Abstract
Despite the paradigmatic shift occurred in recent years for defined molecular subtypes in the metastatic setting treatment, colorectal cancer (CRC) still remains an incurable disease in most of the cases. Therefore, there is an urgent need for new tools and biomarkers for both early tumor diagnosis and to improve personalized treatment. Thus, liquid biopsy has emerged as a minimally invasive tool that is capable of detecting genomic alterations from primary or metastatic tumors, allowing the prognostic stratification of patients, the detection of the minimal residual disease after surgical or systemic treatments, the monitoring of therapeutic response, and the development of resistance, establishing an opportunity for early intervention before imaging detection or worsening of clinical symptoms. On the other hand, preclinical and clinical evidence demonstrated the role of gut microbiota dysbiosis in promoting inflammatory responses and cancer initiation. Altered gut microbiota is associated with resistance to chemo drugs and immune checkpoint inhibitors, whereas the use of microbe-targeted therapies including antibiotics, pre-probiotics, and fecal microbiota transplantation can restore response to anticancer drugs, promote immune response, and therefore support current treatment strategies in CRC. In this review, we aim to summarize preclinical and clinical evidence for the utilization of liquid biopsy and gut microbiota in CRC.
Keywords: CRC, liquid biopsy, CTC, ctDNA, mi-RNA, nc-RNA, gut microbiota
1. Introduction
Colorectal cancer (CRC) is the third leading cause of cancer-related death and morbidity worldwide according to the global cancer statistics (GLOBOCAN) presented in 2018. The 5-year survival rate ranges from 90% to 14% if CRC is diagnosed at a localized or metastatic stage, respectively, and approximately 25% of CRC patients present metastatic disease at diagnosis, while almost half of them will develop metastases [1].
If early diagnosis and treatment of CRC can significantly improve the cure rate, traditional biomarkers (Carcino Embryonic Antigen (CEA), Carbohydrate Antigen 19-9 (CA19-9), Fecal Occult Blood Test (FOBT)) as well as colon/sigmoidoscopy do not fully satisfy clinical needs in CRC screening due to their lack in sensitivity and specificity [2]. Furthermore, primary tumor resection is eventually associated to adjuvant chemotherapy with fluoropyrimidines with or without oxaliplatin according to TNM stage and pathological risk factors in early CRC [3], does not always seem sufficient to eliminate circulating tumor cells (CTCs) and other components involved in establishing pre-metastatic niche-promoting immune evasion and maintenance of stemness [4].
Circulating tumor DNA (ctDNA) and RNAs and non-coding RNAs (ncRNAs) released into the bloodstream via microvescicles or tumor cell lysis represent, together with CTCs, different sides of the same coin: liquid biopsy. Liquid biopsy has emerged as a promising minimally invasive tool for precision medicine due to its ability to provide multiple global snapshots of primary and metastatic tumors at different times and more representative images of the spatial and temporal tumor heterogeneity [5] compared to tissue biopsy. In fact, even though tissue biopsy remains the gold standard for the histopatological definition and the molecular stratification of tumors, it is often difficult to perform, especially in relapsed and metastatic settings, and it does not support intratumoral heterogeneity and clonal evolutions related to driver mutations, which may occur during tumor development or treatment.
Among other elements potentially involved in cancer initiation, development, recurrence, and metastasis, one that only recently received its due attention is the host microbiota—and for CRC, especially the gut microbiota. The host microbiota is composed of bacteria (≈99%), viruses, and mycetes, existing in a condition of eubosis with the human body conferring important benefits related to physical and mental health, and the development of the individual [6]. In turn, this dynamic balance is affected by host genetics, lifestyle [7], and dietary habits [8] and gut microbiota dysbiosis may play a role in promoting inflammatory responses and alterations of the immunosurveillance, which can led to cancer initiation and/or progression [9].
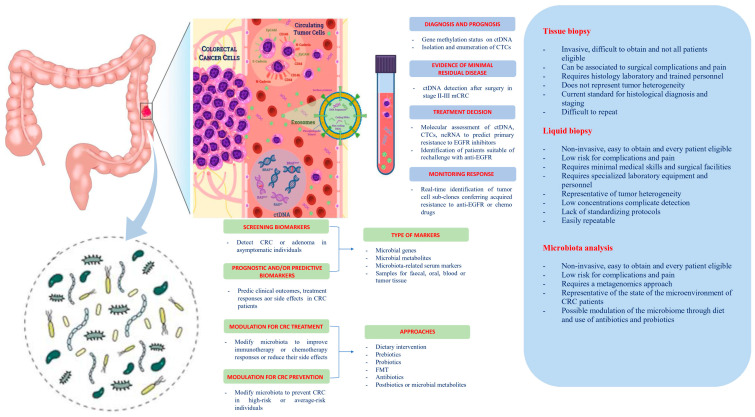
In this review, we summarize the state of the art regarding the potential role and the future perspectives of liquid biopsy and host microbiome as “theragnostic” tools in CRC (Figure 1).
Figure 1.
Potential clinical applications related to liquid biopsy and gut microbiota in colorectal cancer. Circulating tumor cells (CTCs), circulating tumor DNA (ctDNA), non-coding RNA (ncRNA), and exosomes are promising liquid biopsy markers for colorectal cancer with multiple potential advantages compared to tissue biopsy. CTCs from colorectal cancer (CRC) can be shed from the primary tumor into the bloodstream, which also contains ctDNA released from tumor tissue through apoptosis, necrosis, and secretion, as well as circulating normal DNA released from healthy tissue. NcRNAs (miRNAs and lncRNAs) encapsulated by exosomes can be actively secreted into the extracellular fluid by various types of cells in the tumor or passively released due to the apoptosis and necrosis of tumor cells and can eventually be found in the circulation. Besides liquid biopsy, several potential clinical applications for harnessing the gut microbiota in CRC include development of screening, prognostic and predictive biomarkers, and microbiota modulation for CRC prevention and treatment. FMT, fecal microbiota transplantation.
2. Liquid Biopsy
The term liquid biopsy refers to procedures of isolation of cancer-derived components such as CTCs, exosomes, ctDNA, ncRNAs, and proteins from peripheral blood or other body fluids, and their genomic or proteomic evaluation [10]. Assessment of such elements via non-invasive and low-risk blood-based detection tests could improve CRC screening, diagnosis, staging, and predict relapse and metastasis [11,12] and be effective in monitoring residual disease and drug resistance in CRC patients receiving systemic treatment [13,14].
2.1. Circulating Tumor Cells (CTCs)
CTCs are tumor cells released into the bloodstream from the primary tumor or metastases [15], which could escape from immune recognition and drug treatment, and subsequently form a niche in other tissues, promoting tumor recurrence and metastasis [16].
2.1.1. Screening and Early Diagnosis
Since counting CTCs reflects the patient’s tumor burden and the CTCs detection rate is positively correlated to the TNM stages, it is rather difficult and quite uncommon to detect CTCs in early-stage CRC, and therefore, their utility in CRC screening and early detection seems to be very poor [17]. However, a recent prospective study involving 667 patients (including healthy control subjects, patients with adenomas, and those with stage I–IV CRC) showed a significant association between CTC counts (performed using a novel CTC assay) and worsening disease status with respect to the adenoma-carcinoma sequence. Furthermore, the assay showed high specificity (86%) and sensitivity across all CRC stages (95%) and adenomatous lesions (79%) [18].
2.1.2. Prognostic and Predictive Factor, Staging Tool and Guide for Systemic Treatment, Resistance Evaluation, and MRD Assessment
CTCs could potentially play a role as a prognostic marker, in monitoring treatment outcomes and follow-up, for modulating the intensity of systemic therapies and for detecting resistance against these. A meta-analysis of 15 studies including 3129 non-metastatic and metastatic CRC (non-mCRC and mCRC) patients showed significantly worse progression-free survival (PFS) and overall survival (OS) for CTC-positive with respect to CTC-negative CRC patients, regardless of sampling time (baseline or during treatment), detection methods (CellSearch, RT-PCR and others), and cut-off value of CTC (≥1, ≥2 and ≥3/7.5 mL blood), thus providing strong evidence for the presence of CTCs as an independent prognostic factor of poor survival [19]. A study conducted on 158 patients showed that rising of CTCs counts in 2 mL of peripheral blood (0 for healthy, 1 for benign, 5 for non-mCRC, and 36 for mCRC patients) was associated with tumor progression and poor prognosis at baseline. Notably, after 2 year follow-up on the non-mCRC patients, those who had ≥5 CTCs were eight times more likely to develop distant metastasis within one year after curable surgery than those who had <5 [20], therefore providing a support to the possible application of CTC detection during the follow-up of early CRC patients. Intensive first-line regimens with a triplet chemotherapy backbone plus the antiangiogenic bevacizumab provided better survival outcome if compared with doublet regimens, especially in RAS-BRAF mutated mCRC [21,22], paying the price of a major incidence of adverse events. Patient stratification by CTC detection could help modulate the intensity of the systemic treatment by reserving a more aggressive therapy to patients with a worse prognosis. In the randomized phase III VISNÚ-1 trial, a first-line systemic treatment with FOLFOXIRI (oxaliplatin, irinotecan, 5-fluorouracil (5-FU), and leucovorin) plus bevacizumab significantly improved PFS compared with FOLFOX (association of oxaliplatin, 5-FU, and leucovorin) plus bevacizumab in mCRC patients with ≥3 CTCs/7.5 mL blood at baseline [22]. In RAS-BRAF wild-type mCRC, a standard first-line regimen includes a doublet chemotherapy backbone in association with an anti-EGFR antibody (panitumumab or cetuximab), usually followed at disease progression by the alternative doublet regimen in association with an antiangiogenic drug [23,24]. As showed by a prospective study on 38 RAS-BRAF wild-type mCRC patients who received a third-line treatment with irinotecan and cetuximab, early CTC-negative and CTC status changes assessment during treatment were significantly associated with tumor response and better PFS and OS, predicting treatment failure in advance compared to imaging-based tools [25].
2.2. Circulating Tumor DNA (ctDNA)
Circulating tumor DNA (CtDNA) is a kind of double-stranded DNA, a fragment of cell-free DNA (cfDNA), that originates from active, apoptotic, necrotic, or circulating tumor cells. CtDNA retains epigenetic characteristics and harbors tumor-specific mutations detectable in the bloodstream and other body fluids [10,26]. Importantly, ctDNA half-life varies from several minutes to a few hours, and as for CTCs, its plasma levels depend on tumor load, ranging from 50% to 90% in non-metastatic and metastatic cancer patients, respectively [4,10,25,27]. Furthermore, healthy people and cancer patients can be distinguished according to the fragment length distribution pattern of cfDNA [26]. These data suggest that ctDNA analysis may represent a real-time tumor burden assessment.
2.2.1. Screening and Early Diagnosis
Even if a recent meta-analysis concerning quantitative analysis of ctDNA for CRC screening, including 1258 CRC patients and 803 healthy individuals from 14 studies, concluded that the diagnostic accuracy of ctDNA has unsatisfactory sensitivity but acceptable specificity for CRC diagnosis [28], there is growing evidence that ctDNA detection could be used along with the traditional screening methods (i.e., colonscopy, FOBT, digital rectal examination, and serum tumor marker) to improve the diagnosis of early CRC [16,29]. In particular, ctDNA, especially when combined with carcinoembryonic antigen (CEA), showed higher diagnostic capacity (area under the ROC curve (AUC) 0.92, with 84% sensitivity and 88% specificity) [30]. Furthermore, epigenetic changes as DNA methylation and histone modifications are early events in carcinogenesis and clinical data that suggest that ctDNA methylation shows better sensitivity than traditional serum tumor markers in early-stage CRC [31,32]. Particularly, a meta-analysis of 25 studies assessing the diagnostic role of methylated Septin 9 (mSEPT9) promoter in ctDNA for CRC screening highlighted the efficacy of Epi proColon 2.0 with 2/3 algorithm (Epigenomics). A positive ratio of mSEPT9 was higher in advanced CRC stages (45%, 70%, 76%, 79% in I, III, III, and IV, respectively) and low-grade tumors (31%, 73% and 90% in high, moderate, and low grade, respectively), with a sensitivity, specificity, and AUC of 0.71, 0.92, and 0.88, respectively. Previous results confirmed the poor ability of mSEPT9 to identify precancerous lesions [31]. On the other hand, a recent prospective cohort study conducted on a high-risk population of 1493 individuals demonstrated that a particular single ctDNA methylation marker, cg10673833, could reach high sensitivity (89.7%) and specificity (86.8%) for the detection of CRC and precancerous lesions [32].
2.2.2. Prognostic and Predictive Factor, Staging Tool, and Guide for Systemic Treatment, Resistance Evaluation, and MRD Assessment
A systematic review and metanalysis including 1076 mCRC patients treated with chemotherapy and/or targeted agents showed that lower baseline levels of cfDNA correlated with better OS [33]. A more recent systematic review and meta-analysis including 1779 non-mCRC and mCRC patients found that the presence or high concentration of ctDNA with KRAS mutation was associated with poor disease-free survival (DFS), PFS, and OS [34]. Moreover, as anti-EGFR therapy with cetuximab and panitumumab is approved for wild-type RAS mCRC and KRAS and BRAF are considered effective predictors of anti-EGFR therapy [35,36], ctDNA detection could represent an alternative tool for the selection of anti-EGFR treatment due to its correlation with RAS mutational status of tumor tissue [37]. In particular, RAS clones raised in blood during EGFR blockade decline after the withdrawal of anti-EGFR antibodies, therefore restoring the drug sensitivity of cancer cells and providing a rationale for anti-EGFR retreatment [37]. Moreover, ctDNA has a great potential to supplement Response Evaluation Criteria in Solid Tumors (RECIST) evaluation. As already discussed, ctDNA is strictly dependent by tumor load, and tumor burden can be monitored in real-time due to the short half-life of ctDNA [26,27]. Compared to radiological approaches, serial monitoring of ctDNA is able to track treatment response weeks to months earlier, allowing anticipating disease progression and modifying treatment consequently [37]. A prospective phase II clinical trial of cetuximab in RAS wild-type mCRC patients combined the sequential profiling of ctDNA and matched tissue biopsies with imaging and mathematical modeling of cancer evolution, showing that liquid biopsies were able to detect spatial and temporal heterogeneity of resistance to anti-EGFR monoclonal antibodies [38]. In another phase II trial that tested the multikinase inhibitor regorafenib in RAS mutated mCRC patients, combining dynamic contrast-enhanced (DCE), MRI, and ctDNA predicts the duration of antiangiogenic response to regorafenib, improving patient management with potential health and economic implications [39]. As for CTCs, ctDNA concentration is positively correlated with tumor size, resulting lower in stage I with respect to stage IV CRC patients [15,16,40]. As a result of the strong link between CTCs, ctDNA, primary tumor, and metastasis, it has been suggested to integrate the blood-based liquid biopsy into the actual TNM staging system, and the concept of “TNMB” (B as blood) has been proposed to improve the existing cancer staging system [2,4,41]. In this regard, the ability to optimize systemic treatments, especially in the adjuvant setting in stage II-III CRC patients, has been historically limited by the use of clinicopathologic characteristics, which are not always able to properly prognosticate the risk of recurrence [42], and by conventional surveillance modalities (CEA, computed tomography (CT), and colonoscopy), which are not perfectly able to identify MRD and early recurrence [2,4,11,12]. In a prospective cohort of 230 stage II CRC patients, 7.9% were postoperative ctDNA positive, 79% of whom relapsed, while disease relapse occurred only in 9.8% of ctDNA-negative patients. The presence of ctDNA after the completion of chemotherapy was also associated with worse recurrence-free survival [43]. In a recent prospective cohort of 130 stage I–III CRC patients, ctDNA was quantified pre- and postoperatively, and after adjuvant chemotherapy. CtDNA-positive patients after surgery, adjuvant chemotherapy, and during follow-up were respectively 7, 17, and 40 times more likely to relapse with respect to ctDNA-negative patients [44]. Some authors proposed that monitoring ctDNA levels every 3-6 months after surgery can be used to supplement serum markers, CT, endoscopy, and other conventional monitoring tools, emphasizing that positive ctDNA preceded radiological and clinical evidence of recurrence by a median of 3 months, even if 6% of patients with positive ctDNA never relapsed [45]. A great effort is ongoing to validate the clinical utility of ctDNA, particularly in the adjuvant setting of CRC (Table 1).
Table 1.
List of major ongoing prospective trials investigating liquid biopsy in colorectal cancer.
| Brief Study Title | NCT Number/Study Name | Country Study Period | Stage | N | Study Type/Phase/Endp | Target/Assay-Test (If Available) | Study Overview/Schematic Description |
|---|---|---|---|---|---|---|---|
| ctDNA Analysis Informing ACT in Stage III CRC | ACTRN 12617001566325 (DYNAMIC-III) | Australia 2017–2024 |
III | 1000 | Int rand/2–3/DFS, OS, ctDNA clear | ctDNA | Surgery followed by ctDNA detection and clinician’s choice ACT (no ACT > fluoropyrimidine > XELOX/FOLFOX) followed by randomization to: (1) SOC arm: SOC ACT (ctDNA blinded) or (2) EXP arm ctDNA+: escalated ACT (FOLFOXIRI allowed) or (3) EXP arm ctDNA-: de-escalated ACT |
| ctDNA Analysis Informing ACT in Stage II CRC | ACTRN 12615000381583 (DYNAMIC II) | Australia 2015–2024 |
II | 450 | Int rand/2/DFS, OS, ctDNA clear | ctDNA | Surgery followed by ctDNA detection and randomization to: (1) SOC arm: SOC, (2) EXP arm ctDNA+: ACT (fluoropyrimidine or XELOX/FOLFOX according to clinician’s choice), (3) EXP arm ctDNA-: follow-up |
| Tracking mutations in ctDNA to predict relapse in early CRC | NCT04050345 (TRACC) | UK 2016–2024 |
HR II-III | 1000 | Int rand/3/DFS, OS, QoL | ctDNA/RM NGS | Surgery followed by randomization to: (1) SOC arm: SOC ACT, (2) EXP arm: ctDNA guided de-escalated ACT—If ctDNA-: CAPOX × 3 months is reduced to cape x 6 months and CAPE × 6 months is reduced to observation—After 3 months if ctDNA+: switch to CAPOX |
| ctDNA Based Decision for ACT in CRC Stage II Evaluation | NCT04089631 (CIRCULATE) | Germany Austria Switzerland 2019–2026 |
II | 4812 | Int rand/3/DFS, OS, TT ctDNA clear | ctDNA/Dresden NGS | After radical surgery, ctDNA+ are randomized to: (1) CAPE × 6 months (or CAPOX × 3–6 months, investigator choice) or (2) follow-up and CtDNA- are randomized to: (1) follow-up inside the study or (2) follow-up outside the study (off-study) |
| Decision for ACT in stage II CRC based on ctDNA | NCT04120701 (CIRCULATE-PRODIGE 70) | France 2019–2026 |
II | 1980 | Int rand/3/DFS, TTR, OS, ctDNA clear | ctDNA/ddPCR of 2 methylated probes | After radical surgery, ctDNA+ are randomized to: (1) ACT (FOLFOX) or (2) surveillance inside the trial. CtDNA- are randomized to (1) surveillance inside the trial or (2) surveillance outside the trial |
| ctDNA guided ACT in stage II CRC according the trials within cohorts design | Planning NTR6455 (MEDOCC CrEATE) | Netherland 2018–2022 |
LR II | 1320 | Int rand/3/DFS, OS, QoL | ctDNA/gene panel (PG Dx elio platform) | Surgery followed by randomization to: (1) EXP arm: if ctDNA+ FOLFOX/CAPOX × 6 months or follow-up (patient choice), (2) EXP arm: if ctDNA- follow-up, (3) SOC arm: follow up (ctDNA tested later) |
| Intervention Trial Implementing Non-invasive ctDNA Analysis to Optimize the Operative and Postoperative Treatment for CRC Patients | NCT03748680 (IMPROVE-IT) | Denmark 2018–2025 |
I-II | 64 | Int rand/2/DFS, LR, TTR, OS, ctDNA clear | ctDNA/NGS + ddPCR | After radical surgery, ctDNA+ patients with no indication to ACT according to DCCG guidelines are randomized to: (1) SOC arm: intensified follow-up or (2) EXP arm: CAPOX or FOLFOX followed by intensified follow-up |
| ctDNA Testing in Predicting Treatment for Patients With Stage IIA CRC After Surgery | NCT04068103 (COBRA) | USA Canada 2019–2024 |
IIA | 1408 | Int rand/2–3/ctDNA clear, RFS, OS, TTR | ctDNA | After radical surgery, patients are randomized to: (1) SOC arm: active surveillance (blood stored and tested for ctDNA later), (2) EXP arm ctDNA+: FOLFOX or XELOX × 6 months, (3) EXP arm ctDNA-: active surveillance |
| Early identification and treatment of occult metastatic disease in stage III CRC | NCT03803553 | USA 2020–2023 |
III | 500 | Int/3/DFS, OS, ctDNA clear | ctDNA | Surgery followed by SOC ACT followed by ctDNA assessment for MRD: (1) ctDNA+ MSI-h: Nivolumab, (2) ctDNA+ BRAF V600E: Enco/Bini/Cet × 6 months, (3) ctDNA+ others: randomization to FOLFIRI × 6 months or SOC observation, (4) ctDNA-: SOC observation |
| Post-surgical Liquid Biopsy-guided Treatment of Stage III and HR Stage II CRC Patients | NCT04259944 (PEGASUS) | Italy Spain 2020–2023 |
HR II- III | 140 | Int/2/DFS, OS, TT, QoL, ctDNA clear | ctDNA/LUNAR1 test | After surgical surgery: (1) ctDNA+: CAPOX × 3 months, (2) ctDNA-: CAPE × 6 months and early switch to CAPOX if ctDNA+ after first cycleAfter ACT: (3) ctDNA+/+: FOLFIRI × 6 months, 2 ctDNA-/+: CAPOX × 3 months, switch to FOLFIRI if still ctDNA-/+, 3ctDNA+/-: CAPE × 3 months, switch to FOLFIRI if ctDNA+/+ after 3 LB, (4) ctDNA-/-: follow-up, switch to CAPOX if ctDNA+ after 2 LB |
| Initial Attack on Latent Metastasis Using TAS-102 for ctDNA Identified CRC After Curative Resection | NCT04457297 (ALTAIR) | Japan 2020–2023 |
I-IV resected | 240 | Int rand/3/DFS, OS, TT | ctDNA/Signatera test | After radical surgery and SOC ACT, ctDNA+ patients are randomized to: (1) EXPrm: TAS-102 × 6 months or (2) SOC arm: placebo x 6 months |
| A Phase II Clinical Trial Comparing the Efficacy of RO7198457 Versus Watchful Waiting in Patients With ctDNA positive, Resected HR Stage II and Stage III CRC | NCT04486378 BNT122-01 | USA 2020–2023 |
HR II-III | 201 | Int rand/2/DFS, OS, TTR, TTF, TT | ctDNA | After radicalsurgery, ctDNA+ patients receive SOC ACT and are then randomized to: (1) EXP arm: RO7198457 (a personalized cancer vaccine) or (2) SOC arm: watchful waiting |
| ctDNA Analysis to Optimize Treatment for Patients with CRC | NCT03637686 (IMPROVE) | Denmark 2018–2026 |
III | 1800 | Obs/DFS | ctDNA | Part I—Surgery: ctDNA detection pre- and postoperative. Part II—Surveillance: ctDNA detection over 5 years follow-up |
| BESPOKE study of ctDNA guided therapy in CRC | NCT04264702 | USA 2020–2024 |
II-III | 1000 | Obs/DFS | ctDNA/Signatera test | To examine the impact of SIGNATERA test on ACT decisions and clinical outcomes during a 2-year follow-up |
| Use of ctDNA for Monitoring of Stage III CRC | NCT02842203 (PRO16020374) | USA 2016–2021 |
III | 150 | Obs/OS, PFS | ctDNA | ctDNA serial assessment up to 5 years and correlation with CEA and clinical outcomes |
| The implication of ctDNA in the recurrence surveillance of stage II and III CRC | NCT03416478 FFJC2017-01 | China 2018–2020 |
II-III | 50 | Obs/DFS, OS | ctDNA | ctDNA serial assessment before and after curative surgery up to 2 years of follow-up |
| A phase II Clinical Trial comparing Efficacy of RO7198457 vs. watchful waiting in ctDNA positive stage II–III resected CRC | NCT04486378 | USA 2020–2027 |
II-III | 201 | Int rand/2/DFS, RFS, TTR, TTF, OS, TT, ctDNA clear | ctDNA | To compare the efficacy of RO7198457 vs. watchful waiting after surgery and SOC ACT in ctDNA positive stage II–III CRC |
| ctDNA as a Prognostic Marker for Postoperative Relapse in Early and Intermediate Stage CRC | NCT03312374 | China 2017–2020 |
II-III | 350 | Obs/DFS | ctDNA/NGS | ctDNA serial assessment before and after curative surgery and ACT up to 2 years of follow-up |
| The Implication of Plasma ctDNA Methylation Haplotypes in Detecting CRC and Adenomas | NCT03737591 | China 2018–2020 |
I-IV adenomas healthy | 500 | Obs | ctDNA/NGS | To evaluate the sensitivity and specificity of ctDNA methylation haplotypes in detecting CRC and adenomas |
| Dynamic monitoring of ctDNA methylation to predict relapse in stage II–III CRC after radical resection | NCT03737539 | China 2018–2022 |
II-III | 300 | Obs/DFS | ctDNA/NGS | To correlate and compare postoperative, pre- and post-ACT ctDNA methylation markers with radiological imaging and clinical outcomes |
| Ct-DNA Testing in Guiding Treatment for Patients With Advanced or Metastatic CRC | NCT03844620 | USA 2019–2020 |
III (uncurable)-IV | 100 | Int/2/TT, ctDNA clean, QoL, ORR, OS | ctDNA | Monitoring and correlating ctDNA changes and radiological progression or TT incidence during third-line SOC (TAS-102/Regorafenib) (arm A) vs. third-line SOC alone (arm B) |
| Predictive and Prognostic Value of Inflammatory Markers and microRNA in Stage IV CRC | NCT04149613 | USA 2018–2021 |
IV | 100 | Obs | miRNAs | To evaluate the expression of selected microRNAs and inflammatory markers in patients with stage IV CRC and assess their correlation with tumor location, dietary patterns, survival rates, response to systemic chemotherapy, and other clinic-pathological parameters |
| Molecular Pathology of CRC: Investigating the Role of Novel Molecular Profiles, microRNAs, and their Targets in CRC Progression | NCT03309722 | UK 2008–2025 |
I-IV | 1000 | Obs/OS, DFS, LR, DR | miRNA | Single-center observational cohort study of prospectively recruited patients for biomarker evaluation and identification of novel biomarkers |
| Contents of Circulating Extracellular Vesicles: Biomarkers in CRC Patients | NCT04523389 (ExoColon) | France 2020–2021 |
I-IV | 172 | Obs/OS, PFS, LR, DR | Exosomes | To investigate the prognostic and predictive role of exosomes and their contents (miRNAs and others) |
| ColoCare Transdiciplinary Research in CRC Prognosis | NCT02328677 | USA 2007–2030 |
I-IV | 5000 | Obs/OS, DFS, QoL, TT | ctDNA, MiRNAs | To investigate the prognostic and predictive role of liquid biopsy in CRC patients in a 5-year follow-up |
| Timing To Minimally Invasive Surgery After Neoadjuvant Chemoradiotherapy For Rectal Cancer: A Multicenter Randomized Controlled Trial—Biomarkers SubStudy | NCT03962088 (TiMiSNAR) | Italy 2019–2023 |
II-III | 200 | Obs/pCR, DFS | miRNA/miRNeasy Mini kit by Qiagen | (1) To investigate the association between pre-neoadjuvant and post-neoadjuvant expression levels of miRNA with pCR. (2) To investigate the correlation between changes in expression levels of miRNA following complete surgical resection with DFS and the relation between changes in miRNA during surveillance and tumor relapse |
| microRNAs Tool for Stratifying Stage II CRC: a Perspective Study of ACT | NCT02635087 | China 2015–2025 |
II | 630 | Obs/DFS, OS | miRNA | To investigate the predictive and prognostic role of miRNAs in stage II CRC, stratifying patients at “high risk” and at “low risk” of recurrence according to a six miRNAs tool |
| Assessment Of Long Noncoding RNA CCAT1 Using Real-Time Polymerase Chain Reaction In CRC patients | NCT04269746 | Egypt 2020–2021 |
Diagnostic | 100 | Obs | lncRNA | To evaluate the clinical utility of detecting long non-coding RNA (CCAT1) expression in diagnosis of CRC patients and its relation to tumor staging |
ctDNA: circulating tumor DNA; Endp: study endpoints if not reported in study description; N: planned enrollment; Obs: observational; Int: interventional; CT: chemotherapy; LB: liquid biopsy; dPCR: digital PCR; ddPCR: digital droplet PCR; SOC: standard of care; ACT: adjuvant chemotherapy; NA: not available; Enco/Bini/Cet: Encorafenib/Binimetinib/Cetuximab; HR: high risk according to histopathological factors; LR: low risk according to hystopatological factors; ctDNA clear: ctDNA clearance or modification rate of every study arm and correlation with clinical outcome measures (according to the design of each study); OS: overall survival; DFS: disease-free survival; RFS: relapse-free survival; LR: local recurrence; DR: distant recurrence; QoL: quality of life; TT: treatment toxicity/treatment-related adverse events; pCR: pathologic complete response; TTF: time to treatment failure; TTR: time to recurrence.
2.3. MicroRNAs (miRNAs) and Long Non-Coding RNAs (lncRNAs)
MicroRNAs (miRNAs) and long non-coding RNAs (lncRNAs) are ncRNAs molecules involved in the regulation of protein-coding gene expression through mRNA degradation and silencing or activating and repressing genes via a variety of mechanisms at both transcriptional and translational levels. Both classes of ncRNAs regulate multiple cellular processes such as growth, development, and differentiation showing to be crucial for cancer initiation, progression, and dissemination and can be found in serum or other body fluids bound to protein or lipid complexes, or more frequently inside extracellular vescicles (i.e., exosomes) [46]. Furthermore, these elements seem to be strongly associated with the development of drug resistance in CRC [47,48,49,50]. For these reasons, miRNA and lncRNAs could have potential application in diagnosis, prognosis, and treatment of CRC.
2.3.1. Diagnosis and Prognosis
MiR-150 appears upregulated in CRC and its downregulation together with elevated Gli1 (glioma-associated oncogene homolog 1) expression seems to be involved in the process of epithelial–mesenchymal transition (EMT), which is a necessary step in promoting invasion and metastasis in CRC [51]. The results of a recent metanalysis suggest that miR-150 could be effective as a diagnostic biomarker for CRC patients, while no significant evidence was found concerning its prognostic role [52]. Mir-181 seems to be involved in multiple signaling pathways such as FOXO, PI3K-Akt, VEGF, HIF-1, mTOR, and cAMP, therefore representing a promising biomarker with potential predictive and prognostic significance in CRC [53]. MiR-21, miR-200a, miR-543, miR-32, miR92a, miR-26a, miR-1061, and miR-181a act as oncogenes downregulating the oncosuppressor PTEN (phosphatase and tensin homolog), which is a diagnostic factor for CRC patients, therefore representing potential targets for CRC therapy [54]. The upregulation of miR21, miR215, miR143-5p, and miR106a is associated with worse prognosis in stage II CRC patients [55]. A panel of miR-21, miR29a, and miR125b is able to carefully distinguish between early CRC and healthy controls (AUC = 0.827) [56]. Serum miR-203 upregulation seems to be related to worse prognosis (HR = 2.1) and higher risk of liver (OR = 6.2) or peritoneum (OR = 7.2) metastasis [57]. In a population of 400 CRC patients, a four-miRNA panel (miR-142-5p, miR-23a-3p, miR376c-3p, and miR271-3p) showed good diagnostic performance (AUC = 0.922), while a two-miRNA signature (miR-23a-3p and miR-376c-3p) proved to be a prognostic tool for 3-year OS (HR = 2.30) [58].
A study focusing on circulating serum exosomes showed that the levels of lncRNA HOTTIP could predict OS in CRC patients and discriminate between CRC and healthy controls (AUC = 0.75) [59].
A recent systematic review and meta-analysis of 111 articles including 13,103 gastrointestinal cancer patients (3123 with esophageal cancer, 4972 with gastric cancer, and 5008 with CRC) showed that 74 lncRNAs were closely associated with poor prognosis in gastrointestinal cancer, including 58 significantly upregulated and 16 significantly downregulated lncRNA expression, and with a strong interaction with miRNAs for 12 of these lncRNAs [60].
2.3.2. Drug Resistance
Several oncogenic miRNAs can promote platinum and fluoropyrimidine resistance. Complex interactions between miRNAs (miR-181a-5p, miR-136, miR-363-3p, miR20b-5p, miR-218, miR-145, Let-7a, miR141) and lncRNAs (CRNDE, LUCAT1, MALAT1, GIHCG, CASC15, ANRIL, MEG3, CCAL) in the context of Wnt/β-catenin and MDM2-P53 signaling pathways are ultimately involved in oxaliplatin resistance [47]. Moreover, mir-153, miR19b-3p, miR-203, and miR-625-3p upregulation in the context of FOXO3a, SMAD4, and ATM pathways, respectively, is associated with oxaliplatin resistance [48]. The upregulation of LncRNA NEAT1 acts as an oncogene in CRC through the regulation of CPSF4 expression, sponging miR-150-5p. The upregulation of NEAT1 ultimately results in 5-FU resistance, suppressed apoptosis, and enhanced invasion of CRC [49]. A recent systematic review and meta-analysis of 39 studies including 2822 CRC patients consistently showed that multiple miRNAs (almost 60) could act as clinical predictors of chemoresistance and sensitivity for a combination of 14 drugs, including 5-FU and oxaliplatin. Particularly, 28 miRNAs were associated with chemosensitivity, 20 were associated with chemoresistance, 1 was associated with differential expression and radiosensitivity, while 10 were not associated with any impact on chemotherapy. These results outline the importance of almost 34 drug-regulatory pathways of chemoresistance and chemosensitivity in CRC that are potentially targetable [61].
3. Microbiota
The study of microbiota started several years ago, and multiple definitions have been conceived to explain its meaning [62]. In general, the terms “microbiota” and “microbiome” refer to the complex of organisms found within a specific environment and their genomic pool, respectively [63,64]. Thus, the human gut microbiota consists of a multitude of microorganisms colonizing the gut and existing in that complex state of dynamic equilibrium (i.e., eubiosis), which is made of reciprocal interactions and multiple networks between themselves and the host cells. This is an equilibrium with specific spatial and temporal characteristics, whose deregulation might lead to dysbiosis [63].
The human gut microbiota—with its thousands of different bacterial taxa, eucaryotic microbes, and virus together with the intestinal barrier—is a very selective and important filter for the well-being of the whole organism, and as a neuroendocrine structure today considered as a “second brain”, it is a component of the complex gut ecosystem [65,66]. The gastrointestinal microbiota varies according to the anatomical location and among individuals [11], and it plays different roles, from the supply of nutrients to the control of inflammation and carcinogenesis [63]. Commensal bacteria instruct the immune and physiological systems throughout life and are responsible for the presence of inflammatory and immune cells in the healthy intestine: the so-called “physiological” or “controlled” inflammation [67]. For this purpose, numerous evidence has demonstrated that a direct relationship between modification in the gut microbiota composition and some pathologies exist [68,69]. Among these diseases, obesity and metabolic alterations induced by some nutrients and diet, or autoimmune diseases such as type 1 diabetes and inflammatory bowel disease, are characterized by changes in the microbiome and gut dysbiosis [70].
3.1. Microbiota and Cancer
Gut microbiota emerged as a critical player also in the development of cancer. Several studies support the idea that a disturbance of the gut microbiota composition could lead to the onset of CRC [71]. Moreover, several studies reported a deep association between microbiota and CRC, demonstrating that microbiota dysbiosis can affect cancer susceptibility and progression through the modulation of several mechanisms such as inflammation, or inducing DNA damage, and producing metabolites involved in oncogenesis or tumor suppression [72]. For example, various bacterial pathogens are linked with the DNA damage response (DDR) pathway activation, which can be caused by both a direct effect of microbe produced genotoxins or an indirect effect of ROS produced in response to an excessive activation of immune cells stimulated by certain microbes or their metabolic end-products [73,74].
In particular, fecal metagenomic samples from CRC patients identified a CRC-enriched microbiota including Enterobacteriaceae [75], Escherichia coli [76,77], Enterotoxigenic Bacteroides fragilis (ETBF) [78], and Fusobacterium nucleatum (Fn) [79]. These bacteria seem to act as “pro-oncogenic” agents in different ways: promoting inflammation, impairing antitumor activity, inducing DNA damage, and tumor cell proliferation via the activation of β-catenin and other oncogenic pathways [75]. Several studies reported an association between an abundance of Fusobacterium nucleatum, carcinogenetic risk factors, and gene mutations in CRC [80]. In addition, a high abundance of Fusobacterium nucleatum was associated with CIMP status, wild-type p53, and MSI in colon tumor tissue [81].
On the other hand, the Firmicutes phylum (particularly the Ruminococcaceae and Lachnospiraceae families) [82] as well as Bifidobacteria, Lactobacilli [83,84] and non-enterotoxigenic Bacteroides fragilis (NTBF) [84] are substantially underrepresented in CRC patients [85] and have shown “anti-oncogenic” activities, such as a reduction of pro-inflammatory citokines, enhancement of antitumor immunity, epithelial cell renewal, regulation of intestinal barrier integrity, and short-chain fatty acid (SCFA) production [82,83,84,85,86]. SCFAs, by modulating histone deacetylase inhibitory activity, promote the accumulation and differentiation of Treg cells controlling tumor progression [86].
Similarly, a deeper review on the role of gut microbiota in the carcinogenesis of humans and animals observed that some bacteria appeared often augmented (including Fusobacteria, Alistipes, Porphyromonadaceae, Coriobacteridae, Staphylococcaceae, Akkermansia spp., and Methanobacteriales), whereas others decreased in CRC (Bifidobacterium, Lactobacillus, Ruminococcus, Faecalibacterium spp., Roseburia, and Treponema [87]. In addition, some microbial metabolites (such as nitrogenous compounds) were consistently elevated, whereas others (such as butyrate) were decreased throughout colonic carcinogenesis [87].
3.2. Signaling Pathways Activated in Microbiota and Cancer
The gut microenvironment homeostasis requires an intricate balance between cell proliferation, differentiation, and apoptosis processes in which several regulatory pathways are involved such as the Wnt, Notch, BMP, and Hedgehog signaling pathways [88,89]. Deregulation of these main signaling pathways can potentially determine a disruption of intestinal homeostasis and contribute to CRC development. For example, the Wnt/β-catenin signaling pathway is supposed to be closely connected with cancer biology [90]. In particular, the adenomatous polyposis coli (APC) gene truncating mutations that stabilize β-catenin are highly prevalent in CRC, making APC one of the most mutated genes in human cancers [91].
Among the canonical and non-canonical Wnt signaling pathways, the first is certainly the most critical for its function as regulator of the transcriptional co-activator β-catenin, in turn regulating inflammatory, proliferative, and differentiation pathways [92,93]. As reported in several studies, the Wnt pathway has been frequently considered together with the RAS pathway one of the major drivers of CSC expansion [93].
The gut microbiome can be the trigger of the (EMT), a transition taking place through the involvement of WNT and TGF-β signaling, as previously reported, causing the invasion and metastasis of CRC cells [94].
Recently, preclinical evidence demonstrated that defects in the colon barrier integrity associated with dysbiosis and with an increased expression of several inflammatory factors such as IL-17, Cxcl2, Tnf-α, and IL-1 can be responsible for the development of benign (e.g., hyperplastic polyp), pre-malignant (e.g., tubular adenoma), or malignant (e.g., colorectal adenocarcinoma) neoformations [71,95].
Taken together, these data suggest that alterations of gene expression or modifications of microbiota composition can trigger the development of cancer involving the deregulation of proliferative and inflammatory signaling pathways even though a clear cause–effect relationship between microbiota composition and changes in gene expression have not been well elucidated.
In conclusion, not only a genetic but also an epigenetic role has been highlighted in CRC progression and metastatization, as recently reported by Wu et al. [96].
3.3. Microbiota and Efficacy of Anticancer Agents
An emergent approach is taking into consideration the influence of the microbiota on the activity and efficacy of chemotherapy and immunotherapy drugs. For example, the hypothesis that gut microbiota can be strictly related to the pharmacological effects of chemotherapy agents, such as 5-FU, is supported by a pioneer study conducted with a CRC mouse model and high-throughput sequencing. The authors compared the tumor size and profiled the gut microbiota of mice treated with 5-FU, combined with probiotics or ABX (an antibiotic cocktail of antibiotics), demonstrating the importance of pre-existing gut microbiota communities in the host response to 5-FU treatment. In particular, they found that antibiotics-induced dysbiosis during CRC treatment determined a dramatic increase of Proteobacteria, which may interact with the host inducing systemic inflammation and abolishing the therapeutic efficacy of the drug [97].
Regarding human studies, Zhang and colleagues investigated the relationship between Fn infection and efficacy of a systemic treatment with 5-FU in 94 CRC patients. They initially hypothesized a mechanism of reduced chemo-sensitivity of CRC cells to 5-FU linked to the upregulation of BIRC3, which is a member of the inhibitor of apoptosis proteins (IAPs). Next, they demonstrated that Fn-induced BIRC3 expression could be mediated by the TLR4/NFkB pathway. Indeed, other scientists had recently reported that Fn may mediate chemoresistance by activating the autophagic pathway in CRC [98].
Immunotherapy has revolutionized cancer treatment, and immune checkpoint inhibitors (ICIs) are now a standard of care in microsatellite-instable (MSI) CRC patients [99].
Recently, Lang et al. in their study showed that ileal microbiota can orchestrate the immunogenic cell death of ileal intestinal epithelial cells (IECs). They registered an accumulation of follicular T-helper (TFH) cells in CRC patients and mice and the suppression of IEC apoptosis. This effect could be linked to the impairment of the immunosurveillance mechanisms by chemotherapy directed against CRC in mice [100]. Protective immune responses in the ileum were associated with the colonization of specific bacteria such as Bacteroides fragilis and Erysipelotrichaceae that stimulate the production of programmed cell death (PD-1) molecules +TFH by secretion of interleukin 1R1 and interleukin 12. Moreover, the demonstration of apoptosis in the ileum can be considered a prognostic factor for CRC patients [100].
As for the relationship between bacteria species infection and efficacy of treatments, it has been postulated that the richness and diversity of species could be influenced by the different stages of gastric carcinogenesis and progression. In particular, more relevant changes seem to occur at the stage of precancerous lesions of gastric carcinoma (PLGC), suggesting that it is a turning point during GC progression. Moreover, the depletion of some bacteria such as Akkermansia and an enrichment of pathogenic bacteria such as Escherichia Shigella can overlap with the tumor progression stage [100].
Moreover, researchers have reported a reduction in the efficacy of immunotherapy regimens in metastatic renal cell carcinoma (mRCC) patients when treated with antibiotic drugs. In particular, worse clinical outcomes in terms of PFS and OS were found in mRCC patients who received antibiotics within four weeks of treatment initiation with respect to non-users [101].
3.4. Recent Advances in Metagenomics Technology for Diagnosis and Prognosis
Currently, the study of microbiomes, also named metagenomics, is based on two main approaches, which consider different aspects of the microbial community in a given environment. The structural metagenomics approach takes into consideration the structure, composition, and dynamics in a specific ecosystem of the uncultivated microbial population. Instead, functional genomics aims to study a specific gene coding for a function of interest. This approach requires the generation of expression libraries with thousands of metagenomics clones and its subsequent screening [102].
Metagenomics, investigating the wide populations of microbial communities and analyzing all the DNA present within a sample, can provide comprehensive and useful data regarding the state of the microenvironment of CRC patients. In metagenomics, datasets acquired from recent studies of the taxonomic clades related to CRC have been discovered [103].
Moreover, Meyerson et al. by using whole-genome sequences established the configuration of microbiota in healthy and CRC patients [104]. By the way, thanks to the multi-omics approach based on the plethora of recent technologies including genomics, transcriptomics, proteomics, and metabolomics respectively able to analyze DNA markers, RNA transcript, protein, and metabolites produced inside the colon, researchers have a remarkable opportunity for the discovery of novel prognostic, diagnostic, and therapeutic biomarkers [104], even though the question of whether the microbiota and its metabolites could be considered replicable and useful biomarkers across cohorts and populations remains unclear. So, the aim of this interesting approach tries to examine the differences in patients and healthy individuals for identifying biomarker patterns to work toward a personalized medicine therapeutic approach [105].
For example, in a large cohort study conducted on 616 participants undergoing colonoscopy, the presence of distinct patterns of the microbiome in cases of multiple polypoid adenomas has been demonstrated. Fn appeared significantly elevated from intramucosal carcinoma to more advanced stages. Moreover, Atopobium parvulum and Actinomyces odontolyticus, which co-occurred in intramucosal carcinomas, were significantly increased only in multiple polypoid adenomas and/or intramucosal carcinomas. In addition, metabolome analyses indicated a significant increase of metabolites such as branched-chain amino acids and bile acids in intramucosal carcinomas. Futhermore, the authors suggested that the shift in the microbiome and metabolome seemed to occur from the very early stages of CRC development, confirming the potential diagnostic and etiological role of multi-omics data. Therefore, the authors proposed metagenomic and metabolomic markers to discriminate cases of intramucosal carcinoma from the healthy controls, highlighting the possible etiological and diagnostic importance of large-cohort multi-omics data [106]. Indeed, the application of metagenomics to explore the gut microbiota profile has also been prospectively investigated in 60 CRC patients and 30 healthy controls. This study revealed the importance of data from the gut microbiome in association with known clinical risk factors of CRC to discriminate between adenoma and carcinoma clinical groups [107]. On the other hand, a similar conclusion has been reported by a European study based on fecal samples metagenomic sequencing and taxonomic classification of a mixed group of CRC, adenomas patients, and healthy subjects. Indeed, this study indicated that observed gene pool differences may reveal tumor-related host–microbe interactions [108].
An emerging approach to study the intersection of the gut–microbial communities and human health is based on the study of microbe-derived extracellular vesicles (EVs). EVs, separated into three different types, outer membrane vesicles (OMVs), shedding vesicles, and apoptotic bodies, are composed of different macromolecules including lipids, proteins, nucleic acids, and metabolites [109,110].
For example, via metagenomic and metabolomics analysis of gut EVs of CRC and healthy subjects, Kim et al. found an alteration of compositional bacteria and metabolites profile in CRC patients, suggesting a potential diagnostic role of EVs metabolites profiles in the identification of cooperation between microbiome and cancer development [109].
3.5. Organoids Engineering
Organoid engineering has become an important tool for cancer assessment but also in modeling host–microbe interactions. New insights are rapidly being gained on the role of the microbiome in CRC development, and it is clear that CRC patients have an altered gut microbe population compared to healthy ones. However, whether they play a direct or indirect role in cancer development is a topic of great discussion [111].
Research suggests a key role for microbes in developing an inflammatory environment in which cancer cells can grow; they can also influence cancer development by producing metabolites that influence the host metabolism [112].
From a practical point of view, microbes can be administered to cell culture media, allow basolateral exposure, or be microinjected into the lumen of the organoid to faithfully reproduce the microbial activity [113].
For example, Pleguezuelos-Manzano et al. focused on the abundance, in stool samples of CRC patients, of some bacteria including E. coli and pks + E. coli, which are capable of producing the genotoxin colibactin. This toxin has been shown to damage DNA and create a non-physiological base pairing in epithelial cells [77].
By the use of organoids constituted with E. coli pKs + obtained from the colon of CRC patients co-cultured with the epithelial cells, these researchers reproduced in vivo the intestinal situation and demonstrated that exposure to E. coli pKs + would appear to be a risk factor in the development of CRC [114]. Therefore, in conclusion, the specificity of colibactin-induced mutations supports the need for further investigations relating to its link with cellular DNA as well as representing a valid support in the identification of a preventive biomarker [77].
New knowledge is also rapidly gaining in the field of “nutrition and gut microbiota”. Several studies have established that after the ingestion of phytochemicals and fibers, the intestinal microbiota initiates complex catabolism that releases important metabolites of the intestinal microbiome (GMMs). Moreover, thanks to the use of organoids derived from colorectal lesions, the impact of diet and metabolites on tumorigenesis has been also investigated [115].
Recently, Toden and colleagues identified evidence that metabolites produced by the microbial catabolism of flavan-3-ols in the distal gastrointestinal tract could induce programmed cell death, inhibiting cancer and promoting gut health [116]. They used intestinal organoids as a preclinical model system and noted that flavan-3-ols suppressed the formation and growth of both intestinal organoids—those derived from APCM in mouse models and those from human CRC tumors—by inhibiting the cell cycle and inducing apoptosis. The gene expression profile revealed the suppression of survival and self-renewal pathways in organoids treated with flavan-3-ols. Flavan-3-ols is a commercial grape seed extract, consisting of monomers, dimers, and trimers. These compounds include proanthocyanidins (PACs); they can reach the distal gastrointestinal tract almost intact and are effectively transformed into low molecular weight phenolic compounds by the colonic microbiota [117,118,119]. The flavan-3-ols monomers, dimers, and trimers that reach the colon become available for the gut microbiota. Then, microbial catabolism begins, producing hydroxy-phenyl-γ-valerolactones (PVLs) and, to a lesser extent, their derivative hydroxy-phenylvaleric acids (PVAs), with only a small percentage of non-metabolized PACs remaining [120].
3.6. Therapeutic Use of Antibiotics, Probiotics, and Fecal Microbiota Transplantation
Several approaches, which include dietary interventions, antibiotic treatments, pre- and probiotics, and fecal microbiota transplantation (FMT), have been explored to modulate gut microbiota composition, including its physiology and metabolites involved in CRC occurrence, progression, or drug resistance.
Diet plays a significant role in the modulation of the microbiome. A normal gut microbiota depends upon the fermentation of the indigestible fiber component of our diet for its energy supplement. The symbiotic gut microbiota ferments dietary fibers into short-chain fatty acids (SCFAs) such as propionate, acetate and, most importantly, butyrate [67]. In a prospective cohort study, a diet rich in whole grains and dietary fiber was associated with a lower risk to develop F. nucleatum-positive CRC but not F. nucleatum-negative CRC, supporting a potential role for intestinal microbiota in mediating the association between diet and colorectal neoplasms [121]. As no clear guideline regarding the type of nutrition and cancer incidence has been established, different forms of reduced caloric intake, such as fasting, demonstrated a wide range of beneficial effects in cancer prevention and anticancer drug efficacy [122], at least in part mediated by gut microbiota. Indeed, every-other-day fasting leads to an increase in fermentation products such as acetate and lactate altering gut microbiota composition, with enriched levels of Firmicutes, the production of SCFAs, and reduction in Bacteroides, Actinobacteria, and Tenericutes [123]. Since tumors are not able to metabolize ketone bodies due to deficiencies in key mitochondrial enzymes, a ketogenic diet with low-carbohydrate and high-fat intake, mimicking the metabolic state of fasting by inducing a physiological increase in acetoacetate and beta-hydroxybutyrate, might be a reliable therapeutic strategy to inhibit cancer progression [124]. Omega-3 polyunsatured fatty acids (PUFAs) are widely used as nutritional supplements and multiple benefits have been claimed, included anticancer activity. PUFAs seem to increase “anti-oncogenic” bacteria, including Bifidobacterium and Lactobacillus other than SCFA-producing genera such as Blautia, Bacterioides, Roseburia, and Coprococcus [125]. A randomized trial showed that omega-3 PUFA supplementation induces a reversible increase in several SCFA-producing bacteria [126].
Since antibiotic administration represents an aggressive and non-selective means of manipulation of gut microbiota composition, its role in CRC management seems to be controversial. Although preclinical evidence showed that gut microbiome depletion seems to inhibit cancer progression [127], multiple lines of evidence highlight how antibiotics can undermine immunotherapy efficacy or promote disease progression emphasizing microbial dysbiosis [128,129].
Of course, a potential strategy of CRC prevention and management is represented by probiotics and fecal microbiota transplantation (FMT). Probiotics are living microorganisms with the potential to positively influence resident microbiota, intestinal epithelium cells, and the immune system, and they are generally considered safe and well tolerated in healthy subjects [130]. A randomized trial with Lactobacillus and Bifidobacterium strains significantly reduced the levels of proinflammatory cytokines such as TNF-α, IL-6, IL-10, IL-12, IL-17, and IL-22 and prevented post-surgical complications.
FMT consists of the transplantation of gut microbiota from healthy donors to patients to restore intestinal dysbiosis and reduce the activation of inflammatory, proliferative, and procarcinogenic pathways. These specimens are prepared according to well-established protocols to avoid potential risk factors such as viruses and parasites and stored in banks of donated feces [131]. Treatment with chemotherapy and ICIs can result in adverse events including colitis. FMT treatment has been shown to improve ICI-induced colitis in cancer patients [132]. Additionally, FMT reduced the severity of intestinal mucositis and diarrhea following FOLFOX treatment in preclinical models by suppressing IL-6 levels, increasing the number of goblet cells and zonula occludens-1, decreasing apoptotic and NFkB-positive cells as well as the expression of Toll-like receptors and MYD88, leading to a restoration of gut microbiota composition without complications such as bacteremia [133]. Another study conducted in a mouse model to assess the efficacy of FMT to reverse antibiotic- and chemotherapy-induced gut dysbiosis suggests that FMT may effectively help in preventing acute intestinal inflammation and mucosal barrier dysfunction. In particular, the administration of FMT reduced the proportions of pathogenic species and an increase of the relative distribution of Clostridium scindens and Faecalibacterium prausnitzii, which are species that exhibited anti-inflammatory properties [134].
Finally, as demonstrated by Hefazi et al. in cancer patients treated with cytotoxic chemotherapy, FMT treatment determined a reduction of multiply recurrent Clostridium difficile infection (CDI) and diarrhea episodes remarking its highly therapeutic efficacy [135].
4. Future Perspectives and Conclusions
Despite the recent advances in the systemic treatment of molecularly selected CRC patients with advanced disease (i.e., pembrolizumab in MSI [99] or the association of the anti-BRAF encorafenib, the anti-MEK binimetinib and the anti-EGFR cetuximab in BRAF V600E mutated [136] tumors), the survival benefit is limited to a small percentage (10–20%) of patients harboring these alterations.
The use of CTCs, ctDNA, miRNAs, and lncRNA could help find new potentially targetable biomarkers for the management of CRC. Furthermore, as a minimally invasive and repeatable procedure, liquid biopsy can improve CRC screening, early diagnosis, clinical staging, and prognostic stratification, allowing a higher rate of cure. Moreover, liquid biopsy might be useful to monitor minimal residual disease after surgical treatment, possibly allowing a finer modulation of the adjuvant systemic therapy, integrating clinico-pathological risk factors and ctDNA or CTC detection. Finally, if properly integrated with clinical and instrumental assessment, liquid biopsy might help monitor disease progression, treatment efficacy, and acquired resistance to chemotherapy and targeted agents in CRC.
Of course, there is urgent need to optimize pre-analytical and analytical processing for clinical validity, to standardize laboratory methods in ensuring the reproducibility of the results and to properly assess the cost-effectiveness [137]. Indeed, the lack of clinical applicability is currently due to the large quantity of liquid biopsy assays, with different detection limits, sensitivity, and specificity [138]. To solve the pitfalls for liquid biopsies due to the difficulty of CTC detection, the application of various microfluidic platforms based on CTC characteristics has been explored [139]. Recently, for the selection of CTC, a “negative depletion” microfluidic chip has been developed [140]. In this system, named leukapheresis, the leukocyte depletion strategy can enrich for untagged CTCs in a “tumor-independent” manner applicable to all tumor types, as demonstrated in several tumor types [141,142,143,144].
CTC analyses performed on leukapheresis products should improve the reach of liquid biopsies in metastatic cancer, and combined with CTC detection, they may play a critical role in screening high-risk patients for early cancer, identifying the tissue of origin, and reducing the need for invasive biopsies.
Therefore, once the multiple ongoing randomized phase II–III trials will define and validate the role of liquid biopsy especially in the adjuvant setting of early CRC (Table 1), a process of harmonization of procedures and data will be necessary to transfer from bench to bedside this important tool of personalized medicine.
On the other hand, it is clear that CRC carcinogenesis is also defined by gut microbiota metabolic activity and its dysbiotic composition. Therefore, the integrated analysis of the gut microbiome and its interactions with the host, anticancer drugs, and other exogenous factors [7,139] is essential to improve the outcomes of CRC patients. Recent findings support the potential of microbial markers in cancer diagnosis and prognosis and the potential of FMT or pre-probiotics in remodeling the tumor microenvironment or in potentiating antitumor immunity. Continuous monitoring of changes in microbiota profiles and biomarkers may help in the identification of dysplasia. In addition, in this context, an important collaborative effort is required to elucidate the role of the gut microbiota in modulating responses to cancer treatment, and this aspect is particularly clear in several ongoing clinical trials investigating the effect of FMT in patients with cancer who are refractory to ICI. These trials, along with further validations, will determine whether the selective modulation of gut microbiota, either by FMT, probiotic treatment, or other means, enables CRC patients to overcome resistance to chemotherapy or immunotherapy (Table 2). Of course, a more complete and holistic approach toward cancer treatment should include host–microbiota interactions as important screening and treatment factors.
Table 2.
List of major ongoing prospective trials investigating the role of microbiota in colorectal cancer.
| Brief Study Title | NCT Number/Study Name | Country Study Period | Stage | N | Study Type/Phase (If Applicable) | Intervention | Study Overview/Schematic Description |
|---|---|---|---|---|---|---|---|
| Gut Microbiome Dynamics in Metastasized or Irresectable CRC | NCT03941080 GIMICC | Netherlands 2020–2022 |
IV | 300 | Obs | Fecal and blood sample collection + behavioral questionnaire at baseline and every 3 months | To investigate characteristics and alterations of the gut microbiome and its predictive value for RR and TT during CT for mCRC |
| Gut Microbiome and Oral Fluoropyrimidine Study in Patients With CRC | NCT04054908 GO | USA 2018–2022 |
all | 60 | Obs | 1 stool sample at baseline and at least 1 stool sample during treatment + questionnaires regarding bowel habits and dietary habits | To investigate the alterations of the gut microbiome occurring in three cohorts of CRC: Cohort A: patients treated with CAPE as SOC, Cohort B: patients treated with TAS-102 with or without Y-90 radioembolization in T, Cohort C: patients treated with CAPE + pembrolizumab + bevacizumab in T |
| Human Intestinal Microbiome and Surgical Outcomes in Patients Undergoing CRCCancer Surgery | NCT04005118 Microbiota | France | all | 50 | Obs | 2 fresh fecal samples for LM detection (1 pre- and 1 post-operatively) + 1 intraoperatively sample for MAM | To investigate the association between microbiome composition and occurrence of postoperative complications (anastomotic leakage, surgical site infection, prolonged postoperative ileus) |
| Bowel Preparation Impact on the Intestinal Microbiome: Oral Preparation vs. Enema | NCT04013841 BowelPrepMicrobiome | USA 2020–2022 |
Left-sided CRC | 60 | Int rand | Stool samples before and after bowel preparation and surgery | To investigate differences in microbiome composition according to oral and enema bowel preparation for left side colon surgery and its correlation with surgical outcomes |
| The Role of Microbiome in Cancer Therapy | NCT02960282 | USA 2016–2021 |
IV | 80 | Obs | Fecal specimen collection at baseline, prior to each cycle and at PD or off-treatment | To investigate microbiome composition, its gene and protein expression profile and correlation with RR and TT in two cohorts: Cohort A: patients treated with FOLFOX or FOLFIRI CT backbone as first line regimen, Cohort B: patients treated with pembrolizumab |
| Colorectal Cancer Cohort Study | NCT04185779 COLO-COHORT | UK 2019–2024 |
diagnostic | 15000 | Obs | Blood and fecal tests + behavioral questionnaires | To develop a prediction model to stratify patients at risk of having adenomas or CRC (past medical history, family history, blood tests, FIT level, colonscopy, and microbiome stool) |
| Stool and Blood Sample Bank for CRC Patients | NCT04638751 ARGONAUT | USA 2020–2024 |
III–IV | 4000 | 2 blood and stool samples each over a 6-month period | To determine whether the microbiome composition can predict PFS and OS in different cohorts of cancer patients (NSCLC, CRC, TNBC, and PC) treated with CT or IT. To identify correlations between microbiome composition and immune markers | |
| Omega-3 Fatty Acid for the Immune Modulation of Colorectal Cancer | NCT03661047 OMICC | USA 2019–2023 |
I-III, HR adenomas |
36 | Int rand/2/ | Blood and stool samples + lifestyle questionnaire + nutritional survey between CRC/adenomas detection and surgery | To evaluate the effect of a 30-day administration of AMR101 (VASCEPA, icosapent ethyl) on MO3PUFA composition, gut microbiome, and immune system elements concentration (CD8+ T cells, CD49b, CTLA-4, PD-L1, PD-1, LAG-3, IL10, FOXP3) in both normal and tumor tissue |
| Metagenomic Evaluation of the Gut Microbiome in Patients With Lynch Syndrome and Other Hereditary Colonic Polyposis Syndromes | NCT02371135 | USA 2015–2021 |
High hereditary CRC risk | 225 | Obs | Stool sample + Brief Diet and Lifestyle Questionnaire before every colonscopy | To investigate the association of the gut microbiome and dietary factors with risk of adenoma or cancer in Lynch syndrome and other hereditary colonic polyposis syndrome patients |
| Pilot Trial of Resistant Starch in Stage I-III CRC Survivors | NCT03781778 | USA 2018–2020 |
I–III | 24 | Int rand/2 | Stool samples + Diet questionnaire at beginning and at 8 weeks | To compare the effect of a 8-week consumption of foods made of resistant (experimental arm) or corn (control arm) starch in addition to usual daily diet in modifying markers of inflammation, insulin resistance, and gut microbiome composition of CRC patients |
| Development and Analysis of a Stool Bank for Cancer Patients | NCT04291755 | USA 2019–2021 |
all | 100 | Obs | Five stool, blood, and urine samples each over a 12-month period | To investigate the impact of gut microbiota on the efficacy of immune checkpoint inhibitors in NSCLC and CRC patients |
| Microbiome and Rectal Cancer | NCT04223102 | USA 2020–2027 |
II–III | 40 | Int | Serial rectal biopsy specimens in a 5-year follow-up | To investigate the association between microbiome and pathologic response to neoadjuvant therapy in rectal cancer |
| Fecal Microbiota Transplant (FMT) Capsule for Improving the Efficacy of Anti- PD-1 | NCT04130763 | China 2020–2021 |
IV | 10 | Int | Induction dose with FMT capsules one week before anti-PD-1 treatment beginning followed by maintenance dose | To determine whether the FMT capsule improves ORR of anti-PD-1 treatment in resistant/refractory gastrointestinal cancer patients |
Obs: observational; RR: response rate; TT: treatment toxicity/treatment-related adverse events; SOC: standard of care; T: clinical trial; LM: luminal microbiota; MAM: mucosal associated microbiota; CT: chemotherapy; IT: immunotherapy; NSCLC: non-small cell lung cancer; TNBC: triple negative breast cancer; PC: pancreatic cancer; HR: high-risk; MO3UFA: marine omega-3 polyunsaturated fatty acid; FMT: fecal microbiota transplant.
Abbreviations
| 5-FU | 5-Fluorouracil |
| ACT | Adjuvant Chemotherapy |
| Akt | Protein Kinase B |
| APC | Adenomatous Polyposis Coli |
| APCMin | Multiple Intestinal Neoplasia, a mutant allele of the Murine Adenomatous Polyposis Coli Locus |
| ATM | Ataxia Telangiectasia Mutated Serine/Threonine Kinase |
| AUC | Area Under the Curve |
| BIRC3 | Baculoviral IAP Repeat Containing 3 |
| BMP | Bone Morphogenetic Protein |
| CA19-9 | Carbohydrate Antigen 19-9 |
| cAMP | 3′-5′-Cyclic Adenosine Monophosphate |
| CDI | Clostridium Difficile Infection |
| CEA | Carcino Embryonic Antigen |
| CEA | Carcinoembryonic Antigen |
| cf-DNA | Cell-Free DNA |
| CIMP | CpG Island Methylator Phenotype |
| CPSF4 | Cleavage And Polyadenylation Specific Factor 4 |
| CRC | Colorectal Cancer |
| CSC | Cancer Stem Cells |
| CT | Computed Tomography |
| CT | Chemotherapy |
| CTCs | Circulating Tumor Cells |
| ctDNA | Circulating Tumor DNA |
| ctDNA clear | ctDNA clearance or modification rate of every study arm and correlation with clinical outcome measures (according to the design of each study) |
| ctRNAs | Circulating Tumor RNAs |
| Cxcl2 | C-X-C Motif Chemokine Ligand 2 |
| DCE | Dynamic Contrast-Enhanced |
| ddPCR | Digital Droplet PCR |
| DDR | DNA Damage Response |
| DFS | Disease-free Survival |
| dPCR | Digital PCR |
| DR | Distant Recurrence |
| EGFR | Epidermal Growth Factor Receptor |
| EMT | Epithelial–Mesenchymal Transition |
| Enco/Bini/Cet | Encorafenib/Binimetinib/Cetuximab |
| Endp | Study Endpoints if not Reported in Study Description |
| ETBF | Enterotoxigenic Bacteroides Fragilis |
| EVs | Extracellular Vesicles |
| FMT | Fecal Microbiota Transplantation |
| Fn | Fusobacterium Nucleatum |
| FOBT | Fecal Occult Blood Test |
| FOXO | Forkhead Box O3 |
| GC | Gastric Cancer |
| GI | Gastrointestinal |
| Gli1 | Glioma-Associated Oncogene Homolog 1 |
| GLOBOCAN | Global Cancer Statistics |
| GMMs | Metabolites of the Intestinal Microbiome |
| HIF-1 | Hypoxia-Inducible Factor 1 |
| HR | Hazard Ratio |
| HR | High-Risk According to Histopathological Factors |
| HR | High-Risk |
| IAPs | Inhibitor of Apoptosis Proteins |
| ICIs | Immune Checkpoint Inhibitors |
| IECs | Ileal Intestinal Epithelial Cells |
| IL-17 | Interleukin-17 |
| Int | Interventional |
| IT | Immunotherapy |
| LB | Liquid Biopsy |
| LM | Luminal Microbiota |
| lncRNAs | Long non-coding RNAs |
| LR | Low-Risk According to Histopatological Factors |
| LR | Local Recurrence |
| MAM | Mucosal Associated Microbiota |
| mCRC | Metastatic CRC |
| MDM2 | Mouse Double Minute 2 |
| MEK | Mitogen-Activated Protein Kinase |
| MIR | MicroRNA |
| miRNAs | MicroRNAs |
| MO3UFA | Marine Omega-3 Polyunsaturated Fatty Acid |
| mRCC | Metastatic Renal Cell Carcinoma |
| MRD | Minimal Residual Disease |
| MRI | Magnetic Resonance Imaging |
| mSEPT9 | methylated Septin 9 |
| MSI | Micro-Satellite Instability |
| mTOR | Mammalian Target of Rapamycin |
| MYD88 | Myeloid Differentiation Primary Response 88 |
| N | Planned Enrollment |
| NA | Not Available |
| ncRNAs | non-coding RNAs |
| NEAT1 | Nuclear Enriched Abundant Transcript 1 |
| NFkB | Nuclear Factor Kappa-Light-Chain-Enhancer of Activated B Cells |
| NSCLC | Non-Small Cell Lung Cancer |
| NTBF | Non-Enterotoxigenic Bacteroides Fragilis |
| Obs | Observational |
| OMVs | Outer Membrane Vesicles |
| OS | Overall Survival |
| PACs | Proanthocyanidins |
| PC | Pancreatic Cancer |
| pCR | Pathologic Complete Response |
| PD-1 | Programmed Death-1 |
| PFS | Progression-Free Survival |
| PI3K | Phosphatidylinositol 3-Kinase |
| PLGC | Precancerous lesions of gastric carcinoma |
| PTEN | Phosphatase and Tensin Homolog |
| PUFAs | Omega-3 Polyunsatured Fatty Acids |
| PVAs | Hydroxy-Phenylvaleric Acids |
| PVLs | Hydroxy-Phenyl-γ-Valerolactones |
| QoL | Quality of Life |
| RECIST | Response Evaluation Criteria in Solid Tumors |
| RFS | Relapse-Free Survival |
| ROC | Receiver Operating Characteristic Curve |
| ROS | Reactive Oxygen Species |
| RR | Response Rate |
| SCFA | Short-Chain Fatty Acid |
| SMAD4 | Mothers Against Decapentaplegic Homolog 4 |
| SOC | Standard of Care |
| T | Clinical Trial |
| TDEs | Tumor-Derived Exosomes |
| TFH | Follicular T-helper Cell |
| TGF-β | Transforming Growth Factor Beta |
| TLR4 | Toll-like Receptor 4 |
| TNBC | Triple Negative Breast Cancer |
| TNF-α | Tumor Necrosis Factor- alpha |
| TNM | Classification of Malignant Tumors (Tumor-Nodes-Metastasis) |
| TNMB | Tumor-Nodes-Metastasis-Blood |
| TT | Treatment Toxicity/Treatment-Related Adverse Events |
| TTF | Time to Treatment Failure |
| TTR | Time to Recurrence |
| VEGF | Vascular Endothelial Growth Factor |
Author Contributions
A.P. and S.D.M. conceptualized and organized the manuscript; A.P., S.D.M., F.P. have been involved in collection of bibliographic materials and writing—original draft preparation; A.P., S.D.M., F.P, V.M., K.C., G.P. have been involved in writing—review and editing, A.P., S.D.M., G.P and C.F. provided supervision and proofread the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by ALCLI “Giorgio e Silvia” ONLUS, a non-profit association.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ferlay J., Colombet M., Soerjomataram I., Mathers C., Parkin D.M., Pineros M., Znaor A., Bray F. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int. J. Cancer. 2019;144:1941–1953. doi: 10.1002/ijc.31937. [DOI] [PubMed] [Google Scholar]
- 2.Ludwig J.A., Weinstein J.N. Biomarkers in cancer staging, prognosis and treatment selection. Nat. Rev. Cancer. 2005;5:845–856. doi: 10.1038/nrc1739. [DOI] [PubMed] [Google Scholar]
- 3.van Zijl F., Krupitza G., Mikulits W. Initial steps of metastasis: Cell invasion and endothelial transmigration. Mutat. Res. 2011;728:23–34. doi: 10.1016/j.mrrev.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Corcoran R.B., Chabner B.A. Application of Cell-free DNA Analysis to Cancer Treatment. N. Engl. J. Med. 2018;379:1754–1765. doi: 10.1056/NEJMra1706174. [DOI] [PubMed] [Google Scholar]
- 5.Backhed F., Ley R.E., Sonnenburg J.L., Peterson D.A., Gordon J.I. Host-bacterial mutualism in the human intestine. Science. 2005;307:1915–1920. doi: 10.1126/science.1104816. [DOI] [PubMed] [Google Scholar]
- 6.Gomez A., Espinoza J.L., Harkins D.M., Leong P., Saffery R., Bockmann M., Torralba M., Kuelbs C., Kodukula R., Inman J., et al. Host Genetic Control of the Oral Microbiome in Health and Disease. Cell Host Microbe. 2017;22:269–278.e263. doi: 10.1016/j.chom.2017.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.David L.A., Materna A.C., Friedman J., Campos-Baptista M.I., Blackburn M.C., Perrotta A., Erdman S.E., Alm E.J. Host lifestyle affects human microbiota on daily timescales. Genome Biol. 2014;15:R89. doi: 10.1186/gb-2014-15-7-r89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Graf D., Di Cagno R., Fak F., Flint H.J., Nyman M., Saarela M., Watzl B. Contribution of diet to the composition of the human gut microbiota. Microb. Ecol. Health Dis. 2015;26:26164. doi: 10.3402/mehd.v26.26164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wong S.H., Yu J. Gut microbiota in colorectal cancer: Mechanisms of action and clinical applications. Nat. Rev. Gastroenterol. Hepatol. 2019;16:690–704. doi: 10.1038/s41575-019-0209-8. [DOI] [PubMed] [Google Scholar]
- 10.Crowley E., Di Nicolantonio F., Loupakis F., Bardelli A. Liquid biopsy: Monitoring cancer-genetics in the blood. Nat. Rev. Clin. Oncol. 2013;10:472–484. doi: 10.1038/nrclinonc.2013.110. [DOI] [PubMed] [Google Scholar]
- 11.Lampis A., Hahne J.C., Hedayat S., Valeri N. MicroRNAs as mediators of drug resistance mechanisms. Curr. Opin. Pharmacol. 2020;54:44–50. doi: 10.1016/j.coph.2020.08.004. [DOI] [PubMed] [Google Scholar]
- 12.Osumi H., Shinozaki E., Yamaguchi K., Zembutsu H. Clinical utility of circulating tumor DNA for colorectal cancer. Cancer Science. 2019;110:1148–1155. doi: 10.1111/cas.13972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kilgour E., Rothwell D.G., Brady G., Dive C. Liquid Biopsy-Based Biomarkers of Treatment Response and Resistance. Cancer Cell. 2020;37:485–495. doi: 10.1016/j.ccell.2020.03.012. [DOI] [PubMed] [Google Scholar]
- 14.Masuda T., Hayashi N., Iguchi T., Ito S., Eguchi H., Mimori K. Clinical and biological significance of circulating tumor cells in cancer. Mol. Oncol. 2016;10:408–417. doi: 10.1016/j.molonc.2016.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Romiti A., Raffa S., Di Rocco R., Roberto M., Milano A., Zullo A., Leone L., Ranieri D., Mazzetta F., Medda E., et al. Circulating tumor cells count predicts survival in colorectal cancer patients. J. Gastrointest. Liver Dis. JGLD. 2014;23:279–284. doi: 10.15403/jgld.2014.1121.233.arom1. [DOI] [PubMed] [Google Scholar]
- 16.Marcuello M., Vymetalkova V., Neves R.P.L., Duran-Sanchon S., Vedeld H.M., Tham E., van Dalum G., Flugen G., Garcia-Barberan V., Fijneman R.J., et al. Circulating biomarkers for early detection and clinical management of colorectal cancer. Mol. As. Med. 2019;69:107–122. doi: 10.1016/j.mam.2019.06.002. [DOI] [PubMed] [Google Scholar]
- 17.Tsai W.S., You J.F., Hung H.Y., Hsieh P.S., Hsieh B., Lenz H.J., Idos G., Friedland S., Yi-Jiun Pan J., Shao H.J., et al. Novel Circulating Tumor Cell Assay for Detection of Colorectal Adenomas and Cancer. Clin. Transl. Gastroenterol. 2019;10:e00088. doi: 10.14309/ctg.0000000000000088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tan Y., Wu H. The significant prognostic value of circulating tumor cells in colorectal cancer: A systematic review and meta-analysis. Curr. Probl. Cancer. 2018;42:95–106. doi: 10.1016/j.currproblcancer.2017.11.002. [DOI] [PubMed] [Google Scholar]
- 19.Tsai W.S., Chen J.S., Shao H.J., Wu J.C., Lai J.M., Lu S.H., Hung T.F., Chiu Y.C., You J.F., Hsieh P.S., et al. Circulating Tumor Cell Count Correlates with Colorectal Neoplasm Progression and Is a Prognostic Marker for Distant Metastasis in Non-Metastatic Patients. Sci. Rep. 2016;6:24517. doi: 10.1038/srep24517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cremolini C., Schirripa M., Antoniotti C., Moretto R., Salvatore L., Masi G., Falcone A., Loupakis F. First-line chemotherapy for mCRC-a review and evidence-based algorithm. Nat. Rev. Clin. Oncol. 2015;12:607–619. doi: 10.1038/nrclinonc.2015.129. [DOI] [PubMed] [Google Scholar]
- 21.Cortellini A., Cannita K., Parisi A., Lanfiuti Baldi P., Venditti O., D’Orazio C., Dal Mas A., Calvisi G., Giordano A.V., Vicentini V., et al. Weekly alternate intensive regimen FIrB/FOx in metastatic colorectal cancer patients: An update from clinical practice. OncoTargets Ther. 2019;12:2159–2170. doi: 10.2147/OTT.S194745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aranda E., Vieitez J.M., Gomez-Espana A., Gil Calle S., Salud-Salvia A., Grana B., Garcia-Alfonso P., Rivera F., Quintero-Aldana G.A., Reina-Zoilo J.J., et al. FOLFOXIRI plus bevacizumab versus FOLFOX plus bevacizumab for patients with metastatic colorectal cancer and >/=3 circulating tumour cells: The randomised phase III VISNU-1 trial. ESMO Open. 2020;5 doi: 10.1136/esmoopen-2020-000944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Van Cutsem E., Nordlinger B., Cervantes A., Group E.G.W. Advanced colorectal cancer: ESMO Clinical Practice Guidelines for treatment. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2010;21(Suppl. 5):v93–v97. doi: 10.1093/annonc/mdq222. [DOI] [PubMed] [Google Scholar]
- 24.Parisi A., Cortellini A., Cannita K., Venditti O., Camarda F., Calegari M.A., Salvatore L., Tortora G., Rossini D., Germani M.M., et al. Evaluation of Second-line Anti-VEGF after First-line Anti-EGFR Based Therapy in RAS Wild-Type Metastatic Colorectal Cancer: The Multicenter “SLAVE” Study. Cancers. 2020;12:1259. doi: 10.3390/cancers12051259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Musella V., Pietrantonio F., Di Buduo E., Iacovelli R., Martinetti A., Sottotetti E., Bossi I., Maggi C., Di Bartolomeo M., de Braud F., et al. Circulating tumor cells as a longitudinal biomarker in patients with advanced chemorefractory, RAS-BRAF wild-type colorectal cancer receiving cetuximab or panitumumab. Int. J. Cancer. 2015;137:1467–1474. doi: 10.1002/ijc.29493. [DOI] [PubMed] [Google Scholar]
- 26.Cristiano S., Leal A., Phallen J., Fiksel J., Adleff V., Bruhm D.C., Jensen S.O., Medina J.E., Hruban C., White J.R., et al. Genome-wide cell-free DNA fragmentation in patients with cancer. Nature. 2019;570:385–389. doi: 10.1038/s41586-019-1272-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Diehl F., Schmidt K., Choti M.A., Romans K., Goodman S., Li M., Thornton K., Agrawal N., Sokoll L., Szabo S.A., et al. Circulating mutant DNA to assess tumor dynamics. Nat. Med. 2008;14:985–990. doi: 10.1038/nm.1789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang X., Shi X.Q., Zeng P.W., Mo F.M., Chen Z.H. Circulating cell free DNA as the diagnostic marker for colorectal cancer: A systematic review and meta-analysis. Oncotarget. 2018;9:24514–24524. doi: 10.18632/oncotarget.25314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Masuda T., Wang X., Maeda M., Canver M.C., Sher F., Funnell A.P., Fisher C., Suciu M., Martyn G.E., Norton L.J., et al. Transcription factors LRF and BCL11A independently repress expression of fetal hemoglobin. Science. 2016;351:285–289. doi: 10.1126/science.aad3312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Flamini E., Mercatali L., Nanni O., Calistri D., Nunziatini R., Zoli W., Rosetti P., Gardini N., Lattuneddu A., Verdecchia G.M., et al. Free DNA and carcinoembryonic antigen serum levels: An important combination for diagnosis of colorectal cancer. Clin. Cancer Res. 2006;12:6985–6988. doi: 10.1158/1078-0432.CCR-06-1931. [DOI] [PubMed] [Google Scholar]
- 31.Nian J., Sun X., Ming S., Yan C., Ma Y., Feng Y., Yang L., Yu M., Zhang G., Wang X. Diagnostic Accuracy of Methylated SEPT9 for Blood-based Colorectal Cancer Detection: A Systematic Review and Meta-Analysis. Clin. Transl. Gastroenterol. 2017;8:e216. doi: 10.1038/ctg.2016.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Luo H., Zhao Q., Wei W., Zheng L., Yi S., Li G., Wang W., Sheng H., Pu H., Mo H., et al. Circulating tumor DNA methylation profiles enable early diagnosis, prognosis prediction, and screening for colorectal cancer. Sci. Translat. Med. 2020;12:eaax7533m. doi: 10.1126/scitranslmed.aax7533. [DOI] [PubMed] [Google Scholar]
- 33.Spindler K.G., Boysen A.K., Pallisgard N., Johansen J.S., Tabernero J., Sorensen M.M., Jensen B.V., Hansen T.F., Sefrioui D., Andersen R.F., et al. Cell-Free DNA in Metastatic Colorectal Cancer: A Systematic Review and Meta-Analysis. Oncologist. 2017;22:1049–1055. doi: 10.1634/theoncologist.2016-0178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Perdyan A., Spychalski P., Kacperczyk J., Rostkowska O., Kobiela J. Circulating Tumor DNA in KRAS positive colorectal cancer patients as a prognostic factor—A systematic review and meta-analysis. Crit. Rev. Oncol. Hematol. 2020;154:103065. doi: 10.1016/j.critrevonc.2020.103065. [DOI] [PubMed] [Google Scholar]
- 35.Douillard J.Y., Oliner K.S., Siena S., Tabernero J., Burkes R., Barugel M., Humblet Y., Bodoky G., Cunningham D., Jassem J., et al. Panitumumab-FOLFOX4 treatment and RAS mutations in colorectal cancer. N. Engl. J. Med. 2013;369:1023–1034. doi: 10.1056/NEJMoa1305275. [DOI] [PubMed] [Google Scholar]
- 36.Di Nicolantonio F., Martini M., Molinari F., Sartore-Bianchi A., Arena S., Saletti P., De Dosso S., Mazzucchelli L., Frattini M., Siena S., et al. Wild-type BRAF is required for response to panitumumab or cetuximab in metastatic colorectal cancer. J. Clin. Oncol. 2008;26:5705–5712. doi: 10.1200/JCO.2008.18.0786. [DOI] [PubMed] [Google Scholar]
- 37.Siravegna G., Mussolin B., Buscarino M., Corti G., Cassingena A., Crisafulli G., Ponzetti A., Cremolini C., Amatu A., Lauricella C., et al. Clonal evolution and resistance to EGFR blockade in the blood of colorectal cancer patients. Nat. Med. 2015;21:827. doi: 10.1038/nm0715-827b. [DOI] [PubMed] [Google Scholar]
- 38.Khan K.H., Cunningham D., Werner B., Vlachogiannis G., Spiteri I., Heide T., Mateos J.F., Vatsiou A., Lampis A., Damavandi M.D., et al. Longitudinal Liquid Biopsy and Mathematical Modeling of Clonal Evolution Forecast Time to Treatment Failure in the PROSPECT-C Phase II Colorectal Cancer Clinical Trial. Cancer Dis. 2018;8:1270–1285. doi: 10.1158/2159-8290.CD-17-0891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Khan K., Rata M., Cunningham D., Koh D.M., Tunariu N., Hahne J.C., Vlachogiannis G., Hedayat S., Marchetti S., Lampis A., et al. Functional imaging and circulating biomarkers of response to regorafenib in treatment-refractory metastatic colorectal cancer patients in a prospective phase II study. Gut. 2018;67:1484–1492. doi: 10.1136/gutjnl-2017-314178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yang Y.C., Wang D., Jin L., Yao H.W., Zhang J.H., Wang J., Zhao X.M., Shen C.Y., Chen W., Wang X.L., et al. Circulating tumor DNA detectable in early- and late-stage colorectal cancer patients. Biosci. Rep. 2018;38 doi: 10.1042/BSR20180322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yang M., Forbes M.E., Bitting R.L., O’Neill S.S., Chou P.C., Topaloglu U., Miller L.D., Hawkins G.A., Grant S.C., DeYoung B.R., et al. Incorporating blood-based liquid biopsy information into cancer staging: Time for a TNMB system? Ann. Oncol. 2018;29:311–323. doi: 10.1093/annonc/mdx766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schrag D., Rifas-Shiman S., Saltz L., Bach P.B., Begg C.B. Adjuvant chemotherapy use for Medicare beneficiaries with stage II colon cancer. J. Clin. Oncol. 2002;20:3999–4005. doi: 10.1200/JCO.2002.11.084. [DOI] [PubMed] [Google Scholar]
- 43.Tie J., Wang Y., Tomasetti C., Li L., Springer S., Kinde I., Silliman N., Tacey M., Wong H.L., Christie M., et al. Circulating tumor DNA analysis detects minimal residual disease and predicts recurrence in patients with stage II colon cancer. Sci. Transl. Med. 2016;8:346ra392. doi: 10.1126/scitranslmed.aaf6219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Reinert T., Henriksen T.V., Christensen E., Sharma S., Salari R., Sethi H., Knudsen M., Nordentoft I., Wu H.T., Tin A.S., et al. Analysis of Plasma Cell-Free DNA by Ultradeep Sequencing in Patients With Stages I to III Colorectal Cancer. JAMA Oncol. 2019;5:1124–1131. doi: 10.1001/jamaoncol.2019.0528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wang Y., Li L., Cohen J.D., Kinde I., Ptak J., Popoli M., Schaefer J., Silliman N., Dobbyn L., Tie J., et al. Prognostic Potential of Circulating Tumor DNA Measurement in Postoperative Surveillance of Nonmetastatic Colorectal Cancer. JAMA Oncol. 2019;5:1118–1123. doi: 10.1001/jamaoncol.2019.0512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tang X.J., Wang W., Hann S.S. Interactions among lncRNAs, miRNAs and mRNA in colorectal cancer. Biochimie. 2019;163:58–72. doi: 10.1016/j.biochi.2019.05.010. [DOI] [PubMed] [Google Scholar]
- 47.Qi F.F., Yang Y., Zhang H., Chen H. Long non-coding RNAs: Key regulators in oxaliplatin resistance of colorectal cancer. Biomed. Pharmacother. 2020;128:110329. doi: 10.1016/j.biopha.2020.110329. [DOI] [PubMed] [Google Scholar]
- 48.Wei L., Wang X., Lv L., Liu J., Xing H., Song Y., Xie M., Lei T., Zhang N., Yang M. The emerging role of microRNAs and long noncoding RNAs in drug resistance of hepatocellular carcinoma. Mol. Cancer. 2019;18:147. doi: 10.1186/s12943-019-1086-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wang X., Jiang G., Ren W., Wang B., Yang C., Li M. LncRNA NEAT1 Regulates 5-Fu Sensitivity, Apoptosis and Invasion in Colorectal Cancer Through the MiR-150-5p/CPSF4 Axis. OncoTargets Ther. 2020;13:6373–6383. doi: 10.2147/OTT.S239432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Xian Z., Hu B., Wang T., Zeng J., Cai J., Zou Q., Zhu P. lncRNA UCA1 Contributes to 5-Fluorouracil Resistance of Colorectal Cancer Cells Through miR-23b-3p/ZNF281 Axis. OncoTargets Ther. 2020;13:7571–7583. doi: 10.2147/OTT.S258727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.He Z., Dang J., Song A., Cui X., Ma Z., Zhang Y. The involvement of miR-150/beta-catenin axis in colorectal cancer progression. Biomed. Pharmacother. 2020;121:109495. doi: 10.1016/j.biopha.2019.109495. [DOI] [PubMed] [Google Scholar]
- 52.Sur D., Burz C., Sabarimurugan S., Irimie A. Diagnostic and Prognostic Significance of MiR-150 in Colorectal Cancer: A Systematic Review and Meta-Analysis. J. Pers. Med. 2020;10:99. doi: 10.3390/jpm10030099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Peng Q., Yao W., Yu C., Zou L., Shen Y., Zhu Y., Cheng M., Feng Z., Xu B. Identification of microRNA-181 as a promising biomarker for predicting the poor survival in colorectal cancer. Cancer Med. 2019;8:5995–6009. doi: 10.1002/cam4.2520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Liu J., Ke F., Chen T., Zhou Q., Weng L., Tan J., Shen W., Li L., Zhou J., Xu C., et al. MicroRNAs that regulate PTEN as potential biomarkers in colorectal cancer: A systematic review. J. Cancer Res. Clin. Oncol. 2020;146:809–820. doi: 10.1007/s00432-020-03172-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sabarimurugan S., Madhav M.R., Kumarasamy C., Gupta A., Baxi S., Krishnan S., Jayaraj R. Prognostic Value of MicroRNAs in Stage II Colorectal Cancer Patients: A Systematic Review and Meta-Analysis. Mol. Diagn. Ther. 2020;24:15–30. doi: 10.1007/s40291-019-00440-y. [DOI] [PubMed] [Google Scholar]
- 56.Yamada A., Horimatsu T., Okugawa Y., Nishida N., Honjo H., Ida H., Kou T., Kusaka T., Sasaki Y., Yagi M., et al. Serum miR-21, miR-29a, and miR-125b Are Promising Biomarkers for the Early Detection of Colorectal Neoplasia. Clin. Cancer Res. 2015;21:4234–4242. doi: 10.1158/1078-0432.CCR-14-2793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hur K., Toiyama Y., Okugawa Y., Ide S., Imaoka H., Boland C.R., Goel A. Circulating microRNA-203 predicts prognosis and metastasis in human colorectal cancer. Gut. 2017;66:654–665. doi: 10.1136/gutjnl-2014-308737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Vychytilova-Faltejskova P., Radova L., Sachlova M., Kosarova Z., Slaba K., Fabian P., Grolich T., Prochazka V., Kala Z., Svoboda M., et al. Serum-based microRNA signatures in early diagnosis and prognosis prediction of colon cancer. Carcinogenesis. 2016;37:941–950. doi: 10.1093/carcin/bgw078. [DOI] [PubMed] [Google Scholar]
- 59.Oehme F., Krahl S., Gyorffy B., Muessle B., Rao V., Greif H., Ziegler N., Lin K., Thepkaysone M.L., Polster H., et al. Low level of exosomal long non-coding RNA HOTTIP is a prognostic biomarker in colorectal cancer. RNA Biol. 2019;16:1339–1345. doi: 10.1080/15476286.2019.1637697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kang W., Zheng Q., Lei J., Chen C., Yu C. Prognostic Value of Long Noncoding RNAs in Patients with Gastrointestinal Cancer: A Systematic Review and Meta-Analysis. Dis. Markers. 2018;2018:5340894. doi: 10.1155/2018/5340894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Madurantakam Royam M., Kumarasamy C., Baxi S., Gupta A., Ramesh N., Kodiveri Muthukaliannan G., Jayaraj R. Current Evidence on miRNAs as Potential Theranostic Markers for Detecting Chemoresistance in Colorectal Cancer: A Systematic Review and Meta-Analysis of Preclinical and Clinical Studies. Mol. Diagn. Ther. 2019;23:65–82. doi: 10.1007/s40291-019-00381-6. [DOI] [PubMed] [Google Scholar]
- 62.Brussow H. Problems with the concept of gut microbiota dysbiosis. Microb. Biotechnol. 2020;13:423–434. doi: 10.1111/1751-7915.13479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ursell L.K., Metcalf J.L., Parfrey L.W., Knight R. Defining the human microbiome. Nutr. Rev. 2012;70(Suppl. 1):S38–S44. doi: 10.1111/j.1753-4887.2012.00493.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Marchesi J.R., Ravel J. The vocabulary of microbiome research: A proposal. Microbiome. 2015;3:31. doi: 10.1186/s40168-015-0094-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Human Microbiome Project Consortium Structure, function and diversity of the healthy human microbiome. Nature. 2012;486:207–214. doi: 10.1038/nature11234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Qin J., Li R., Raes J., Arumugam M., Burgdorf K.S., Manichanh C., Nielsen T., Pons N., Levenez F., Yamada T., et al. A human gut microbial gene catalogue established by metagenomic sequencing. Nature. 2010;464:59–65. doi: 10.1038/nature08821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.O’Keefe S.J. Diet, microorganisms and their metabolites, and colon cancer. Nat. Rev. Gastroenterol. Hepatol. 2016;13:691–706. doi: 10.1038/nrgastro.2016.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tilg H., Adolph T.E., Gerner R.R., Moschen A.R. The Intestinal Microbiota in Colorectal Cancer. Cancer Cell. 2018;33:954–964. doi: 10.1016/j.ccell.2018.03.004. [DOI] [PubMed] [Google Scholar]
- 69.Garrett W.S. Cancer and the microbiota. Science. 2015;348:80–86. doi: 10.1126/science.aaa4972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gagniere J., Raisch J., Veziant J., Barnich N., Bonnet R., Buc E., Bringer M.A., Pezet D., Bonnet M. Gut microbiota imbalance and colorectal cancer. World J. Gastroenterol. 2016;22:501–518. doi: 10.3748/wjg.v22.i2.501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Sanchez-Alcoholado L., Ramos-Molina B., Otero A., Laborda-Illanes A., Ordonez R., Medina J.A., Gomez-Millan J., Queipo-Ortuno M.I. The Role of the Gut Microbiome in Colorectal Cancer Development and Therapy Response. Cancers. 2020;12:1406. doi: 10.3390/cancers12061406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bhatt A.P., Redinbo M.R., Bultman S.J. The role of the microbiome in cancer development and therapy. CA A Cancer J. Clin. 2017;67:326–344. doi: 10.3322/caac.21398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gagnaire A., Nadel B., Raoult D., Neefjes J., Gorvel J.P. Collateral damage: Insights into bacterial mechanisms that predispose host cells to cancer. Nat. Rev. Microbiol. 2017;15:109–128. doi: 10.1038/nrmicro.2016.171. [DOI] [PubMed] [Google Scholar]
- 74.Fahrer J., Huelsenbeck J., Jaurich H., Dorsam B., Frisan T., Eich M., Roos W.P., Kaina B., Fritz G. Cytolethal distending toxin (CDT) is a radiomimetic agent and induces persistent levels of DNA double-strand breaks in human fibroblasts. DNA Repair. 2014;18:31–43. doi: 10.1016/j.dnarep.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 75.Levy M., Kolodziejczyk A.A., Thaiss C.A., Elinav E. Dysbiosis and the immune system. Nat. Rev. Immunol. 2017;17:219–232. doi: 10.1038/nri.2017.7. [DOI] [PubMed] [Google Scholar]
- 76.Dalmasso G., Cougnoux A., Delmas J., Darfeuille-Michaud A., Bonnet R. The bacterial genotoxin colibactin promotes colon tumor growth by modifying the tumor microenvironment. Gut Microbes. 2014;5:675–680. doi: 10.4161/19490976.2014.969989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Pleguezuelos-Manzano C., Puschhof J., Rosendahl Huber A., van Hoeck A., Wood H.M., Nomburg J., Gurjao C., Manders F., Dalmasso G., Stege P.B., et al. Mutational signature in colorectal cancer caused by genotoxic pks(+) E. coli. Nature. 2020;580:269–273. doi: 10.1038/s41586-020-2080-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zamani S., Taslimi R., Sarabi A., Jasemi S., Sechi L.A., Feizabadi M.M. Enterotoxigenic Bacteroides fragilis: A Possible Etiological Candidate for Bacterially-Induced Colorectal Precancerous and Cancerous Lesions. Front. Cell. Infect. Microbiol. 2019;9:449. doi: 10.3389/fcimb.2019.00449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Brennan C.A., Garrett W.S. Fusobacterium nucleatum—Symbiont, opportunist and oncobacterium. Nat. Rev. Microbiol. 2019;17:156–166. doi: 10.1038/s41579-018-0129-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sun C.H., Li B.B., Wang B., Zhao J., Zhang X.Y., Li T.T., Li W.B., Tang D., Qiu M.J., Wang X.C., et al. The role of Fusobacterium nucleatum in colorectal cancer: From carcinogenesis to clinical management. Chronic Dis. Transl. Med. 2019;5:178–187. doi: 10.1016/j.cdtm.2019.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Koi M., Okita Y., Carethers J.M. Fusobacterium nucleatum Infection in Colorectal Cancer: Linking Inflammation, DNA Mismatch Repair and Genetic and Epigenetic Alterations. J. Anus Rectum Colon. 2018;2:37–46. doi: 10.23922/jarc.2017-055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Zitvogel L., Daillere R., Roberti M.P., Routy B., Kroemer G. Anticancer effects of the microbiome and its products. Nat. Rev. Microbiol. 2017;15:465–478. doi: 10.1038/nrmicro.2017.44. [DOI] [PubMed] [Google Scholar]
- 83.Feng Q., Liang S., Jia H., Stadlmayr A., Tang L., Lan Z., Zhang D., Xia H., Xu X., Jie Z., et al. Gut microbiome development along the colorectal adenoma-carcinoma sequence. Nat. Commun. 2015;6:6528. doi: 10.1038/ncomms7528. [DOI] [PubMed] [Google Scholar]
- 84.Lee A., Lee Y.J., Yoo H.J., Kim M., Chang Y., Lee D.S., Lee J.H. Consumption of Dairy Yogurt Containing Lactobacillus paracasei ssp. paracasei, Bifidobacterium animalis ssp. lactis and Heat-Treated Lactobacillus plantarum Improves Immune Function Including Natural Killer Cell Activity. Nutrients. 2017;9:558. doi: 10.3390/nu9060558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Long S., Yang Y., Shen C., Wang Y., Deng A., Qin Q., Qiao L. Metaproteomics characterizes human gut microbiome function in colorectal cancer. NPJ Biofilms Microbiomes. 2020;6:14. doi: 10.1038/s41522-020-0123-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Wang G., Yu Y., Wang Y.Z., Wang J.J., Guan R., Sun Y., Shi F., Gao J., Fu X.L. Role of SCFAs in gut microbiome and glycolysis for colorectal cancer therapy. J. Cell. Physiol. 2019;234:17023–17049. doi: 10.1002/jcp.28436. [DOI] [PubMed] [Google Scholar]
- 87.Borges-Canha M., Portela-Cidade J.P., Dinis-Ribeiro M., Leite-Moreira A.F., Pimentel-Nunes P. Role of colonic microbiota in colorectal carcinogenesis: A systematic review. Rev. Esp. de Enferm. Dig. 2015;107:659–671. doi: 10.17235/reed.2015.3830/2015. [DOI] [PubMed] [Google Scholar]
- 88.Grazioso T.P., Brandt M., Djouder N. Diet, Microbiota, and Colorectal Cancer. iScience. 2019;21:168–187. doi: 10.1016/j.isci.2019.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wan M.L., Wang Y., Zeng Z., Deng B., Zhu B.S., Cao T., Li Y.K., Xiao J., Han Q., Wu Q. Colorectal cancer (CRC) as a multifactorial disease and its causal correlations with multiple signaling pathways. Biosci. Rep. 2020;40 doi: 10.1042/BSR20200265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Duchartre Y., Kim Y.M., Kahn M. The Wnt signaling pathway in cancer. Crit. Rev. Oncol. Hematol. 2016;99:141–149. doi: 10.1016/j.critrevonc.2015.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Zhang L., Shay J.W. Multiple Roles of APC and its Therapeutic Implications in Colorectal Cancer. J. Natl. Cancer Inst. 2017;109 doi: 10.1093/jnci/djw332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wang B., Tian T., Kalland K.H., Ke X., Qu Y. Targeting Wnt/beta-Catenin Signaling for Cancer Immunotherapy. Trends Pharmacol. Sci. 2018;39:648–658. doi: 10.1016/j.tips.2018.03.008. [DOI] [PubMed] [Google Scholar]
- 93.Koni M., Pinnaro V., Brizzi M.F. The Wnt Signalling Pathway: A Tailored Target in Cancer. Int. J. Mol. Sci. 2020;21:7697. doi: 10.3390/ijms21207697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hofman P., Vouret-Craviari V. Microbes-induced EMT at the crossroad of inflammation and cancer. Gut Microbes. 2012;3:176–185. doi: 10.4161/gmic.20288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Vogelstein B., Fearon E.R., Hamilton S.R., Kern S.E., Preisinger A.C., Leppert M., Nakamura Y., White R., Smits A.M., Bos J.L. Genetic alterations during colorectal-tumor development. N. England J. Med. 1988;319:525–532. doi: 10.1056/NEJM198809013190901. [DOI] [PubMed] [Google Scholar]
- 96.Wu R., Wang L., Yin R., Hudlikar R., Li S., Kuo H.D., Peter R., Sargsyan D., Guo Y., Liu X., et al. Epigenetics/epigenomics and prevention by curcumin of early stages of inflammatory-driven colon cancer. Mol. Carcinog. 2020;59:227–236. doi: 10.1002/mc.23146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Yuan L., Zhang S., Li H., Yang F., Mushtaq N., Ullah S., Shi Y., An C., Xu J. The influence of gut microbiota dysbiosis to the efficacy of 5-Fluorouracil treatment on colorectal cancer. Biomed. Pharmacother. 2018;108:184–193. doi: 10.1016/j.biopha.2018.08.165. [DOI] [PubMed] [Google Scholar]
- 98.Zhang S., Yang Y., Weng W., Guo B., Cai G., Ma Y., Cai S. Fusobacterium nucleatum promotes chemoresistance to 5-fluorouracil by upregulation of BIRC3 expression in colorectal cancer. J. Exp. Clin. Cancer Res. CR. 2019;38:14. doi: 10.1186/s13046-018-0985-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Andre T., Shiu K.K., Kim T.W., Jensen B.V., Jensen L.H., Punt C., Smith D., Garcia-Carbonero R., Benavides M., Gibbs P., et al. Pembrolizumab in Microsatellite-Instability-High Advanced Colorectal Cancer. N. Engl. J. Med. 2020;383:2207–2218. doi: 10.1056/NEJMoa2017699. [DOI] [PubMed] [Google Scholar]
- 100.Lang M., Baumgartner M., Rozalska A., Frick A., Riva A., Jarek M., Berry D., Gasche C. Crypt residing bacteria and proximal colonic carcinogenesis in a mouse model of Lynch syndrome. Int. J. Cancer. 2020;147:2316–2326. doi: 10.1002/ijc.33028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Lalani A.A., Xie W., Braun D.A., Kaymakcalan M., Bosse D., Steinharter J.A., Martini D.J., Simantov R., Lin X., Wei X.X., et al. Effect of Antibiotic Use on Outcomes with Systemic Therapies in Metastatic Renal Cell Carcinoma. Eur. Urol. Oncol. 2020;3:372–381. doi: 10.1016/j.euo.2019.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ngara T.R., Zhang H. Recent Advances in Function-based Metagenomic Screening. Genom. Proteom. Bioinform. 2018;16:405–415. doi: 10.1016/j.gpb.2018.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Dai Z., Coker O.O., Nakatsu G., Wu W.K.K., Zhao L., Chen Z., Chan F.K.L., Kristiansen K., Sung J.J.Y., Wong S.H., et al. Multi-cohort analysis of colorectal cancer metagenome identified altered bacteria across populations and universal bacterial markers. Microbiome. 2018;6:70. doi: 10.1186/s40168-018-0451-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Dalal N., Jalandra R., Sharma M., Prakash H., Makharia G.K., Solanki P.R., Singh R., Kumar A. Omics technologies for improved diagnosis and treatment of colorectal cancer: Technical advancement and major perspectives. Biomed. Pharmacother. 2020;131:110648. doi: 10.1016/j.biopha.2020.110648. [DOI] [PubMed] [Google Scholar]
- 105.Behrouzi A., Nafari A.H., Siadat S.D. The significance of microbiome in personalized medicine. Clin. Transl. Med. 2019;8:16. doi: 10.1186/s40169-019-0232-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Yachida S., Mizutani S., Shiroma H., Shiba S., Nakajima T., Sakamoto T., Watanabe H., Masuda K., Nishimoto Y., Kubo M., et al. Metagenomic and metabolomic analyses reveal distinct stage-specific phenotypes of the gut microbiota in colorectal cancer. Nat. Med. 2019;25:968–976. doi: 10.1038/s41591-019-0458-7. [DOI] [PubMed] [Google Scholar]
- 107.Gao R., Kong C., Huang L., Li H., Qu X., Liu Z., Lan P., Wang J., Qin H. Mucosa-associated microbiota signature in colorectal cancer. Eur. J. Clin. Microbiol. Infect. Dis. 2017;36:2073–2083. doi: 10.1007/s10096-017-3026-4. [DOI] [PubMed] [Google Scholar]
- 108.Zeller G., Tap J., Voigt A.Y., Sunagawa S., Kultima J.R., Costea P.I., Amiot A., Bohm J., Brunetti F., Habermann N., et al. Potential of fecal microbiota for early-stage detection of colorectal cancer. Mol. Syst. Biol. 2014;10:766. doi: 10.15252/msb.20145645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kim D.J., Yang J., Seo H., Lee W.H., Ho Lee D., Kym S., Park Y.S., Kim J.G., Jang I.J., Kim Y.K., et al. Colorectal cancer diagnostic model utilizing metagenomic and metabolomic data of stool microbial extracellular vesicles. Sci. Rep. 2020;10:2860. doi: 10.1038/s41598-020-59529-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ahmadi Badi S., Moshiri A., Fateh A., Rahimi Jamnani F., Sarshar M., Vaziri F., Siadat S.D. Microbiota-Derived Extracellular Vesicles as New Systemic Regulators. Front. Microbiol. 2017;8:1610. doi: 10.3389/fmicb.2017.01610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Tjalsma H., Boleij A., Marchesi J.R., Dutilh B.E. A bacterial driver-passenger model for colorectal cancer: Beyond the usual suspects. Nat. Rev. Microbiol. 2012;10:575–582. doi: 10.1038/nrmicro2819. [DOI] [PubMed] [Google Scholar]
- 112.Oke S., Martin A. Insights into the role of the intestinal microbiota in colon cancer. Ther. Adv. Gastroenterol. 2017;10:417–428. doi: 10.1177/1756283X17694832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Farin H.F., Karthaus W.R., Kujala P., Rakhshandehroo M., Schwank G., Vries R.G., Kalkhoven E., Nieuwenhuis E.E., Clevers H. Paneth cell extrusion and release of antimicrobial products is directly controlled by immune cell-derived IFN-gamma. J. Exp. Med. 2014;211:1393–1405. doi: 10.1084/jem.20130753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Sato T., Stange D.E., Ferrante M., Vries R.G., Van Es J.H., Van den Brink S., Van Houdt W.J., Pronk A., Van Gorp J., Siersema P.D., et al. Long-term expansion of epithelial organoids from human colon, adenoma, adenocarcinoma, and Barrett’s epithelium. Gastroenterology. 2011;141:1762–1772. doi: 10.1053/j.gastro.2011.07.050. [DOI] [PubMed] [Google Scholar]
- 115.Rubert J., Schweiger P.J., Mattivi F., Tuohy K., Jensen K.B., Lunardi A. Intestinal Organoids: A Tool for Modelling Diet-Microbiome-Host Interactions. Trends Endocrinol. Metab. TEM. 2020;31:848–858. doi: 10.1016/j.tem.2020.02.004. [DOI] [PubMed] [Google Scholar]
- 116.Toden S., Ravindranathan P., Gu J., Cardenas J., Yuchang M., Goel A. Oligomeric proanthocyanidins (OPCs) target cancer stem-like cells and suppress tumor organoid formation in colorectal cancer. Sci. Rep. 2018;8:3335. doi: 10.1038/s41598-018-21478-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Ozdal T., Sela D.A., Xiao J., Boyacioglu D., Chen F., Capanoglu E. The Reciprocal Interactions between Polyphenols and Gut Microbiota and Effects on Bioaccessibility. Nutrients. 2016;8:78. doi: 10.3390/nu8020078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Zhang L.S., Davies S.S. Microbial metabolism of dietary components to bioactive metabolites: Opportunities for new therapeutic interventions. Genome Med. 2016;8:46. doi: 10.1186/s13073-016-0296-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Trost K., Ulaszewska M.M., Stanstrup J., Albanese D., De Filippo C., Tuohy K.M., Natella F., Scaccini C., Mattivi F. Host: Microbiome co-metabolic processing of dietary polyphenols—An acute, single blinded, cross-over study with different doses of apple polyphenols in healthy subjects. Food Res. Int. 2018;112:108–128. doi: 10.1016/j.foodres.2018.06.016. [DOI] [PubMed] [Google Scholar]
- 120.Mena P., Bresciani L., Brindani N., Ludwig I.A., Pereira-Caro G., Angelino D., Llorach R., Calani L., Brighenti F., Clifford M.N., et al. Phenyl-gamma-valerolactones and phenylvaleric acids, the main colonic metabolites of flavan-3-ols: Synthesis, analysis, bioavailability, and bioactivity. Nat. Prod. Rep. 2019;36:714–752. doi: 10.1039/C8NP00062J. [DOI] [PubMed] [Google Scholar]
- 121.Mehta R.S., Nishihara R., Cao Y., Song M., Mima K., Qian Z.R., Nowak J.A., Kosumi K., Hamada T., Masugi Y., et al. Association of Dietary Patterns With Risk of Colorectal Cancer Subtypes Classified by Fusobacterium nucleatum in Tumor Tissue. JAMA Oncol. 2017;3:921–927. doi: 10.1001/jamaoncol.2016.6374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Nencioni A., Caffa I., Cortellino S., Longo V.D. Fasting and cancer: Molecular mechanisms and clinical application. Nat. Rev. Cancer. 2018;18:707–719. doi: 10.1038/s41568-018-0061-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Li G., Xie C., Lu S., Nichols R.G., Tian Y., Li L., Patel D., Ma Y., Brocker C.N., Yan T., et al. Intermittent Fasting Promotes White Adipose Browning and Decreases Obesity by Shaping the Gut Microbiota. Cell Metabo. 2017;26:672–685.e674. doi: 10.1016/j.cmet.2017.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Nakamura K., Tonouchi H., Sasayama A., Ashida K. A Ketogenic Formula Prevents Tumor Progression and Cancer Cachexia by Attenuating Systemic Inflammation in Colon 26 Tumor-Bearing Mice. Nutrients. 2018;10:206. doi: 10.3390/nu10020206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Robertson R.C., Seira Oriach C., Murphy K., Moloney G.M., Cryan J.F., Dinan T.G., Paul Ross R., Stanton C. Omega-3 polyunsaturated fatty acids critically regulate behaviour and gut microbiota development in adolescence and adulthood. Brain Behav. Immun. 2017;59:21–37. doi: 10.1016/j.bbi.2016.07.145. [DOI] [PubMed] [Google Scholar]
- 126.Watson H., Mitra S., Croden F.C., Taylor M., Wood H.M., Perry S.L., Spencer J.A., Quirke P., Toogood G.J., Lawton C.L., et al. A randomised trial of the effect of omega-3 polyunsaturated fatty acid supplements on the human intestinal microbiota. Gut. 2018;67:1974–1983. doi: 10.1136/gutjnl-2017-314968. [DOI] [PubMed] [Google Scholar]
- 127.Bullman S., Pedamallu C.S., Sicinska E., Clancy T.E., Zhang X., Cai D., Neuberg D., Huang K., Guevara F., Nelson T., et al. Analysis of Fusobacterium persistence and antibiotic response in colorectal cancer. Science. 2017;358:1443–1448. doi: 10.1126/science.aal5240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Routy B., Le Chatelier E., Derosa L., Duong C.P.M., Alou M.T., Daillere R., Fluckiger A., Messaoudene M., Rauber C., Roberti M.P., et al. Gut microbiome influences efficacy of PD-1-based immunotherapy against epithelial tumors. Science. 2018;359:91–97. doi: 10.1126/science.aan3706. [DOI] [PubMed] [Google Scholar]
- 129.Buti S., Bersanelli M., Perrone F., Tiseo M., Tucci M., Adamo V., Stucci L.S., Russo A., Tanda E.T., Spagnolo F., et al. Effect of concomitant medications with immune-modulatory properties on the outcomes of patients with advanced cancer treated with immune checkpoint inhibitors: Development and validation of a novel prognostic index. Eur. J. Cancer. 2021;142:18–28. doi: 10.1016/j.ejca.2020.09.033. [DOI] [PubMed] [Google Scholar]
- 130.Sanchez B., Delgado S., Blanco-Miguez A., Lourenco A., Gueimonde M., Margolles A. Probiotics, gut microbiota, and their influence on host health and disease. Mol. Nutr. Food Res. 2017;61:1600240. doi: 10.1002/mnfr.201600240. [DOI] [PubMed] [Google Scholar]
- 131.Chen D., Wu J., Jin D., Wang B., Cao H. Fecal microbiota transplantation in cancer management: Current status and perspectives. Int. J. Cancer. 2019;145:2021–2031. doi: 10.1002/ijc.32003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Wang Y., Wiesnoski D.H., Helmink B.A., Gopalakrishnan V., Choi K., DuPont H.L., Jiang Z.D., Abu-Sbeih H., Sanchez C.A., Chang C.C., et al. Fecal microbiota transplantation for refractory immune checkpoint inhibitor-associated colitis. Nat. Med. 2018;24:1804–1808. doi: 10.1038/s41591-018-0238-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Chang C.W., Lee H.C., Li L.H., Chiang Chiau J.S., Wang T.E., Chuang W.H., Chen M.J., Wang H.Y., Shih S.C., Liu C.Y., et al. Fecal Microbiota Transplantation Prevents Intestinal Injury, Upregulation of Toll-Like Receptors, and 5-Fluorouracil/Oxaliplatin-Induced Toxicity in Colorectal Cancer. Int. J. Mol. Sci. 2020;21:386. doi: 10.3390/ijms21020386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Le Bastard Q., Ward T., Sidiropoulos D., Hillmann B.M., Chun C.L., Sadowsky M.J., Knights D., Montassier E. Fecal microbiota transplantation reverses antibiotic and chemotherapy-induced gut dysbiosis in mice. Sci. Rep. 2018;8:6219. doi: 10.1038/s41598-018-24342-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Hefazi M., Patnaik M.M., Hogan W.J., Litzow M.R., Pardi D.S., Khanna S. Safety and Efficacy of Fecal Microbiota Transplant for Recurrent Clostridium difficile Infection in Patients With Cancer Treated With Cytotoxic Chemotherapy: A Single-Institution Retrospective Case Series. Mayo Clin. Proc. 2017;92:1617–1624. doi: 10.1016/j.mayocp.2017.08.016. [DOI] [PubMed] [Google Scholar]
- 136.Kopetz S., Grothey A., Yaeger R., Van Cutsem E., Desai J., Yoshino T., Wasan H., Ciardiello F., Loupakis F., Hong Y.S., et al. Encorafenib, Binimetinib, and Cetuximab in BRAF V600E-Mutated Colorectal Cancer. N. Engl. J. Med. 2019;381:1632–1643. doi: 10.1056/NEJMoa1908075. [DOI] [PubMed] [Google Scholar]
- 137.Kolencik D., Shishido S.N., Pitule P., Mason J., Hicks J., Kuhn P. Liquid Biopsy in Colorectal Carcinoma: Clinical Applications and Challenges. Cancers. 2020;12:1376. doi: 10.3390/cancers12061376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Castro-Giner F., Gkountela S., Donato C., Alborelli I., Quagliata L., Ng C.K.Y., Piscuoglio S., Aceto N. Cancer Diagnosis Using a Liquid Biopsy: Challenges and Expectations. Diagnostics. 2018;8:31. doi: 10.3390/diagnostics8020031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Blaser M.J. Antibiotic use and its consequences for the normal microbiome. Science. 2016;352:544–545. doi: 10.1126/science.aad9358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Nagrath S., Sequist L.V., Maheswaran S., Bell D.W., Irimia D., Ulkus L., Smith M.R., Kwak E.L., Digumarthy S., Muzikansky A., et al. Isolation of rare circulating tumour cells in cancer patients by microchip technology. Nature. 2007;450:1235–1239. doi: 10.1038/nature06385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Mishra A., Dubash T.D., Edd J.F., Jewett M.K., Garre S.G., Karabacak N.M., Rabe D.C., Mutlu B.R., Walsh J.R., Kapur R., et al. Ultrahigh-throughput magnetic sorting of large blood volumes for epitope-agnostic isolation of circulating tumor cells. Proc. Natl. Acad. Sci. USA. 2020;117:16839–16847. doi: 10.1073/pnas.2006388117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Kalinich M., Bhan I., Kwan T.T., Miyamoto D.T., Javaid S., LiCausi J.A., Milner J.D., Hong X., Goyal L., Sil S., et al. An RNA-based signature enables high specificity detection of circulating tumor cells in hepatocellular carcinoma. Proc. Natl. Acad. Sci. USA. 2017;114:1123–1128. doi: 10.1073/pnas.1617032114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Yu M., Bardia A., Aceto N., Bersani F., Madden M.W., Donaldson M.C., Desai R., Zhu H., Comaills V., Zheng Z., et al. Cancer therapy. Ex vivo culture of circulating breast tumor cells for individualized testing of drug susceptibility. Science. 2014;345:216–220. doi: 10.1126/science.1253533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Fachin F., Spuhler P., Martel-Foley J.M., Edd J.F., Barber T.A., Walsh J., Karabacak M., Pai V., Yu M., Smith K., et al. Monolithic Chip for High-throughput Blood Cell Depletion to Sort Rare Circulating Tumor Cells. Sci. Rep. 2017;7:10936. doi: 10.1038/s41598-017-11119-x. [DOI] [PMC free article] [PubMed] [Google Scholar]