Watch a video presentation of this article
Abbreviations
- AASLD
American Association for the Study of Liver Diseases
- AIH
autoimmune hepatitis
- ALT
alanine aminotransferase
- AST
aspartate aminotransferase
- AZA
azathioprine
- DEXA
dual energy X‐ray absorptiometry
- IgG
immunoglobulin G
- MMF
mycophenolate mofetil
- SMA
smooth muscle antibody
T`his article will summarize practice guidance/guidelines put forth by the American Association for the Study of Liver Diseases (AASLD) in an easy‐to‐read format for patients and their caregivers. The difference between guidance and guidelines is that guidelines are supported by very strong evidence, such as large randomized trials, whereas guidance statements are supported by smaller studies and expert opinion. This summary will hopefully help patients better understand their condition, but it should not replace expert medical care. The full document is available online at: https://aasldpubs.onlinelibrary.wiley.com/doi/10.1002/hep.31065. 1
Autoimmune Hepatitis
Autoimmune hepatitis (AIH) is a condition where the body’s immune system attacks the liver by mistake (Fig. 1). This immune attack leads to inflammation in the liver, which can eventually lead to damage, such as cirrhosis and liver failure. However, there are treatments that can prevent this damage in most cases.
FIG 1.
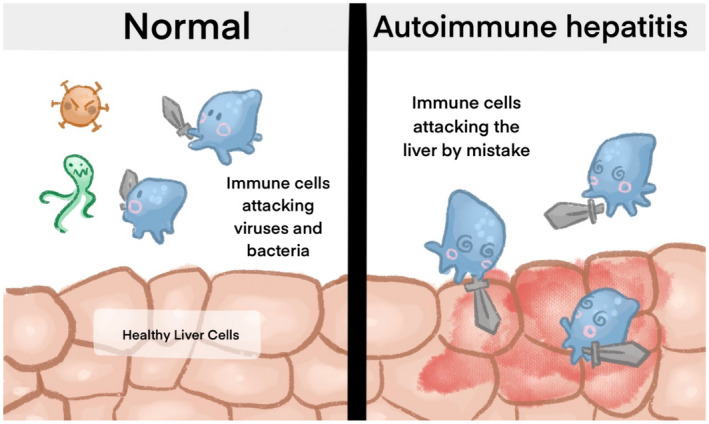
Mechanism of Autoimmune Hepatitis. Courtesy Aria Puri.
Diagnosis
Guidance statement: The diagnosis of AIH requires compatible histological findings and is further supported by the following features: (1) elevated serum aminotransaminase levels; (2) elevated serum immunoglobulin G (IgG) level and/or positive serological marker(s); (3) exclusion of viral, hereditary, metabolic, cholestatic, and drug‐induced diseases that may resemble AIH.
Patient summary: AIH is diagnosed in patients with elevated liver blood tests (aspartate aminotransferase [AST] and alanine aminotransferase [ALT]), positive autoantibodies in the blood (IgG level, antinuclear antibody, smooth muscle antibody [SMA]), other liver diseases ruled out (such as hepatitis B and C), and typical findings on liver biopsy. There is no single test to make the diagnosis but rather a combination of tests. Twenty percent (one in five cases) of patients with AIH do not have any autoantibodies. Figure 2 shows how AIH is diagnosed.
FIG 2.
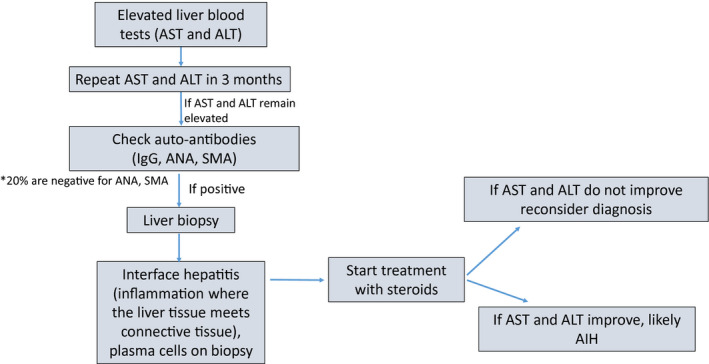
Approach to diagnosing AIH in adults.
Key Point: AIH should not be diagnosed without liver biopsy.
Treatment
Guidelines: For children and adults who present with AIH who do not have cirrhosis or acute severe AIH, the AASLD suggests as initial first‐line treatment budesonide and azathioprine (AZA) or prednisone/prednisolone and AZA. For children and adults with AIH who have cirrhosis or who present with acute severe AIH, the AASLD suggests that budesonide not be used.
Patient summary: Initial treatment of AIH is with steroids (prednisone or budesonide) and AZA. Budesonide is great because it works like prednisone on the AIH, but most patients do not experience all the steroid side effects (weight gain, puffy face, thin bones, etc.). However, budesonide cannot be used in patients with cirrhosis or acute severe AIH.
Key Point: Ask your doctor if budesonide is an option for you, to help minimize side effects!
Guidelines: In children or adults with AIH who experience treatment failure, incomplete response, or drug intolerance to first‐line agents, the AASLD suggests the use of mycophenolate mofetil (MMF) or tacrolimus to achieve and maintain biochemical remission. Based on a superior ease of use and side‐effect profile, the AASLD suggests a trial of MMF over tacrolimus as the initial second‐line agent in patients with AIH.
Patient summary: Most patients with AIH respond well to steroids and AZA, with the liver blood tests becoming normal within several months. However, in some patients, the inflammation is more difficult to treat. In these cases, mycophenolate is usually tried next and then tacrolimus. Figure 3 shows the different drugs and investigational treatments used to treat AIH.
FIG 3.
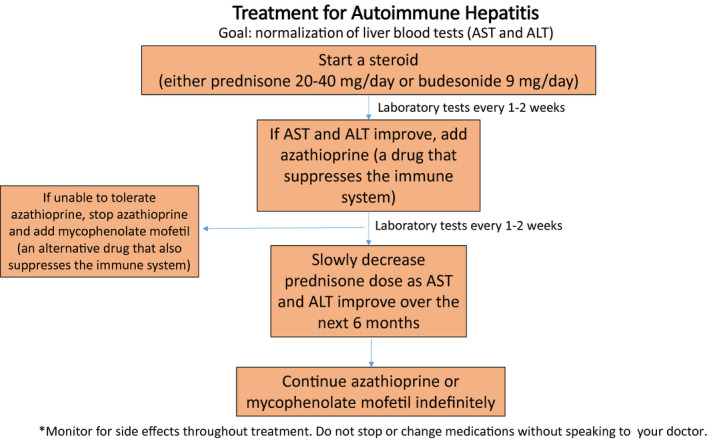
Treatment for AIH.
Key Point: If your disease does not get under control right away, do not give up!
Guidance statements:
Drug withdrawal and achievement of a long‐term treatment‐free remission of AIH are possible in a minority of patients and should be considered in patients who have normalized serum aminotransferase and IgG levels for at least 2 years.
Liver tissue examination prior to drug withdrawal is valuable in excluding unsuspected inflammation and reducing the frequency of relapse, but it is not mandatory in adults.
Patients must be closely monitored for relapse with regular laboratory assessments during the first 12 months after treatment withdrawal and annually thereafter to cover for lifelong risk.
Relapse requires prompt reinstitution of the original treatment until biochemical remission and subsequent transition to a long‐term maintenance regimen.
Patient summary: The goal of treatment is to eliminate the inflammation, which means normal liver blood tests (AST and ALT) and normal IgG level. Some, but not all, patients can get off of medications completely and still have normal liver blood tests. The chances for success are higher if the enzymes and IgG are normal for 2 years first. Sometimes repeat liver biopsy is helpful, but it is not always required. Liver biopsy is usually done if the liver enzymes do not normalize, or to look for other causes, such as fatty liver. Up to 80% of patients will have their immune disease become active after medications are stopped ( Fig. 4 ). It is not easy to predict when this will occur, although it often happens in the first year. Because it could occur months to years after treatment has been stopped, liver blood tests to check for relapse must be done at regular intervals forever.
FIG 4.
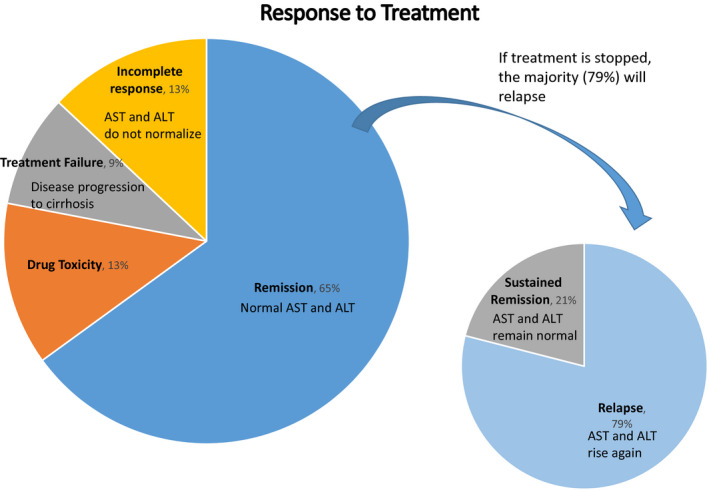
Response to AIH treatment. Reproduced with permission from GI/Liver Secrets Plus. 2 Copyright 2010, Mosby Elsevier.
Key Point: Do not stop medications too soon! Treatment is given for at least 2 years before it is possible to stop. Autoimmune disease is not curable and must be monitored even if medications are not needed.
Health Maintenance
Guidance statements: Bone mineral densitometry should be performed at baseline in all adult patients with AIH who have risk factors for osteoporosis, and it should be repeated every 2‐3 years of continuous glucocorticoid treatment. Serum levels of 25‐hydroxyvitamin D should be determined at diagnosis and annually thereafter.
Patients with AIH should be screened for celiac disease and thyroid disease at diagnosis.
Vaccines should be administered to all susceptible patients with AIH according to Centers for Disease Control and Prevention guidelines.
Patient summary: Patients with AIH are at increased risk for osteoporosis (thin bones) and should be screened with dual energy X‐ray absorptiometry (DEXA; bone density) scans and vitamin D levels.
Patients with AIH often have other autoimmune conditions. Autoimmune thyroid disease is the most common additional immune problem.
Vaccines are important to protect patients with AIH from other infections, especially hepatitis A and hepatitis B.
Key Point: Do not forget about bone health! Look for other immune conditions, especially if there are symptoms. Table 1 is a summary of other medical conditions that should be monitored if you are diagnosed with AIH.
TABLE 1.
Other Medical Conditions To Be Monitored if You Are Diagnosed With AIH
| Possible Condition | Preventative Actions |
|---|---|
| Increased risk for thin bones (osteoporosis) | DEXA scan, vitamin D levels |
| Increased risk for infection | Vaccinations, especially hepatitis A and B |
| Increased risk for other autoimmune disease | Check thyroid test |
Pregnancy
Guidance statements: Family planning should include the goal of achieving biochemical remission of AIH for 1 year prior to conception.
Women of reproductive potential should receive prenatal counseling on the significant adverse effects of active AIH on pregnancy and the risk for flares during and after pregnancy. Maintenance doses of glucocorticoids and/or AZA should be continued throughout pregnancy.
MMF is contraindicated during pregnancy, and women should be counseled about the adverse effects of MMF on pregnancy prior to initiating MMF treatment.
Women with cirrhosis who are pregnant or plan to become pregnant within the next year should be screened for varices by endoscopy either prior to conception or during the second trimester of gestation and treated with band ligation.
Patient summary: Women with AIH should have their disease under control ideally for a year before becoming pregnant. Most of the medications are safe during pregnancy, and it is actually higher risk to the baby if AIH becomes active, so it is important to continue the medications. However, MMF should not be used during pregnancy. Women who have advanced liver disease, such as cirrhosis, are at extra risk and should be evaluated for varices (dilated veins in the esophagus, which can burst and bleed) ( Fig. 5 ).
FIG 5.

Pregnancy with Autoimmune Hepatitis. Courtesy Aria Puri.
Key Point: Talk to your doctor before becoming pregnant!
Potential conflict of interest: M.V. consults for Salix, Biovie, and Natera.
References
- 1. Mack CL, Adams D, Assis DN, et al. Diagnosis and Management of Autoimmune Hepatitis in Adults and Children: 2019 Practice Guidance and Guidelines From the American Association for the Study of Liver Diseases. Hepatology 2020;72:671‐722. [DOI] [PubMed] [Google Scholar]
- 2. Czaja AJ. Autoimmune hepatitis: treatment. In: McNally PR, ed. GI/Liver Secrets Plus. Philadelphia: Mosby Elsevier; 2010. [Google Scholar]


