Abstract
Purpose
Vertebral body tethering (VBT) is an alternative to fusion for selected scoliosis patients. As VBT does not limit spine mobility, it has been propagated that this technique allows a quicker return to physical activity than fusion. However, no data are available to support this statement. Aim of this study was to quantify how much time patients required to resume preoperative activity level and to seek possible associations between return to physical activity and demographic, radiographic and surgical data.
Methods
One year postoperatively, the validated sport activity questionnaire (SAQ) was administered to all skeletally immature patients who underwent VBT at our institution. SAQ data were analyzed and a multivariate analysis was conducted to investigate associations between SAQ and demographic, radiographic and surgical data.
Results
Thirty-one patients aged 14.5 years completed the SAQ. Within 3 months from VBT, 97% returned to school, 61% resumed physical education, 97% carried a backpack, 68% run, and 82% rode a bike; 70% bent within a month from VBT. Ninety-four percent of patients returned to their preoperative athletic level. Within 3 months, 63% of responders resumed noncontact, 61% contact and 53% collision sports. No relevant associations were observed between the SAQ and demographic, radiographic and surgical data. In particular, number of instrumented vertebrae, level of the lowest instrumented vertebra and postoperative Cobb angle did not influence patients’ return to preoperative activities.
Conclusion
VBT allows patients to quickly return to their preoperative activity level, irrespectively of the postoperative Cobb angle or type of instrumentation.
Keywords: Vertebral body tethering, Fusionless anterior scoliosis correction, Sport activity questionnaire, Patient reported outcome measures, Sport, Physical activity, Adolescent idiopathic scoliosis
Introduction
The gold standard in the treatment of adolescent idiopathic scoliosis (AIS) is currently represented by spine fusion [1]. While this technique allows for predictable and stable results over time, it limits spine mobility and delays return to physical activity, especially after instrumentation of the lumbar spine [2]. Furthermore, many surgeons request postoperative mobility restriction (e.g., avoiding forward bending) and ask their patients to refrain from sport activities for some months after surgery [3–5].
Considering that many AIS patients undergo surgery while attending high school, long absence from educational and recreational activities may affect scholastic profit and sociality. Socioeconomic considerations also come into play, as parents need to take time off work to supply for the supervision otherwise provided by schools or athletic institutions. Vertebral body tethering (VBT) is being developed as alternative to fusion in patients with AIS, showing positive short- to midterm results [6–10]. VBT does not impair postoperative spine mobility [11], allowing a short recovery given its minimally invasive approach [11–13]. As loss of flexibility is the main self-reported reason for reduction in physical activity after fusion [2], VBT has been hypothesized to allow a quicker return to everyday activities compared to fusion. However, current literature does not offer data to support this statement.
The Scoliosis Research Society (SRS) questionnaire is commonly used to evaluate quality of life of the patients after spinal fusion for AIS [14]. However, this questionnaire lacks detailed information on the return to physical and athletic activity. Recently, Sarwahi and colleagues developed and validated the sport activity questionnaire (SAQ) [4]. This questionnaire is administered one year postoperatively to assess patients’ return to sport and activities of daily living after surgical treatment of AIS. In the questionnaire, different sport activities are classified as defined by the American Academy of Pediatrics [15], with limited contact considered as noncontact [4]. The SAQ has been routinely used at our institution for the follow-up of patients undergoing surgery for AIS. We retrospectively analyzed SAQ data one year after VBT, to assess the time required to resume the preoperative activity level after surgery. We also investigated possible associations between the SAQ items and patients demographic, radiographic and surgical parameters.
Materials and methods
Patient recruitment
The present retrospective study was conducted according to the Strengthening the Reporting of Observational Studies in Epidemiology: the STROBE Statement [16].
Data from of all consecutive patients were collected, who underwent single or bilateral VBT for AIS at our institution between January 2018 and October 2019, and for whom an in-office, 1-year follow-up was available. All patients were included in this study, who were skeletally immature (Risser ≤ 4 and/or Sanders ≤ 7) and who presented a scoliotic curve that could not be ascribed to a specific cause after careful clinic and radiographic investigations.
The study was approved by the ethics committee of the University of Aachen (EK 130/19): due to the retrospective nature of this work, a signed informed consent to participation to the study was not required by local law.
Surgical technique
One senior surgeon (PDT) performed all surgeries. Lumbar curves were addressed via a mini-retroperitoneal approach, while thoracic curves to L1 were instrumented with a video-assisted thoracic surgery (VATS). Correction of bilateral curves was performed in a single stage [17]. Choice of the kind of instrumentation (single- or double-curve) and of the upper and lower instrumented vertebrae (UIV and LIV, respectively) was based on a previously published algorithm [18]. Starting January 2019, all lumbar curves were instrumented with a 2-cord construct [19] to improve intraoperative correction and reduce the rate of cord rupture.
Immediately after surgery, mobilization was allowed without restrictions and without walking aids. During hospitalization, all patients received daily physiotherapy to improve posture and increase confidence when walking and climbing stairs. The surgeon placed no restrictions toward resuming activities of daily living or sports, so that each patient autonomously decided when to return to the activities performed prior to surgery.
Outcomes of interest and statistical analysis
Demographic data and data regarding the instrumentation (single or double instrumentation, upper instrumented vertebra—UIV, lowest instrumented vertebra—LIV), and curve correction were collected. The complication rate was also analyzed in terms of intra- and perioperative complications, mechanical complications (implant loosening, vertebral fracture, cord rupture) and revisions. Furthermore, the results of the SAQ completed at the 1-year follow-up were analyzed. We compared the rate of return to sports between the whole cohort and specific groups, namely patients with an instrumentation down to L3 or L4 and patients who had a 2-cord construct to investigate the effects instrumentation of the low lumbar spine or the use of 2-cord on the return to physical activity.
The statistical analyses were performed by one author (FM). For statistical analysis, STATA/MP software version 16 (StataCorp, College Station, TX) was used. Continuous data were expressed as mean and standard deviation, while categorical variables were expressed as percentage.
A multivariate diagnostic through the Pearson product–moment correlation coefficient (r) was performed to investigate if demographic (age, gender), radiographic parameters (Risser, Sanders, coronal and sagittal parameters) and surgical data (UIV, LIV, number of instrumented vertebrae, use of a 2-cord construct, cord rupture) have an association with the SAQ. According to the Cauchy–Schwarz equation of inequality, the final effect ranks between + 1 (positive linear correlation) and − 1 (negative linear correlation). Values of 0.1 <|r|< 0.3, 0.3 <|r|< 0.5, and |r|> 0.5 detected weak, moderate and strong correlation, respectively. The test of overall significance was performed through the χ2 test, with values of P > 0.05 considered statistically significant.
Results
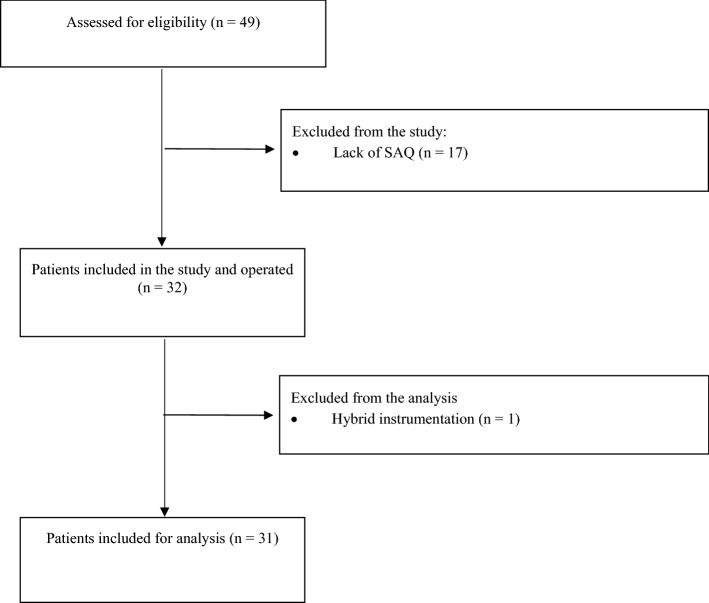
During the observation period, 49 patients who fulfilled the inclusion criteria for this study underwent VBT at our institution. Due to corona virus pandemic and since many patients live far away from our institution or abroad, an in-office follow-up was available for 32 patients. For patients who could not come to our office, follow-up was performed remotely or at the office of other orthopedic surgeons; however, these patients did not receive the SAQ questionnaire and could thus not be included in this study. One further patient was excluded as she was treated with a hybrid construct (thoracic fusion and lumbar VBT). Thus, 31 patients were recruited. A flowchart of the recruitment process is shown in Fig. 1.
Fig. 1.
Flowchart of patients’ recruitment
Demographic data
Of the 31 patients included, three were male (10%) and 28 were female (90%); the mean age at surgery was 14.5 ± 1.5 years. Regarding skeletal maturity at surgery, eight patients were Risser 0 (26%), five were Risser 1 (16%), three were Risser 2 (10%), three were Risser 3 (10%), and 12 were Risser 4 (38%). For 28 patients, the Sanders score was also available: eight were Sanders 3 (29%), two were Sanders 4 (7%), two were Sanders 5 (7%), and 16 were Sanders 7 (57%). Demographic data are summarized in Table 1.
Table 1.
Summary of demographic data and data regarding the instrumentation.
| Demographic and instrumentation data | |||
|---|---|---|---|
| N | TOT | ||
| Age (mean) | 14.5±1.5 years | ||
| Sex | F | 28 | 31 |
| M | 3 | ||
| Curve type* | Type 1 | 4 | 31 |
| Type 2 | 15 | ||
| Type 3/4 | 12 | ||
| Type 5 | 0 | ||
| Instrumented vertebrae (median) | 10 (range 6-12) | ||
| Upper instrumented vertebra | T5 | 16 | 31 |
| T6 | 7 | ||
| T7 | 2 | ||
| T10 | 3 | ||
| T11 | 2 | ||
| T12 | 1 | ||
| LIV | T11 | 1 | 31 |
| T12 | 3 | ||
| L1 | 4 | ||
| L2 | 3 | ||
| L3 | 14 | ||
| L4 | 6 | ||
| Double cord | Yes | 6 | 31 |
| No | 25 | ||
*Curve type according to Trobisch et al. [12]
Radiographic and surgical data
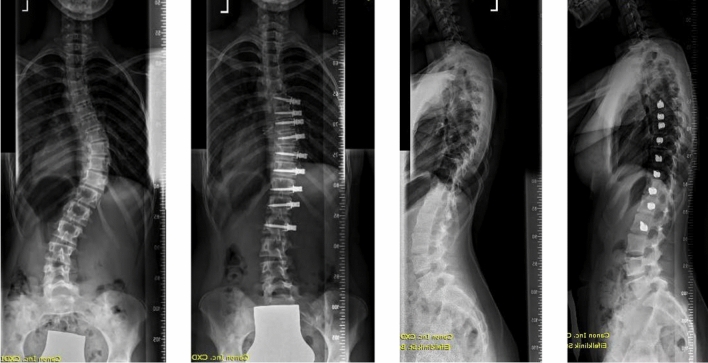
For thoracic curves, the mean Cobb angle was 56 ± 16.6° before surgery and 31.5 ± 10.1° after VBT (P < 0.001); for lumbar curves, the mean Cobb angle was 48.5 ± 15.3° before surgery and 25.2 ± 10.2° after VBT (P < 0.0001). A summary of all radiographic parameters before surgery and at the 1-year follow-up is presented in Table 2. According to the Trobisch classification [12], four patients were type 1 and underwent thoracolumbar/lumbar instrumentation, 15 patients were type 2 and underwent bilateral instrumentation, and 12 were type 3 or 4 and underwent thoracic instrumentation. Six patients had a 2-cord construct in the thoracolumbar/lumbar spine. UIV was T5 in 16 patients, T6 in seven, T7 in two, T10 in three, T11 in two and T12 in one. LIV was T11 in one patient, T12 in three, L1 in four, L2 in three, L3 in 14 and L4 in six. Data regarding the instrumentation are summarized in Table 1. A clinical example of a patient before and 1 year after VBT is shown in Fig. 2.
Table 2.
Summary of radiographic parameters before VBT and at the 1-year follow-up
| Summary of radiographic parameters | |||
|---|---|---|---|
| Preoperative | 1-year follow-up | P | |
| Cobb thoracic (°) | 56 ± 16.6 | 31.5 ± 10.1 | < 0.001 |
| Cobb lumbar (°) | 48.5 ± 15.3 | 25.2 ± 10.2 | < 0.002 |
| Coronal balance (mm) | 9.7 ± 19.1 | 7.3 ± 15.5 | 0.7 |
| Thoracic kyphosis (°) | 35.7 ± 11.2 | 39.7 ± 9.8 | 0.04 |
| Lumbar lordosis (°) | 55.1 ± 11.4 | 54 ± 10.6 | 0.2 |
| Pelvic incidence (°) | 50.8 ± 13.1 | – | – |
| Pelvic tilt (°) | 8.2 ± 8 | 6.1 ± 7.3 | 0.9 |
| Sagittal vertical axis (mm) | 2.5 ± 31.3 | 6.1 ± 21.1 | 0.6 |
Fig. 2.
Clinical example of a patient before and 1 year after VBT
Complications
No intraoperative complications were observed. One patient experienced a recurrent pleural effusion after bilateral surgery and recovered without sequelae. One patient underwent revision VBT, for add-on scoliosis after lumbar VBT. A cord rupture was observed in 14 patients; however, none of them required revision surgery for loss of correction. None of the patients required fusion. We did not observe any case of implant loosening or vertebral fracture.
Sport activity questionnaire
All patients stood up on the first postoperative day and were able to climb stairs without walking aids by the fifth postoperative day.
Overall, 30 patients responded for school: 17 returned to school less than a month after surgery (57%) and 12 one to three months after surgery (40%). All 31 patients responded for physical education/gym, with 61% of subjects returning to this activity within three months after surgery. Thirty patients answered for carrying a backpack, and 97% of them were able to do so within three months from surgery. Twenty-eight patients answered for running, and 68% could do so within 3 months after VBT (29% in less than a month after surgery). Twenty-seven patients answered for riding a bike, and 84% could perform this activity within three months from surgery. Thirty patients answered for bending: all could bend forward within three months after VBT, and 70% of them could do so already after one month. Detailed data are reported in Table 3.
Table 3.
Summary of overall data regarding return to school and physical activity after VBT
| School and physical activity after VBT | ||||||
|---|---|---|---|---|---|---|
| School | PE/Gym | Backpack | Run | Bend | Bike | |
| Patients (N) | 30 | 31 | 30 | 28 | 30 | 27 |
| < 1 month | 17 (57%) | 2 (6%) | 16 (54%) | 8 (29%) | 21 (70%) | 7 (26%) |
| 1–3 months | 12 (40%) | 17 (55%) | 13 (43%) | 11 (39%) | 9 (30%) | 15 (56%) |
| 4–6 months | 1 (3%) | 9 (29%) | 1 (3%) | 8 (29%) | – | 4 (15%) |
| 7–12 months | – | 1 (3%) | – | 1 (3%) | – | 1 (3%) |
| > 12 months | – | 2 (7%) | – | – | – | – |
Regarding sport activity, 23 patients performed noncontact sports before surgery, 16 contact and 14 collision sport. Two of the patients who did not do sports before surgery began noncontact and contact sports within six months after VBT, and six patients who only performed contact or collision sports before VBT started also noncontact and contact or collision sport one to six months postoperatively. One patient who performed noncontact and contact sports before VBT returned only to noncontact sports after surgery, and another who performed all types of sports only returned to noncontact and contact sport. Of the 27 patients who answered for noncontact sports, 63% returned to sport within three months after surgery. Eighteen answered for contact sport: 61% of patients returned to sports within 3 months and 100% within six months from VBT. Fifteen patients answered for collision sport: 53% resumed sports within 3 months and 88% within 6 months after VBT. Among the 27 patients that answered regarding their athletic performance after VBT, 56% answered that it had improved at least “somewhat.” Further details are reported in Tables 4.
Table 4.
Summary of overall data regarding return to athletic activity after VBT
| Athletic activity after VBT | |||||
|---|---|---|---|---|---|
| Noncontact | Contact | Collision | |||
| Athletic activity prior to VBT | Tot | 27 | 18 | 15 | Improvement |
| Noncontact (N = 23) | < 1 month | 2 (7%) | 3 (17%) | – | N = 27 |
| Contact (N = 16) | 1–3 months | 15 (56%) | 8 (44%) | 8 (53%) | Yes = 7 (26%) |
| Collision (N = 14) | 4–6 months | 9 (33%) | 7 (39%) | 5 (33%) | Somewhat = 8 (30%) |
| 7–12 months | 1 (4%) | - | 2 (14%) | No = 12 (44%) | |
| > 12 months | – | – | – | ||
Regarding patients who underwent instrumentation of the low lumbar spine (L3 or L4), data from 20 patients were available. In this subgroup, 19 patients responded for school and 10 of them (53%) returned to this activity within a month after VBT (95% within three months). All patients responded for physical education/gym, and 60% of them resumed these activities within three months after VBT. Fifty-three percent of patients could carry a backpack within one month from surgery (95% within three months). Nineteen patients responded for running and 68% of them could run within 3 months after VBT. Seventy-three percent patients could bend forward within a month from surgery; all were able to do so within 3 months. Nineteen patients responded for riding a bike, and 85% of them could perform this activity within 3 months from surgery.
Seventeen of the patients who were instrumented to L3 or L4 performed sports before surgery (16 noncontact, 11 contact and 11 collision sports). After VBT, 17 patients performed noncontact sports (71% within three months), 12 performed contact sport (58% within three months), and 12 performed collision sports (67% within three months). All patients who practiced sport after surgery answered to the question regarding the improvement of their athletic performance after VBT, and 53% of them noticed at least a little improvement. Further details regarding return to daily activities and sports after instrumentation of the low lumbar spine are reported in Table 5 and 6.
Table 5.
Summary of data regarding return to school and physical activity after VBT in patients with lumbar instrumentation
| School and physical activity after VBT | ||||||
|---|---|---|---|---|---|---|
| School | PE/Gym | Backpack | Run | Bend | Bike | |
| Patients (N) | 19 | 20 | 19 | 19 | 19 | 19 |
| < 1 month | 10 (53%) | 2 (10%) | 10 (53%) | 4 (21%) | 14 (73%) | 5 (27%) |
| 1–3 months | 8 (42%) | 10 (50%) | 8 (42%) | 9 (47%) | 5 (27%) | 10 (53%) |
| 4–6 months | 1 (5%) | 7 (35%) | 1 (5%) | 5 (27%) | – | 3 (15%) |
| 7–12 months | – | – | – | 1 (5%) | – | – |
| > 12 months | – | 1 (5%) | – | – | – | 1 (5%) |
Table 6.
Summary data regarding return to athletic activity after VBT in patients with lumbar instrumentation
| Athletic activity after VBT | |||||
|---|---|---|---|---|---|
| Noncontact | Contact | Collision | |||
| Athletic activity prior to VBT | Tot | 17 | 12 | 12 | Improvement |
| Noncontact (N = 16) | < 1 month | 2 (12%) | 3 (25%) | – | N = 17 |
| Contact (N = 11) | 1–3 months | 10 (59%) | 4 (33%) | 8 (67%) | Yes = 5 (29%) |
| Collision (N = 11) | 4–6 months | 5 (29%) | 5 (42%) | 3 (25%) | Somewhat = 4 (24%) |
| 7–12 months | – | – | 1 (8%) | No = 8 (47%) | |
| > 12 months | – | – | – | ||
Only six patients had a double cord instrumentation, in all cases in the thoracolumbar/lumbar spine. All of them returned to school, carried a backpack, bent forward and rode a bike within three months from surgery. Also, 83% of them returned to physical education/gym and running within 3 months after VBT. Five of the patients practiced sports before VBT and did so also after surgery as well (5 noncontact, 4 contact and 4 collision sports): within 3 months, 83% returned to noncontact sport, 60% to contact and 60% to noncontact. Eighty-three percent of the patients observed at least a little improvement in their athletic performance. Further details are reported in Table 7 and 8.
Table 7.
Summary of data regarding return to school and physical activity after VBT in patients with 2-cord construct
| School and physical activity after VBT | ||||||
|---|---|---|---|---|---|---|
| School | PE/Gym | Backpack | Run | Bend | Bike | |
| Patients (N) | 6 | 6 | 6 | 6 | 6 | 6 |
| < 1 month | 2 (34%) | 1 (17%) | 4 (66%) | 2 (34%) | 4 (66%) | 3 (50%) |
| 1–3 months | 4 (66%) | 4 (66%) | 2 (34%) | 3 (50%) | 2 (34%) | 3 (50%) |
| 4–6 months | – | 1 (17%) | – | 1 (16%) | – | – |
| 7–12 months | – | – | – | – | – | – |
| > 12 months | – | – | – | – | – | – |
Table 8.
Summary data regarding return to athletic activity after VBT in patients with 2-cord construct
| Athletic activity after VBT | |||||
|---|---|---|---|---|---|
| Noncontact | Contact | Collision | |||
| Athletic activity prior to VBT | Tot | 5 | 5 | 4 | Improvement |
| Noncontact (N = 5) | < 1 month | – | 1 (20%) | – | N = 5 |
| Contact (N = 4) | 1–3 months | 4 (80%) | 2 (40%) | 3 (75%) | Yes = 2 (40%) |
| Collision (N = 4) | 4–6 months | 1 (20%) | 2 (40%) | 1 (25%) | Somewhat = 1 (20%) |
| 7–12 months | – | – | – | No = 2 (40%) | |
| > 12 months | – | – | – | ||
The multivariate analyses showed few statistically significant associations with the SAQ. A moderate positive correlation was found between LIV and return to school (r = 0.39, P = 0.03) and carry a backpack (r = 0.42, P = 0.02). A moderate negative correlation was observed between postoperative bending and preoperative thoracic Cobb (r = − 0.49, P = 0.006), preoperative PT (r = − 0.39, P = 0.03); and between preoperative LL and return to school (r = –0.47, P = 0.01). Lastly, a moderate positive correlation was observed between return to collision sport and preoperative SVA (r = 0.48, P = 0.04). No other significant association was observed between return to physical activity and other demographic, radiographic or surgical data.
Discussion
The main finding of this study was that the majority of patients were able to resume activities of daily living and sports within three months from surgery. The majority of patients reported an improvement in their athletic performance, and some of them even engaged in more sport activities than they did before VBT.
Consensus regarding return to physical activity after spine fusion for AIS is lacking [4]. At the authors’ institution, forward bending and weight lifting (> 5 kg) are restricted for the first six weeks after surgery, while walking is encouraged. Low impact activities are allowed six weeks to six months after surgery, while unrestricted activity can begin six to 12 months postoperatively. This protocol is similar to that published by other authors [3]. As VBT does not result in disruption of any of the three spine column described by Denis et al.[20], spine stability is maintained and does not depend on the implants or on the formation of new bony structures, as is the case for fusion. Thus, there is no anatomical or biomechanical reason to restrict physical activity after VBT, and patients at our institution are allowed to self-assess and self-manage their return to sport and activity of daily living. Furthermore, we did not observe any case of screw loosening or other adverse events at the bone-implant interface (e.g., vertebral fracture), supporting the concept that no restrictions are required after VBT.
It is debatable whether an early return to sport activities has an impact on the rate of cord rupture. Among the observed subjects, no rupture was observed at the 6-week and 3-month follow-up: as most patients resumed their preoperative athletic activities within 3 months from VBT, it is unlikely that an early return to sports would increase the rupture rate. This hypothesis is supported by the fact that cord rupture did not have any significant association with any of the items of the SAQ questionnaire. However, further researches on are required to clarify this point.
Comparing our results at three months after surgery with those reported by Sarwahi et al. for fusion [4], we observed a higher rate of patients returning to school (97% vs 71%). The rate of patients returning to the gym and carrying a backpack was almost double (61% vs. 35% for gym, 97% vs. 49.5% for backpack). While all patients who underwent VBT could bend forward by three months, only 58% of fusion patients could do so. Similar trends were observed for running (68% vs. 43%) and biking (82% vs. 16%). The rate of patients returning to sports three months after VBT was consistently higher than the one observed for fusion: 63% vs. 26% for noncontact sports, 61% vs. 24% for contact sports, 53% vs. 0% for collision sports. Similar results were yielded comparing our data to the work by Tarrant and colleagues, who investigated return to activity after fusion for AIS [3]: in this setting, most patients (77%) returned to school by four months, but only a half of patients had returned to unrestricted sport activity after six months. Fabricant reported a clearance to perform athletic activity seven months after fusion [2]. Observing available data, VBT patients return to sports and activities of daily living faster than patients undergoing fusion.
Overall, only two out of 31 patients did not return to the preoperative activity level, while seven subjects begun practicing sports they did not practice before VBT. The rate of patients not returning to sports was similar to Sarwahi and Tarrant after fusion [3, 4]. However, none of the studies regarding fusion reported an increase in the kind of sports performed after surgery, as was the case after VBT.
Some authors described instrumentation of the low lumbar spine as a factor delaying return to sport or limiting the athletic performance after fusion for AIS [2, 15], while others did not observed this association [3, 4]. Sarwahi and colleagues also observed that fusion of the low lumbar spine had a negative impact on returning to the gym and carrying a backpack [4]. While we observed a moderate association between return to school and carry a backpack and LIV, this correlation is probably of little clinical relevance, as almost all patients were able to return to school and carry a backpack within three months after VBT. Also, no significant association was observed between LIV and return to sport. Thus, we conclude that LIV does not influence the return to physical activities after VBT, and an instrumentation of the low lumbar spine does not limit the range of activities that patients perform or on the time required to resume preoperative physical condition.
The most valuable data obtained from the multivariate analysis is that there was no association between SAQ parameters and radiographic or surgical parameters. Thus, even if some patients retained a residual scoliotic curve after VBT, this did not impact their ability to resume the activities they performed before surgery. Sagittal parameters also did not show association SAQ items. This finding is not surprising, as AIS patients usually do not present a sagittal imbalance: for this reason, an impairment in the ability to perform physical activities is not to be expected, and parameters such as SVA and PI remain stable after VBT.
According to the limited amount of data available for this study, the employment of a 2-cord construct did not seem to negatively affect return to activities of daily living. Also, no correlation was observed between the use of a 2-cord construct and the SAQ items. However, more studies on a larger cohort are required to further investigate this point.
This study does not come without limitations. The retrospective nature of this work along with the limited number of patients involved are the most important ones. This may increase the risk of publication bias; thus, further studies on a larger cohort are required, specially to investigate the effects of advanced correction techniques such as 2-cord constructs, and to compare the return to sport in patients with 1 or 2-cord construct in the low lumbar spine. Furthermore, given the limited number of fusions for AIS performed during the observation period, a direct comparison between these two cohorts was not possible. Also, socioeconomic and psychological factors that are involved in the return to physical activity after surgery were not analyzed, along with the impact of curve characteristics such as coronal or sagittal alignment [18, 21]. Further studies with a longer follow-up will be required to confirm the results obtained one year after VBT and compare the outcomes of this technique with those obtained with fusion.
Conclusion
Compared to available literature regarding fusion, patients undergoing VBT for AIS experienced a faster recovery and a quicker return to activities of daily living and sports. Furthermore, demographic, radiographic and surgical data did not have an association with SAQ items: in particular, LIV and residual curve magnitude did not impact the ability of patients to return to return to the physical activities they performed before surgery.
Data availability
Data can be made available in anonymized form and upon reasonable request.
Compliance with ethical standards
Conflict of interest
PDT was involved in Globus Medical (personal fees), Medtronic (personal fees), K2M (travel support). AB, AB, PK, MT, JE, SDP, FM were involved in none.
Ethical approval
RWTH Aachen, Faculty of Medicine, approval EK 130/19.
Consent for publication
Due to the retrospective nature of the study, consent to participate or for publication was not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Trobisch P, Suess O, Schwab F. Idiopathic scoliosis. Deutsch Arztebl Int. 2010;107(49):875–883. doi: 10.3238/arztebl.2010.0875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fabricant PD, Admoni S-h, Green DW, Ipp LS, Widmann RF. Return to athletic activity after posterior spinal fusion for adolescent idiopathic scoliosis: analysis of independent predictors. J Pediatr Orthop. 2012;32(3):259–265. doi: 10.1097/BPO.0b013e31824b285f. [DOI] [PubMed] [Google Scholar]
- 3.Tarrant RC, OʼLoughlin PF, Lynch S, Queally JM, Sheeran P, Moore DP, Kiely PJ. Timing and predictors of return to short-term functional activity in adolescent idiopathic scoliosis after posterior spinal fusion: a prospective study. Spine. 2014;39(18):1471–1478. doi: 10.1097/BRS.0000000000000452. [DOI] [PubMed] [Google Scholar]
- 4.Sarwahi V, Wendolowski S, Gecelter R, Maguire K, Gambassi M, Orlando D, Lo Y, Amaral T. When do patients return to physical activities and athletics after scoliosis surgery?: a validated patient questionnaire based study. Spine. 2018;43(3):167–171. doi: 10.1097/BRS.0000000000002284. [DOI] [PubMed] [Google Scholar]
- 5.Rubery PT, Bradford DS. Athletic activity after spine surgery in children and adolescents: results of a survey. Spine. 2002;27(4):423–427. doi: 10.1097/00007632-200202150-00019. [DOI] [PubMed] [Google Scholar]
- 6.Samdani AF, Ames RJ, Kimball JS, Pahys JM, Grewal H, Pelletier GJ, Betz RR. Anterior vertebral body tethering for idiopathic scoliosis: two-year results. Spine. 2014;39(20):1688–1693. doi: 10.1097/BRS.0000000000000472. [DOI] [PubMed] [Google Scholar]
- 7.Samdani AF, Ames RJ, Kimball JS, Pahys JM, Grewal H, Pelletier GJ, Betz RR. Anterior vertebral body tethering for immature adolescent idiopathic scoliosis: one-year results on the first 32 patients. Eur Spine J. 2015;24(7):1533–1539. doi: 10.1007/s00586-014-3706-z. [DOI] [PubMed] [Google Scholar]
- 8.Newton PO, Bartley CE, Bastrom TP, Kluck DG, Saito W, Yaszay B. Anterior Spinal growth modulation in skeletally immature patients with idiopathic scoliosis: a comparison with posterior spinal fusion at 2–5 years postoperatively. J Bone Joint Surg. 2020 doi: 10.2106/JBJS.19.01176. [DOI] [PubMed] [Google Scholar]
- 9.Hoernschemeyer DG, Boeyer ME, Robertson ME, Loftis CM, Worley JR, Tweedy NM, Gupta SU, Duren DL, Holzhauser CM, Ramachandran VM. Anterior vertebral body tethering for adolescent scoliosis with growth remaining: a retrospective review of 2–5-year postoperative results. J Bone Joint Surg. 2020;102(13):1169–1176. doi: 10.2106/JBJS.19.00980. [DOI] [PubMed] [Google Scholar]
- 10.Newton PO, Kluck DG, Saito W, Yaszay B, Bartley CE, Bastrom TP. Anterior spinal growth tethering for skeletally immature patients with scoliosis: a retrospective look two to four years postoperatively. J Bone Joint Surg. 2018;100(19):1691–1697. doi: 10.2106/JBJS.18.00287. [DOI] [PubMed] [Google Scholar]
- 11.Jain V, Lykissas M, Trobisch P, Wall EJ, Newton PO, Sturm PF, Cahill PJ, Bylski-Austrow DI. Surgical aspects of spinal growth modulation in scoliosis correction. Instr Course Lect. 2014;63:335–344. [PubMed] [Google Scholar]
- 12.Baroncini A, Trobisch PD, Migliorini F. Learning curve for vertebral body tethering: analysis on 90 consecutive patients. Spine Deform. 2020 doi: 10.1007/s43390-020-00191-5. [DOI] [PubMed] [Google Scholar]
- 13.Chen E, Sites BD, Rubenberg LA, Meador GD, Braun JT, Schroeck H. Characterizing anesthetic management and perioperative outcomes associated with a novel, fusionless scoliosis surgery in adolescents. AANA J. 2019;87(5):404–410. [PubMed] [Google Scholar]
- 14.Mariconda M, Andolfi C, Cerbasi S, Servodidio V. Effect of surgical correction of adolescent idiopathic scoliosis on the quality of life: a prospective study with a minimum 5-year follow-up. Eur Spine J. 2016;25(10):3331–3340. doi: 10.1007/s00586-016-4510-8. [DOI] [PubMed] [Google Scholar]
- 15.Rice SG. Medical conditions affecting sports participation. Pediatrics. 2008;121(4):841–848. doi: 10.1542/peds.2008-0080. [DOI] [PubMed] [Google Scholar]
- 16.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–349. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 17.Baroncini A, Rodriguez L, Verma K, Trobisch PD. Feasibility of single-staged bilateral anterior scoliosis correction in growing patients. Glob Spine J. 2019;21:219256821989290. doi: 10.1177/2192568219892904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Trobisch PD, Kobbe P, Baroncini A. Die dynamische skoliosekorrektur als therapieoption bei adoleszenter idiopathischer skoliose (dynamic scoliosis correction as alternative treatment for patients with adolescent idiopathic scoliosis: a non-fusion surgical technique) Zeitschrift fur Orthopadie und Unfallchirurgie. 2019 doi: 10.1055/a-0983-1265. [DOI] [PubMed] [Google Scholar]
- 19.Elsadig M, Aslanturk O, Ozturk H, Akman YE, Sinan Kahraman S, Yetisyigit Y, Tunay Sanli T, Karadereler S, Enercan M, Hamzaoglu A (2020) Surgical treatment of thoracolumbar/lumbar curves with vertebral body tethering/non-fusion anterior scoliosis correction using double screw-double cord fixation
- 20.Denis F (1984) Spinal instability as defined by the three-column spine concept in acute spinal trauma. Clinical Orthop Relat Res (189):65–76 [PubMed]
- 21.Baroncini A, Migliorini F, Trobisch PD [2020] Non-Fusion anterior scoliosis correction (ASC) positively influences sagittal parameters. 27th, April, Athens, Greece, Athens
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data can be made available in anonymized form and upon reasonable request.