Abstract
Recent advancements in orthopaedic devices have instilled a renewed interest in repair of the anterior cruciate ligament. Biological augmentation of the repair has also recently been investigated with the hopes of improving repair outcomes and improving biological healing. The advent of needle arthroscopy allows for potentially decreased recovery times and potentially reduced complication rates compared with traditional arthroscopy. The purpose of this article is to present a percutaneous technique to repair the anterior cruciate ligament with suture tape augmentation while also augmenting with the biological byproducts from the native effusion using needle arthroscopy.
Technique Video
Surgical technique for repair of the anterior cruciate ligament using suture tape augmentation, needle arthroscopy, and biological augmentation in the right knee with the patient in the supine position.
Needle arthroscopy has been available for use since the early 1990s.1 As the technology of needle arthroscopy advances, so do its indications and delineated benefits. The resolution of needle arthroscopy is approaching that of standard arthroscopy cameras, and multiple studies have shown its safe, effective use as a diagnostic tool in place of magnetic resonance imaging.2, 3, 4, 5, 6, 7 Given the quality of imaging, some surgeons are exploring the use of a needle arthroscope as a primary visualization tool in surgery as a replacement for a standard arthroscopy camera. The camera and picture quality, combined with instruments the size of the needle arthroscope, allows for percutaneous surgery, thus minimizing tissue damage and yielding a theoretical reduction in complications. There has also been an increased interest in anterior cruciate ligament (ACL) repair with multiple techniques recently described using modern orthopaedic devices such as the needle arthroscope and implants, including suture anchors,8 dynamic intraligamentary stabilization,9 and internal bracing,10 that were not available in the historical studies, giving a reason to reassess the outcomes of primary repair in the more recent era.
ACL repair offers many theoretical benefits in comparison to reconstruction, including no graft use or graft-site morbidity; maintenance of native ACL tissue, preserving the ligament nervous structures, which are important for knee proprioception11; and preservation of patient biology and accelerated recovery.12 Theoretically, repairing the native ACL would therefore restore the knee with its original mechanoreceptors.13,14 Furthermore, in case of failure of primary ACL repair, possible revision surgery is similar to primary reconstruction, which is not the case with ACL reconstruction surgery.15
Recent systematic reviews have shown that the survivorship of ACL repair ranges from 60% to 100%, but considering only the subgroup of proximal ACL tears treated with repair, the rate of revision ACL reconstruction and the total reoperation rate were as high as 12% and 18%, respectively,16 similar to systematic reviews of ACL reconstruction.17,18 There has also been additional interest in biological augmentation of ACL repair, with the hopes of improving tissue healing.19
The purpose of this article is to share an ACL repair technique with suture tape augmentation using needle arthroscopy and augmenting the repair site with cellular byproducts and platelet-rich plasma.
Technique
After informed consent is obtained from the patient, the operating room is prepared for surgery on the knee (Video 1). The disposable kit is prepared on a sterile field, including a 20-mL syringe with an equal mixture of 1% lidocaine with epinephrine and 0.25% bupivacaine, a separate 20-mL syringe with only 0.25% bupivacaine, a 60-mL syringe, chlorhexidine scrub, the needle arthroscopy handpiece (Nanoscope; Arthrex, Naples, FL), a skin marker, pump tubing, a femoral-sided suture anchor (SwiveLock; Arthrex) with suture tape (LabralTape; Arthrex), a tibial-sided suture anchor (PushLock; Arthrex), and sterile bandages. Further equipment, such as needle-sized arthroscopic baskets and a shaver (Arthrex), is placed on the operative field as needed. The display from the needle arthroscope is placed in easy sight for the physician.
The patient is placed supine on the operating table with the operative lower extremity prepared with ChloraPrep scrub (BD, Franklin Lakes, NJ) and then draped in standard sterile fashion to allow for access to and manipulation of the surgical site. A stockinet is placed over the foot and ankle and secured in place just distal to the tibial tuberosity with Coban wrap (3M, St Paul, MN). The portal sites are marked on the operative extremity and include a lateral portal site, superolateral portal site, medial portal site, and accessory medial portal site. The 20-mL syringe with a 25-gauge needle is used to infiltrate 10 mL of the mixed local anesthetic to each portal site (Fig 1) and the surrounding capsule to anesthetize the area. Once cutaneous anesthesia is achieved, the Nanoscope camera trocar and cannula are inserted into the knee joint. The trocar is slightly pulled back, and a 60-mL syringe is used to aspirate the effusion present after ACL injury. This fluid is then augmented with additional whole blood through phlebotomy in the patient’s arm to obtain a total of 60 mL (Fig 1). The syringe is placed in the centrifuge (Angel; Arthrex) and spun to obtain the cellular and platelet-rich plasma components.
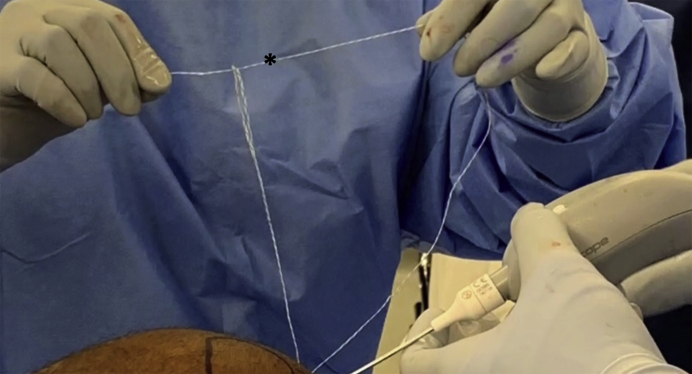
Fig 1.
Knee effusion aspiration (asterisk) after an injury to the anterior cruciate ligament, shown through the lateral portal in a right knee with the patient in the supine position.
The needle arthroscope is connected to the viewing tablet in sterile fashion, and a 60-mL syringe of sterile saline solution is attached to the inflow port of the needle arthroscope handpiece. On entrance into the knee, an accessory superolateral portal is placed percutaneously to act as an inflow cannula (Fig 2). A medial portal is then placed to allow both instrumentation and visualization as needed. The blunt trocar of the needle arthroscopy system or a probe can be used for inspection of the intra-articular structures. After a diagnostic arthroscopy has been completed, an accessory medial portal is placed 1.5 to 2 cm medial to the medial portal and used as another working portal. The camera may be switched between the standard and accessory medial portals as needed to better visualize and address the pathology, as well as the fluid pump and inflow connected to the camera system.
Fig 2.
Portals used for percutaneous anterior cruciate ligament repair using needle arthroscopy. The superolateral portal (SL), lateral portal (L), medial portal (M), and accessory medial portal (AM) are labeled on a right knee with the patient in the supine position.
The camera is then switched to the medial portal, and a Micro SutureLasso (Arthrex) is used to pass a nitinol wire in the lateral to medial direction through one of the bundles of the ACL (Fig 3). The wire is retrieved with a “nano” suture grasper (Arthrex) through the far medial portal. The suture tape is then looped through the nitinol wire and passed from medial to lateral through the ACL. The same grasper retrieves the passed tail from the far medial portal, and the suture is looped onto itself, creating a luggage tag–type stitch (Fig 4). This cinches the ACL, and this step can be repeated as needed to obtain adequate fixation of the ACL remnant.
Fig 3.
The Micro SutureLasso is used to pass a nitinol wire in the lateral to medial direction for anterior cruciate ligament repair in a right knee with the patient in the supine position.
Fig 4.
A luggage-tag stitch (asterisk) is placed through the torn bundle of the anterior cruciate ligament during anterior cruciate ligament repair in a right knee with the patient in the supine position.
Next, the punch for the suture anchor is impacted through the far medial portal into the femoral side near the ACL origin for marrow stimulation and then just distal to the ACL origin for placement of the suture anchor. It is also recommended to use a tap because the bone in this area can be quite hard. The suture anchor (SwiveLock) is then loaded with both the repair stitch through the ACL and the suture tape (LabralTape) (Fig 5). This is impacted into the femoral origin with appropriate tension on the repair stitch that allows approximation of the femoral socket and is secured.
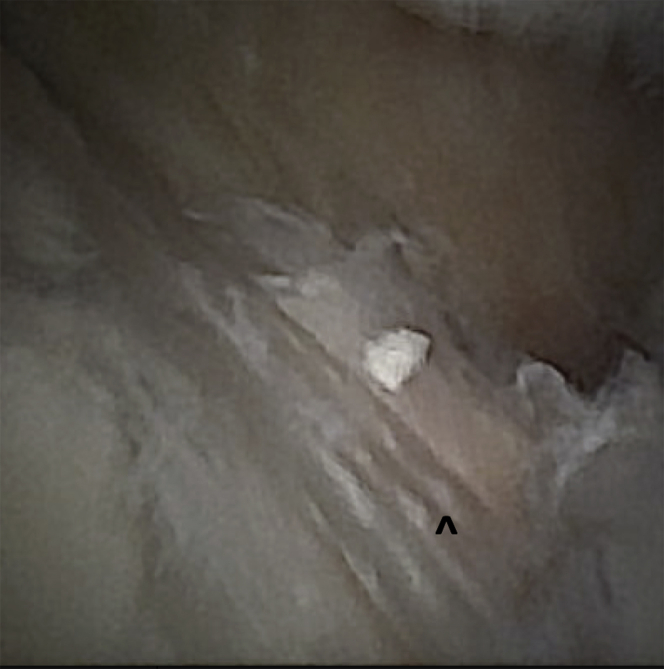
Fig 5.
The suture anchor with repair stitch (asterisk) and suture tape (caret) (Arthrex) is impacted into the femoral socket during anterior cruciate ligament repair in a right knee with the patient in the supine position.
The fluid inflow is transferred to the medial portal, the suture grasper is placed through the superolateral portal, and the suture tape is retrieved. The punch is then impacted into the ACL insertion site on the tibia. The suture tape is threaded through the suture anchor and secured near 45° of flexion. The access suture is then cut (Fig 6).
Fig 6.
Placement of the suture tape augmentation (caret) is complete after anterior cruciate ligament repair in a right knee with the patient in the supine position.
The camera is placed in the medial portal, and the arthroscopic fluid is aspirated with a 60-mL syringe. Visualization of the ACL repair site is maintained as the arthroscopic fluid is removed. The camera is removed, and the biological byproducts from the effusion are then injected into the repair site (Fig 7). The cannula is removed, and a sterile bandage is placed. Immediate physiotherapy is implemented focused on early range of motion and quadriceps activation. Toe-touch weight bearing is performed for 2 weeks; then, progressive physical therapy and activity are performed following a standardized ACL reconstruction protocol.
Fig 7.
The cellular byproducts and platelet-rich plasma are injected into the repair site of the anterior cruciate ligament through the needle arthroscopy cannula (Arthrex).
Discussion
Our technique comprises percutaneous ACL repair with needle arthroscopy. ACL repair has recently regained interest as a potential treatment option for femoral-sided injuries to the ACL in the acute setting. Recently, in a case-control study, van der List et al.20 reported that 44% of 316 total patients included in the study group were considered to have reparable tears on the basis of tear location and tissue quality. They also suggested that primary repair was more likely to be possible in older patients; in patients with a lower body mass index; and in patients in whom surgery was performed in the acute setting, within 4 weeks of injury.20 A recent systematic review showed failure rates of 7% and 13% for ACL repair with and without additional internal bracing, respectively, with functional outcome scores greater than 85% of the maximum score.15 Similarly, in their systematic review of recent literature, Nwachukwu et al.16 showed that in a subgroup analysis of proximal ACL ruptures treated with repair, the rate of repair revision was 12.9%. Moreover, in their recent systematic review of clinical outcomes, Houck et al.21 found a 0% to 25% failure rate in studies examining reinjury rates for acute repair of femoral-sided ACL injuries. Moreover, 0% to 20% of patients underwent reoperation, which is consistent with published results for ACL reconstruction.21 As suggested by van Eck et al.,22 ACL repair may be a viable option in patients with acute proximal ACL tear and it is possible that with the use of an internal brace, biological augmentation, and scaffold tissue, the success rate of ACL repair may increase.
Our technique also uses suture tape augmentation as an adjunct to the repair, which is thought to protect ligament healing during early range of motion; in fact, the rationale of this augmentation is to provide additional stability to the repaired ligament and protect its healing during early mobilization,10,22 acting like a “seat-belt support” and allowing an instant stability and accelerated rehabilitation. Although preclinical studies have shown improved healing and biomechanical properties of the ACL by adding a mechanical augmentation to a repaired ACL, the real clinical benefits of internal bracing have not yet been assessed.23, 24, 25 Suture tape augmentation has shown increased strength when used with an ACL graft,26 but it is unknown whether those findings translate to a stronger construct in ACL repair.23 Simultaneously with the advent of advanced arthroscopic procedures, several biological enhancement techniques have been developed.27,28
Our technique uses 2 different sources of biological augmentation: We perform marrow stimulation with the notch at the femoral origin, and we aspirate the effusion from the injured knee and centrifuge the aspirate to obtain the biological byproducts. Anz et al.29 showed that the effusion from the injury contains many viable cells. Culture analysis of fibroblast colony-forming units showed that the effusion itself contains over 1,900 progenitor cells.29 By combining marrow stimulation and the centrifuged aspirate, the goal is to augment the documented inherent healing response of the tibial-sided remnant and the repair.30,31
Some technical tips of the described technique should be noted (Table 1), as well as several limitations (Table 2). Although there has been a resurgence of interest in ACL repair, ACL repair as a tool for ACL surgery is limited to a small subset of patients with ACL injury. No long-term clinical data are available for ACL repair through needle arthroscopy because this is the first published description. Visualization through the needle arthroscope can be a challenge, and it is important to have standard arthroscopic equipment available if needed. Technically, passing the SutureLasso (Arthrex) through the ACL stump can be challenging, and it is important to limit the number of passes of the lasso through the ACL stump to prevent further damaging the tissue. Obtaining appropriate tension on the ACL repair is important, and placement of the femoral-sided suture anchor on the anterior portion of the femoral origin of the ACL allows for appropriate positioning. Prospective studies of ACL repair versus reconstruction are limited, and it is unknown if using needle arthroscopy and biological augmentation instead of traditional arthroscopy will further improve outcomes.
Table 1.
Pearls and Pitfalls of Percutaneous Repair of ACL Tears Using Needle Arthroscopy
| Surgical Technique | Pearls | Pitfalls |
|---|---|---|
| Portal placement | Placing the portals just superior to the joint line will allow access to all parts of the joint. | Errant portal placement will make visualization and technique completion difficult. |
| Passage of ACL repair stitch | A stitch should be placed into each bundle, and passing the instruments should be limited to 1 pass through the ACL. | Passing the instruments through the ACL multiple times can result in damage to the native ACL tissue. |
| Fixation of ACL repair | Some slack should be maintained in the repair stitches prior to impacting the suture anchor into the femur. | Too much tension on the repair suture may result in tearing through the ACL remnant. |
| Fixation of suture tape augmentation | Fixating the suture tape in slight flexion can allow for optimal placement at the tibial insertion. | Errant superior-lateral portal placement may result in an inability to obtain the optimal angle for suture tape fixation. |
ACL, anterior cruciate ligament.
Table 2.
Advantages, Disadvantages, Risks, and Limitations of Percutaneous Repair of ACL Tears Using Needle Arthroscopy
| Advantages |
| Minimally invasive |
| Decreased morbidity |
| Theoretically faster recovery |
| Disadvantages |
| Visualization altered owing to 0° needle arthroscope |
| Technically challenging procedure |
| Unknown long-term outcomes |
| Risks |
| Errant portal placement will make visualization and technique completion difficult. |
| Passing the instruments through the ACL multiple times can result in damage to the native ACL tissue. |
| Hardware failure or iatrogenic injury from hardware placement can occur. |
| Limitations |
| ACL repair can be performed only for select patients based on multiple factors such as tear location, age, sports participation, and concurrent injury. |
| Needle arthroscopy in nature has some limitations, and other concurrent injuries identified at the time of arthroscopy may be better evaluated and treated using traditional arthroscopy. |
| Visualization of the entire knee can be challenging and requires experience with the needle scope. |
ACL, anterior cruciate ligament.
In conclusion, ACL repair allows ligament healing rather than ligament replacement, respecting the anatomy of the native knee. On the basis of the recent literature showing good clinical outcomes and failure rates similar to those of primary ACL reconstruction, ACL repair has regained interest in the past few years, especially in patients with acute proximal ACL tears. In this Technical Note, we have described the percutaneous arthroscopic technique to repair the ACL with suture tape augmentation while also augmenting with the biological byproducts from the native effusion using needle arthroscopy for the treatment of an acute proximal ACL tear in the knee.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: M.C.D. is a consultant for Arthrex, outside the submitted work. A.F. is a consultant for Arthrex, outside the submitted work. E.M. is a consultant for Arthrex, outside the submitted work. A.S. is a consultant for Arthrex, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Surgical technique for repair of the anterior cruciate ligament using suture tape augmentation, needle arthroscopy, and biological augmentation in the right knee with the patient in the supine position.
References
- 1.Patel K.A., Hartigan D.E., Makovicka J.L., Dulle D.L., III, Chhabra A. Diagnostic evaluation of the knee in the office setting using small-bore needle arthroscopy. Arthrosc Tech. 2017;7:e17–e21. doi: 10.1016/j.eats.2017.08.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arthrex Introduction to the NanoScope operative arthroscopy system. https://www.arthrex.com/resources/pdv/iTghsDif_EiP3QFsBuW-_g/introduction-to-the-nanoscope-arthroscopy-system Accessed December 16, 2019.
- 3.Trice Medical Introducing my-eye 2. https://pacmedical.com/wp-content/uploads/2019/01/mi-eye2-Product-Brochure.pdf Accessed December 16, 2019.
- 4.Zhang K., Crum R.J., Samuelsson K., Cadet E., Ayeni O.R., de Sa D. In-office needle arthroscopy: A systematic review of indications and clinical utility. Arthroscopy. 2019;35:2709–2721. doi: 10.1016/j.arthro.2019.03.045. [DOI] [PubMed] [Google Scholar]
- 5.Amin N., McIntyre L., Carter T., Xerogeanes J., Voigt J. Cost-effectiveness analysis of needle arthroscopy versus magnetic resonance imaging in the diagnosis and treatment of meniscal tears of the knee. Arthroscopy. 2019;35:554–562.e13. doi: 10.1016/j.arthro.2018.09.030. [DOI] [PubMed] [Google Scholar]
- 6.Gill T.J., Safran M., Mandelbaum B., Huber B., Gambardella R., Xerogeanes J. A prospective, blinded, multicenter clinical trial to compare the efficacy, accuracy, and safety of in-office diagnostic arthroscopy with magnetic resonance imaging and surgical diagnostic arthroscopy. Arthroscopy. 2018;34:2429–2435. doi: 10.1016/j.arthro.2018.03.010. [DOI] [PubMed] [Google Scholar]
- 7.McMillan S., Saini S., Alyea E., Ford E. Office-based needle arthroscopy: A standardized diagnostic approach to the knee. Arthrosc Tech. 2017;6:e1119–e1124. doi: 10.1016/j.eats.2017.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Achtnich A., Herbst E., Forkel P. Acute proximal anterior cruciate ligament tears: Outcomes after arthroscopic suture anchor repair versus anatomic single-bundle reconstruction. Arthroscopy. 2016;32:2562–2569. doi: 10.1016/j.arthro.2016.04.031. [DOI] [PubMed] [Google Scholar]
- 9.Kohl S., Evangelopoulos D.S., Schar M.O., Bieri K., Muller T., Ahmad S.S. Dynamic intraligamentary stabilisation: Initial experience with treatment of acute ACL ruptures. Bone Joint J. 2016;98:793–798. doi: 10.1302/0301-620X.98B6.35040. [DOI] [PubMed] [Google Scholar]
- 10.van der List J.P., DiFelice G.S. Arthroscopic primary anterior cruciate ligament repair with suture augmentation. Arthrosc Tech. 2017;6:e1529–e1534. doi: 10.1016/j.eats.2017.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Papalia R., Maffulli N., Denaro V. The anterior cruciate ligament remnant: To leave it or not. Arthroscopy. 2013;29:1736–1737. doi: 10.1016/j.arthro.2013.08.019. [DOI] [PubMed] [Google Scholar]
- 12.Taylor S.A., Khair M.M., Roberts T.R., DiFelice G.S. Primary repair of the anterior cruciate ligament: A systematic review. Arthroscopy. 2015;31:2233–2247. doi: 10.1016/j.arthro.2015.05.007. [DOI] [PubMed] [Google Scholar]
- 13.Bali K., Dhillon M.S., Vasistha R.K. Efficacy of immunohistological methods in detecting functionally viable mechanoreceptors in the remnant stumps of injured anterior cruciate ligaments and its clinical importance. Knee Surg Sports Traumatol Arthrosc. 2012;20:75–80. doi: 10.1007/s00167-011-1526-9. [DOI] [PubMed] [Google Scholar]
- 14.Iwasa J., Ochi M., Uchio Y. Decrease in anterior knee laxity by electrical stimulation of normal and reconstructed anterior cruciate ligaments. J Bone Joint Surg Br. 2006;88:477–483. doi: 10.1302/0301-620X.88B4.17186. [DOI] [PubMed] [Google Scholar]
- 15.Jonkergouw A., van der List J.P., DiFelice G.S. Arthroscopic primary repair of proximal anterior cruciate ligament tears: Outcomes of the first 56 consecutive patients and the role of additional internal bracing. Knee Surg Sports Traumatol Arthrosc. 2019;27:21–28. doi: 10.1007/s00167-018-5338-z. [DOI] [PubMed] [Google Scholar]
- 16.Nwachukwu B.U., Patel B.H., Lu Y., Allen A.A., Williams R.J., III Anterior cruciate ligament repair outcomes: An updated systematic review of recent literature. Arthroscopy. 2019;35:2233–2247. doi: 10.1016/j.arthro.2019.04.005. [DOI] [PubMed] [Google Scholar]
- 17.van der List J.P., Vermeijden H.D., Sierevelt I.N., DiFelice G.S., van Noort A., Kerkhoffs G.M.M.J. Arthroscopic primary repair of proximal anterior cruciate ligament tears seems safe but higher level of evidence is needed: A systematic review and meta-analysis of recent literature. Knee Surg Sports Traumatol Arthrosc. 2020;28:1946–1957. doi: 10.1007/s00167-019-05697-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hoogeslag R.A.G., Brouwer R.W., Boer B.C., de Vries A.J. Huis In 't Veld R. Acute anterior cruciate ligament rupture: Repair or reconstruction? Two-year results of a randomized controlled clinical trial. Am J Sports Med. 2019;47:567–577. doi: 10.1177/0363546519825878. [DOI] [PubMed] [Google Scholar]
- 19.Dallo I., Chahla J., Mitchell J.J., Pascual-Garrido C., Feagin J.A., LaPrade R.F. Biologic approaches for the treatment of partial tears of the anterior cruciate ligament: A current concepts review. Orthop J Sports Med. 2017;5 doi: 10.1177/2325967116681724. 2325967116681724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.van der List J.P., Jonkergouw A., van Noort A., Kerkhoffs G.M.M.J., DiFelice G.S. Identifying candidates for arthroscopic primary repair of the anterior cruciate ligament: A case-control study. Knee. 2019;26:619–627. doi: 10.1016/j.knee.2019.02.004. [DOI] [PubMed] [Google Scholar]
- 21.Houck D.A., Kraeutler M.J., Belk J.W., Goode J.A., Mulcahey M.K., Bravman J.T. Primary arthroscopic repair of the anterior cruciate ligament: A systematic review of clinical outcomes. Arthroscopy. 2019;35:3318–3327. doi: 10.1016/j.arthro.2019.06.034. [DOI] [PubMed] [Google Scholar]
- 22.van Eck C.F., Limpisvasti O., ElAttrache N.S. Is there a role for internal bracing and repair of the anterior cruciate ligament? A systematic literature review. Am J Sports Med. 2018;46:2291–2298. doi: 10.1177/0363546517717956. [DOI] [PubMed] [Google Scholar]
- 23.Murray M.M., Magarian E., Zurakowski D., Fleming B.C. Bone-to-bone fixation enhances functional healing of the porcine anterior cruciate ligament using a collagen-platelet composite. Arthroscopy. 2010;26:S49–S57. doi: 10.1016/j.arthro.2009.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Seitz H., Menth-Chiari W.A., Lang S., Nau T. Histological evaluation of the healing potential of the anterior cruciate ligament by means of augmented and non-augmented repair: An in vivo animal study. Knee Surg Sports Traumatol Arthrosc. 2008;16:1087–1093. doi: 10.1007/s00167-008-0599-6. [DOI] [PubMed] [Google Scholar]
- 25.Seitz H., Pichl W., Matzi V., Nau T. Biomechanical evaluation of augmented and nonaugmented primary repair of the anterior cruciate ligament: An in vivo animal study. Int Orthop. 2013;37:2305–2311. doi: 10.1007/s00264-013-2098-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bachmaier S., Smith P.A., Bley J., Wijdicks C.A. Independent suture tape reinforcement of small and standard diameter grafts for anterior cruciate ligament reconstruction: A biomechanical full construct model. Arthroscopy. 2018;34:490–499. doi: 10.1016/j.arthro.2017.10.037. [DOI] [PubMed] [Google Scholar]
- 27.Kanazawa T., Soejima T., Noguchi K. Tendon-to bone healing using autologous bone marrow-derived mesenchymal stem cells in ACL reconstruction without a tibial bone tunnel—A histological study. Muscles Ligaments Tendons J. 2014;4:201–206. [PMC free article] [PubMed] [Google Scholar]
- 28.Rizzello G., Longo U.G., Petrillo S. Growth factors and stem cells for the management of anterior cruciate ligament tears. Open Orthop J. 2012;6:525–530. doi: 10.2174/1874325001206010525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Anz A.W., Branch E.A., Rodriguez J. Viable stem cells are in the injury effusion fluid and arthroscopic byproducts from knee cruciate ligament surgery: An in vivo analysis. Arthroscopy. 2017;33:790–797. doi: 10.1016/j.arthro.2016.09.036. [DOI] [PubMed] [Google Scholar]
- 30.Nayak M., Nag H.L., Nag T.C., Yadav R., Singh V., Maredupaka S. Ultrastructural characterization of cells in the tibial stump of ruptured human anterior cruciate ligament, their changes and significance with duration of injury. Med Mol Morphol. 2020;53:86–93. doi: 10.1007/s00795-019-00233-6. [DOI] [PubMed] [Google Scholar]
- 31.Nayak M., Nag H.L., Nag T.C., Digge V., Yadav R. Ultrastructural and histological changes in tibial remnant of ruptured anterior cruciate ligament stumps: A transmission electron microscopy and immunochemistry-based observational study. Musculoskelet Surg. 2020;104:67–74. doi: 10.1007/s12306-019-00599-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical technique for repair of the anterior cruciate ligament using suture tape augmentation, needle arthroscopy, and biological augmentation in the right knee with the patient in the supine position.
Surgical technique for repair of the anterior cruciate ligament using suture tape augmentation, needle arthroscopy, and biological augmentation in the right knee with the patient in the supine position.