Watch a video presentation of this article
Watch an interview with the author
Abbreviations
- CSC
Correctional Service Canada
- HCV
hepatitis C virus
- PWAI
people who are incarcerated
- PWID
people who inject drugs
- STBBI
sexually transmitted and blood‐borne infection
More than 50% of people who are incarcerated (PWAI) in Canada report a history of drug use, 1 and about 76% of people who inject drugs (PWID) in Canada have a history of incarceration, 2 resulting in higher prevalence of hepatitis C virus (HCV) among PWAI compared with the general population. 3 The Blueprint to Inform Hepatitis C Elimination Efforts in Canada, 4 published by the Canadian Network on Hepatitis C in 2019, identifies PWAI as a priority group for increased access to HCV care. Consequently, HCV screening and treatment in correctional settings are priorities to improve the health of PWID and PWAI and to achieve the World Health Organization’s 2030 HCV elimination targets. Although promising HCV screening strategies and models of care in correctional settings exist across Canada, efforts to implement HCV prevention, screening, and treatment programs in correctional settings have been slow. However, recent policy changes have made HCV elimination within Canadian custodial settings by 2030 a possibility.
HCV in the Canadian Federal Correctional System
Correctional Service Canada (CSC) manages and maintains 43 institutions where people sentenced for 2 years or more are detained. Statistics Canada reported an average daily count of 14,129 people in federal custody in 2017/2018, with 6903 admissions over the same period. 5 In 2014, HCV antibody prevalence rate was estimated by CSC at 18.6% among federally incarcerated men and 22.7% among women (Fig. 1). 6 As a result of ongoing colonization in Canada, indigenous people are vastly overrepresented among PWAI and disproportionately impacted by HCV 7 ; among indigenous men and women who are incarcerated, 27.7% and 44.8%, respectively, are estimated to have HCV antibodies. 8 Among people who entered federal custody without prior HCV exposure, incidence of HCV acquisition is estimated at 25 cases per 1000 PWAI at risk per year. 9
FIG 1.
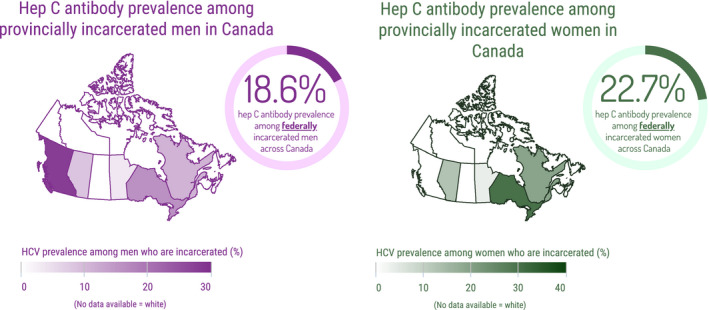
Most recent published HCV (Hep C) antibody prevalence estimates among men and women who are incarcerated federally and provincially in Canada (see Table 1 for a detailed breakdown and references). See http://www.hepcorrections.org/map for a similar map of HCV antibody prevalence among people who are incarcerated in the United States (map by Emory Center for the Health of Incarcerated Persons and MGH Institute for Technology Assessment).
HCV screening at intake to federal corrections is universally offered to all entrants, with 80% to 90% accepting testing. 6 Universal, or opt‐out, testing in correctional settings results in higher uptake compared with opt‐in or on‐demand testing, 10 , 11 , 12 and therefore should be a high‐priority intervention for all correctional settings. All PWAI in federal institutions are eligible for HCV treatment irrespective of fibrosis staging and are offered treatment by CSC‐contracted physicians. Beginning in 2018, CSC began rolling out prison needle exchange programs in federal institutions, with 11 implemented so far. 13 In 2019, CSC also began an Overdose Prevention Service at Drumheller Institution in Alberta, where drugs can be consumed by PWAI under supervision, with sterile drug use equipment provided. 14 CSC has not yet published data regarding the proportion of PWAI who initiate and complete treatment; however, CSC is well positioned to achieve HCV elimination within federal Canadian correctional institutions within the next decade as best practices such as universal HCV screening, access to treatment, and harm reduction services are available.
HCV Infection Among People Who Are Provincially Incarcerated in Canada
Provincial and territorial governments are responsible for their correctional systems, respectively, across Canada. Both systems detain people who are on remand (awaiting trial or sentencing) and people who are sentenced to a custodial period of less than 2 years. People sentenced in federal corrections may have served an initial period of their sentence in provincial corrections while awaiting trial or sentencing. Provincial/territorial corrections are characterized by a large number of intakes and releases because of the short average duration of incarceration, with 234,675 custodial admissions to provincial and territorial correctional centers in 2017/2018. 5 There are large gaps in published estimates for HCV antibody prevalence among PWAI in provincial/territorial corrections across Canada, and significant heterogeneity exists among published estimates (Table 1 and Fig. 1). One consistent aspect is that incarcerated women have a higher HCV antibody prevalence compared with incarcerated men. This is likely because incarcerated women are more often detained for drug‐related offenses compared with men, resulting in a higher proportion of incarcerated women also being PWID. HCV antibody prevalence in published estimates appears to decrease over time among both men and women, explained by secular trends such as a lower proportion of people being incarcerated for drug‐related offenses, or a cohort effect, with HCV antibody prevalence being lower among younger cohorts entering prison in more recent decades. However, this may also be a sampling or measurement bias.
TABLE 1.
Published HCV Antibody Prevalence Estimates Among Men and Women Who Are Incarcerated Federally and Provincially in Canada
| HCV Antibody Prevalence Rate | Province or Territory | Federal or Provincial | Sex | Study Type | Study Period | Year Published | First Author |
|---|---|---|---|---|---|---|---|
| 28.00% | British Columbia | Federal | Male | Cross‐sectional | 1989 | 1994 | Préfontaine 40 |
| 27.90% | Ontario | Federal | Male | Cross‐sectional | 1994 | 1995 | Pearson 41 |
| 39.80% | Ontario | Federal | Female | Cross‐sectional | 1994 | 1995 | Ford 42 |
| 33.00% | Ontario | Federal | Male | Cross‐sectional | 1998 | 2000 | Ford 43 |
| 25.90% | National | Federal | Male | Cross‐sectional | 2002 | 2004 | De 44 |
| 34.00% | National | Federal | Female | Cross‐sectional | 2002 | 2004 | De 44 |
| 16.60% | Quebec | Provincial | Male | Cross‐sectional | 2003 | 2007 | Poulin 45 |
| 29.20% | Quebec | Provincial | Female | Cross‐sectional | 2003 | 2007 | Poulin 45 |
| 15.90% | Ontario | Provincial* | Male | Cross‐sectional | 2003/2004 | 2007 | Calzavara 46 |
| 30.20% | Ontario | Provincial* | Female | Cross‐sectional | 2003/2004 | 2007 | Calzavara 46 |
| 21.70% | National | Federal | All | Modeled | 2005 | 2007 | Remis 47 |
| 16.9% | National | Provincial | All | Modeled | 2005 | 2007 | Remis 47 |
| 24.90% | National | Federal | Male | Retrospective | 2005‐2012 | 2016 | CSC 8 |
| 33.10% | National | Federal | Female | Retrospective | 2005‐2012 | 2016 | CSC 8 |
| 24.00% | National | Federal | All | Modeled | 2011 | 2014 | Trubnikov 48 |
| 23.25% | National | Provincial | All | Modeled | 2011 | 2014 | Trubnikov 48 |
| 3.50% | Manitoba | Provincial* | All | Retrospective | 2012 | 2014 | Hodge 49 |
| 18.60% | National | Federal | Male | Retrospective | 2014 | 2016 | CSC 6 |
| 22.70% | National | Federal | Female | Retrospective | 2014 | 2016 | CSC 6 |
| 19.2% | Quebec | Provincial | Female | Cross‐sectional | 2014/2015 | 2018 | Courtemanche 50 |
| 11.90% | Quebec | Provincial | Male | Cross‐sectional | 2014/2015 | 2018 | Courtemanche 50 |
| 11.00% | Quebec | Provincial | Male | Retrospective | 2017/2018 | 2019 | Kronfli 51 |
| 12.60% | Alberta | Provincial | Female | Retrospective | 2012‐2015 | 2019 | Gratix 52 |
| 8.50% | Alberta | Provincial | Male | Retrospective | 2012‐2015 | 2019 | Gratix 52 |
Only remand centers were included in this study (people awaiting trial or awaiting sentencing).
Due to short sentences and high numbers of intakes and releases, continuity of care on release to the community should be prioritized. For example, the average length of stay is 59 days among sentenced PWAI in British Columbia Provincial Corrections, with 37,000 intakes and releases per year. 15 However, due to competing priorities at release, and the absence of systematic discharge planning and services such as patient navigation, linkage to care remains a major challenge. Continuity of care on release is a major challenge globally, with calls to streamline provision of health care in corrections with health care in the community. 16 As a result, several Canadian provinces have transferred the responsibility for the provision of health care from corrections authorities to local health authorities. In provinces where this has occurred, improvements in health care have been reported. 15 , 17 , 18 Transfer of responsibility for health care to health authorities in other jurisdictions could assist in streamlining the provision of HCV screening, treatment, and retention in care after release.
Most provincial/territorial correctional centers across Canada offer risk‐based or opt‐in HCV screening, although Alberta recently implemented universal sexually transmitted and blood‐borne infection (STBBI) screening on entrance to remand centers. 19 Furthermore, HCV treatment is offered in provincial/territorial corrections; however, depending on the province/territory, restrictions such as advanced fibrosis/cirrhosis and sentence length exist. 20 , 21 Fibrosis stage eligibility restrictions were deemed an infringement on human rights in federal corrections; however, because of jurisdictional and funding issues, the lifting of this restriction has not yet occurred in all provinces and territories. These restrictions must all be removed before HCV elimination in Canada is possible. Further, unlike in federal correctional institutions, sterile injection equipment is not available; therefore, PWAI who inject drugs in these centers must share drug use equipment and consume drugs in ways that increase the risk for harm. This increases their risk for acquiring and transmitting HCV (both primary and reinfection), further concentrating the epidemic among PWAI and undermining HCV elimination efforts. 2 , 22 Until best practices for HCV prevention, screening, and treatment can be modeled after federal corrections, HCV care to PWAI in provincial/territorial corrections will lag behind.
Evidence Supporting HCV Treatment Scale‐Up in Correctional Settings
Several studies have demonstrated that scaling up HCV testing and treatment in correctional settings, or “microelimination” approaches, can reduce HCV transmission among PWID, both in prisons and the community, 23 , 24 , 25 and are demonstrated to be cost‐effective. 26 , 27 , 28 “Treat all” approaches aiming to achieve microelimination of HCV infection in correctional settings are feasible, as demonstrated in Australian prisons, 29 , 30 the United States, 31 and Spain. 32 Because screening is the first step in HCV care, increasing uptake is crucial to improving care pathways for PWAI and may positively impact transition into the community 33 ; therefore, universal STBBI screening at intake should be implemented, as has been done by CSC and in Alberta. Point‐of‐care 34 , 35 or dried blood spot 11 testing could facilitate universal HCV testing strategies among PWAI. To increase overall HCV care of PWAI, responsibility for the provision of health care in correctional centers should be transferred to local health authorities, as has now been done in several Canadian provinces. To further optimize treatment uptake and linkage to care, scale‐up of evidence‐based interventions is needed in provincial and territorial corrections. These include telemedicine, 10 , 36 team‐based care, 36 and peer support and education programs. 37 Finally, mobile phone‐based applications and text messaging, also known as mHealth, 38 have been shown to increase HIV treatment adherence among PWAI released to the community and could improve linkage to HCV care after release. 34 “Prison health is public health” 3 , 22 , 39 and efforts to reduce the burden of HCV among PWAI will undoubtedly also reduce its prevalence in the community. It is unlikely that global initiatives such as the elimination of viral hepatitis by 2030 will be achieved while the standard of HCV care available in prisons remains low.
Potential conflict of interest: S.R.B. advises and is on the speakers’ bureau for Gilead. N.K. consults for, advises, is on the speakers’ bureau for, and received grants from Gilead, and consults for and advises ViiV Healthcare and Merck.
References
- 1. Degenhardt L, Peacock A, Colledge S, et al. Global prevalence of injecting drug use and sociodemographic characteristics and prevalence of HIV, HBV, and HCV in people who inject drugs: a multistage systematic review. Lancet Global Health 2017;5:e1192‐e1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Stone J, Fraser H, Lim AG, et al. Incarceration history and risk of HIV and hepatitis C virus acquisition among people who inject drugs: a systematic review and meta‐analysis. Lancet Infect Dis 2018;18:1397‐1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kouyoumdjian F, Schuler A, Matheson FI, et al. Health status of prisoners in Canada: narrative review. Can Fam Physician 2016;62:215‐222. [PMC free article] [PubMed] [Google Scholar]
- 4. Canadian Network on Hepatitis C Blueprint Writing Committee and Working Groups . Blueprint to Inform Hepatitis C Elimination Efforts in Canada. Montreal: Canadian Network on Hepatitis C; 2019. Available at: https://www.canhepc.ca/sites/default/files/media/documents/blueprint_hcv_2019_05.pdf. Published May 2019.
- 5. Statistics Canada . Table 35‐10‐0015‐01 Adult custody admissions to correctional services by sex. Available at: 10.25318/3510001501-eng. Published 2019. [DOI]
- 6. Correctional Service Canada . Infectious Disease Surveillance 2014 Hepatitis C Virus (HCV). Available at: https://www.csc-scc.gc.ca/publications/092/005007-3038-eng.pdf. Published September 2016.
- 7. Public Health Agency of Canada . Summary: Estimates of HIV Incidence, Prevalence and Proportion Undiagnosed in Canada, 2014. Available at: https://www.catie.ca/ga-pdf.php?file=sites/default/files/2014-HIV-Estimates-in-Canada-EN.pdf. Published November 2015.
- 8. Correctional Service Canada . Hepatitis C Virus (HCV) Age, Gender and Indigenous Ancestry. Available at: https://www.csc-scc.gc.ca/publications/092/005007-3037-eng.pdf. Published September 2016.
- 9. Correctional Service Canada . Hepatitis C Virus (HCV) Repeat Testing and Seroconversion, 2016. Available at: https://www.csc-scc.gc.ca/publications/092/005007-3039-eng.pdf. Published September 2016.
- 10. Morey S, Hamoodi A, Jones D, et al. Increased diagnosis and treatment of hepatitis C in prison by universal offer of testing and use of telemedicine. J Viral Hepat 2019;26:101‐108. [DOI] [PubMed] [Google Scholar]
- 11. Arif T. Hepatitis service provision at HMP birmingham: progressing a previous service improvement plan. BMJ Open Qual 2018;7:e000192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kronfli N, Linthwaite B, Kouyoumdjian F, et al. Interventions to increase testing, linkage to care and treatment of hepatitis C virus (HCV) infection among people in prisons: A systematic review. Int J Drug Policy 2018;57:95‐103. [DOI] [PubMed] [Google Scholar]
- 13. Correctional Service Canada . The Prison Needle Exchange Program. Available at: https://www.csc-scc.gc.ca/health/002006-2004-en.shtml. Updated August 28, 2019.
- 14. Correctional Service Canada . The Overdose Prevention Service. Available at: https://www.csc-scc.gc.ca/health/002006-2002-en.shtml. Updated August 28, 2019.
- 15. Pelletier L, MacFarlane A, Sharifi N. Correctional Health Services: Transition to the Provincial Health Services Authority. Available at: https://cchl-ccls.ca/uploaded/web/BCHLC_2018/presentations/BCHLC2018_Pelletier-MacFarlane-Sharif.pdf. Updated October 25, 2018.
- 16. McCall‐Smith K. United Nations standard minimum rules for the treatment of prisoners (Nelson Mandela Rules). Int Legal Mater 2017;55:1180‐1205. [Google Scholar]
- 17. Webster PC. Integrating prison health care into public health care: the global view. Can Med Assoc J 2013;185:E283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Albetra Health Services . Improving Health Behind Bars. Available at: https://www.albertahealthservices.ca/careers/Page12889.aspx. Published June 19, 2017.
- 19. Gratrix J, Payne D, Smyczek P, et al. P015 Introduction of chlamydia and gonorrhea opt‐out testing in a short‐term correctional facility in Alberta, Canada. Sex Transm Infect 2019;95(Suppl. 1):A88. [Google Scholar]
- 20. Kronfli N, Buxton JA, Jennings L, et al. Hepatitis C virus (HCV) care in Canadian correctional facilities: where are we and where do we need to be? Can Liver J 2019;2:171‐183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kronfli N, Cox J. Care for people with hepatitis C in provincial and territorial prisons. Can Med Assoc J 2018;190:E93‐E94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kamarulzaman A, Reid SE, Schwitters A, et al. Prevention of transmission of HIV, hepatitis B virus, hepatitis C virus, and tuberculosis in prisoners. Lancet 2016;388:1115‐1126. [DOI] [PubMed] [Google Scholar]
- 23. Girardin F, Hearmon N, Castro E, et al. Modelling the impact and cost‐effectiveness of extended hepatitis C virus screening and treatment with direct‐acting antivirals in a swiss custodial setting. Clin Infect Dis 2019;69:1980‐1986. [DOI] [PubMed] [Google Scholar]
- 24. He T, Li K, Roberts MS, et al. Prevention of hepatitis C by screening and treatment in U.S. prisons. Ann Intern Med 2016;164:84‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Godin A, Kronfli N, Cox J, et al. The role of prison‐based interventions for hepatitis C virus (HCV) micro‐elimination among people who inject drugs in Montréal, Canada. Int J Drug Policy 2020;2020:102738. [DOI] [PubMed] [Google Scholar]
- 26. Dalgic OO, Samur S, Spaulding AC, et al. Improved health outcomes from hepatitis C Treatment scale‐up in Spain’s prisons: a cost‐effectiveness study. Sci Rep 2019;9:16849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Chen CP, Cheng CY, Zou H, et al. Evaluation of cost‐effectiveness of peginterferon plus ribavirin for chronic hepatitis C treatment and direct‐acting antiviral agents among HIV‐infected patients in the prison and community settings. J Microbiol Immunol Infect 2019;52:556‐562. [DOI] [PubMed] [Google Scholar]
- 28. Assoumou SA, Tasillo A, Vellozzi C, et al. Cost‐effectiveness and budgetary impact of hepatitis C virus testing, treatment, and linkage to care in US prisons. Clin Infect Dis 2019;70:1388‐1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bartlett SR, Fox P, Cabatingan H, et al. Demonstration of near‐elimination of hepatitis C virus among a prison population: The lotus glen correctional centre hepatitis C treatment project. Clin Infect Dis 2018;67:460‐463. [DOI] [PubMed] [Google Scholar]
- 30. Blogg J, Wood J, McGrath C, et al. Eradicating hepatitis C from the New South Wales prison system. Med J Aust 2018;208:276. [DOI] [PubMed] [Google Scholar]
- 31. Mazur WP. Management of hepatitis C in delaware prisons: approaching micro‐environmental eradication. Delaware J Public Health 2019;5:article 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Marco A, Guerrero RA, Turu E, et al. Is it possible to eliminate hepatitis C from the prisons of Catalonia, Spain, in 2021? Rev Esp Sanid Penit 2019;21:38‐41. [PMC free article] [PubMed] [Google Scholar]
- 33. Janssen PA, Korchinski M, Desmarais SL, et al. Factors that support successful transition to the community among women leaving prison in British Columbia: a prospective cohort study using participatory action research. CMAJ Open 2017;5:e717‐e723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Yanes‐Lane M, Dussault C, Linthwaite B, et al. Using the barriers and facilitators to linkage to HIV care to inform hepatitis C virus (HCV) linkage to care strategies for people released from prison: findings from a systematic review. J Viral Hepat 2020;27:205‐220. [DOI] [PubMed] [Google Scholar]
- 35. Sharafi H, Poustchi H, Azimian F, et al. Performance of a rapid diagnostic test for screening of hepatitis C in a real‐life prison setting. J Clin Virol 2019;113:20‐23. [DOI] [PubMed] [Google Scholar]
- 36. Papaluca T, McDonald L, Craigie A, et al. Outcomes of treatment for hepatitis C in prisoners using a nurse‐led, state‐wide model of care. J Hepatol 2019;70:839‐846. [DOI] [PubMed] [Google Scholar]
- 37. Thornton K, Sedillo ML, Kalishman S, et al. The New Mexico Peer Education Project: filling a critical gap in HCV prison education. J Health Care Poor Underserved 2018;29:1544‐1557. [DOI] [PubMed] [Google Scholar]
- 38. Tofighi B, Hein P, Carvalho AMS, et al. Technology preferences to enhance HIV and HCV care among patients with substance use disorders. J Addict Dis 2018;37:157‐159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. McLeod KE, Martin RE. Health in correctional facilities is health in our communities. CMAJ 2018;190:e274‐e275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Préfontaine R, Chaudhary R, Mathias R. Analysis of risk factors associated with hepatitis B and C infection in correctional institutions in British Columbia. Can J Infect Dis 1994;5:153‐156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Pearson M, Mistry PS, Ford PM. Voluntary screening for hepatitis C in a Canadian federal penitentiary for men. Can Commun Dis Rep 1995;21:134‐136. [PubMed] [Google Scholar]
- 42. Ford PM, White C, Kaufmann H, et al. Voluntary anonymous linked study of the prevalence of HIV infection and hepatitis C among inmates in a Canadian federal penitentiary for women. CMAJ 1995;153:1605‐1609. [PMC free article] [PubMed] [Google Scholar]
- 43. Ford PM, Pearson M, Sankar‐Mistry P, et al. HIV, hepatitis C and risk behaviour in a Canadian medium‐security federal penitentiary. QJM 2000;93:113‐119. [DOI] [PubMed] [Google Scholar]
- 44. De P, Connor N, Bouchard F, et al. HIV and Hepatitis C virus testing and seropositivity rates in Canadian federal penitentiaries: a critical opportunity for care and prevention. Can J Infect Dis Med Microbiol 2004;15:695483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Poulin C, Alary M, Lambert G, et al. Prevalence of HIV and hepatitis C virus infections among inmates of Quebec provincial prisons. CMAJ 2007;177:252‐256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Calzavara L, Ramuscak N, Burchell AN, et al. Prevalence of HIV and hepatitis C virus infections among inmates of Ontario remand facilities. CMAJ 2007;177:257‐261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Remis RS. Modelling the incidence and prevalence of hepatitis c infection and its sequelae in Canada, 2007. Public Health Agency of Canada. Available at: https://www.canada.ca/content/dam/phac-aspc/migration/phac-aspc/sti-its-surv-epi/model/pdf/model07-eng.pdf. [Google Scholar]
- 48. Trubnikov M, Yan P, Archibald C. Estimated prevalence of hepatitis C Virus infection in Canada, 2011. Can Commun Dis Rep 2014;40:429‐436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Hodge KR, Ross C. STBBI Evaluation Report—Winnipeg Remand Centre. Available at: https://professionals.wrha.mb.ca/old/extranet/publichealth/files/services/healthy-sexuality/WRCEvaluationReport.pdf. Published April 2014.
- 50. Courtemanche Y, Poulin C, Serhir B, et al. HIV and hepatitis C virus infections in Quebec's provincial detention centres: comparing prevalence and related risky behaviours between 2003 and 2014‐2015. Can J Public Health 2018;109:353‐361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Kronfli N, Dussault C, Klein MB, et al. The hepatitis C virus cascade of care in a Quebec provincial prison: a retrospective cohort study. CMAJ Open 2019;7:E674‐E679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Gratrix J, Smyczek P, Bertholet L, et al. A cross‐sectional evaluation of opt‐in testing for sexually transmitted and blood‐borne infections in three Canadian provincial correctional facilities: a missed opportunity for public health? Int J Prisoner Health 2019;15:273‐281. [DOI] [PubMed] [Google Scholar]


