Abstract
Introduction:
The optimal patient transportation destination of acute ischemic stroke (AIS) patients remains uncertain. The purpose of this study was to evaluate the predictive variables that determine stroke outcomes depending on the patient transportation destination.
Materials and Methods:
We performed a retrospective study using an acute ischemic stroke database consisting of patients, who underwent thrombectomy admitted to our institution from November 1, 2011 through October 1, 2018.
Results:
A total of 171 patients were included in the statistical analysis; 42.1% (72/171) of patients were in the mothership group (directly admitted) and 57.9% (99/171) in the drip-and-ship group (transferred). Multivariable logistic regression revealed the predictive factors for favorable outcomes were driving distance (expressed in miles) between the patient’s home and a Comprehensive Stroke Center (CSC) (OR=0.95 (0.90–0.99), p=0.035), absence of diabetes mellitus (OR=3.60 (1.20–10.82), p=0.022), lower National Institutes of Health Stroke Scale (NIHSS) score at admission (OR=0.91 (0.85–0.97), p=0.003), and shorter symptom onset to CSC arrival time (expressed in hours) (OR=0.84 (0.72–0.99), p=0.038).
Conclusions:
Our study revealed that shorter driving distance between patient’s home and CSC, absence of diabetes, lower NIHSS score, and shorter onset to hospital arrival time positively impacted the outcomes of endovascularly treated AIS patients.
Introduction
Stroke is the fifth leading cause of death in the United States [1]. Acute ischemic stroke (AIS) accounts for 87% of all stroke types [1] and up to 12% of AIS cases are caused by a large vessel occlusion (LVO) [2]. Mechanical thrombectomy (MT) is a highly effective treatment option for AIS patients with LVO. In many cases, intravenous tissue-type plasminogen activator (IV-tPA) is administered prior to or concurrently with MT [3–5], and the 2019 Stroke Guidelines recommend IV-tPA if patients are eligible [3]. The purpose of both IV-tPA and MT is to achieve successful recanalization in order to restore blood flow and tissue perfusion. Both types of recanalization therapies are time-sensitive [4–6].
In the United States, the Joint Commission1 and other certifying bodies provide eligible stroke centers with 4 types of certification: Acute Stroke Ready Hospital (ASRH), Primary Stroke Center (PSC), Thrombectomy-Capable Stroke Center (TSC) and Comprehensive Stroke Center (CSC)2. While all of them offer IV-tPA, CSCs/TSCs provide MT around the clock. This key difference has led to two triage strategies for patients with potential LVO. In the drip-and-ship strategy, patients are first transported to the closest ASRH/PSC for initial evaluation and IV-tPA treatment (if eligible). AIS patients with LVO who are eligible for MT are then transferred to the CSC/TSC. In the mothership strategy, Emergency Medical Services (EMS) personnel bypass the ASRH/PSC and transport patients directly to the nearest CSC/TSC for evaluation and treatment with IV-tPA and/or MT, if indicated. The main disadvantage of mothership strategy is that the patients who are not eligible for MT treatment get transported to the CSC/TSC, potentially overloading CSC/TSC with cases that could have been managed by an ASRH/PSC. In addition, transporting a patient to a CSC/TSC might lead to delays in IV-tPA administration for eligible patients, although an ASRH/PSC could be closer. However, the main disadvantage of drip-and-ship strategy is that transfer delay may result in thrombectomy-eligible LVO patients getting a longer onset to groin puncture time due to the long door-in-door-out times experienced at most ASRHs/PSCs, and the transport time to a CSC/TSC, resulting in potentially worse outcomes due to delays in MT [7]. On the other hand, non-LVOs, which may constitute roughly 88% of stroke patients, can be adequately treated at ASRHs/PSCs, provided computed tomography angiography (CTA) or magnetic resonance angiography (MRA) is available [2].
The purpose of this study was to evaluate the predictive variables that determine stroke outcomes depending on the patient transportation destination. We hypothesized that patients that underwent MT and were admitted directly at our CSC had better outcomes than those who were transferred from a PSC to our CSC for the MT procedure. Additionally, we hypothesized that shorter distance between the patient home and a CSC, air medical transportation, and shorter time from symptom onset to treatment was associated with better outcomes after MT.
Materials and Methods
Study population
Ethics approval from the local institutional review board was obtained with waiver of patient informed consent due to the retrospective nature of this study.
This is a retrospective observational cohort study using our institution’s stroke database to assess the clinical and imaging outcomes of AIS patients undergoing MT at our CSC. We included all AIS patients with MT who met the following criteria: presented to our CSC from November 1, 2011 – October 1, 2018 with the following inclusion criteria: (1) AIS with LVO diagnosis confirmed on imaging using either CTA, MRA and/or digital subtraction angiography (DSA), (2) mechanical thrombectomy performed, (3) admitted to our CSC either directly or through a transfer from a PSC, (4) Symptom Onset (or last known well) to CSC arrival Time (SOT) less than 24 hours. We excluded the following patients from the analysis (1) if the outcome data, such as mRS at discharge was not available in the database, and (2) SOT greater than 24 hours. Patients were categorized into two comparison groups: (1) Mothership – AIS patients who arrived directly to the CSC, and (2) Drip-and-Ship – AIS patients who were potential candidates for MT treatment and were transferred from a PSC to the CSC after starting IV-tPA, when eligible.
Stroke Database
For this analysis we used our SHOUT (Stroke Health Outcomes) database. This database consists of all stroke patients presenting to our CSC from November 1, 2011 – October 1, 2018. The database contains information on patient demographics (age, sex, race/ethnicity, patient and provider zip codes, insurance status), arrival and admission information (how patient arrived to the CSC, directly from scene/home or transfer from PSC, ground or air transportation), clinical information (initial NIHSS, SOT, comorbidities (prior stroke, hypertension, hypercholesterolemia, kidney disease, diabetes, obesity), resource utilization (type and date of head and neck imaging and treatment), quality performance metrics (onset-to-imaging, onset-to-puncture, onset-to-recanalization, imaging-to-puncture times), type of mechanical thrombectomy device used and health outcomes (mRS at discharge, at 30 days, and at 90 days, mortality information, modified Thombolysis In Cerebral Infarction (mTICI) scores, length-of-stay (LOS), discharge disposition). Distance parameter was calculated as the distance between the patient and provider (CSC) zip codes.
Predictor and Outcome Variables
The primary outcome was the clinical functional status assessed by the mRS score at hospital discharge. An early favorable outcome was defined as independent ambulation (mRS 0–3) at hospital discharge. The secondary outcome was the degree of reperfusion at the end of the MT procedure, defined by the post thrombectomy DSA images, using the mTICI score. Successful reperfusion was defined as substantial or complete recanalization (mTICI 2b-3). We also studied mortality as a tertiary outcome as in-hospital and 7-day mortality rates.
We evaluated several predictor variables to assess their association with the clinical and imaging outcomes. The following factors were assessed: (1) patient demographic data - age, sex, (2) clinical stroke severity – NIHSS at presentation, SOT (hours), (3) distance parameter – distance (miles) from patient’s home to CSC, (4) post discharge information –mRS at discharge was used as a dependent variable in the regression analysis, (5) arrival and admission information – how patient arrived to the CSC (directly from scene/home or transfer from PSC), (7) Comorbidities (prior stroke, hypertension, hypercholesterolemia, kidney disease, diabetes, obesity), (8) Treatment –if IV-tPA was given, and mTICI score, and (9) mode of transportation – ground or air. None of the patients arrived by an airplane, therefore air transportation option was limited to a helicopter transportation.
Statistical analysis
We performed the analysis using the mRS at discharge as the outcome metric, because this data was the most complete in our database. Standard descriptive statistics were used, including mean and standard deviation for continuous variables and frequency distribution for categorical variables. For between-group comparisons the following tests were used: t-tests for continuous variables, and χ2 tests/ Fisher’s exact tests for categorical variables. Statistical significance was considered for p-values < 0.05.
To determine the relative importance of the covariates on the clinical and imaging outcomes, a multivariate logistic regression model was developed. All predictor and outcome variables were entered in the model. Odds-ratio (OR) and their 95% confidence intervals were reported. In this analysis, the primary outcome variable – mRS 0–3 at discharge was modeled against predictors of interest using logistic regression. We selected the parameters for the model based on clinical relevance. In this model, age, SOT (expressed in hours), NIHSS score, and driving distance (expressed in miles) between the patient’s home and CSC were regarded as continuous variables. Sex, diabetes, hypertension, obesity, transfer status, IV-tPA, TICI score 2b/3, and air transportation were categorical variables. Confidence intervals and odds ratios (ORs) were derived using normal approximation based on standard errors. The distribution of discharge mRS between groups was compared using the Mantel-Haenszel ordinal χ2 statistic. All analyses were performed using IBM SPSS 2019 v.1.0.0 software (IBM, Inc, Armonk, NY).
Results
Study population
A total of 7,558 stroke patients were treated at our comprehensive stroke center from November 1, 2011 to October 1, 2018. Of these, 57.5% (4,344/7,558), had an AIS and 4.05% of AIS patients (176/4,344) underwent MT at our comprehensive stroke center. Among patients that underwent MT, five patients had their discharge mRS missing and 3.9% of AIS patients (171/4,344) had discharge mRS documented. Forty-two percent (72/171) of MT patients were in the mothership group and 57.9% (99/171) of patients were in the drip-and-ship group. For 30-day mRS, 12.9% (22/171) patients had missing data, including 15.3% (11/72) patients in the mothership group and 11.1% (11/99) patients in the drip-and-ship group. There were 49.1% (84/171) patients missing mRS at 90 days, including 52.8% (38/72) patients in the mothership group and 46.5% (46/99) patients in the drip-and-ship group. A majority of both groups were treated with IV-tPA, including 65.3% (47/72) patients in the mothership group, and 72.7% (72/99) patients in the drip-and-ship group (p=0.296).
The demographic and clinical characteristics of the mothership and drip-and-ship groups are presented in Table 1. The mothership and drip-and-ship groups did not differ significantly in terms of demographic characteristics, such as age, sex, SOT, initial NIHSS, and comorbidities. In addition, the groups did not significantly differ according to mechanical thrombectomy device used and process time measured (onset-to-imaging, onset-to-puncture, onset-to-recanalization, imaging-to-puncture time). There was only one statistically significantly different characteristic variable against the mothership and drip-and-ship groups. It was air transportation parameter. This means that in the drip-and-ship group there were statistically significantly more patients transported by air, than in mothership group. In our region, if stroke patients are transported by air, these are typically interhospital transfer patients.
Table 1.
Demographic and Clinical Characteristics of Acute Stroke Patients With Mechanical Thrombectomy
| Characteristics | Mothership (n=72) | Drip-and-Ship (n=99) | P-Value |
|---|---|---|---|
| Age <50 | 11.1% (8/72) | 12.1% (12/99) | 0.446 |
| Age 50–80 | 56.9% (41/72) | 64.6% (64/99) | |
| Age >80 | 31.9% (23/72) | 23.2% (23/99) | |
| Age years, mean (SD) | 70 (14.6) | 68.7 (14.4) | 0.561 |
| SOT 0–4.5 hours | 81.8% (54/66) | 75.5% (74/98) | 0.704 |
| SOT >4.5–6 hours | 9.1% (6/66) | 12.2% (12/98) | |
| SOT >6–24 hours | 9.1% (6/66) | 11.2% (11/98) | |
| SOT, mean (SD) | 3:46:30 (4:37:24) | 4:26.03 (3:52:23) | 0.336 |
| NIHSS 0 | 0% (0/72) | 1% (1/98) | 0.289 |
| NIHSS 1–4 | 2.8% (2/72) | 0% (0/98) | |
| NIHSS 5–9 | 4.2% (3/72) | 6.1% (6/98) | |
| NIHSS 10–42 | 93.1% (67/72) | 92.9% (91/98) | |
| Baseline NIHSS Score, mean (SD) | 19.32 (6.65) | 18.89 (6.62) | 0.675 |
| Female | 48.6% (35/72) | 43.4% (43/99) | 0.502 |
| Vascular Risk Factors | |||
| Hypertension | 55.6% (40/72) | 58.6% (58/99) | 0.692 |
| Diabetes | 19.4% (14/72) | 25.3% (25/99) | 0.371 |
| Obesity/Overweight | 44.4% (32/72) | 48.5% (48/99) | 0.601 |
| Hypercholesterolemia | 40.3% (29/72) | 39.4% (39/99) | 0.907 |
| Previous stroke | 12.5% (9/72) | 8.1% (8/99) | 0.340 |
| Smoking | 9.7% (7/72) | 15.2% (15/99) | 0.295 |
| Antiplatelet or anticoagulant Medications | 54.2% (39/72) | 47.5% (47/99) | 0.388 |
| Mechanical thrombectomy device | |||
| Retrievable stent | 51.4% (37/72) | 59.6% (59/99) | 0.286 |
| Other mechanical clot retriever device (not retrievable stent) | 8.3% (6/72) | 5.1% (5/99) | 0.388 |
| Clot suction device | 43.1% (31/72) | 54.5% (54/99) | 0.138 |
| Process time | |||
| Onset-to-imaging, mean (SD) | 2:19:43 (3:49:30) | 2:26:24 (2:44:53) | 0.893 |
| Onset-to-puncture, mean (SD) | 4:57:03 (4:49:35) | 6:11:38 (6:22:10) | 0.246 |
| Onset-to-recanalization, mean (SD) | 5:20:12 (4:21:33) | 6:41:39 (6:22:11) | 0.179 |
| Imaging-to-puncture, mean (SD) | 2:15:19 (3:22:40) | 4:49:00 (7:06:25) | 0.094 |
| Air transportation | 1.4% (1/72) | 10.1% (10/99) | 0.026 |
NIHSS - National Institutes of Health Stroke Scale
SD – standard deviation
SOT – Symptom Onset Time
Clinical and Imaging Outcomes
There was no statistically significant difference between the mothership and drip-and-ship groups in the univariate analysis for the outcome measures (Table 2). The secondary outcome, assessed by successful recanalization (TICI 2b-3) rates, was not significantly different between the mothership and drip-and-ship groups. Mortality (in-hospital and 7-day) was also similar between the two groups.
Table 2.
Clinical and Imaging Outcomes in Acute Stroke Patients with Mechanical Thrombectomy
| Outcomes | Mothership (n=72) | Drip-and-Ship (n=99) | P-Value |
|---|---|---|---|
| mRS<=1 at discharge | 25% (18/72) | 20.2% (20/99) | 0.456 |
| mRS<=2 at discharge | 36.1% (26/72) | 29.3% (29/99) | 0.346 |
| mRS<=3 at discharge | 47.2% (34/72) | 43.4% (43/99) | 0.623 |
| Recanalization (TICI 2B-3) | 88.5% (54/61) | 87.4% (76/87) | 0.831 |
| IV-tPA | 65.3% (47/72) | 72.7% (72/99) | 0.296 |
| In-hospital mortality | 13.9% (10/72) | 17.2% (17/99) | 0.561 |
| 7-day mortality | 6.9% (5/72) | 11.1% (11/99) | 0.356 |
IV-tPA - Intravenous tissue-type Plasminogen Activator
mRS – modified Rankin Scale
TICI - Thrombolysis In Cerebral Infarction
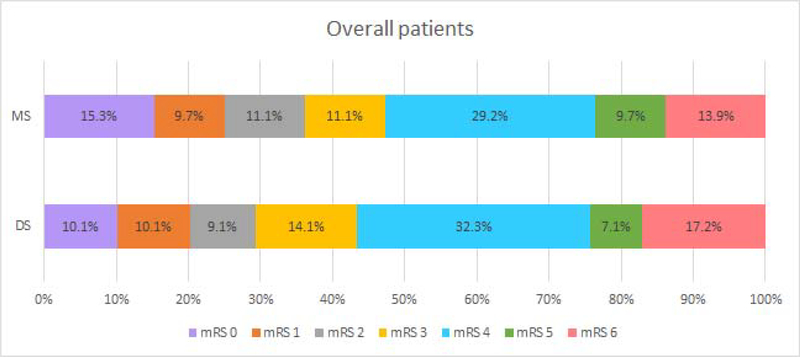
Even though clinical outcomes at discharge were better in the mothership group, with 47% (34/72) patients achieving independent ambulation (mRS 0–3) compared with 43% (43/99) in the drip-and-ship group, this difference was not statistically significant (unadjusted OR 0.86 (0.47–1.58); p=0.623) (Figure 1).
Figure 1.
Unadjusted clinical outcomes at discharge, overall.
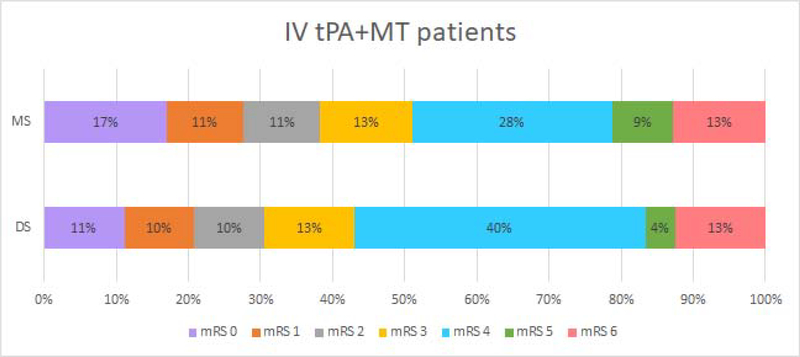
Subgroup analysis was performed among patients who received IV-tPA before MT, and independent ambulation was achieved in 51% (24/47) of mothership patients compared to 43% (31/72) of drip-and-ship patients, although this difference was not statistically significant (unadjusted OR 0.73 (0.35–1.52); p=0.39) (Figure 2).
Figure 2.
Unadjusted clinical outcomes at discharge, IV-tPA + MT
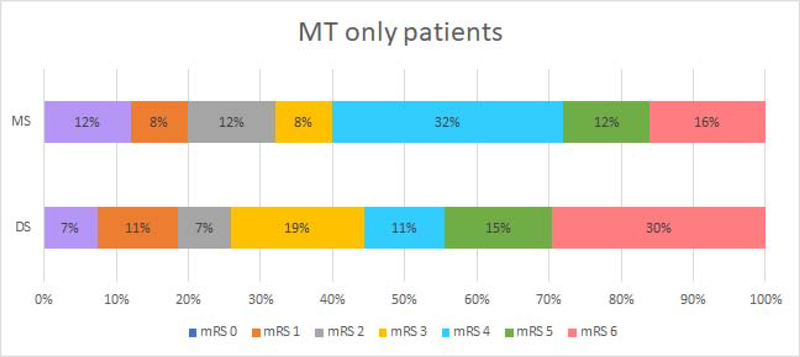
In the subgroup analysis of the MT-alone patients (without prior IV-tPA), independent ambulation was less common in the mothership group 40% (10/25) compared to the drip-and-ship group 44% (12/27), although this difference was not statistically significant (unadjusted OR 1.2 (0.40–3.62); p=0.75) (Figure 3).
Figure 3.
Unadjusted clinical outcomes at discharged, MT only.
Logistic Regression Analysis
For the primary outcome of independent ambulation (mRS 0–3) at discharge, logistic regression demonstrated the following predictor variables as statistically different (Table 3): shorter driving distance (miles) between the patient’s home and the CSC (OR=0.95 (0.90–0.99), p=0.035), absence of diabetes mellitus (OR=3.60 (1.20–10.82), p=0.022), lower admission NIHSS score (OR=0.91 (0.85–0.97), p=0.003), and lower SOT (hours) (OR=0.84 (0.72–0.99), p=0.038). Whether the patient was directly admitted to the CSC was not statistically significant in the regression model (OR=0.89 (0.37–2.10), p=0.751). Likewise, whether the patient was transported by air was not statistically significant in the regression model (OR=1.88 (0.42–8.34), p=0.405). Thus, the first part of the original hypothesis that mothership was associated with better outcomes than drip-and-ship was not supported by our regression model. Although we did not see that air transportation was associated with better outcomes, the regression model showed that shorter distance between a patient’s home and the CSC, and shorter time between SOT and treatment was associated with better outcomes.
Table 3.
Adjusted Odds Ratios (ORs) for Independent Ambulation (Modified Rank Scale Score of 0 to 3 at Discharge)
| Outcome | OR (95% CI) | P-Value adjusted |
|---|---|---|
| Driving distance (expressed in miles) between the patient home and CSC | 0.95 (0.90–0.99) | 0.035 |
| Absence of diabetes mellitus | 3.60 (1.20–10.82) | 0.022 |
| NIHSS score at admission | 0.91 (0.85–0.97) | 0.003 |
| Symptom onset to arrival time, expressed in hours | 0.84 (0.72–0.99) | 0.038 |
| Air transportation | 1.88 (0.42–8.34) | 0.405 |
| Mothership | 0.89 (0.37–2.10) | 0.751 |
CSC - Comprehensive Stroke Center
NIHSS - National Institutes of Health Stroke Scale
Discussion
Given the continued uncertainty regarding an optimal triage strategy for AIS patients with potential LVO, we hypothesized that the need for patient transfer in the drip-and-ship model would result in worse clinical outcomes compared to the mothership model. Our analysis shows that this is not the case.
Our study found that AIS patients with LVO did not have statistically different early outcomes comparing the mothership and drip-and-ship strategies. Likewise, in the subgroup of patients who did not receive IV-tPA, the outcomes of drip-and-ship patients were improved, although not statistically significantly. Furthermore, neither triage strategy was statistically significantly associated with better early outcomes in the regression model.
Several prior observational studies also did not find differences in functional outcomes between mothership and drip-and-ship strategies [8–10]. When the studies did find differences in outcomes between these two strategies, the findings were often conflicting. Some observational studies found improved CSC processing efficiency and better outcomes (functional independence with mRS 0–2 at 90 days) in the mothership strategy [11–13]. These studies found significant treatment delays in the drip-and-ship strategy compared to the mothership strategy. However, in our study, no statistically significant CSC process efficiency difference was found between mothership and drip-and-ship patients. Froehler (2017) [13] found that patients who received MT with long interhospital transfer delays experienced worse outcomes than those without interhospital transfer. Nevertheless, a recent systematic review and meta-analysis [14] concluded that patients with an acute ischemic stroke admitted directly to a comprehensive stroke center for endovascular treatment (mothership patients) may have had better 90-day outcomes compared to drip-and-ship patients.
Two modeling studies [15, 16] explored outcomes between drip-and-ship and mothership strategies when PSC and CSC centers were 60 minutes or less from each other. As suggested by Holodinsky (2017) [16], the mothership strategy was superior to drip-and-ship strategy when transport times between PSC and CSC were short (10–30 minutes). In our regression model, we found that shorter distance between the patient’s home and CSC increased the odds of a favorable early outcomes. In addition, Holodinsky (2017) [16] showed that the drip-and-ship model became the superior option when the patient was close to the PSC, and the time between the PSC and CSC was 45 minutes or longer. Consistent with their prior study, a third modeling study by Holodnitsky (2018) [17], found that the mothership strategy was better only in regions close to a CSC. They demonstrated that in regions further away from a CSC, both transport approaches resulted in equivalent outcomes. The sensitivity analysis employed by these three modeling studies, using probabilistic modeling of stroke care in Alberta, Canada, suggested that the mothership approach may be preferable when the additional travel time between PSC hospitals and a CSC was <60 minutes [15–17]. In a modeling study by Benoit (2018) [18], mothership was superior until the additional transport time exceeded 44 minutes. The decision modeling study by Xu (2019) [19], found that in addition to the impact of travel distance, the utilization of pre-hospital LVO screening tools positively impacted the efficacy of the mothership strategy for potential LVO patients. However, if it was not possible for EMS to determine if a patient has an LVO or not, then the drip-and-ship strategy became superior to the mothership strategy.
One important limitation of the drip-and-ship paradigm that is often overlooked is the issue of access to MT. In a retrospective observational study, Sablot (2017) [20] found that transfer to a distant CSC was associated with reduced access to early MT in acute stroke patients with LVO. In a subgroup analysis, the authors noticed that in the drip-and-ship strategy, a group of 73 patients who may have benefited from MT lost this opportunity because by the time of CSC arrival, they were already out of the time window, or transportation to the CSC was unavailable. At least some of these patients would have been eligible for MT if the mothership strategy was used. Likewise, Pérez de la Ossa (2016) [21] who divided their study region (Catalonia) into three groups, depending on transfer time to the CSC, found that many MT-eligible patients admitted to a PSC more than 30 min away from the CSC were not transferred for MT. Similarly, Park (2016) [9] reported fewer MT treated patients using the drip-and-ship paradigm. Many patients were excluded from the MT procedure after the transfer, while they may have been eligible if the first stroke center contact had been a CSC. Detraz (2018) [22] found that the drip-and-ship patients might be less likely to have a good outcome, not because of the MT procedure per se, but because of limited access to it.
Our study has several important limitations. First, we used independent ambulation with mRS 0–3 at discharge as our outcome measure because it was readily available in our database. Nearly all studies of endovascular treatment consider a favorable outcome as functional independence (mRS 0–2) at 90 days. By using independent ambulation at discharge, we are focused on early stroke outcomes, instead of 90-day outcomes. Several studies have shown early stroke outcome is a good predictor of longer-term outcome [23–25]. Second, our sample size of 171 patients is relatively small and may have resulted in missing statistically small differences between groups. However, the ratio of the number of participants to the number of variables in our regression model is comparable to other studies [26,27]. Due to access limitations to MT in clinical practice, many of the published observational studies have a comparable or smaller number of patients [8–10,20]. Third, we did not account for conditions potentially impacting driving times such as weather or road conditions. Finally, between 2011 to 2018, stroke treatment practice significantly evolved with improvements in devices, techniques, and efficiencies, and indications for treatment have expanded up to 24 hours from last known well, resulting in many more patients becoming eligible for MT then were previously.
Conclusions
Although there was a trend towards better outcomes in acute stroke patients with LVO in the mothership strategy compared to the drip-and-ship strategy, there was no statistically significant difference. Factors predicting early independent ambulation (mRS 0–3) for LVO patients were shorter distance from a patient’s home to the CSC, absence of diabetes mellitus, lower initial NIHSS score, and shorter symptom onset to treating hospital presentation time.
Acknowledgments
Grant support: This is an investigator-initiated study. Jeffrey M. Katz, Jason J. Wang, and Pina C. Sanelli received research funding from Siemens Medical Solutions USA, Inc. Artem T. Boltyenkov and Maria G. Martinez are employees of Siemens Medical Solutions USA, Inc.
Research reported in this publication was supported by The Feinstein Institutes for Medical Research, Northwell Health, National Institute of Neurological Disorders and Stroke of the National Institutes of Health under award number R56NS114275, and Siemens Medical Solutions USA, Inc.. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health
List of abbreviations
- AIS
Acute Ischemic Stroke
- ASRH
Acute Stroke Ready Hospital
- CSC
Comprehensive Stroke Center
- CTA
Computed Tomography Angiography
- DSA
Digital Subtraction Angiography
- EMS
Emergency Medical Services
- IV-tPA
Intravenous tissue-type Plasminogen Activator
- LOS
Length of Stay
- LVO
Large Vessel Occlusion
- MRA
Magnetic Resonance Angiography
- mRS
modified Rankin Scale
- MT
Mechanical Thrombectomy
- mTICI
modified Thrombolysis In Cerebral Infarction
- NIHSS
National Institutes of Health Stroke Scale
- OR
Odds Ratio
- PSC
Primary Stroke Center
- SOT
Symptom Onset Time
- SHOUT
Stroke Health Outcomes
- TSC
Thrombectomy-Capable Stroke Center
Biography

Footnotes
Ethics approval from the local institutional review board was obtained with waiver of patient informed consent due to the retrospective nature of this study.
The Joint Commission. www.jointcommission.org, Address: One Renaissance Blvd. Oakbrook Terrace, IL 60181
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation. 2016;133:e38–e360. [DOI] [PubMed] [Google Scholar]
- 2.Rai AT, Seldon AE, Boo S, Link PS, Domico JR, Tarabishy AR, et al. A population-based incidence of acute large vessel occlusions and thrombectomy eligible patients indicates significant potential for growth of endovascular stroke therapy in the USA. J Neurointerv Surg 2017;9:722–726. doi: 10.1136/neurintsurg-2016-012515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. ; Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. 2019; 50(12):e344–e418. doi: 10.1161/STR.0000000000000211 [DOI] [PubMed] [Google Scholar]
- 4.Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E, et al. ; Stroke Thrombolysis Trialists’ Collaborative Group. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet. 2014;384:1929–1935. doi: 10.1016/S0140-6736(14)60584-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saver JL, Goyal M, van der Lugt A, Menon BK, Majoie CB, Dippel DW, et al. ; HERMES Collaborators. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. JAMA. 2016;316:1279–1288. doi: 10.1001/jama.2016.13647 [DOI] [PubMed] [Google Scholar]
- 6.Kim JT, Fonarow GC, Smith EE, Reeves MJ, Navalkele DD, Grotta JC, et al. Treatment with tissue plasminogen activator in the golden hour and the shape of the 4.5-hour time-benefit curve in the National United States Get With The Guidelines-Stroke Population. Circulation. 2017;135:128–139. doi: 10.1161/CIRCULATIONAHA.116.023336 [DOI] [PubMed] [Google Scholar]
- 7.Ng FC, Low E, Andrew E, Smith K, Campbell BCV, Hand PJ, Crompton DE, Wijeratne T, Dewey HM, Choi PM. Deconstruction of Interhospital Transfer Workflow in Large Vessel Occlusion: Real-World Data in the Thrombectomy Era. Stroke. 2017. July;48(7):1976–1979. doi: 10.1161/STROKEAHA.117.017235. Epub 2017 May 16. [DOI] [PubMed] [Google Scholar]
- 8.Gerschenfeld G, Muresan IP, Blanc R, Obadia M, Abrivard M, Piotin M, Alamowitch S. Two paradigms for endovascular thrombectomy after intravenous thrombolysis for acute ischemic stroke. JAMA Neurol 2017;74:549–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Park MS, Yoon W, Kim JT, Choi KH, Kang SH, Kim BC et al. Drip, ship, and on-demand endovascular therapy for acute ischemic stroke. PLoS One. 2016;11:e150668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ishihara H, Oka F, Oku T, Shinoyama M, Suehiro E, Sugimoto K, et al. Safety and time course of drip-and-ship in treatment of acute ischemic stroke. J Stroke Cerebrovasc Dis 2017;26:2477–2481. doi: 10.1016/j.jstrokecerebrovasdis.2017.03.008 [DOI] [PubMed] [Google Scholar]
- 11.Park MS, Lee JS, Park TH, Cho YJ, Hong KS, Park JM et al. Characteristics of the drip-and-ship paradigm for patients with acute ischemic stroke in South Korea. J Stroke Cerebrovasc Dis 2016;25:2678–87. [DOI] [PubMed] [Google Scholar]
- 12.Mohamad NF, Hastrup S, Rasmussen M, Andersen MS, Johnsen SP, Andersen G et al. Bypassing primary stroke centre reduces delay and improves outcomes for patients with large vessel occlusion. Eur Stroke J 2016;1:85–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Froehler MT, Saver JL, Zaidat OO, et al.Interhospital transfer prior to thrombectomy is associated with delayed treatment and worse outcome in the STRATIS Registry. Circulation. 2017; 136(24):2311–2321. doi: 10.1161/CIRCULATIONAHA.117.028920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ismail M, Armoiry X, Tau N, Zhu F, Sadeh-Gonik U, Piotin M, Blanc R, Mazighi M, Bracard S, Anxionnat R, Schmitt E, Mione G, Humbertjean L, Lacour JC, Richard S, Barbier C, Lapergue B, Gory B. Mothership versus drip and ship for thrombectomy in patients who had an acute stroke: a systematic review and meta-analysis. J Neurointerv Surg 2019. January;11(1):14–19. [DOI] [PubMed] [Google Scholar]
- 15.Milne MS, Holodinsky JK, Hill MD, Nygren A, Qiu C, Goyal M et al. Drip’n ship versus mothership for endovascular treatment: modeling the best transportation options for optimal outcomes. Stroke. 2017;48:791–4. [DOI] [PubMed] [Google Scholar]
- 16.Holodinsky JK, Williamson TS, Kamal N, Mayank D, Hill MD, Goyal M. Drip and ship versus direct to comprehensive stroke center. Stroke. 2017;48:233–8. [DOI] [PubMed] [Google Scholar]
- 17.Holodinsky JK, Williamson TS, Demchuk AM, Zhao H, Zhu L, Francis MJ, et al. Modeling stroke patient transport for all patients with suspected large-vessel occlusion. JAMA Neurol 2018;75:1477–1486. doi: 10.1001/jamaneurol.2018.2424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Benoit JL, Khatri P, Adeoye OM, Broderick JP, McMullan JT, Scheitz JF, et al. Prehospital triage of acute ischemic stroke patients to an intravenous tPA-ready versus endovascular-ready hospital: a decision analysis. Prehosp Emerg Care. 2018;22:722–733. doi: 10.1080/10903127.2018.1465500 [DOI] [PubMed] [Google Scholar]
- 19.Xu Y, Parikh NS, Jiao B, Willey JZ, Boehme AK, Elkind MSV. Decision Analysis Model for Prehospital Triage of Patients With Acute Stroke. Stroke. 2019. April;50(4):970–977. doi: 10.1161/STROKEAHA.118.023272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sablot D, Gaillard N, Smadja P, Bonnec J-M, Bonafe A. Thrombectomy accessibility after transfer from a primary stroke center: analysis of a three-year prospective registry. Int J Stroke. 2017;12:519–23. [DOI] [PubMed] [Google Scholar]
- 21.Pérez de la Ossa N, Abilleira S, Dorado L, Urra X, Ribó M, Cardona P et al. Catalan Stroke Code and Reperfusion Consortium. Access to endovascular treatment in remote areas: analysis of the Reperfusion Treatment Registry of Catalonia. Stroke. 2016;47:1381–4. [DOI] [PubMed] [Google Scholar]
- 22.Detraz L, Ernst M, Bourcier R. Stroke Transfer and its Organizational Paradigm. Clin Neuroradiol (2018) 28:473–480 [DOI] [PubMed] [Google Scholar]
- 23.Qureshi AI, Chaudhry SA, Sapkota BL, Rodriguez GJ, Suri MF. Discharge destination as a surrogate for Modified Rankin Scale defined outcomes at 3- and 12-months poststroke among stroke survivors. Arch Phys Med Rehabil 2012. August;93(8):1408–1413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Asuzu D, Nystrom K, Amin H, Schindler J, Wira C, Greer D, Chi NF, Halliday J, Sheth KN. Modest association between the discharge modified Rankin Scale score and symptomatic intracerebral hemorrhage after intravenous thrombolysis. J Stroke Cerebrovasc Dis 2015. March;24(3):548–53. [DOI] [PubMed] [Google Scholar]
- 25.Mahmoud Fouad M, Mohamed Farag S, Hegazy MI, Abd Elalem Aziz M. Prediction of Functional Outcome in Ischemic Stroke Patients: An Observational Study on Egyptian Population. Cureus 2017. June 26;9(6):e1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.van der Ploeg T, Austin PC & Steyerberg EW Modern modelling techniques are data hungry: a simulation study for predicting dichotomous endpoints. BMC Med Res Methodol 14, 137 (2014). 10.1186/1471-2288-14-137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Riley RD, Snell KI, Ensor J, Burke DL, Harrell FE Jr, Moons KG, Collins GS. Minimum sample size for developing a multivariable prediction model: PART II - binary and time-to-event outcomes. Stat Med 2019. March 30;38(7):1276–1296. doi: 10.1002/sim.7992. Epub 2018 Oct 24. Erratum in: Stat Med. 2019 Dec 30;38(30):5672. [DOI] [PMC free article] [PubMed] [Google Scholar]