Abstract
Superior capsule reconstruction has gained popularity as a treatment option for massive rotator cuff tears. The initial graft described was a tensor fascia lata. In the United States, acellular dermal matrix or dermal allograft has gained popularity. The results from published reports have been promising, but graft tear on postoperative imaging has been reported in several studies. Strives are being made to reduce the graft tear rate. One such way is to increase the thickness of the graft. Biomechanical studies have shown that thicker and stiffer grafts perform better in restoring superior stability. We present a technique of doubling a commercially available 3 mm dermal allograft and making it into a 6 mm graft for superior capsule reconstruction.
Technique Video
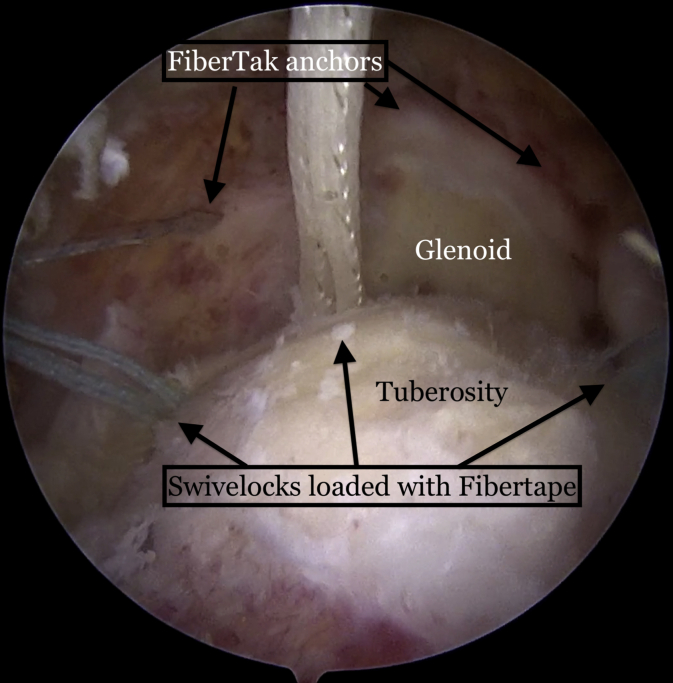
This is a left shoulder, viewing from the anterolateral portal demonstrating a massive rotator cuff tear. Three knotless FiberTak anchors (Arthrex) are placed percutaneously in the glenoid at the 10, 12, and 2 o’clock positions. Three SwiveLock anchors (Arthrex), loaded with FiberTape (Arthrex), are placed in the medial row of the greater tuberosity. A 4 × 7 cm, 3mm–thick ArthroFlex dermal allograft (LifeNet Health) is folded over, and the free edges are sutured together with SutureTape (Arthrex). FiberLink sutures (Arthrex) are then passed to allow easier passage of the FiberTapes once they are brought out the cannula. The thick graft will not fit through a commercially available cannula, so a 20 mL syringe is used, with the end cut off, to allow passage of the graft. The repair stitch and the loop stitch from the FiberTak anchor are brought out of the syringe. The repair stitch is then passed through the graft 5 mm from the medial edge, with a reverse cutting needle in a mattress fashion. The repair stitch is then passed through the loop of the shuttle loop stitch, and the corresponding SutureTape pull stitch from the same anchor is pulled percutaneously until the repair stitch passes through the anchor and can no longer back out. The steps are repeated individually for each anchor until all three mattress stitches are passed on the medial side of the graft. The FiberTapes from each medial row anchor are then brought out of the syringe cannula and kept separated. The FiberTapes from the medial row are placed 15 mm from the lateral edge of the graft approximately 7 mm to 10 mm apart with the previously placed FiberLink sutures. The side to side SutureTapes should also be passed before bringing the graft into the SAS. The graft is folded and introduced into the syringe. The pull stitches of each of the three FiberTaks are pulled percutaneously, thus pulling the graft into the subacromial space (SAS). As the graft advances into the SAS, the FiberTapes tend to bunch up, so the tails of the FiberTapes should also be pulled laterally to take the slack out of them. Once the graft is fully reduced and fixed medially, a suture grasping device is passed through the infraspinatus and the side to side SutureTape is grasped and passed through the tendon. This is also repeated anteriorly for the subscapularis. The side-to-side sutures are then tied and cut. The lateral row is then addressed by grasping a FiberTape limb from the posterior anchor and one FiberTape from the middle anchor and fixed laterally with SwiveLock anchors. The process is repeated with the other three anchors and a transosseous equivalent double row repair is achieved.
Massive rotator cuff tears are a challenging problem to treat, and superior capsule reconstruction (SCR) has gained popularity as a treatment option. Tensor fascia lata grafting was initially described by Teruhisa Mihata in his pioneering procedure.1 In the United States, acellular dermal matrix or dermal allograft has gained popularity.2 The clinical results from published reports have been promising, but graft tear has been reported in several studies.3,4 Attempts at reducing the graft tear rate are being made. One such way is to increase the thickness of the graft because biomechanical studies have shown that thicker and stiffer grafts perform better in restoring superior stability.5, 6, 7, 8 We present a technique of doubling a commercially available 3 mm dermal allograft and making it into a 6 mm graft. Table 1 summarizes the advantages and disadvantages, and Table 2 summarizes pearls and pitfalls of this technique.
Table 1.
Advantages and Disadvantages
| Advantages |
|
|
|
| Disadvantages |
|
|
|
Table 2.
Pearls and Pitfalls
| Pearls |
|
|
|
|
|
|
|
|
| Pitfalls |
|
|
|
Arthrex.
Technique
A standard diagnostic arthroscopy from the posterior viewing portal is performed with the patient in the lateral decubitus position (Video 1). The subacromial space (SAS) is debrided, and the greater tuberosity is prepared by removing soft tissue remnants and roughening the bone to a bleeding surface. Three knotless FiberTak anchors (Arthrex) are percutaneously placed using stab incisions in the superior glenoid at 10, 12, and 2 o’clock positions (Fig 1). Two to 3 BioComposite SwiveLock anchors (Arthrex) loaded with FiberTape (Arthrex) are then inserted into the medial row just lateral to the articular margin (Fig 1).
Fig 1.
Patient in lateral decubitus position with a lateral view of a left shoulder demonstrating 3 FiberTak anchors (Arthrex) placed into the glenoid at the 10, 12, and 2 o’clock positions and 3 SwiveLock anchors (Arthrex) in the medial row of the greater tuberosity
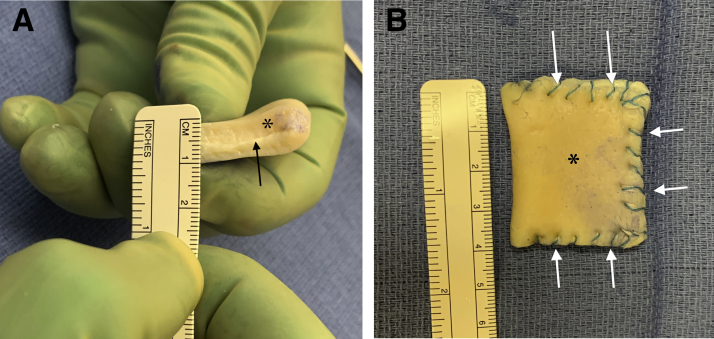
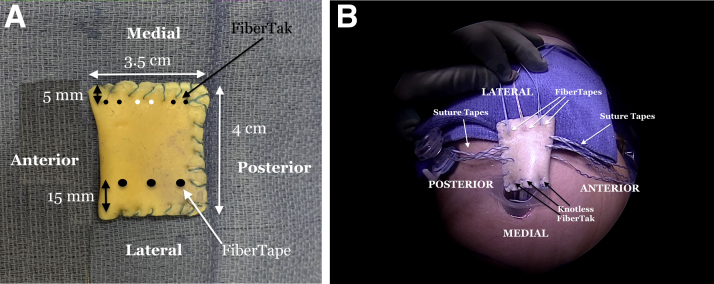
A 4 × 7 cm, 3 mm thick, dermal allograft (ArthroFlex 301, LifeNet Health) is folded over to attain a minimum 6 mm thick graft (Fig 2A). The edges are sutured together with SutureTape (Arthrex) (Fig 2B). A schematic of where suture passage occurs in the graft is shown in Fig 3. The repair stitch from the FiberTak anchors are passed in a mattress fashion approximately 5 mm from the medial edge of the doubled graft (small circles), and the FiberTapes from the medial row of the humeral head are passed approximately 15 mm from the lateral edge of the graft (large circles) (Fig 3A). Side-to-side SutureTapes (Arthrex) are also passed on the anterior edge (for repair to the subscapularis) and the posterior edge (for repair to the infraspinatus) (Fig 3B).
Fig 2.
(A) A 3mm dermal allograft (∗) folded over showing a thick final graft. Arrow pointing to the folded center of the graft. (B) The free edges of the graft (∗) are sutured together with SutureTape (Arthrex) (white arrows).
Fig 3.
A. Diagram showing where the FiberTak (small black and white dots) sutures will be passed in a mattress fashion 5 mm from the medial edge of the graft approximately 5 mm apart. The FiberTapes will be passed through 15 mm from the lateral edge of the graft approximately 8-10 mm apart. B. View of the graft placed over the left shoulder once all the sutures have been passed through it. The additional SutureTapes on the anterior and posterior sides are for side-to-side suturing of the graft to the subscapularis and infraspinatus, respectively.
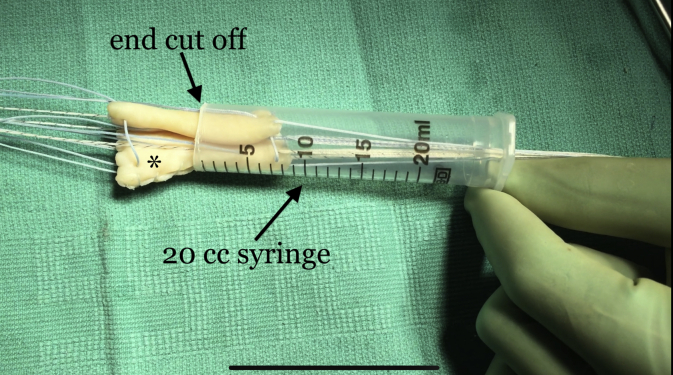
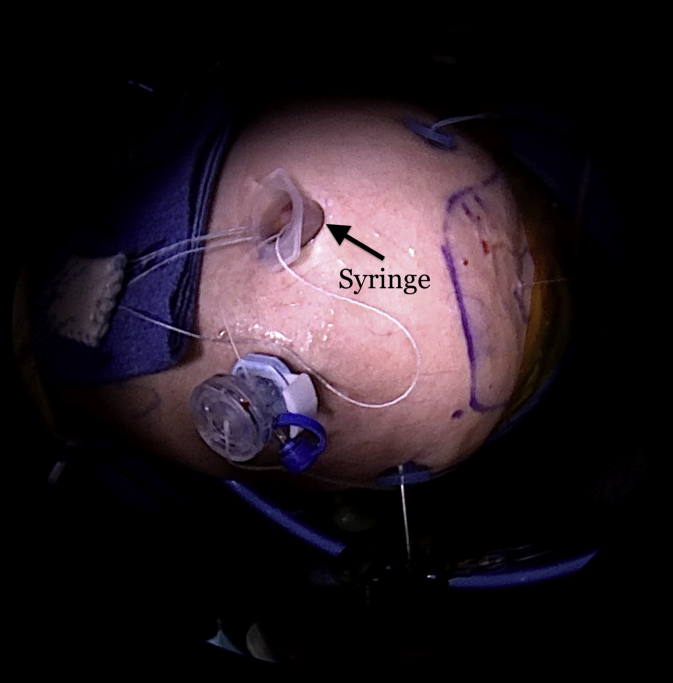
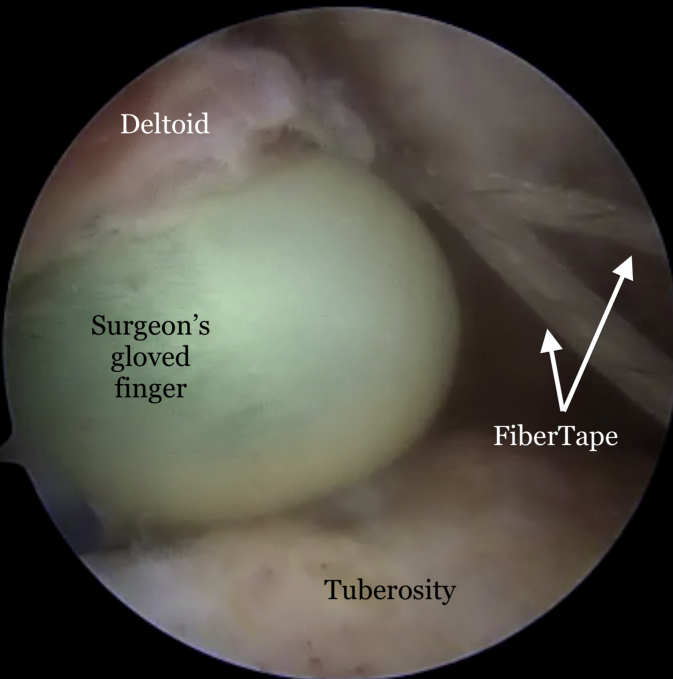
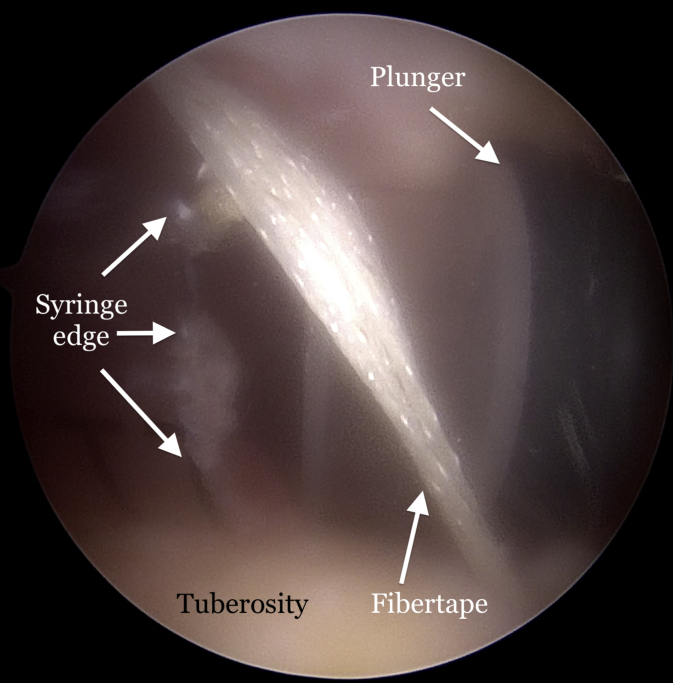
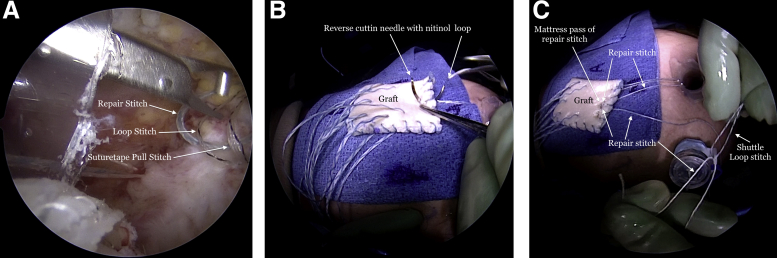
The prepared graft is too large to pass through commercially available cannulas, so a 20 mL syringe is fashioned by cutting the tip end of the syringe with a sharp knife or sterile bandage-cutting scissors (Fig 4). The anterolateral working portal is extended to approximately 1.5 cm in length or large enough to allow the syringe to be placed into the SAS (Fig 5). Dilation with digital probing can split the deltoid fibers to allow for easier syringe placement (Fig 6), and the syringe plunger is left in the syringe during insertion to act as a trocar (Fig 7). The pump pressure is maintained and does not need to be increased. If any actively bleeding vessels are noted, they should be cauterized before syringe cannula placement. The repair stitch and shuttle loop from the posterior FiberTak anchor are then brought out of the syringe (Fig 8A). The repair stitch is passed through the graft using a reverse cutting free needle with a nitinol loop in a mattress fashion, 5 mm from edge of graft and 5 to 7 mm apart from each other (Fig 8B). The repair stitch is then passed through the shuttle loop, folded over and crimped (Fig 8C). The corresponding SutureTape pull stitch from the same anchor is pulled percutaneously until the repair stitch passes through the anchor and can no longer back out. This process is repeated one anchor at a time, 12 to 15 mm apart from each other, to avoid suture scrambling in the syringe. The FiberTapes from the medial row anchors are then brought out the syringe and passed through the graft using the preloaded FiberLink sutures (Fig 3B). After the FiberTapes have been passed through the graft, the three pull stitches from the FiberTak anchors are then sequentially pulled thus pulling the graft into the SAS. As the graft enters, the FiberTapes can bunch up and therefore, occasionally the FiberTape tails need to be tensioned out of the syringe to remove the slack from SAS and allow better visualization. Once the FiberTak sutures are firmly tightened up and the glenoid end of the graft is secured, the suture grasping device is used to pass the SutureTape through the infraspinatus and subscapularis to achieve side to side repairs. Last, a transosseous equivalent repair is achieved with the FiberTapes in the lateral row using 4.75 mm SwiveLock anchors (Fig 9). Postoperative magnetic resonance imaging (MRI) demonstrates full healing and integration of the graft at a mean of 6 months (Fig 10). There have been no cases of seroma formation between the 2 layers.
Fig 4.
A 20 mL syringe is used as a cannula to deliver the graft into the subacromial space. The tip of the syringe is cut with a sharp surgical knife or bandage-cutting scissors.
Fig 5.
External view of the posterior aspect of the left shoulder with patient in lateral decubitus position demonstrating the syringe placement in the anterolateral working portal. The initial portal is extended distally approximately 1.5 cm to allow syringe placement. Once the graft is passed, the syringe is removed, a standard cannula placed, and the inferior portal incision is sutured to hold the cannula.
Fig 6.
View of left shoulder from posterior portal demonstrating the surgeon’s finger creating a path for the cannula to be placed into the subacromial space by a deltoid splitting approach.
Fig 7.
View of left shoulder from posterior portal demonstrating the plunger of the syringe to act as a trocar and allow placement into subacromial space.
Fig 8.
(A) View of left shoulder from posterior portal demonstrating the repair stitch and the loop stitch being brought out the syringe (one anchor at a time for suture management). the pull stitch is left is a percutaneous position to be used later to pull the graft into the subacromial space. (B) External view of the posterior aspect of the left shoulder with patient in lateral decubitus position with the repair stitch being passed through the graft with a reverse cutting free needle with a nitinol suture eyelet. Do not use suture passing devices in this step as the graft thickness prevents the needle passage from such devices. (C) External view of the posterior aspect of the left shoulder with patient in lateral decubitus position with the repair stitch, once passed in a mattress fashion through the graft, then passed through the loop of the shuttle loop stitch. The pull stitch from the same anchor is then pulled, bringing the repair stitch into the anchor, which then acts to prevent it from backing out.
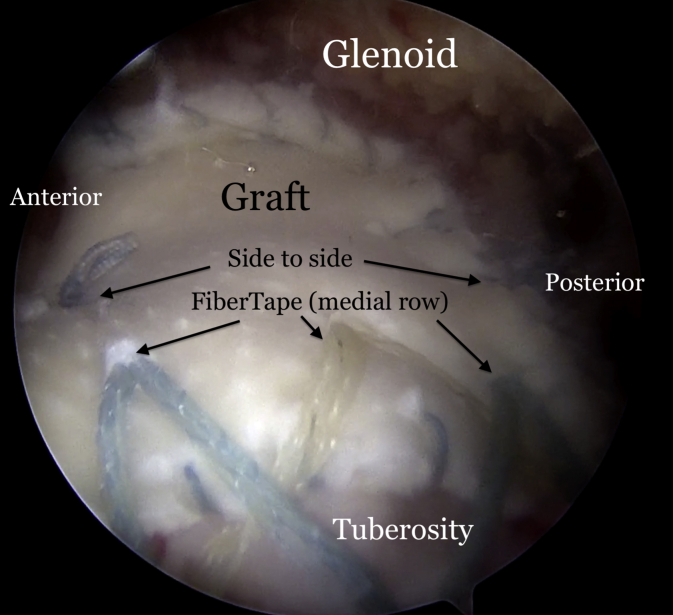
Fig 9.
View of left shoulder from the anterolateral portal showing the doubled-over graft fixated medially to the glenoid and laterally with a transosseous equivalent technique and side-to-side sutures.
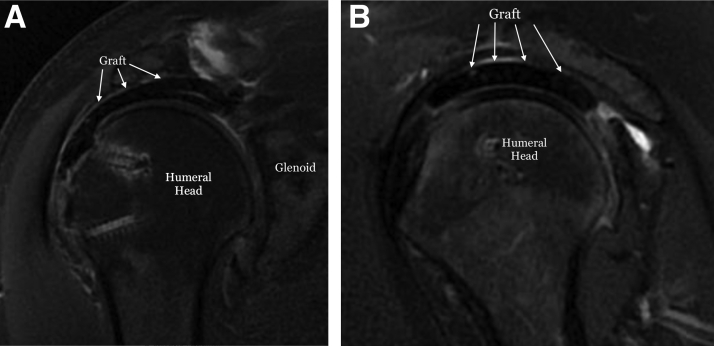
Fig 10.
(A) T2-weighted, coronal oblique magnetic resonance imaging (MRI) scan 6 months after surgery of a doubled-over dermal allograft used in superior capsule reconstruction showing healing of the graft to the glenoid and tuberosity. Note there is no seroma collection between the two layers. (B) T2-weighted sagittal oblique MRI scan showing the doubled-over graft (white arrows) 6 months after procedure.
Rehabilitation Protocol
The arm is placed in a padded immobilizer for the first 6 weeks, removing it for hygiene and for hand/wrist/elbow range of motion exercises. Codman exercises are initiated at 3 weeks. Active and active-assist range of motion is initiated with scapular stabilization between 6 and 12 weeks. At 12 weeks, full pain-free active range of motion should be attainable. It is at this phase when the graft is at its weakest point, and care should be taken not to aggressively strengthen the shoulder girdle muscles, and patients should be cautioned not to overuse their shoulder because most feel pain-free and have returned to most activities of daily living. Strengthening should be initiated at 4 to 6 months after surgery.
Discussion
Superior capsule reconstruction was introduced by Teruhisa Mihata to address a challenging problem for shoulder surgeons.1 The original description used autologous fascia lata as a graft, with superior clinical results, as well as low tear rates on postoperative imaging.9 In the United States, acellular dermal allograft has become the popular graft of choice.2, 3, 4 Significant clinical and functional improvements have been reported with the use of dermal allografts.4,10 However, graft tears have been reported anywhere from 50%11 to 75%.10 Denard et al.4 reported on 59 patients who underwent SCR with a dermal allograft. Of those, 20 patients underwent an MRI with 11 (55%) demonstrating a graft tear. Pennington et al.10 reported results on 88 patients who underwent SCR. Only 4 (4.5%) patients underwent MRI, 3 (75%) of whom demonstrated a tear from the tuberosity. Lacheta et al.11 reported on 22 SCR patients, 20 (91%) of whom had a postoperative MRI. Of those, 10 had an intact graft, and 10 (50%) had either a midsubstance tear or a tear from the glenoid. Patients with healed and intact grafts have better functional outcomes than those with a tear,3,4,12 so attempts need to be made to improve graft integrity rates.
One such way is to increase the thickness of the graft being used as graft thickness and stiffness play an important role in superior stability of the glenohumeral joint.6, 7, 8 Nimura et al.13 have shown that the normal thickness of the native superior capsule is 4.4 to 9.1 mm. Mihata et al.,9 in his original technique, used fascia lata autograft, folded multiple times to achieve a thickness of 6.1 to 8 mm. In a biomechanical study, Mihata et al.7 found that 8 mm fascia lata grafts restored superior stability in a massive rotator cuff tear shoulder model better than 4 mm grafts. In another study, Mihata et al.8 compared an 8 mm TFL to a 3.3 mm human dermal allograft and found fascia lata restored superior translation of the humerus better than dermal allograft. The authors also found that the dermal allograft elongated by 15% whereas the fascia lata did not change in dimensions. Denard et al.4 also reported that although the overall success rate in their series was 68%, the success rate with the use of 1 mm grafts was only 40%.
As a result of these biomechanical and clinical findings, we chose to fold a commercially available 3 mm dermal allograft, thickening it to a 6 mm graft, to perform superior capsule reconstruction. We have seen promising results in our initial 10 patients with only 1 graft tear on postoperative MRI, but further investigation is warranted with larger numbers to draw significant conclusions.
Footnotes
The authors report the following potential conflict of interest or source of funding: R.M. received grants and personal fees from Arthrex. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This is a left shoulder, viewing from the anterolateral portal demonstrating a massive rotator cuff tear. Three knotless FiberTak anchors (Arthrex) are placed percutaneously in the glenoid at the 10, 12, and 2 o’clock positions. Three SwiveLock anchors (Arthrex), loaded with FiberTape (Arthrex), are placed in the medial row of the greater tuberosity. A 4 × 7 cm, 3mm–thick ArthroFlex dermal allograft (LifeNet Health) is folded over, and the free edges are sutured together with SutureTape (Arthrex). FiberLink sutures (Arthrex) are then passed to allow easier passage of the FiberTapes once they are brought out the cannula. The thick graft will not fit through a commercially available cannula, so a 20 mL syringe is used, with the end cut off, to allow passage of the graft. The repair stitch and the loop stitch from the FiberTak anchor are brought out of the syringe. The repair stitch is then passed through the graft 5 mm from the medial edge, with a reverse cutting needle in a mattress fashion. The repair stitch is then passed through the loop of the shuttle loop stitch, and the corresponding SutureTape pull stitch from the same anchor is pulled percutaneously until the repair stitch passes through the anchor and can no longer back out. The steps are repeated individually for each anchor until all three mattress stitches are passed on the medial side of the graft. The FiberTapes from each medial row anchor are then brought out of the syringe cannula and kept separated. The FiberTapes from the medial row are placed 15 mm from the lateral edge of the graft approximately 7 mm to 10 mm apart with the previously placed FiberLink sutures. The side to side SutureTapes should also be passed before bringing the graft into the SAS. The graft is folded and introduced into the syringe. The pull stitches of each of the three FiberTaks are pulled percutaneously, thus pulling the graft into the subacromial space (SAS). As the graft advances into the SAS, the FiberTapes tend to bunch up, so the tails of the FiberTapes should also be pulled laterally to take the slack out of them. Once the graft is fully reduced and fixed medially, a suture grasping device is passed through the infraspinatus and the side to side SutureTape is grasped and passed through the tendon. This is also repeated anteriorly for the subscapularis. The side-to-side sutures are then tied and cut. The lateral row is then addressed by grasping a FiberTape limb from the posterior anchor and one FiberTape from the middle anchor and fixed laterally with SwiveLock anchors. The process is repeated with the other three anchors and a transosseous equivalent double row repair is achieved.
References
- 1.Mihata T., McGarry M.H., Pirolo J.M., Kinoshita M., Lee T.Q. Superior capsule reconstruction to restore superior stability in irreparable rotator cuff tears: a biomechanical cadaveric study. Am J Sports Med. 2012;40:2248–2255. doi: 10.1177/0363546512456195. [DOI] [PubMed] [Google Scholar]
- 2.Tokish J.M., Beicker C. Superior capsule reconstruction technique using an acellular dermal allograft. Arthrosc Tech. 2015;4:e833–e839. doi: 10.1016/j.eats.2015.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mirzayan R., Stone M.A., Batech M., Acevedo D.C., Singh A. Failed dermal allograft procedures for irreparable rotator cuff tears can still improve pain and function: the “biologic tuberoplasty effect”. Orthop J Sports Med. 2019;7 doi: 10.1177/2325967119863432. 2325967119863432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Denard P.J., Brady P.C., Adams C.R., Tokish J.M., Burkhart S.S. Preliminary results of arthroscopic superior capsule reconstruction with dermal allograft. Arthroscopy. 2018;34:93–99. doi: 10.1016/j.arthro.2017.08.265. [DOI] [PubMed] [Google Scholar]
- 5.Scheiderer B., Kia C., Obopilwe E. Biomechanical effect of superior capsule reconstruction using a 3-mm and 6-mm thick acellular dermal allograft in a dynamic shoulder model. Arthroscopy. 2020;36:355–364. doi: 10.1016/j.arthro.2019.08.026. [DOI] [PubMed] [Google Scholar]
- 6.Mihata T. Editorial commentary: Superior capsule reconstruction: grafts for superior capsular reconstruction must be thick and stiff. Arthroscopy. 2019;35:2535–2536. doi: 10.1016/j.arthro.2019.04.019. [DOI] [PubMed] [Google Scholar]
- 7.Mihata T., McGarry M.H., Kahn T., Goldberg I., Neo M., Lee T.Q. Biomechanical effect of thickness and tension of fascia lata graft on glenohumeral stability for superior capsule reconstruction in irreparable supraspinatus tears. Arthroscopy. 2016;32:418–426. doi: 10.1016/j.arthro.2015.08.024. [DOI] [PubMed] [Google Scholar]
- 8.Mihata T., Bui C.N.H., Akeda M. A biomechanical cadaveric study comparing superior capsule reconstruction using fascia lata allograft with human dermal allograft for irreparable rotator cuff tear. J Shoulder Elbow Surg. 2017;26:2158–2166. doi: 10.1016/j.jse.2017.07.019. [DOI] [PubMed] [Google Scholar]
- 9.Mihata T., Lee T.Q., Watanabe C. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013;29:459–470. doi: 10.1016/j.arthro.2012.10.022. [DOI] [PubMed] [Google Scholar]
- 10.Pennington W.T., Bartz B.A., Pauli J.M., Walker C.E., Schmidt W. Arthroscopic superior capsular reconstruction with acellular dermal allograft for the treatment of massive irreparable rotator cuff tears: short-term clinical outcomes and the radiographic parameter of superior capsular distance. Arthroscopy. 2018;34:1764–1773. doi: 10.1016/j.arthro.2018.01.009. [DOI] [PubMed] [Google Scholar]
- 11.Lacheta L., Horan M.P., Schairer W.W. Clinical and imaging outcomes after arthroscopic superior capsule reconstruction with human dermal allograft for irreparable posterosuperior rotator cuff tears: a minimum 2-year follow-up. Arthroscopy. 2020;36:1011–1019. doi: 10.1016/j.arthro.2019.12.024. [DOI] [PubMed] [Google Scholar]
- 12.Lim S., AlRamadhan H., Kwak J.M., Hong H., Jeon I.H. Graft tears after arthroscopic superior capsule reconstruction (ASCR): pattern of failure and its correlation with clinical outcome. Arch Orthop Trauma Surg. 2019;139:231–239. doi: 10.1007/s00402-018-3025-7. [DOI] [PubMed] [Google Scholar]
- 13.Nimura A., Kato A., Yamaguchi K. The superior capsule of the shoulder joint complements the insertion of the rotator cuff. J Shoulder Elbow Surg. 2012;21:867–872. doi: 10.1016/j.jse.2011.04.034. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This is a left shoulder, viewing from the anterolateral portal demonstrating a massive rotator cuff tear. Three knotless FiberTak anchors (Arthrex) are placed percutaneously in the glenoid at the 10, 12, and 2 o’clock positions. Three SwiveLock anchors (Arthrex), loaded with FiberTape (Arthrex), are placed in the medial row of the greater tuberosity. A 4 × 7 cm, 3mm–thick ArthroFlex dermal allograft (LifeNet Health) is folded over, and the free edges are sutured together with SutureTape (Arthrex). FiberLink sutures (Arthrex) are then passed to allow easier passage of the FiberTapes once they are brought out the cannula. The thick graft will not fit through a commercially available cannula, so a 20 mL syringe is used, with the end cut off, to allow passage of the graft. The repair stitch and the loop stitch from the FiberTak anchor are brought out of the syringe. The repair stitch is then passed through the graft 5 mm from the medial edge, with a reverse cutting needle in a mattress fashion. The repair stitch is then passed through the loop of the shuttle loop stitch, and the corresponding SutureTape pull stitch from the same anchor is pulled percutaneously until the repair stitch passes through the anchor and can no longer back out. The steps are repeated individually for each anchor until all three mattress stitches are passed on the medial side of the graft. The FiberTapes from each medial row anchor are then brought out of the syringe cannula and kept separated. The FiberTapes from the medial row are placed 15 mm from the lateral edge of the graft approximately 7 mm to 10 mm apart with the previously placed FiberLink sutures. The side to side SutureTapes should also be passed before bringing the graft into the SAS. The graft is folded and introduced into the syringe. The pull stitches of each of the three FiberTaks are pulled percutaneously, thus pulling the graft into the subacromial space (SAS). As the graft advances into the SAS, the FiberTapes tend to bunch up, so the tails of the FiberTapes should also be pulled laterally to take the slack out of them. Once the graft is fully reduced and fixed medially, a suture grasping device is passed through the infraspinatus and the side to side SutureTape is grasped and passed through the tendon. This is also repeated anteriorly for the subscapularis. The side-to-side sutures are then tied and cut. The lateral row is then addressed by grasping a FiberTape limb from the posterior anchor and one FiberTape from the middle anchor and fixed laterally with SwiveLock anchors. The process is repeated with the other three anchors and a transosseous equivalent double row repair is achieved.
This is a left shoulder, viewing from the anterolateral portal demonstrating a massive rotator cuff tear. Three knotless FiberTak anchors (Arthrex) are placed percutaneously in the glenoid at the 10, 12, and 2 o’clock positions. Three SwiveLock anchors (Arthrex), loaded with FiberTape (Arthrex), are placed in the medial row of the greater tuberosity. A 4 × 7 cm, 3mm–thick ArthroFlex dermal allograft (LifeNet Health) is folded over, and the free edges are sutured together with SutureTape (Arthrex). FiberLink sutures (Arthrex) are then passed to allow easier passage of the FiberTapes once they are brought out the cannula. The thick graft will not fit through a commercially available cannula, so a 20 mL syringe is used, with the end cut off, to allow passage of the graft. The repair stitch and the loop stitch from the FiberTak anchor are brought out of the syringe. The repair stitch is then passed through the graft 5 mm from the medial edge, with a reverse cutting needle in a mattress fashion. The repair stitch is then passed through the loop of the shuttle loop stitch, and the corresponding SutureTape pull stitch from the same anchor is pulled percutaneously until the repair stitch passes through the anchor and can no longer back out. The steps are repeated individually for each anchor until all three mattress stitches are passed on the medial side of the graft. The FiberTapes from each medial row anchor are then brought out of the syringe cannula and kept separated. The FiberTapes from the medial row are placed 15 mm from the lateral edge of the graft approximately 7 mm to 10 mm apart with the previously placed FiberLink sutures. The side to side SutureTapes should also be passed before bringing the graft into the SAS. The graft is folded and introduced into the syringe. The pull stitches of each of the three FiberTaks are pulled percutaneously, thus pulling the graft into the subacromial space (SAS). As the graft advances into the SAS, the FiberTapes tend to bunch up, so the tails of the FiberTapes should also be pulled laterally to take the slack out of them. Once the graft is fully reduced and fixed medially, a suture grasping device is passed through the infraspinatus and the side to side SutureTape is grasped and passed through the tendon. This is also repeated anteriorly for the subscapularis. The side-to-side sutures are then tied and cut. The lateral row is then addressed by grasping a FiberTape limb from the posterior anchor and one FiberTape from the middle anchor and fixed laterally with SwiveLock anchors. The process is repeated with the other three anchors and a transosseous equivalent double row repair is achieved.