Abstract
Case series
Patients: Male, 31-year-old • Male, 70-year-old
Final Diagnosis: Extra-peritoneal foreign bodies
Symptoms: Abdominal pain and fever
Medication: —
Clinical Procedure: Mini-percutaneous nephrolithotomy
Specialty: Radiology
Objective:
Unusual setting of medical care
Background:
Foreign bodies (FBs) in the intra- or extra-peritoneal cavity are relatively rare. The aim of treatment is to remove the FB to prevent chronic inflammation and/or infection. Traditionally, surgical management is necessary, as the detection and localization of FBs can be difficult. Mini-percutaneous nephrolithotomy (Mini-PCNL) under the guidance of ultrasonography (US-guided) has recently been used as an alternative to conventional therapeutic options for FB removal.
Case Reports:
In this article, we report the cases of 2 patients with an extra-peritoneal wooden toothpick FB treated using the mini-percutaneous nephrolithotomy technique as an effective treatment for removing the FBs. These patients recovered quickly and were discharged uneventfully.
Conclusions:
Using ultrasound to guide mini-PCNL represents a potential alternative to laparoscopic surgery for the detection and removal of FBs, allowing the patient to recover quickly. This approach is simple, minimally invasive, and feasible under local anesthesia and should be considered as an alternative to surgery.
Keywords: Case Reports; Foreign Bodies; Radiology, Interventional
Background
Foreign bodies (FBs) in either the intra- or extra-peritoneal cavity are exceedingly rare. Commonly ingested FBs include fish bones, coins, and toothpicks. An ingested toothpick is a sharp object that could cause the perforation of the digestive tract at various locations. During migration, toothpicks are most commonly found in the stomach and duodenum, and toothpicks have been reported to appear in the retroperitoneal cavity in approximately 10% of cases [1]. The most common treatment options include open surgery and laparoscopic surgery [1–3]. Başıbüyük et al [4] reported the first case using a nephoscope to remove a retroperitoneal FB. In this paper, we aimed to report 2 patients with FBs and describe the use of mini-percutaneous nephrolithotomy (Mini-PCNL) under the guidance of ultrasonography (US-guided) as an alternative to conventional therapeutic options for FB removal.
Case Reports
Case 1
The first patient was a 31-year-old man with no history of mental disorders. He had a habit of using toothpicks but did not realize or remember that he had swallowed one. The patient presented with localized abdominal pain and fever. Clinical examination confirmed localized abdominal guarding, and laboratory investigations showed an elevated white blood cell count (WBC, 12.03 G/l, 77.2% were neutrophils). On computed tomography (CT) scan, 2 adjacent thin hyperdensity FBs (11 mm and 21 mm in length, respectively) were identified between the ascending colon and the right abdominal wall (Figure 1A, 1B). Associated fat stranding was observed around the FBs, but no free air or fluid was observed.
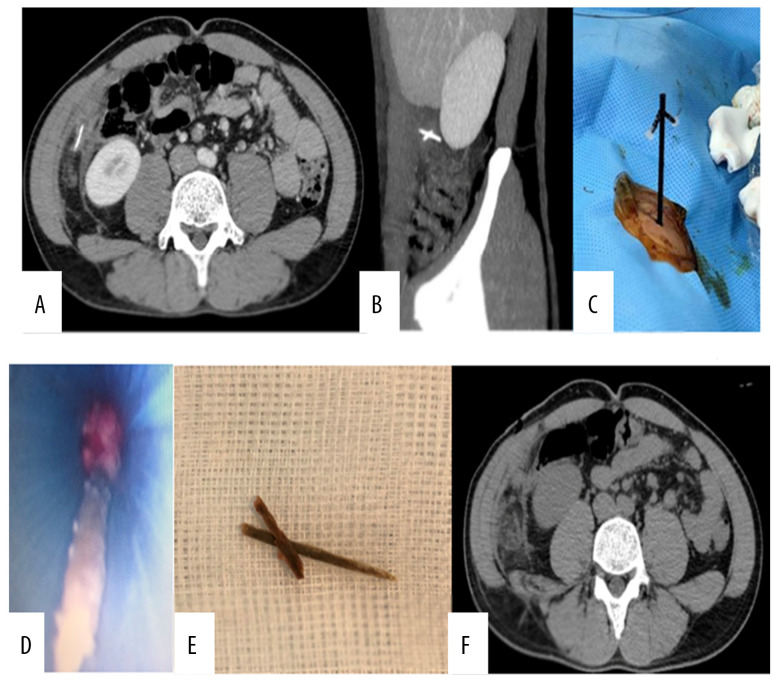
Figure 1.
(A, B) Abdominal CT scan before the intervention. The FBs appeared as hyperdensity lesions, located adjacent to each other and between the ascending colon and the right abdominal wall. (C) A plastic 14-F port was used to approach the FBs under the guidance of ultrasonography. (D) The FBs were removed through the port. (E) The FBs were 2 pieces of a wooden toothpick (11 and 21 mm). (F) The patient’s post-intervention abdominal CT scan showed that the FBs had been completely removed.
The interventional radiologists performed the ultrasound-guided mini-PCNL technique because the small FB could be removed through a 14-French (F) plastic port (Figure 1C) (Percutaneous nephrostomy set, Seplou Medical, USA). According to our hospital’s guideline, local anesthesia was initially chosen for ultra-sound-guided mini-PCNL. After administering 10 ml of diluted lidocaine (2%) (Egis Pharmaceuticals Public Ltd. Co., Hungary), a 16-G×20 cm angiocath needle (Becton Dickinson Infusion Therapy Systems Inc., USA) was inserted near the FB under the guidance of ultrasonography. Then, a 0.035-inch super stiff guide wire (Terumo Medical Corp., USA) was inserted into the lumen of the angiocath sheath. We generated a tunnel using a 14-F dilator. Later, the 14-F port was passed over the wire. Finally, we used a of 9.5-F nephroscope (Kalz Storz NDTec, Germany) to find the FB under the guidance of real-time ultrasonography. A blood pressure bandage, pumped up to 150 mmHg, was wrapped around a saline bottle, and the fluid was infused through the channel of the nephroscope and escaped from the affected area through the gap between the nephroscope and the port. The FBs were removed by using forceps (Karl Storz, Germany) inserted into the channel of the nephroscope. The FBs retrieved were 2 different-sized pieces of a wooden toothpick (Figure 1D, 1E). The patient made an excellent recovery. The CT scan on day 5 after the procedure showed no residual FBs and no collected fluids or abscess (Figure 1F). The patient took 1 g IV q12h of ceftriaxone (Pfizer, USA) and 500 mg IV q12h of metronidazole (Pfizer, USA) 1 day before and 6 days after the treatment. He was then discharged home without any complications.
Case 2
The second patient was a 70-year-old man with a history of appendectomy. One week prior to hospitalization, he developed sudden abdominal pain in his right flank, accompanied by a mild fever. His laboratory findings showed an elevated WBC of 12.37 G/L, with 78.6% neutrophils. Ultrasonography and CT scan noted a thin and straight FB (60 mm in length) behind the ascending colon, protruding into the retroperitoneum space (Figure 2A, 2B), surrounded by a 30×47 mm abscess. No free intraperitoneal air/fluid was noted. Colon endoscopy found no abnormalities. Because the FB was very thin, we decided to use the mini-PCNL technique to remove it.
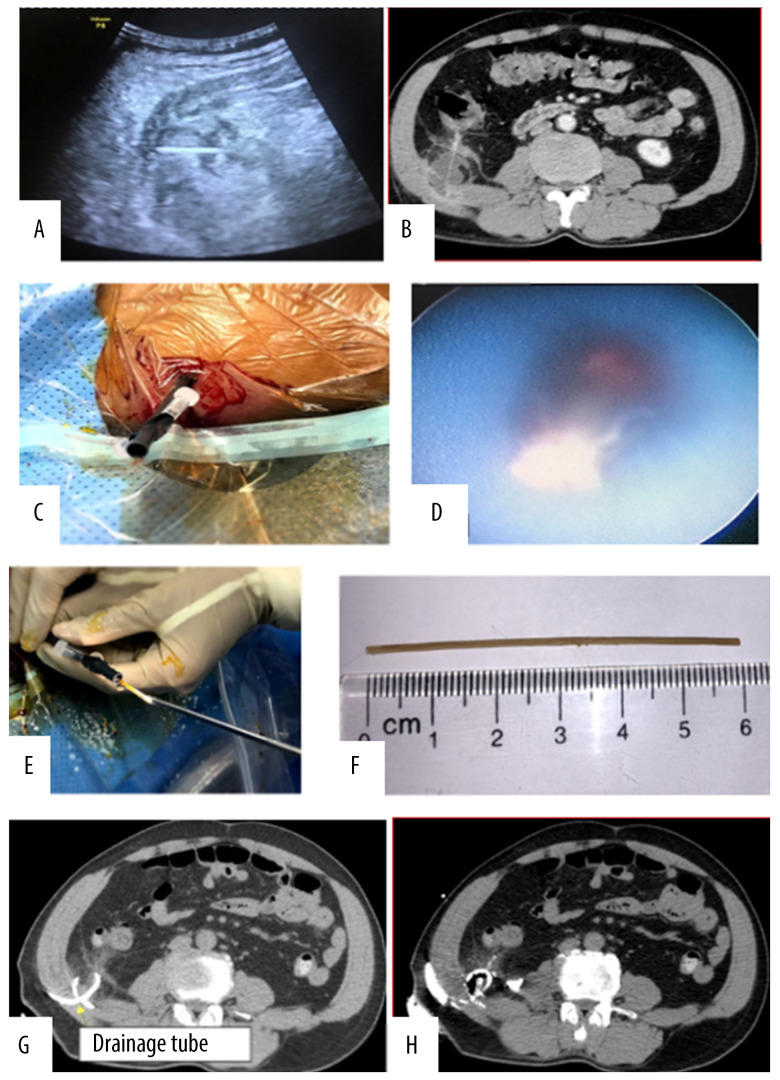
Figure 2.
(A, B) Abdominal ultrasound image and CT scan showing a small abscess surrounding the FB. (C) A 14-F Amplatz was used to approach the FB. (D, E) The FB was removed through the Amplatz. (F) The FB was a bamboo toothpick, 60 mm in length. (G, H) CT scans showed that after the intervention, a slight inflammatory infiltration remained near the drainage tube, with no indication of contrast agent passing into the peritoneal cavity or colon.
Initially, the abscess was drained under the guidance of ultrasonography, using an 8-F pigtail catheter (Biotech Corp, Taiwan). Twenty-two hours later, the ultrasonographer had confirmed that the pus was completely removed, and we decided to dilate the tract by replacing the previous drain with a 14-F dilator and a 14-F port (Figure 2C) with the same steps described in the first case. The FB was removed using 9.5-F nephroscope and forceps with ultrasonographic guidance (Figure 2D, 2E). Finally, an 8-F drain was reinserted into the affected area. A bamboo toothpick, as observed in the CT scan, was removed within 30 min of the interventional procedure (Figure 2F). The follow-up axial abdominal CT with contrast enhancement via the 8-F drain at 1 day after treatment showed an improvement in the abscess, with no indication of the contrast agent passing from the peritoneal cavity into the right colon (Figure 2G, 2H). The patient took 1g IV q12h of Ceftriaxone (Pfizer, USA) and 500 mg IV q12h of Flagyl (Pfizer, USA) 1 day before and 6 days after the treatment. The drain was removed and the patient was discharged on the seventh day without any adverse events.
Discussion
FBs can be divided into 2 groups. The first group includes small FBs (<3 mm), such as broken sewing needles, bamboo toothpicks, uterine contraceptive devices, and small shrapnel. The second group includes larger FBs, such as larger shrapnel, inadvertently remaining surgical instruments, swabs, and trauma-related FBs. FBs can enter the body through several possible routes [5]: direct routs (via the skin, mucosa, and sclera), swallowing (accidental or on purpose), iatrogenic (post-procedure/operation), or through the vagina. In both of our cases, the FBs were toothpicks that punctured the right colon and migrated from the right colon to the adjacent retroperitoneal cavity. Compared with other positions in the digestive tract, the colon has the thinnest-walled structure, making it easy to puncture. The right and left colon are located in the posterior peritoneal cavity, allowing the FB to enter this compartment, as described in a previous case report [6].
Treatment options for FB removal include open surgery and laparoscopic surgery [1], which is a minimally invasive technique that is sometimes used to remove FBs, either with or without the aid of radiological modalities [4]. Use of laparoscopy has been increasingly described, with the use of a rigid or flexible optic endoscope [7–9]. However, mini-PCNL is a less invasive method, using a port size ranging from 14 F to 18 F (approximately 4.5 to 6 mm), which is smaller than that required for open surgery and laparoscopy with 1 or more trocar ports (10 mm) [4,8]. In 2009, Kurita et al [9] designed a new laparoscopic system for the removal of an FB in the pelvic cavity through a single 5-mm port using a flexible cholangioscope.
Because the FB was in the peritoneal cavity, they used a closed port, which does not allow air to escape. Nevertheless, saline was utilized to create an endoscopic environment in our cases and we also chose to use an open port, which can allow liquids to continuously drain out. The port size of 14 F was sufficient to collect objects found in the urinary tract when using the mini-PCNL technique, such as a JJ stent or small kidney stones; therefore, it can be applied to the removal of FBs, such as the toothpicks in these cases.
Some authors have used only ultrasound to guide the process of removing shallow objects under the skin in the limbs and fingers [10,11]. However, this procedure is difficult to implement with deeply located objects. Therefore, we combined ultrasound with endoscopy to locate the FB. The success or failure of this technique is determined by whether the FB is accessible. We used ultrasound to guide the placement of the port’s tip until it made contact with the FB, which made the process of identifying the FB easier. Ultrasonography can provide real-time imaging and be used to detect FBs, whereas endoscopy helps to pinpoint the location of anomalies during removal. Ultrasound can also be useful during hydro-dissection techniques to separate the FB from surrounding organs, making it easier to remove [11].
In normal laparoscopic techniques, a gas environment used, making ultrasound not supportable [4]. The use of a water environment during the mini-PCNL technique allowed the ultra-sound to easily identify the lesion and orient the endoscope in real time. Furthermore, saline washes out blood, and performs better in distinguishing between the FB and the surrounding soft tissue compared with the use of CO2, as reported previously [4].
In the second case, the FB appeared within an associated abscess; thus, a drain needed to be placed. Because no air bubbles were identified around the object or in the abscess, in both cases, the likelihood of colon perforation was determined to be low. We injected a contrast agent into this area through an 8-F pigtail drain after the treatment and performed a CT scan to assess fistula formation, which was not observed. The patient experienced complete recovery without a recurrent abscess. The use of low water pressure and constant drainage may also help prevent the abscess spreading into the surrounding tissues, but further studies must be performed to determine the effectiveness of this technique.
Another advantage of the mini-PCNL technique under ultra-sound guidance is that it provides a quick, minimally invasive option for the removal of FBs in difficult locations that can be accessed under imaging guidance [10,12–14]. The disadvantage of this technique is that larger FBs (larger than the port diameter) cannot be removed. The technique may also be limited in patients who have diffuse and/or acute peritonitis, as the fluid injected into the peritoneal cavity could aggravate inflammation.
Conclusions
We described the successful removal of toothpicks from the retroperitoneal cavity using mini-PCNL in 2 patients. Using ultrasound to guide mini-PCNL represents a potential alternative to laparoscopic surgery for the detection and removal of FBs, allowing the patient to recover quickly.
Footnotes
Conflict of Interests
None.
References:
- 1.Steinbach C, Stockmann M, Jara M, et al. Accidentally ingested toothpicks causing severe gastrointestinal injury: A practical guideline for diagnosis and therapy based on 136 case reports. World J Surg. 2014;38:371–77. doi: 10.1007/s00268-013-2307-z. [DOI] [PubMed] [Google Scholar]
- 2.Sarici IS, Topuz O, Sevim Y, et al. Endoscopic management of colonic perforation due to ingestion of a wooden toothpick. Am J Case Rep. 2017;18:72–75. doi: 10.12659/AJCR.902004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guelfguat M, Kaplinskiy V, Reddy SH, et al. Clinical guidelines for imaging and reporting ingested foreign bodies. Am J Roentgenol. 2014;203:37–53. doi: 10.2214/AJR.13.12185. [DOI] [PubMed] [Google Scholar]
- 4.Başıbüyük İ, Tosun M, Kalkan S, et al. Removal of a retroperitoneal foreign body through single port laparoscopy using nephroscope. Turk J Urol. 2017;43:386–89. doi: 10.5152/tud.2017.14306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fujiwara T, Mitsunori Y, Kuramochi J, et al. Laparoscopic removal of a foreign body (a piece of wire) from the abdominal cavity: A case report and review of thirty-two cases in Japan. J Jpn Endosc Surg. 2007;12:415–19. [Google Scholar]
- 6.Birindelli A, Tugnoli G, Biscardi A, et al. Retroperitoneal colonic perforation from a foreign body – ‘cannibalization’ effect of a toothpick – video vignette. Colorectal Dis. 2016;18:319–21. doi: 10.1111/codi.13259. [DOI] [PubMed] [Google Scholar]
- 7.Hara M, Takayama S, Imafuji H, et al. Single-port retrieval of peritoneal foreign body using SILS port: Report of a case. Surg Laparosc Endosc Percutan Tech. 2011;21:e126–29. doi: 10.1097/SLE.0b013e31820df9d0. [DOI] [PubMed] [Google Scholar]
- 8.Lupascu C, Dabija M, Ursulescu C, et al. Removal of an intraperitoneal foreign body using a single port laparoscopic procedure. JSLS. 2011;15:257–60. doi: 10.4293/108680811X13071180407113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kurita N, Shimada M, Nakao T, et al. Laparoscopic removal of a foreign body in the pelvic cavity through one port using a flexible cholangioscope. Dig Surg. 2009;26:205–8. doi: 10.1159/000219325. [DOI] [PubMed] [Google Scholar]
- 10.McArthur T, Abell BA, Levsky ME. A procedure for soft tissue foreign body removal under real-time ultrasound guidance. Mil Med. 2007;172:858–59. doi: 10.7205/milmed.172.8.858. [DOI] [PubMed] [Google Scholar]
- 11.Park HJ, Lee SM, Lee SY, et al. Ultrasound-guided percutaneous removal of wooden foreign bodies in the extremities with hydro-dissection technique. Korean J Radiol. 2015;16:1326–31. doi: 10.3348/kjr.2015.16.6.1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Paziana K, Fields JM, Rotte M, et al. Soft tissue foreign body removal technique using portable ultrasonography. Wilderness Environ Med. 2012;23:343–48. doi: 10.1016/j.wem.2012.04.006. [DOI] [PubMed] [Google Scholar]
- 13.Fu Y, Cui LG, Romagnoli C, et al. Ultrasound-guided removal of retained soft tissue foreign body with late presentation. Chin Med J (Engl) 2017;130:1753–54. doi: 10.4103/0366-6999.209910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Razdan RN, Dube T, Specht N. Ultrasound-guided removal of an infected loose body from the quadriceps muscle. Radiol Case Rep. 2015;3:143. doi: 10.2484/rcr.v3i3.143. [DOI] [PMC free article] [PubMed] [Google Scholar]