asked to record their agreement on 4 statements related to potential recovery planning. The statement included trainee's involvement in the planning stages of re-introduction of services, training during dual consultant operating lists, trainee involvement in “cancer hubs”, and training in the private sector. Table 4 highlights levels of agreement.
Table 4.
Weighted averages of respondent agreement with recovery planning statements.
| Recovery planning Statement | Strongly disagree (%) | Disagree (%) | Neutral (%) | Agree (%) | Strongly agree (%) | Total (n) | Weighted Average |
|---|---|---|---|---|---|---|---|
| Trainees should be involved in the planning stages of re-introduction of services | 4 | 1 | 10 | 45 | 40 | 641 | 4.15 |
| In instances of dual consultant operating consideration should be given to best utilise the trainee skillset | 3 | 0 | 8 | 41 | 49 | 639 | 4.31 |
| Trainees should be involved in training in areas where “cancer hubs” have been set up | 2 | 0 | 11 | 39 | 47 | 639 | 4.27 |
| Trainees should be supported to work in the private sector in a training capacity | 4 | 5 | 15 | 32 | 44 | 640 | 4.05 |
4. Discussion
The COVID-19 pandemic has had a detrimental effect on various aspects of healthcare on a global scale. Sadly, patient death as a direct result of COVID-19 and the impact on their families and close friends, remain the first and greatest victim of the pandemic. This has had an impact on the health and wellbeing of the international healthcare workforce [14]. The predicted number of elective surgical cancellations are unprecedented [22] and have necessitated changes to service delivery and staffing to continue effective care provision [23].
Deficiencies in surgical training have existed prior to COVID-19. Mandatory surveys of training experiences have highlighted areas of concern including rota gaps, lack of protected personal study time and achievement of theatre quality indicators. The COVID-19 pandemic has compounded these problems further. The 2020 GMC national training survey [24] demonstrated that 80% of doctors in training reported that the disruption caused by coronavirus reduced their access to the learning they needed to progress. In addition, around three-fifths of trainees, and four-fifths of trainers, saw their work change significantly during the Spring peak. Many clinicians were redeployed into other specialties to meet service demands and were working at the edge of their comfort zone. The findings from the COVID-STAR study are consistent with these findings.
Governmental and public health guidance have placed strain on the delivery of surgical services. This has resulted in major service reconfiguration which is clearly reflected in the trainee response. 41% of surgical trainees surveyed were redeployed demonstrating the demand on NHS staff and services during the first wave of the pandemic. It highlights the wider contribution of surgical trainees to the clinical care of both COVID and non-COVID patients during the pandemic to date. The lack of educational value from these experiences should be recognised by educational bodies and considered in future decision making in the event of future waves.
The complete suspension of elective non-cancer surgery and endoscopy in many cases, alongside the changes to the delivery of MDM and outpatient consultations have resulted in a unanimously negative trainee experience, with significant reduction in training opportunities reported during this period.
The impact on trainee mental health and wellbeing is not to be underestimated. Data presented in this paper demonstrate the negative impact of the pandemic and altered work patterns on trainee mental health with 81% reporting some degree of impact. In addition, blanket cancellation of annual leave, lack of support from individuals and institutions further compounded the situation. With 15% of respondents shielding during the first wave and 40% undergoing a period of self-isolation, the cumulative lost time at work may have reduced the ability of these trainees to meet ARCP competencies whilst placing increasing demands on the remaining workforce. Pregnant trainees were also required to work from home if in the third trimester and this represented a significant time out of the clinical environment. All these changes in the working dynamic will have compounded to compromise training opportunities.
The mandatory cancellation of major extra-curricular activity was demonstrated through the high volume of study leave and course cancellations. Cancellation of the majority of teaching programmes without rescheduling, lack of perceived ability to undertake work-based assessments, cancellation of exams and inability to travel on overseas fellowships have not only limited educational experiences but have clearly impacted on trainee progression. The voluntary engagement with educational material from external bodies is reflective of the continual appetite for education and motivation to progress. The uptake of virtual education platforms was a positive finding from this study.
Despite only 9% of trainees reporting the likelihood of achieving all of their competencies for the training period, the majority (65%) reported confidence to progress. This seems highly incongruous given the loss of opportunity and may purely reflect the eagerness of trainees to advance regardless of the compromising circumstances. The four statutory educational bodies have responded to the dynamic landscape across all training specialties [25]. Adaptation to local and national recruitment processes and modes of assessment of competence and progression (ARCP) have had to be altered at critical training progression points to maintain equilibrium in the workforce [26]. The stance relating to ARCP outcomes and progression may reflect the trainee desire for flexibility in training or the appropriate use of the COVID related ARCP outcome 10.
The positive trainee response to recovery planning options is most likely reflective of a desire for trainee involvement in decision making about future training plans and to access training opportunities of any kind outside the standard channels.
High quality training is essential to equip the next generation of consultant surgeons with the skills to deliver safe and effective care to patients. Thus, the recovery phase of the COVID-19 pandemic must be considered as an opportunity, not just to restore normal surgical services and training, but to introduce and establish a new, improved normal. The full impact and consequences of the pandemic will not be clear for some time however this study has demonstrated an overall negative impact on surgical education and training in all specialties in the UK & ROI.
4.1. Limitations
We acknowledge both the low response rate and the exclusion rate as study limitations.
The overall length of the survey may have contributed to the incomplete responses.
Studies such as the one described will inherently suffer from a low response rate [[27], [28], [29]]. Given the nature of the pandemic, the optimal timing of dissemination and duration of data capture was carefully considered. It was not possible to mandate completion of the survey, however the collaborative approach and outlined study design was chosen to minimise bias and in the absence of no other proposed national capture of training experience during the study period makes this study the largest contemporary series of its kind.
5. Conclusion
This study highlights the many aspects of surgical training in the UK & ROI affected during the first wave of the COVID-19 pandemic. Mandatory redeployment as well as the change in surgical landscape and delivery of service have drastically reduced training opportunities and the perceived abilities of trainees to meet the training requirements to progress.
The status of the pandemic is dynamic and the true duration and impact on training is unlikely to be known for some time. Serial prospective studies of both the qualitative and quantitative impact of COVID-19 on surgical training are necessary to guide key educational stakeholders on the training deficit and to mandate action to ensure the current training standards are met and our future generation of surgeons are equipped to provide excellent patient care.
Ethical approval
Not applicable.
Sources of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contribution
CRediT authorship contribution statement.
Steering Committee: Joshua Michael Clements: Conceptualization, Methodology, Software, Validation, Investigation, Project administration and Visualization. Supervision. Josh Burke: Conceptualization, Methodology, Software, Validation, Investigation, Project administration and Visualization. Supervision. Deirdre Nally: Conceptualization, Methodology, Software, Validation, Investigation, Project administration and Visualization. Supervision. Mohamed Rabie: Conceptualization, Methodology, Software, Validation, Investigation, Project administration and Visualization. Supervision. Elizabeth Kane: Conceptualization, Methodology, Software, Validation, Investigation, Project administration and Visualization. Supervision. Emma Barlow: Conceptualization, Methodology, Software, Validation, Investigation, Project administration and Visualization. Supervision. Walid Mohamed: Conceptualization, Methodology, Software, Validation, Investigation, Project administration and Visualization. Supervision. Martin King: Conceptualization, Methodology, Software, Validation, Investigation, Project administration and Visualization. Supervision. Liusaidh McClymont: Conceptualization, Methodology, Software, Validation, Investigation, Project administration and Visualization. Supervision.
Writing Group: Joshua Michael Clements: Writing – original draft, Writing - review & editing. Josh Burke: Writing – original draft, Writing - review & editing. Deirdre Nally: Writing – original draft, Writing - review & editing. Mohamed Rabie: Writing – original draft, Writing - review & editing. Elizabeth Kane: Writing – original draft, Writing - review & editing. Emma Barlow: Writing – original draft, Writing - review & editing. Walid Mohamed: Writing – original draft, Writing - review & editing. Martin King: Writing – original draft, Writing - review & editing.
Data-Analysis Group: Joshua Michael Clements: Formal analysis. Josh Burke: Formal analysis. Deirdre Nally: Formal analysis. Mohamed Rabie: Formal analysis. Elizabeth Kane: Formal analysis. Emma Barlow: Formal analysis. Walid Mohamed: Formal analysis. Martin King: Formal analysis. Liusaidh McClymont: Formal analysis.
Surgical Trainee Association Presidents - Collaborators & Dissemination Group: Manish George: Conceptualization, Methodology and Writing - review & editing. Sotonye Tolofari: Conceptualization, Methodology and Writing - review & editing. Siobhan McKay: Conceptualization, Methodology and Writing - review & editing. Ashan Jayasekera: Conceptualization, Methodology and Writing - review & editing. Duncan Steele: Conceptualization, Methodology and Writing - review & editing. Abdul Badran: Conceptualization, Methodology and Writing - review & editing. Dominic Summers: Conceptualization, Methodology and Writing - review & editing. Deena Harji: Conceptualization, Methodology and Writing - review & editing. Gina Weston-Petrides: Conceptualization, Methodology and Writing - review & editing. Omar Nasher: Conceptualization, Methodology and Writing - review & editing. Benjamin Baker: Conceptualization, Methodology and Writing - review & editing. Shaneel Patel: Conceptualization, Methodology and Writing - review & editing. Raghuram Boyapati: Conceptualization, Methodology and Writing - review & editing.
Surgical Trainee Association ASiT Representative - Collaborators & Dissemination Group: Adam Peckham-Cooper: Conceptualization, Methodology and Writing - review & editing. Anthony Bashyam: Conceptualization, Methodology and Writing - review & editing. Matthew Stovell: Conceptualization, Methodology and Writing - review & editing. Catherine Zhang: Conceptualization, Methodology and Writing - review & editing. Rachel Thomas: Conceptualization, Methodology and Writing - review & editing. Panchali Sarmah: Conceptualization, Methodology and Writing - review & editing. Alexander Wilkins: Conceptualization, Methodology and Writing - review & editing. Radhika Dua: Conceptualization, Methodology and Writing - review & editing. Vimal Gokani: Conceptualization, Methodology and Writing - review & editing. George Dovell: Conceptualization, Methodology and Writing - review & editing. Sophie Rintoul-Hoad: Conceptualization, Methodology and Writing - review & editing.
Research registration Unique Identifying number (UIN)
Name of the registry: Research Registry.
Unique Identifying number or registration ID: researchregistry6308.
Hyperlink to the registration (must be publicly accessible): researchregistry6308.
Guarantor
Joshua Michael Clements & Josh Burke.
Association of Surgeons in Training.
35-43 Lincoln's Inn Fields, London, WC2A 3 PE
Office: +44 (0) 207 869 6681.
Email: info@asit.org.uk.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Data statement
There are no linked research data sets for this submission. The individual responses are not available in order to preserve responder anonymity and confidentiality.
Declaration of competing interest
The authors are current surgical trainees. The authors have no other relevant financial or personal conflicts of interest to declare in relation to this paper.
Acknowledgements
We would like to thank the Royal College of Surgeons of England for their help with the survey dissemination.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijsu.2021.105903.
Contributor Information
COVID-STAR Collaborative Study Group:
Joshua Michael Clements, Josh Burke, Deirdre Nally, Mohamed Rabie, Elizabeth Kane, Emma Barlow, Walid Mohamed, Martin King, Liusaidh McClymont, Manish George, Sotonye Tolofari, Siobhan McKay, Ashan Jayasekera, Duncan Steele, Abdul Badran, Dominic Summers, Deena Harji, Gina Weston-Petrides, Omar Nasher, Benjamin Baker, Shaneel Patel, Raghuram Boyapati, Adam Peckham-Cooper, Anthony Bashyam, Matthew Stovell, Catherine Zhang, Rachel Thomas, Panchali Sarmah, Alexander Wilkins, Radhika Dua, Vimal Gokani, George Dovell, and Sophie Rintoul-Hoad
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Carenzo L., Costantini E., Greco M., Barra F.L., Rendiniello V., Mainetti M., Bui R., Zanella A., Grasselli G., Lagioia M., Protti A., Cecconi Hospital surge capacity in a tertiary emergency referral centre during the COVID-19 outbreak in Italy. Anaesthesia. 2020 Jul;75(7):928–934. doi: 10.1111/anae.15072. [DOI] [PubMed] [Google Scholar]
- 2.Department of Health Urgent written statement to the assembly by health minister robin swann – thursday 19 March 2020 at 14.00 – health and social care planning for the period mid-march to mid-april 2020 during the delay phase for coronavirus. https://www.health-ni.gov.uk/sites/default/files/publications/health/Coronavirus-19-03-2020.pdf Available from: Accessed 10th June 2020.
- 3.NHS England and NHS Improvement Next steps on NHS response to COVID-19: letter from sir simon stevens and amanda pritchard. https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/20200317-NHS-COVID-letter-FINAL.pdf Available from: Accessed 10th June 2020.
- 4.Scottish Parliament Coronavirus (COVID-19): speech by cabinet secretary for health and sport 17 March 2020. https://www.gov.scot/publications/coronavirus-covid-19-update-scottish-parliament/ Available from: Accessed 10th June 2020.
- 5.Welsh Government Written statement: coronavirus (COVID-19) https://gov.wales/written-statement-coronavirus-covid-19-2 Available from: Accessed 10th June 2020.
- 6.Hettiaratchy S., Deakin D. Guidance for surgeons working during the COVID-19 pandemic [internet]. Surgical royal Colleges of the United Kingdom and Ireland. https://www.rcseng.ac.uk/coronavirus/joint-guidance-for-surgeons-v1/ 20th March 2020. Available from:
- 7.Surgical Royal Colleges of the UK and Ireland Guidance for surgeons working during the COVID-19 pandemic. https://www.rcseng.ac.uk/coronavirus/joint-guidance-for-surgeons-v1/ Available from: Accessed 27th September 2020.
- 8.The Federation of Specialty Surgical Associations Clinical guide to surgical prioritisation during the coronavirus pandemic. https://fssa.org.uk/_userfiles/pages/files/covid19/prioritisation_master_240820.pdf Available from: Accessed 27th September 2020.
- 9.NHS England and NHS Improvement and Health Education England Agreed principles and guidance around training in the independent sector for organisations working under the COVID-19 national contract. https://www.england.nhs.uk/coronavirus/publication/agreed-principles-and-guidance-around-training-in-the-independent-sector-for-organisations-working-under-the-covid-19-national-contract/ Available from: Accessed 7th November 2020.
- 10.Burke J. The impact of COVID-19 on surgical training. RCS Bull. 2020 Sept. 102;(S1):3. [Google Scholar]
- 11.Lund J. Training during and after COVID-19. RCS Bull. 2020 Sept. 102;S1:10–13. [Google Scholar]
- 12.ASiT & the trainee speciality associations' joint letter to surgical trainees. https://www.asit.org/news/asit-the-trainee-speciality-associations-joint-letter-to-surgical-trainees/nwc11200 Avaiable from. Accessed 19th August 2020.
- 13.General Medical Council (GMC) 2019. National Training Surveys.https://www.gmc-uk.org/about/what-we-do-and-why/data-and-research/national-training-surveys-reports Available from: Accessed 19th August 2020. [Google Scholar]
- 14.Sanghera J., Pattani N., Hashmi Y., Varley K.F., Cheruvu M.S., Bradley A., Burke J.R. The impact of SARS‐CoV‐2 on the mental health of healthcare workers in a hospital setting—a Systematic Review. J. Occup. Health. 2020 Jan;62(1) doi: 10.1002/1348-9585.12175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jones T.L., Baxter M.A., Khanduja V. A quick guide to survey research. Ann. R. Coll. Surg. Engl. 2013;95:5–7. doi: 10.1308/003588413X13511609956372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of internet E-surveys (CHERRIES) J. Med. Internet Res. 2004;6:e34. doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Woodward C.A. Questionnaire construction and question writing for research in medical education. Med. Educ. 1988;22:345–363. doi: 10.1111/j.1365-2923.1988.tb00764.x. [DOI] [PubMed] [Google Scholar]
- 18.Institute for government Coronavirus lockdown rules in each part of the UK. https://www.instituteforgovernment.org.uk/explainers/boris-johnson-plan-ease-coronavirus-lockdown Available from: Accessed 10th June 2020.
- 19.Royal College of Surgeons of England Recovery of surgical services during and after COVID-19. https://www.rcseng.ac.uk/coronavirus/recovery-of-surgical-services/ Available from: Accessed 10th June 2020.
- 20.National Research Collaborative & Association of Surgeons in Training Collaborative Consensus Group Recognising contributions to work in research collaboratives: guidelines for standardising reporting of authorship in collaborative research. Int. J. Surg. 2018;52:355–360. doi: 10.1016/j.ijsu.2017.12.019. [DOI] [PubMed] [Google Scholar]
- 21.Agha R., Abdall-Razak A., Crossley E., Dowlut N., Iosifidis C., Mathew G., for the STROCSS Group The STROCSS 2019 guideline: strengthening the reporting of cohort studies in surgery. Int. J. Surg. 2019;72:156–165. doi: 10.1016/j.ijsu.2019.11.002. [DOI] [PubMed] [Google Scholar]
- 22.COVIDSurg collaborative Elective surgery cancellations due to the COVID‐19 pandemic: global predictive modelling to inform surgical recovery plans. Br. J. Surg. 2020 May 12 doi: 10.1002/bjs.11746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.British Medical Association COVID-19: managing Junior doctor rota changes. https://www.bma.org.uk/advice-and-support/covid-19#rota-changes Available from: accessed 7th november 2020.
- 24.General Medical Council (GMC) National training surveys. 2020. https://www.gmc-uk.org/education/how-we-quality-assure/national-training-surveys Available from: Accessed 27th September 2020.
- 25.The four statutory educational bodies (health education England, health education and improvement wales, NHS education for scotland and the northern Ireland medical and dental training agency) supporting the COVID-19 response: guidance regarding medical education and training. https://www.gmc-uk.org/news/news-archive/guidance-regarding-medical-education-and-training-supporting-the-covid-19-response Available from: accessed 27th September 2020.
- 26.Joint Committee on Surgical training COVID-19 and trainee progression in 2020 (update V) – 7 august 2020. https://www.jcst.org/jcst-news/2020/08/07/news-item/ Available from: Accessed 27th September 2020.
- 27.Cunningham C.T., Quan H., Hemmelgarn B., Noseworthy T., Beck C.A., Dixon E., et al. Exploring physician specialist response rates to web-based surveys. BMC Med. Res. Methodol. 2015;15(1):4–11. doi: 10.1186/s12874-015-0016-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.James K.M., Ziegenfuss J.Y., Tilburt J.C., Harris A.M., Beebe T.J. Getting physicians to respond: the impact of incentive type and timing on physician survey response rates. Health Serv. Res. 2011;46(1):232–242. doi: 10.1111/j.1475-6773.2010.01181.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fan W., Yan Z. Factors affecting response rates of the web survey: a systematic review. Comput. Hum. Behav. 2010;26(2):132–139. doi: 10.1016/j.chb.2009.10.015. Available from: [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.