Abstract
The anterior cruciate ligament (ACL) is the most commonly injured ligament in the knee, with injury usually occurring as a result of multidirectional sports. The incidence of ACL injury has continued to increase, with most patients opting for surgery to improve stability as well as permit a return to sport. Traditional methods of ACL reconstruction can achieve this but are not without their problems, including graft rupture, residual laxity, and donor-site morbidity. There is therefore a requirement for further research into newer, innovative surgical techniques to help improve complication rates. This article describes, with video illustration, ACL reconstruction using a reduced-size bone–patellar tendon–bone autograft with suture tape augmentation. The augmentation acts as a stabilizer during the early stages of graft incorporation while resisting against reinjury during an accelerated recovery. The ability to use a reduced-size graft decreases the donor-site burden, and retention of residual native ACL tissue, when possible, may help with proprioception.
Technique Video
Narrated step-by-step guide for anterior cruciate ligament (ACL) reconstruction with suture tape augmentation using reduced-size bone–patellar tendon–bone autograft. A standard midline incision is made for graft harvesting, aiming for a reduced, 7- to 8-mm bone–patellar tendon–bone autograft. The graft is then attached to a suture button with the suture tape running alongside it. Standard anterolateral and anteromedial portals are used, and the ACL remnant is preserved when possible without debridement. The tibial tunnel and femoral tunnel are prepared; the graft is then shuttled from distal to proximal using the lead sutures, and an interference screw is used to fix the bone plug in the femur. A bone anchor with both ends of the suture tape is placed just distal to the tibial tunnel with the knee in full extension. An interference screw is then inserted to secure the bone plug in the tibia with modest tension.
The anterior cruciate ligament (ACL) arises from the medial wall of the lateral femoral condyle and inserts onto the intercondylar area of the tibia. It is derived from multiple small fibers and can be divided into anteromedial and posterolateral fiber bundles.1,2 Its primary function is to prevent anterior tibial translation on the femur, but it also has a role in preventing internal tibial rotation and thus reducing the risk of anterior subluxation of the lateral and medial tibiofemoral components.3 The ultrastructural organization of collagen fibers within the ACL resists multidirectional forces at varying tensile strains.1,4 When the ultimate tensile force of the fibers is exceeded, usually during a sudden, noncontact twist of an extended knee, damage occurs, causing a partial or complete tear of the macrostructure. The ACL is the most commonly injured ligament in the knee, with a reported incidence as high as 0.8 per 1,000 population in the United Kingdom.5,6 Most ACL injuries occur in athletes taking part in multidirectional sports such as skiing, basketball, and football. Recent studies have suggested that female individuals are more susceptible, with several potential factors postulated, including weaker hamstrings, increased valgus angulation at the knee, and hormonal influences.7
Concerns regarding the healing capacity of the ACL led to the development of ACL reconstruction, usually with autograft, as the gold standard for the past 30 years. However, ACL reconstruction does not come without complications, being challenged by residual laxity, variable performance outcomes, rerupture, and donor-site morbidity.8, 9, 10
It is therefore necessary to establish innovative techniques in an attempt to overcome these complications. Our group has previously shown the use of suture augmentation for ACL repair, as well as for other procedures in both the knee and other joints.11 High-strength suture tape acts as a stabilizer, enhancing the strength of the construct and allowing for graft preservation. It acts to protect the graft during the initial incorporation phase, while the patient can begin accelerated rehabilitation. In this Technical Note, we describe ACL reconstruction with suture tape augmentation using a reduced-size bone–patellar tendon–bone autograft (Video 1).
Surgical Technique
The patient is placed in the supine position, and a tourniquet is placed on the upper thigh. The injured leg is prepared and draped in the surgeon's preferred position, similarly to a standard ACL reconstruction procedure.
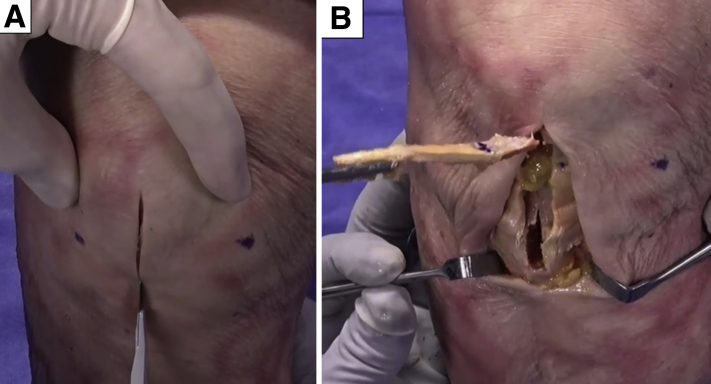
A midline incision is made from the inferior pole of the patella to the tibial tubercle for graft harvesting. This is achieved in a standard fashion aiming for a reduced, 7- to 8-mm bone–patellar tendon–bone autograft (Fig 1).
Fig 1.
Anteroposterior view of right knee in flexion. A midline incision is made from the inferior pole of the patella to the tibial tubercle (A) for graft harvesting (B).
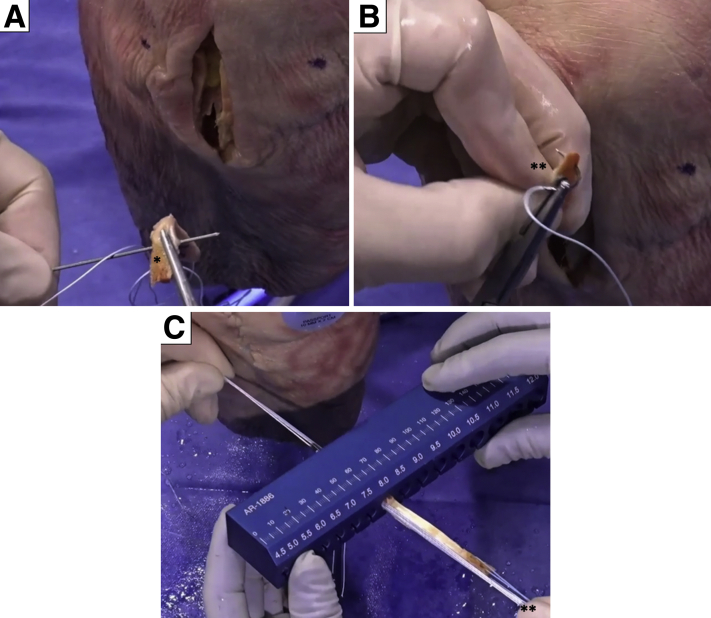
The middle third of the tendon is used, aiming for a 15-mm V-shaped bone plug from the patella and a 20-mm length of bone plug from the tibia. The tibial plug is reduced in size by nibbling the cancellous bone, which is used as autograft for the tibial donor site. Two holes are made in the tibial bone plug with a 2-mm drill bit. One hole is made in the patellar bone plug 5 mm from the tip. FiberWire (Arthrex, Naples, FL) is passed through these drill holes to allow graft shuttling (Fig 2). FiberTape (Arthrex) is then attached to a Retrobutton (Arthrex) (Fig 3). The suture tape is an ultrahigh-strength 2-mm-wide tape, consisting of a long-chain ultrahigh-molecular-weight polyethylene.
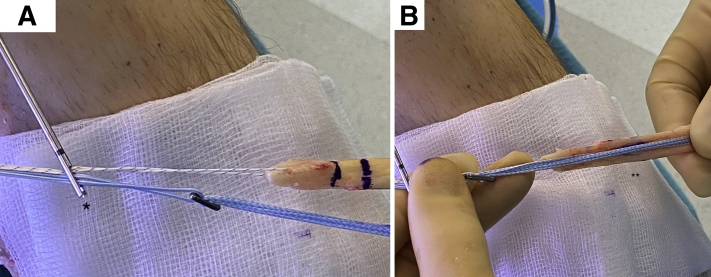
Fig 2.
Tendon graft. The middle third of the tendon is used, aiming for a 15-mm length of bone from the patella and 20-mm length from the tibia. (A) Two holes are made in the tibial bone plug with a 2-mm drill bit (asterisk). (B) One hole is made in the patellar bone plug 5 mm from the tip (asterisks). (C) A suture is passed through the drill holes to allow graft shuttling, aiming for a reduced, 7- to 8-mm bone–patellar tendon–bone autograft (asterisks).
Fig 3.
Graft preparation. (A) A single suture is passed through the drill hole in the patellar bone plug (1 asterisk) and 2 sutures are passed through the drill holes in the tibial bone plug (2 asterisks) to allow graft shuttling. (B) The suture tape is attached to a Retrobutton (asterisks).
Standard anterolateral and anteromedial portals are created, and a PassPort cannula (Arthrex) is placed in the anteromedial portal (Fig 4). Arthroscopic inspection of the knee is performed, and if necessary, meniscal or cartilage surgery is undertaken. The ACL remnant is preserved when possible, without debridement.
Fig 4.
(A) Anteroposterior view of right knee in flexion. Standard anterolateral and anteromedial portals (asterisks) are created. (B) Lateral view of right knee in flexion. A PassPort cannula is placed in the anteromedial portal (asterisks).
At the center of the ACL footprint, a standard tibial ACL guide is placed at 55°. A skin incision is made above the pes anserinus, and a guidewire is passed through the tibial guide just beyond the tibial cortex at the ACL footprint. The tibial tunnel is then created using an impaction reamer matching the size of the graft. A transtibial drilling technique is used to create the femoral tunnel using the ACL remnants at the femoral footprint as a guide. A stab incision is made through the skin at the exit point of the guidewire. The femoral tunnel is reamed to 20 to 25 mm in length and to a diameter based on the reduced-size bone plug (7-8 mm). The femoral tunnel is reamed with an acorn reamer, which allows translation even with the transtibial approach. The graft is then shuttled from distal to proximal using the lead sutures (Fig 5). The suture tape is secured to the cortex first; then, a 6-mm interference screw is used to fix the bone plug in the femur, which retains tension on the suture tape (Fig 6).
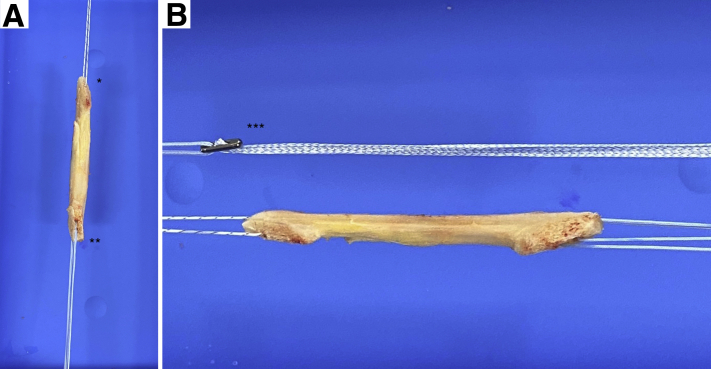
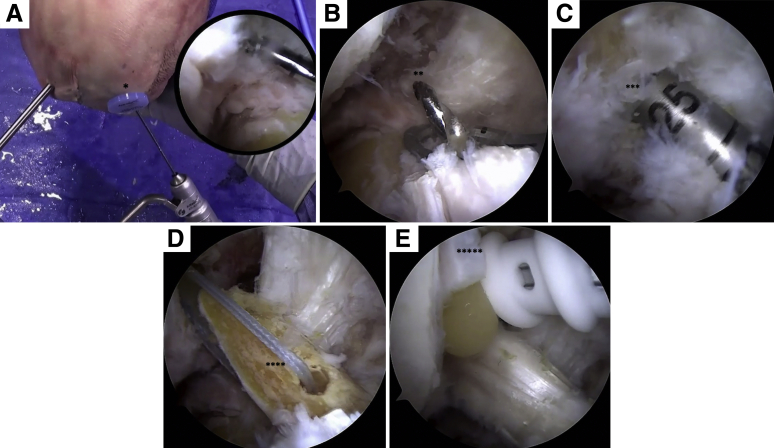
Fig 5.
Graft shuttling. (A) The graft and suture tape are inserted through a passing pin (asterisk). (B) The completed construct (asterisks) prior to graft shuttling with suture tape augmentation in the knee.
Fig 6.
Arthroscopic view of right knee in flexion. (A) A skin incision is made above the pes anserinus, and a guidewire is passed through the tibial guide just beyond the tibial cortex at the anterior cruciate ligament footprint (asterisk). (B) The tibial tunnel is created using an impaction reamer (asterisks) matching the size of the graft. A transtibial approach is used to create the femoral tunnel using the anterior cruciate ligament remnants at the femoral footprint as a guide. A stab incision is made through the skin at the exit point of the guidewire. (C) The femoral tunnel is reamed to 20 to 25 mm (asterisks). (D) The graft is shuttled from distal to proximal using the lead sutures (asterisks). (E) The button is secured to the cortex; then, a 6-mm interference screw is used to fix the bone plug in the femur (asterisks).
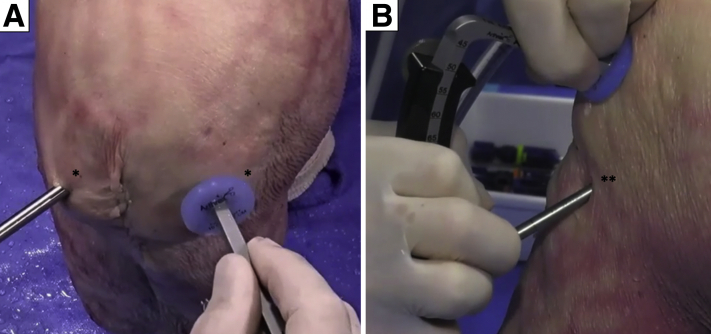
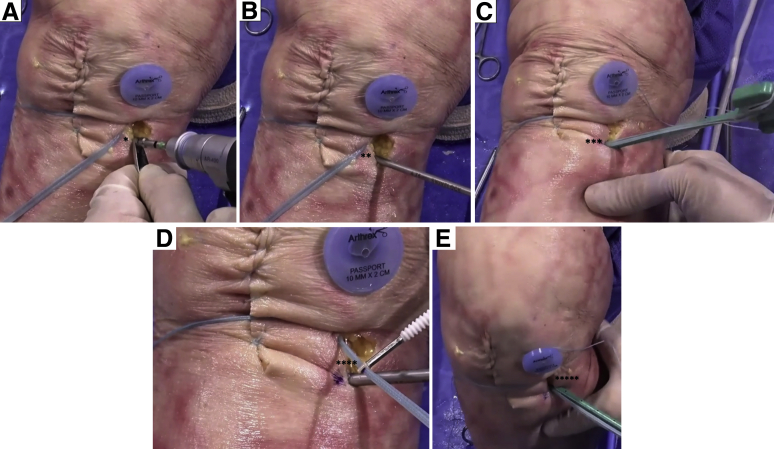
After predrilling 1 cm distal to the tibial tunnel with a 3.5-mm drill, followed by tapping, a 4.75-mm SwiveLock (Arthrex) loaded with both ends of the suture tape is placed with the knee in full extension. To avoid over-tightening, the suture tape is marked at the beginning of the screw of the suture anchor, repositioned in the eye at the marked level, and taken through a range of motion; last, the anchor is placed in the drill hole (Fig 7).
Fig 7.
Anteroposterior view of right knee. After predrilling 1 cm distal to the tibial tunnel with a 3.5-mm drill (1 asterisk) (A), followed by tapping (2 asterisks) (B), a 4.75-mm bone anchor loaded with both ends of the suture tape (asterisks) is placed with the knee in full extension (C). To avoid over-tightening, the suture tape is marked at the beginning of the screw of the suture anchor, repositioned in the eye at the marked level (4 asterisks) (D), and taken through a range of motion; last, the anchor is placed in the drill hole (5 asterisks) (E).
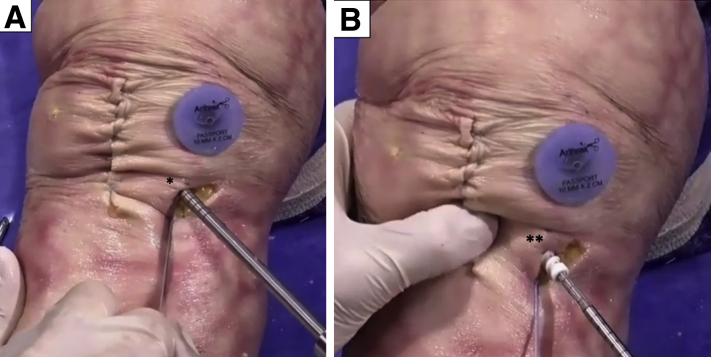
Finally, the knee is taken through a range of motion. A 7-mm interference screw is then inserted in the tibial tunnel to secure the bone plug with modest tension. Care is taken to close the paratendon, which contains the fat pad (Fig 8).
Fig 8.
Anteroposterior view of right knee. (A) The knee is taken through a range of motion, and the tibial tunnel is tapped (asterisk) with the knee in full extension. (B) A 7-mm interference screw is inserted to secure the bone plug (asterisks) with modest tension.
The patient is allowed full weight bearing during the first weeks, with no requirement for external bracing. Physical therapy focuses on early range of movement, muscle control, and restoration of function. This is facilitated by the limited pain and swelling from the reduced surgical morbidity, allowing accelerated early-phase rehabilitation. Patients are allowed to perform pivoting sports if the neuromuscular function has recovered, usually from around 5 months. The advantages and disadvantages of our technique are outlined in Table 1, and some pearls and pitfalls are shown in Table 2.
Table 1.
Advantages and Disadvantages of ACL Reconstruction With Suture Tape Augmentation
| Advantages |
| Less traumatic to donor tissues |
| Bone conserving |
| Simple and reproducible |
| Protection provided by suture tape during early-phase rehabilitation, minimizing risk of failure |
| Reduced risk of anterior knee pain and fracture |
| Disadvantages |
| Potential for donor-site morbidity still exists |
| Sensory loss and skin wound issues |
ACL, anterior cruciate ligament.
Table 2.
Pearls and Pitfalls of ACL Reconstruction With Suture Tape Augmentation
| Pearls |
| Perform careful patellar tendon harvest. |
| Bear in mind that independent fixation for the suture tape and graft is biomechanically stronger. |
| Lock the button on the cortex, and apply tension before fixing the femoral bone plug. |
| Pitfalls |
| Avoid securing in flexion to avoid over-tensioning. |
| Do not use force to elevate the bone plug. |
| Insert the suture anchor gently because excessive force will damage the screw threads. |
ACL, anterior cruciate ligament.
Discussion
A ruptured ACL was once a life-changing event and potentially a career-ending injury for athletes. Now, with the advancements in surgical technique, equipment, and reconstruction, patients can return to nearly normal levels of function. Despite good functional outcomes postoperatively, there are still potential complications associated with ACL reconstruction, such as ligament laxity, rerupture, anterior knee pain, and stiffness.8, 9, 10
This Technical Note describes a simple and reproducible technique for ACL reconstruction with suture tape augmentation. The advent of suture tape has revolutionized this procedure because it acts as a secondary stabilizer allowing for the natural healing process to take place while facilitating early rehabilitation and minimizing the risk of graft failure.11 A recent biomechanical study showed that suture tape reinforcement of a cadaveric ACL reconstruction significantly reduced elongation and graft failure rates; it is thought that this would correlate clinically to reduced rerupture rates in vivo.12,13 Despite increasing popularity of the use of suture tape augmentation in extra-articular ligament procedures, its use in ACL reconstruction has not been widely described, and to our knowledge, there are currently no long-term follow-up data available.
We describe a technique in which the use of suture augmentation facilitates a reduced-size graft harvest from the patellar tendon, which may reduce the risk of anterior knee pain. This was the most common complication in a recent cohort study on postoperative complications after ACL reconstruction using patellar tendon autograft.14 However, as with any graft harvest, there is still potential to cause donor-site morbidity.
In conclusion, this Technical Note has discussed the technique of ACL reconstruction with suture tape augmentation using a reduced-size bone–patellar tendon–bone autograft. This is a simple and reproducible technique with reduced surgical morbidity and the advantage of a stabilizer to protect the graft while it is incorporating during initial accelerated rehabilitation. Clinical studies are necessary to determine the overall outcomes of this procedure, and we look forward to presenting these as we follow up our patients prospectively over the next 2 years.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: Arthrex facilitated the making of the video in this article. G.M.M. is a consultant for teaching for Arthrex and has a patent for the InternalBrace, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Narrated step-by-step guide for anterior cruciate ligament (ACL) reconstruction with suture tape augmentation using reduced-size bone–patellar tendon–bone autograft. A standard midline incision is made for graft harvesting, aiming for a reduced, 7- to 8-mm bone–patellar tendon–bone autograft. The graft is then attached to a suture button with the suture tape running alongside it. Standard anterolateral and anteromedial portals are used, and the ACL remnant is preserved when possible without debridement. The tibial tunnel and femoral tunnel are prepared; the graft is then shuttled from distal to proximal using the lead sutures, and an interference screw is used to fix the bone plug in the femur. A bone anchor with both ends of the suture tape is placed just distal to the tibial tunnel with the knee in full extension. An interference screw is then inserted to secure the bone plug in the tibia with modest tension.
References
- 1.Odensten M., Gillquist J. Functional anatomy of the anterior cruciate ligament and a rationale for reconstruction. J Bone Joint Surg Am. 1985;67:257–262. [PubMed] [Google Scholar]
- 2.Duthon V.B., Barea C., Abrassart S., Fasel J.H., Fritschy D., Menetrey J. Anatomy of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2006;14:204–213. doi: 10.1007/s00167-005-0679-9. [DOI] [PubMed] [Google Scholar]
- 3.Haimes J.L., Wroble R.R., Grood E.S., Noyes F.R. Role of the medial structures in the intact and anterior cruciate ligament-deficient knee. Limits of motion in the human knee. Am J Sports Med. 1994;22:402–409. doi: 10.1177/036354659402200317. [DOI] [PubMed] [Google Scholar]
- 4.Girgis F.G., Marshall J.L., Monajem A. The cruciate ligaments of the knee joint. Anatomical, functional and experimental analysis. Clin Orthop Relat Res. 1975;106:216–231. doi: 10.1097/00003086-197501000-00033. [DOI] [PubMed] [Google Scholar]
- 5.Frobell R.B., Lohmander L.S., Roos H.P. Acute rotational trauma to the knee: Poor agreement between clinical assessment and magnetic resonance imaging findings. Scand J Med Sci Sports. 2007;17:109–114. doi: 10.1111/j.1600-0838.2006.00559.x. [DOI] [PubMed] [Google Scholar]
- 6.Gianotti S.M., Marshall S.W., Hume P.A., Bunt L. Incidence of anterior cruciate ligament injury and other knee ligament injuries: A national population-based study. J Sci Med Sport. 2009;12:622–627. doi: 10.1016/j.jsams.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 7.Gupta R., Malhotra A., Sood M., Masih G.D. Is anterior cruciate ligament graft rupture (after successful anterior cruciate ligament reconstruction and return to sports) actually a graft failure or a re-injury? J Orthop Surg (Hong Kong) 2019;27 doi: 10.1177/2309499019829625. 2309499019829625. [DOI] [PubMed] [Google Scholar]
- 8.Schlumberger M., Schuste P., Schulz M. Traumatic graft rupture after primary and revision anterior cruciate ligament reconstruction: Retrospective analysis of incidence and risk factors in 2915 cases. Knee Surg Sports Traumatol Arthrosc. 2017;25:1535–1541. doi: 10.1007/s00167-015-3699-0. [DOI] [PubMed] [Google Scholar]
- 9.Frobell R.B., Roos H.P., Roos E.M., Roemer F.W., Ranstam J., Lohmander L.S. Treatment for acute anterior cruciate ligament tear: Five year outcome of randomised trial. BMJ. 2013;346:F232. doi: 10.1136/bmj.f232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harter R.A., Osternig L.R., Singer K.M., James S.L., Larson R.L., Jones D.C. Long-term evaluation of knee stability and function following surgical reconstruction for anterior cruciate ligament insufficiency. Am J Sports Med. 1988;16:434–443. doi: 10.1177/036354658801600502. [DOI] [PubMed] [Google Scholar]
- 11.Mackay G.M., Blyth M.J., Anthony I., Hopper G.P., Ribbans W.J. A review of ligament augmentation with the InternalBrace: The surgical principle is described for the lateral ankle ligament and ACL repair in particular, and a comprehensive review of other surgical applications and techniques is presented. Surg Technol Int. 2015;26:239–255. [PubMed] [Google Scholar]
- 12.Rousseau R., Labruyere C., Kajetanek C., Deschamps O., Makridis K.G., Djian P. Complications after anterior cruciate ligament reconstruction and their relation to the type of graft: A prospective study of 958 cases. Am J Sports Med. 2019;47:2543–2549. doi: 10.1177/0363546519867913. [DOI] [PubMed] [Google Scholar]
- 13.Bachmaier S., Smith P.A., Bley J., Wijdicks C.A. Independent suture tape reinforcement of small and standard diameter grafts for anterior cruciate ligament reconstruction: A biomechanical full construct model. Arthroscopy. 2018;34:490–499. doi: 10.1016/j.arthro.2017.10.037. [DOI] [PubMed] [Google Scholar]
- 14.Desai N., Andernord D., Sundemo D. Revision surgery in anterior cruciate ligament reconstruction: A cohort study of 17,682 patients from the Swedish national knee ligament register. Knee Surg Sports Traumatol Arthrosc. 2017;25:1542–1554. doi: 10.1007/s00167-016-4399-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Narrated step-by-step guide for anterior cruciate ligament (ACL) reconstruction with suture tape augmentation using reduced-size bone–patellar tendon–bone autograft. A standard midline incision is made for graft harvesting, aiming for a reduced, 7- to 8-mm bone–patellar tendon–bone autograft. The graft is then attached to a suture button with the suture tape running alongside it. Standard anterolateral and anteromedial portals are used, and the ACL remnant is preserved when possible without debridement. The tibial tunnel and femoral tunnel are prepared; the graft is then shuttled from distal to proximal using the lead sutures, and an interference screw is used to fix the bone plug in the femur. A bone anchor with both ends of the suture tape is placed just distal to the tibial tunnel with the knee in full extension. An interference screw is then inserted to secure the bone plug in the tibia with modest tension.
Narrated step-by-step guide for anterior cruciate ligament (ACL) reconstruction with suture tape augmentation using reduced-size bone–patellar tendon–bone autograft. A standard midline incision is made for graft harvesting, aiming for a reduced, 7- to 8-mm bone–patellar tendon–bone autograft. The graft is then attached to a suture button with the suture tape running alongside it. Standard anterolateral and anteromedial portals are used, and the ACL remnant is preserved when possible without debridement. The tibial tunnel and femoral tunnel are prepared; the graft is then shuttled from distal to proximal using the lead sutures, and an interference screw is used to fix the bone plug in the femur. A bone anchor with both ends of the suture tape is placed just distal to the tibial tunnel with the knee in full extension. An interference screw is then inserted to secure the bone plug in the tibia with modest tension.