Abstract
Pathology of the acromioclavicular joint is common and often resistant to conservative treatment, requiring distal clavicle excision for definitive relief. First described as an open technique by Mumford and Gurd in 1941, distal clavicle excision has evolved greatly, with arthroscopic techniques currently predominating. No significant difference has been found in patient satisfaction or rate of complication between the techniques in a recent meta-analysis. Indeed, open excisions are still performed at a high rate, owing to the difficulty in technique and visualization with arthroscopic methods. One major critique of arthroscopic distal clavicle excision is difficulty safeguarding against under- and overexcision of the distal clavicle due to the lack of depth perception and visual reference points of the arthroscopic perspective. This Technical Note and accompanying video describe an indirect subacromial arthroscopic distal clavicle excision using a fluoroscopic Kirschner wire guide placed at the proximal border prior to resection to serve as a visual and mechanical reference to overexcision.
Technique Video
Distal clavicle excision for acromioclavicular joint osteoarthritis using a fluoroscopic Kirschner (K) wire guide. Preoperative magnetic resonance imaging of the right shoulder in the anteroposterior view confirms osteoarthritis of the AC joint. A blunt trocar and scope sheath are placed in line with the AC joint to obtain access to the AC joint. An 18-gauge spinal needle is placed perpendicular to the lateral end of the distal clavicle and an electrocautery is used to clean up the AC joint. The mobile distal clavicle is observable and clear. A ruler is used to measure 7 mm medially from the spinal needle to the distal clavicle. The 1.5-mm K-wire is then fired into the distal clavicle perpendicular to the distal clavicle and parallel to the spinal needle. Radiographs confirm the proper positioning of the K-wire and then the spinal needle is removed. A 5-mm burr is introduced and begins resection of the distal clavicle from the anterior portal. Resection continues until the K-wire comes into view. Once the entire K-wire is observable, a fluoroscopic image is taken to confirm the 7 mm excision using a K-wire. (AC, acromioclavicular.)
Acromioclavicular (AC) joint osteoarthritis is the most common source of shoulder pain, most prevalent among weightlifters, former athletes, and elderly patients.1, 2, 3 Evaluation of the AC joint involves a thorough history and physical examination in addition to radiography.4 Initial treatment of AC joint osteoarthritis involves anti-inflammatory medications, physical therapy, activity modification, and injections. Only after failure of conservative treatment are suitable candidates recommended surgical intervention.1,5, 6, 7 Open distal clavicle excision (DCE), first described by Mumford and Gurd in 1941, remains the traditional gold standard of treatment.8,9 However, reports of residual pain, stiffness, infection, and unsatisfactory cosmesis in open procedures have been reported and contribute to the increasing popularity of the arthroscopic approach.9, 10, 11 Biomechanical studies also have found 0.5 cm to 1.0 cm of resection with the arthroscopic approach is sufficient for maintaining AC joint space and eliminating bony contact, which is less than the recommended 1.5 cm to 2.0 cm for open resections.12, 13, 14
Arthroscopic DCE has increased in the past decade, with data suggesting a faster recovery and return to sport compared with the open technique.15, 16, 17, 18 No significant quantitative difference in clavicular stability, strength, or complication rate has been found between the techniques in both functional and cadaveric studies.6,9,19 Two primary arthroscopic approaches to DCE exist, the indirect and direct approach. A direct approach uses an anterior superior and posterosuperior portal for resection. In comparison, the indirect approach uses a bursal approach through standard arthroscopic portals.17,19 Both arthroscopic techniques are challenged by limited visualization in addition to increased difficulty judging the depth of resection compared with the open technique.17,20 Our technique and accompanying Video 1 aims to use a Kirschner (K) wire placed at the proximal resection border to be used as a visual reference to guard against over-resection of the distal clavicle.
Surgical Technique (With Video Illustration)
Preoperative Considerations
The preoperative assessment consists of physical examination and radiographs to make a diagnosis of AC joint pathology and evaluate the degree of osteoarthritis or osteolysis. Further imaging with magnetic resonance imaging is recommended before surgery to assess ligamentous and soft tissue anatomy (Fig 1).4
Fig 1.
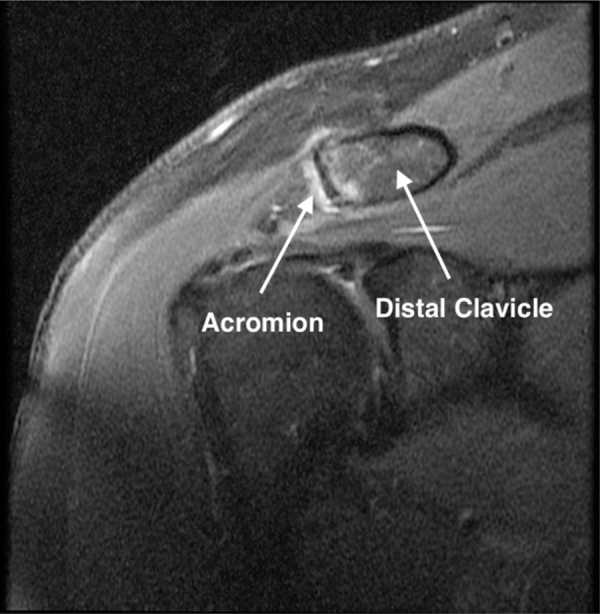
Preoperative magnetic resonance imaging (anteroposterior view) of the right shoulder confirming osteoarthritis of the acromioclavicular joint.
Patient Positioning
The patient is positioned in the beach chair position. The head and bony prominences of the patient are well-padded, and care is taken to ensure proper alignment of the C-spine. The right upper extremity is then prepped and draped in the usual sterile fashion.
Subacromial Decompression
A blunt trocar and scope sheath enter the subacromial space through the standard posterior portal. An #11 blade is used to create a lateral percutaneous portal under needle localization. A combination of the shaver and electrocautery debride the bursal tissue and dissect down to the inferior border of the acromion. A 5-mm burr is used to resect approximately 4 mm of bone from the acromion.
Preparation and Placement of K-Wire Into the Distal Clavicle
The AC joint is first palpated, and an 18-gauge spinal needle is inserted into the joint in a vertical fashion to be used as a landmark. The shaver and electrocautery enter through the anterior portal and are used to debride until the needle and AC joint are visible (Fig 2). The distal portion of the clavicle is pressed down to confirm localization of the AC joint (Fig 3). The spinal needle is reinserted to confirm arthroscopically that it was passed just lateral to the distal end of the clavicle (Fig 4). A ruler is placed on the skin overlying the AC joint to measure 7 mm medially from the spinal needle along the clavicle. The 1.5-mm K-wire is then fired vertically into the clavicle at this spot measured by the rule (Fig 5). The location and trajectory of the K-wire is confirmed with a radiograph (Fig 6). The pin is placed perpendicular to the clavicle. The spinal needle is then removed.
Fig 2.
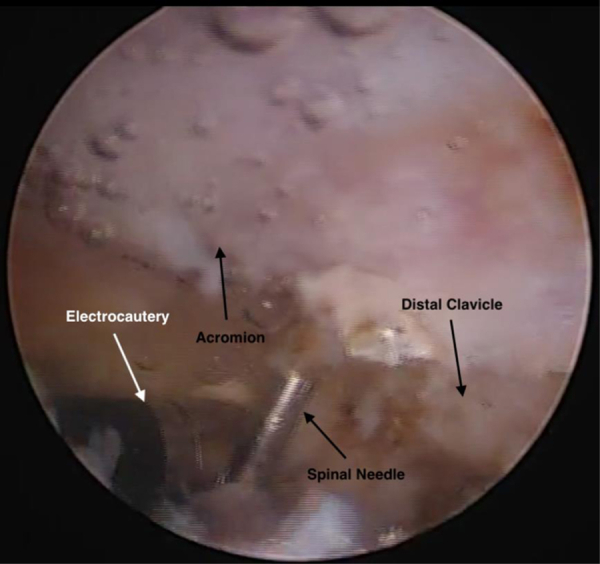
Patient positioned in the beach chair position. Arthroscopic photograph of the right shoulder through the anterior portal of the debridement of the AC joint using an electrocautery until the 18-gauge spinal needle and AC joint are visible. The 18-gauge spinal needle is inserted in a vertical fashion to be used as a landmark.
Fig 3.
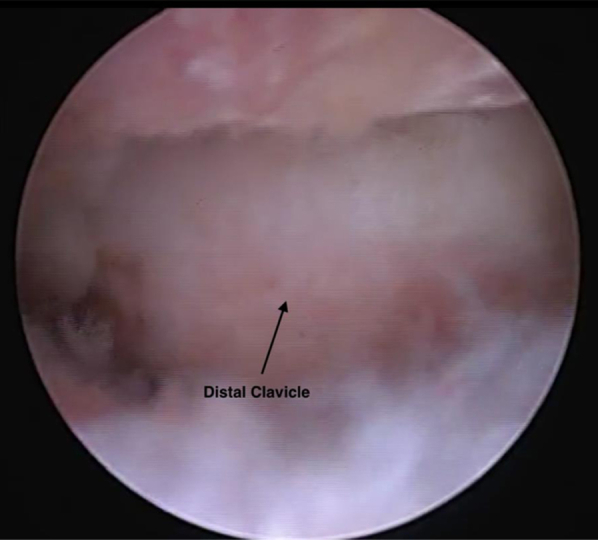
Patient positioned in the beach chair position. Arthroscopic photograph of the right shoulder through the anterior portal of a mobile distal clavicle after debridement of the AC joint and prior to resection.
Fig 4.
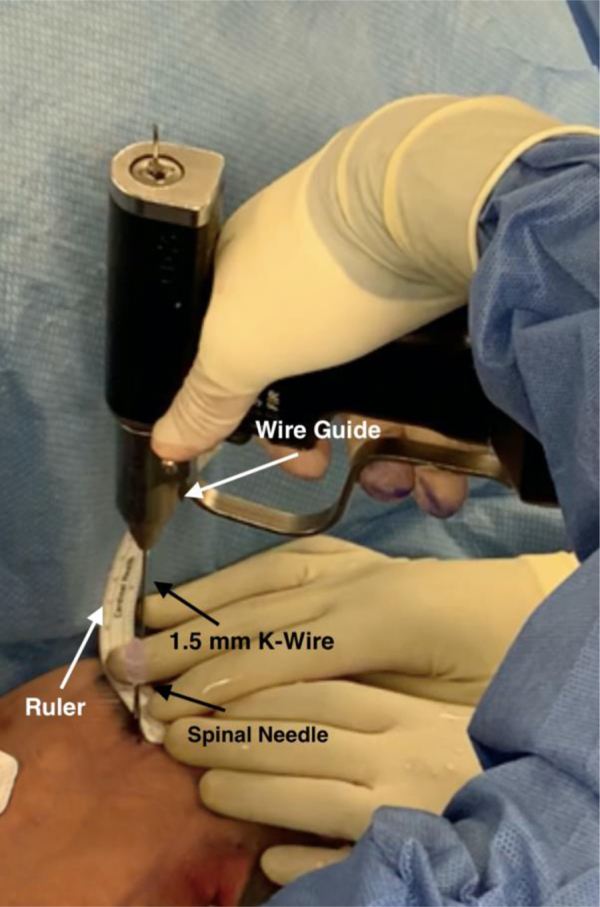
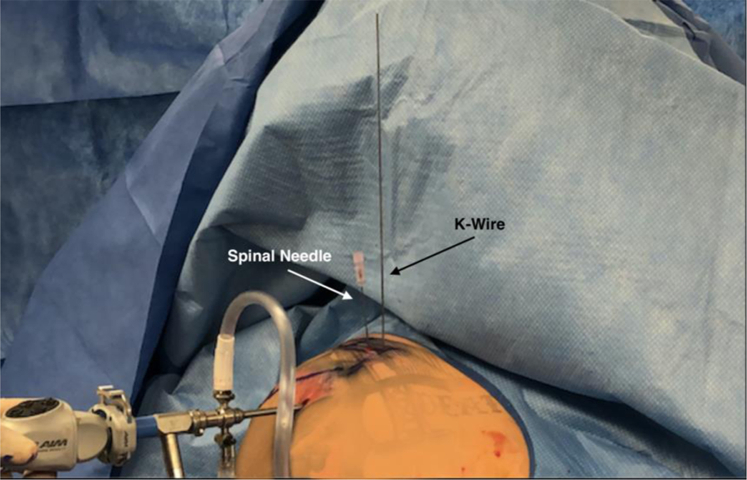
Patient positioned in the beach chair position. Intraoperative image of a 1.5-mm Kirschner (K) wire being fired vertically into the distal clavicle with a wire guide tool. The K-wire is inserted 7 mm medially from the 18-gauge spinal needle that was inserted just lateral to the distal clavicle. Image has been altered to protect identification of the patient.
Fig 5.
Patient positioned in the beach chair position. Intraoperative photograph (anterior view) displaying Kirschner (K) wire and 18-gauge spinal needle placement 7 mm apart from one another before resection. The image has been altered to protect the identity of the patient.
Fig 6.
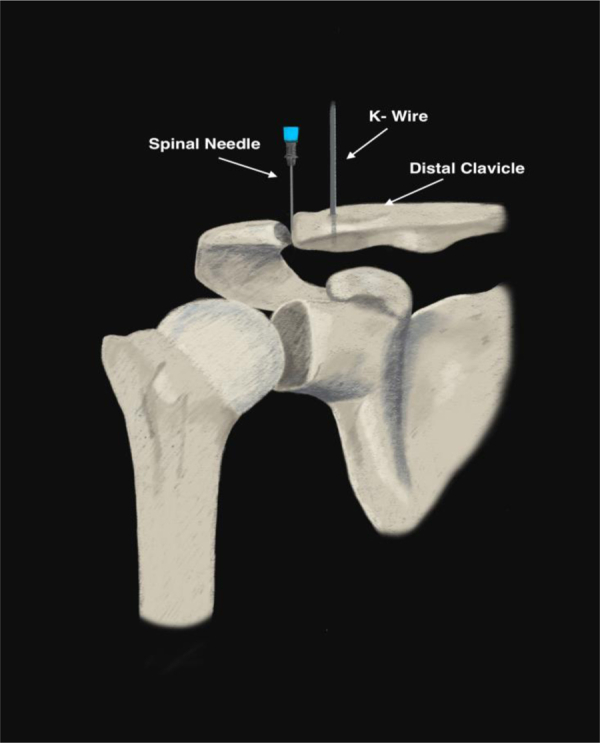
Diagram of the intraoperative radiograph used to confirm the location and trajectory of the Kirschner (K) wire is perpendicular to the distal clavicle and parallel to the 18-gauge spinal needle. The 18-gauge spinal needle is placed in the acromioclavicular joint, closer to the distal clavicle and the K-wire is approximately 7 mm medial from the spinal needle along the distal clavicle.
Subacromial DCE
A 5-mm burr is then introduced to resect the distal clavicle (Fig 7). Bone is evenly resected until the burr encounters the tip of the K-wire (Fig 8). Resection continues vertically along the K-wire to ensure an even resection of both the inferior and superior borders of the clavicle (Fig 9). A 70° scope is then used to gain better visualization of the superior clavicle and AC capsule. Next, the K-wire is removed, and resection continues to ensure a smooth even surface to the distal clavicle (Fig 10). A total of 7 mm of bone is resected.
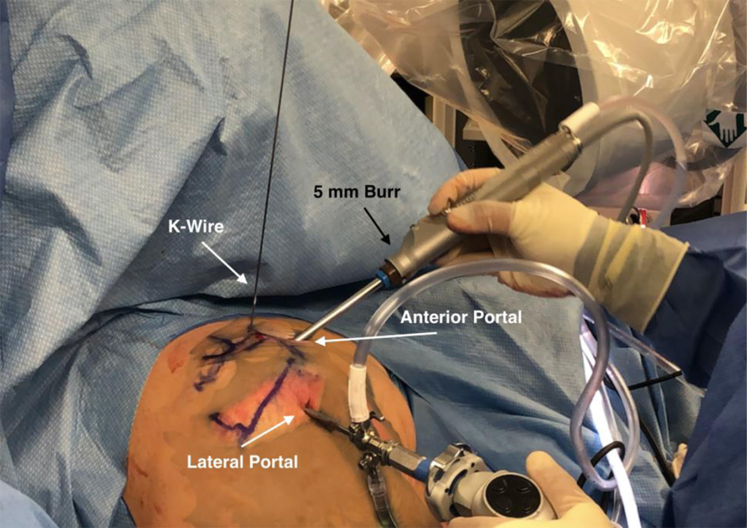
Fig 7.
Patient positioned in the beach chair position. Intraoperative image of distal clavicle excision using a 5-mm burr through the anterior portal until reaching the Kirschner wire. Image has been altered to protect the identity of the patient.
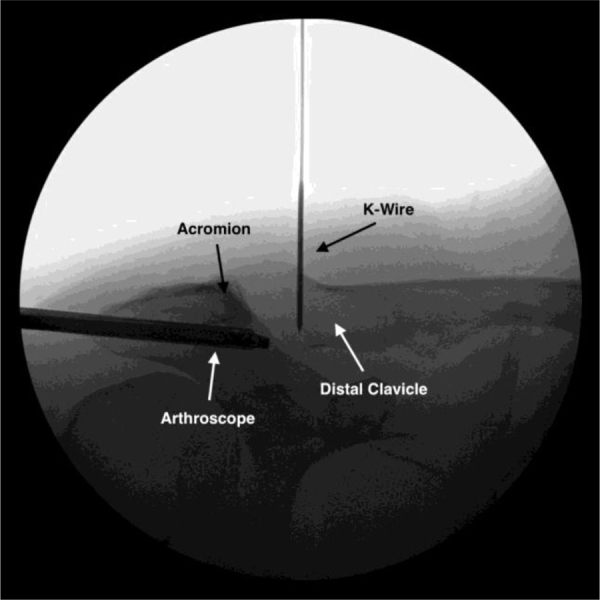
Fig 8.

Patient positioned in the beach chair position. Arthroscopic photograph of the right shoulder through the anterior portal of the distal clavicle midway through excision showing the initial view of the K-Wire.
Fig 9.
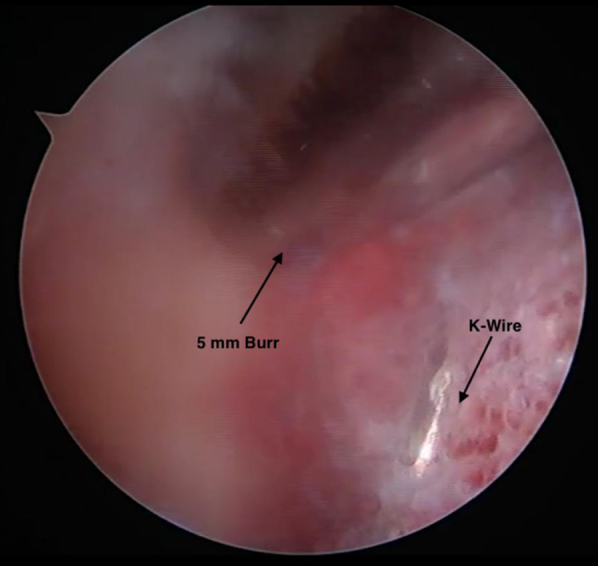
Patient positioned in the beach chair position. Arthroscopic image of the right shoulder through the anterior portal of the 5 mm Burr resecting vertically along the K-Wire. The burr is shown to be coming into contact with the K-Wire.
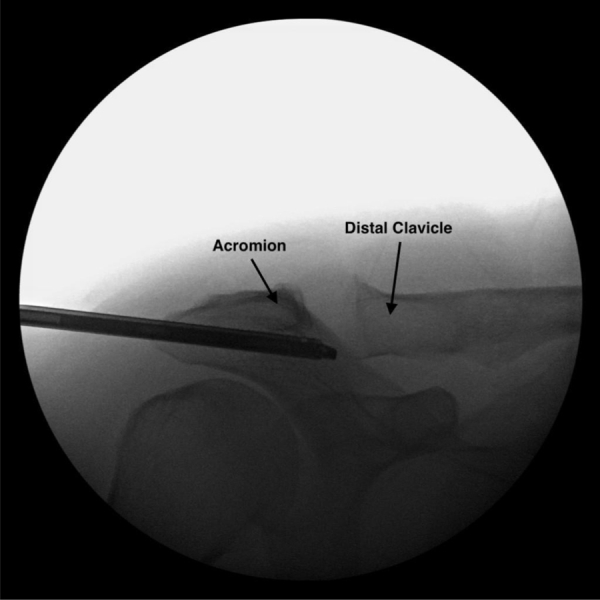
Fig 10.
Patient positioned in the beach chair position. Intraoperative radiograph displaying Kirschner (K) wire placement and remaining clavicle after complete resection of the distal clavicle. Approximately 7 mm of distal clavicle is excised as shown by the space in the acromioclavicular joint from the acromion to the K-wire.
Final Examination and Postoperative Care
Fluoroscopic imaging of the AC joint is obtained to confirm an even resection and smooth vertical surface of the distal clavicle and intact superior AC joint capsule and coracoclavicular ligaments (Fig 11). The arthroscopic incisions are closed with 3-0 nylon. The patient is placed in an abductor sling for 1 week with formal physical therapy to commence thereafter. Pearls and pitfalls of the procedure are described in Table 1.
Fig 11.
Patient positioned in the beach chair position. Postoperative radiograph of the right acromioclavicular joint, anterior view, showing a complete 7-mm resection of the distal clavicle.
Table 1.
Pearls and Pitfalls of Arthroscopic Distal Clavicle Excision for AC-Joint Osteoarthritis Using a Fluoroscopic K-Wire Guide
| Pearls |
|---|
|
|
|
| Pitfalls |
|
|
|
AC, acromioclavicular; K, Kirschner.
Discussion
Both open and arthroscopic methods for DCE provide effective treatment for AC joint osteoarthritis.1 Open resections provide improved visualization of the acromion and distal clavicle, allowing for more precise excisions but carry increased risk for scar formation, infection, and damage to the deltoid muscles, as well as surrounding capsular and ligamentous structures.5,9,10 The different arthroscopic approaches also come with varied results with the direct approach, allowing for faster return to activity and better visualization while the indirect approach avoids possible damage of the surrounding ligaments.16,17,21,22
Flatow et al. describe the direct arthroscopic resection using a superior approach, which allows for more precise localization of the AC joint and faster recovery compared with the indirect method.15,21 However, similar to the open procedure, this method poses a potential risk to the surrounding AC capsular ligaments and specifically to the superior capsular ligament due to the portals introduced through the ligament.18,22,23 This is concerning because the AC ligaments and joint capsule are the primary restraints to horizontal translation.5,19 Damage to the AC capsular ligaments with subsequent joint instability can lead to increased postoperative pain.22,24, 25, 26
The indirect arthroscopic resection instead uses standard arthroscopic portals and resects the inferior distal clavicle cortex through the subacromial space, reducing the risk of damaging AC capsular ligaments.17 Although the indirect approach theoretically allows for the best preservation of the AC capsule and its ligaments, no significant difference has been found in postoperative strength or clavicular stability between the arthroscopic techniques.19,21,22 In addition, Amirtharaj et al. report a 7.6% complication rate for arthroscopic methods derived from incomplete resections.20,27,28 Under- and over-resection (<5 mm and >15 mm) have been identified as the most common errors leading to DCE failure and revision surgery.14,26 Inaccurate resection from lack of depth perception and inadequate visualization has been reported to be more common among arthroscopic procedures.26
The described technique in this Technical Note attempts to remedy the challenges of indirect arthroscopic resection while avoiding the risk of a superior arthroscopic approach. K-wire placement allows for direct guidance during resection and helps avoid under- and over-resection. In addition, the benefits of indirect arthroscopic resection in avoiding the AC capsular ligaments still hold. However, a subacromial decompression must be performed before the indirect DCE to provide the visualization necessary to access the inferior distal clavicle. Another disadvantage of the described technique is the potential risk of iatrogenic injury to structures during K-Wire placement. This risk is reduced by clearly marking out bony landmarks before the case and careful advancement of the K-wire during the procedure. Advantages and disadvantages of the procedures are listed in Table 2.
Table 2.
Advantages and Disadvantages of Arthroscopic Distal Clavicle Excision for AC Joint Osteoarthritis Using a Fluoroscopic K-Wire Guide
| Advantages |
|---|
|
|
|
| Disadvantages |
|
|
|
AC, acromioclavicular; K, Kirschner.
The purpose of this Technical Note and accompanying video is to show how to implement a fluoroscopic K-wire guide for an arthroscopic DCE using an indirect subacromial approach. Once K-wire placement is successful, the procedure is far more likely to accomplish an accurate resection. This is especially useful for new orthopaedic surgeons adjusting to arthroscopic procedures for an otherwise technically demanding procedure.27,28
Footnotes
The authors report the following potential conflicts of interest or sources of funding: J.L.C. is an educational consultant for Arthrex and receives compensation for medical educational lectures and instruction only. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Distal clavicle excision for acromioclavicular joint osteoarthritis using a fluoroscopic Kirschner (K) wire guide. Preoperative magnetic resonance imaging of the right shoulder in the anteroposterior view confirms osteoarthritis of the AC joint. A blunt trocar and scope sheath are placed in line with the AC joint to obtain access to the AC joint. An 18-gauge spinal needle is placed perpendicular to the lateral end of the distal clavicle and an electrocautery is used to clean up the AC joint. The mobile distal clavicle is observable and clear. A ruler is used to measure 7 mm medially from the spinal needle to the distal clavicle. The 1.5-mm K-wire is then fired into the distal clavicle perpendicular to the distal clavicle and parallel to the spinal needle. Radiographs confirm the proper positioning of the K-wire and then the spinal needle is removed. A 5-mm burr is introduced and begins resection of the distal clavicle from the anterior portal. Resection continues until the K-wire comes into view. Once the entire K-wire is observable, a fluoroscopic image is taken to confirm the 7 mm excision using a K-wire. (AC, acromioclavicular.)
References
- 1.Docimo S., Kornitsky D., Futterman B., Elkowitz D.E. Surgical treatment for acromioclavicular joint osteoarthritis: Patient selection, surgical options, complications, and outcome. Curr Rev Musculoskelet Med. 2008;1:154–160. doi: 10.1007/s12178-008-9024-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Buttaci C.J., Stitik T.P., Yonclas P.P., Foye P.M. Osteoarthritis of the acromioclavicular joint: A review of anatomy, biomechanics, diagnosis, and treatment. Am J Phys Med Rehabil. 2004;83:791–797. doi: 10.1097/01.phm.0000140804.46346.93. [DOI] [PubMed] [Google Scholar]
- 3.Auge W.K., Fischer R.A. Arthroscopic distal clavicle resection for isolated atraumatic osteolysis in weight lifters. Am J Sports Med. 1998;26:189–192. doi: 10.1177/03635465980260020701. [DOI] [PubMed] [Google Scholar]
- 4.Frigg A., Song D., Willi J., Freiburghaus A.U., Grehn H. Seven-year course of asymptomatic acromioclavicular osteoarthritis diagnosed by MRI. J Shoulder Elbow Surg. 2019;28:e344–e351. doi: 10.1016/j.jse.2019.04.004. [DOI] [PubMed] [Google Scholar]
- 5.Lervick G.N. Direct arthroscopic distal clavicle resection: A technical review. Iowa Orthop J. 2005;25:149–156. [PMC free article] [PubMed] [Google Scholar]
- 6.Hohmann E., Tetsworth K., Glatt V. Open versus arthroscopic acromioclavicular joint resection: A systematic review and meta-analysis. Arch Orthop Trauma Surg. 2019;139:685–694. doi: 10.1007/s00402-019-03114-w. [DOI] [PubMed] [Google Scholar]
- 7.DeFroda S.F., Nacca C., Waryasz G.R., Owens B.D. Diagnosis and management of distal clavicle osteolysis. Orthopedics. 2017;40:119–124. doi: 10.3928/01477447-20161128-03. [DOI] [PubMed] [Google Scholar]
- 8.Mumford E.B. Acromioclavicular dislocation: a new operative treatment. J Bone Joint Surg. 1941;23:799–802. [Google Scholar]
- 9.Elhassan B., Ozbaydar M., Diller D., Massimini D., Higgins L.D., Warner J.J.P. Open versus arthroscopic acromioclavicular joint resection: A retrospective comparison study. Arthroscopy. 2009;25:1224–1232. doi: 10.1016/j.arthro.2009.06.010. [DOI] [PubMed] [Google Scholar]
- 10.Chronopoulos E., Gill H.S., Freehill M.T., Petersen S.A., McFarland E.G. Complications after open distal clavicle excision. Clin Orthop. 2008;466:646–651. doi: 10.1007/s11999-007-0084-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rabalais R.D., McCarty E. Surgical treatment of symptomatic acromioclavicular joint problems: A systematic review. Clin Orthop. 2007;455:30–37. doi: 10.1097/BLO.0b013e31802f5450. [DOI] [PubMed] [Google Scholar]
- 12.Matthews L.S., Parks B.G., Pavlovich L.J., Giudice M.A. Arthroscopic versus open distal clavicle resection: A biomechanical analysis on a cadaveric model. Arthroscopy. 1999;15:237–240. doi: 10.1016/s0749-8063(99)70027-7. [DOI] [PubMed] [Google Scholar]
- 13.Eskola A., Santavirta S., Viljakka H.T., Wirta J., Partio T.E., Hoikka V. The results of operative resection of the lateral end of the clavicle. J Bone Joint Surg Am. 1996;78:584–587. doi: 10.2106/00004623-199604000-00013. [DOI] [PubMed] [Google Scholar]
- 14.Hohmann E., Shea K., Scheiderer B., Millett P., Imhoff A. Indications for arthroscopic subacromial decompression. A level V evidence clinical guideline. Arthroscopy. 2020;36:913–922. doi: 10.1016/j.arthro.2019.06.012. [DOI] [PubMed] [Google Scholar]
- 15.Flatow E.L., Duralde X.A., Nicholson G.P., Pollock R.G., Bigliani L.U. Arthroscopic resection of the distal clavicle with a superior approach. J Shoulder Elbow Surg. 1995;4:41–50. doi: 10.1016/s1058-2746(10)80007-2. [DOI] [PubMed] [Google Scholar]
- 16.Snyder S.J., Banas M.P., Karzel R.P. The arthroscopic Mumford procedure: An analysis of results. Arthroscopy. 1995;11:157–164. doi: 10.1016/0749-8063(95)90061-6. [DOI] [PubMed] [Google Scholar]
- 17.Pensak M., Grumet R.C., Slabaugh M.A., Bach B.R. Open versus arthroscopic distal clavicle resection. Arthroscopy. 2010;26:697–704. doi: 10.1016/j.arthro.2009.12.007. [DOI] [PubMed] [Google Scholar]
- 18.Edwards S.L., Wilson N.A., Flores S.E., Koh J.L., Zhang L.-Q. Arthroscopic distal clavicle resection: A biomechanical analysis of resection length and joint compliance in a cadaveric model. Arthroscopy. 2007;23:1278–1284. doi: 10.1016/j.arthro.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 19.Miller C.A., Ong B.C., Jazrawi L.M., Joseph T., Heywood C.S., Rosen J., Rokito A.S. Assessment of clavicular translation after arthroscopic Mumford procedure: Direct versus indirect resection—A cadaveric study. Arthroscopy. 2005;21:64–68. doi: 10.1016/j.arthro.2004.09.017. [DOI] [PubMed] [Google Scholar]
- 20.Duindam N., Kuiper J.W.P., Hoozemans M.J.M., Burger B.J. Comparison between open and arthroscopic procedures for lateral clavicle resection. Int Orthop. 2014;38:783–789. doi: 10.1007/s00264-013-2161-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Charron K.M., Schepsis A.A., Voloshin I. Arthroscopic distal clavicle resection in athletes: A prospective comparison of the direct and indirect approach. Am J Sports Med. 2007;35:53–58. doi: 10.1177/0363546506294855. [DOI] [PubMed] [Google Scholar]
- 22.Kay S.P., Dragoo J.L., Lee R. Long-term results of arthroscopic resection of the distal clavicle with concomitant subacromial decompression. Arthroscopy. 2003;19:805–809. doi: 10.1016/s0749-8063(03)00682-0. [DOI] [PubMed] [Google Scholar]
- 23.Levine W.N., Soong M., Ahmad C.S., Blaine T.A., Bigliani L.U. Arthroscopic distal clavicle resection: A comparison of bursal and direct approaches. Arthroscopy. 2006;22:516–520. doi: 10.1016/j.arthro.2006.01.013. [DOI] [PubMed] [Google Scholar]
- 24.Corteen D.P., Teitge R.A. Stabilization of the clavicle after distal resection: A biomechanical study. Am J Sports Med. 2005;33:61–67. doi: 10.1177/0363546504268038. [DOI] [PubMed] [Google Scholar]
- 25.Blazar P.E., Iannotti J.P., Williams G.R. Anteroposterior instability of the distal clavicle after distal clavicle resection. Clin Orthop. 1998;348:114–120. [PubMed] [Google Scholar]
- 26.Strauss E.J., Barker J.U., McGill K., Verma N.N. The evaluation and management of failed distal clavicle excision. Sports Med Arthrosc Rev. 2010;18:213–219. doi: 10.1097/JSA.0b013e3181e892da. [DOI] [PubMed] [Google Scholar]
- 27.Amirtharaj M.J., Wang D., McGraw M.H., Camp C.L., Degen R.A., Dines D.M., Dines J.S. Trends in the surgical management of acromioclavicular joint arthritis among board-eligible US orthopaedic surgeons. Arthroscopy. 2018;34:1799–1805. doi: 10.1016/j.arthro.2018.01.024. [DOI] [PubMed] [Google Scholar]
- 28.Burns J. Editorial Commentary: The “Mumford” & Sons: For distal clavicle excisions, what are our young surgeons doing, and how well are they doing it? Arthroscopy. 2018;34:1806–1808. doi: 10.1016/j.arthro.2018.03.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Distal clavicle excision for acromioclavicular joint osteoarthritis using a fluoroscopic Kirschner (K) wire guide. Preoperative magnetic resonance imaging of the right shoulder in the anteroposterior view confirms osteoarthritis of the AC joint. A blunt trocar and scope sheath are placed in line with the AC joint to obtain access to the AC joint. An 18-gauge spinal needle is placed perpendicular to the lateral end of the distal clavicle and an electrocautery is used to clean up the AC joint. The mobile distal clavicle is observable and clear. A ruler is used to measure 7 mm medially from the spinal needle to the distal clavicle. The 1.5-mm K-wire is then fired into the distal clavicle perpendicular to the distal clavicle and parallel to the spinal needle. Radiographs confirm the proper positioning of the K-wire and then the spinal needle is removed. A 5-mm burr is introduced and begins resection of the distal clavicle from the anterior portal. Resection continues until the K-wire comes into view. Once the entire K-wire is observable, a fluoroscopic image is taken to confirm the 7 mm excision using a K-wire. (AC, acromioclavicular.)
Distal clavicle excision for acromioclavicular joint osteoarthritis using a fluoroscopic Kirschner (K) wire guide. Preoperative magnetic resonance imaging of the right shoulder in the anteroposterior view confirms osteoarthritis of the AC joint. A blunt trocar and scope sheath are placed in line with the AC joint to obtain access to the AC joint. An 18-gauge spinal needle is placed perpendicular to the lateral end of the distal clavicle and an electrocautery is used to clean up the AC joint. The mobile distal clavicle is observable and clear. A ruler is used to measure 7 mm medially from the spinal needle to the distal clavicle. The 1.5-mm K-wire is then fired into the distal clavicle perpendicular to the distal clavicle and parallel to the spinal needle. Radiographs confirm the proper positioning of the K-wire and then the spinal needle is removed. A 5-mm burr is introduced and begins resection of the distal clavicle from the anterior portal. Resection continues until the K-wire comes into view. Once the entire K-wire is observable, a fluoroscopic image is taken to confirm the 7 mm excision using a K-wire. (AC, acromioclavicular.)