Abstract
A 15-year-old boy presented with left-sided hip pain and imaging consistent with the diagnosis of femoroacetabular impingement. Following hip arthroscopy, which included an osteochondroplasty, labral repair, and capsular repair, the patient's anterior hip pain improved. However, his deep aching hip pain persisted until an ischial osteoid osteoma was identified and treated with radiofrequency ablation. At 3 years follow-up, the patient reports high satisfaction and minimal pain. We present this case to illustrate the importance of considering all potential causes of persistent hip pain following hip arthroscopy, including benign bone tumors which may be difficult to visualize on plain radiographs.
Keywords: Pediatric, Femoroacetabular impingement, Osteoid osteoma
Introduction
Persistent hip pain following hip arthroscopy for femoroacetabular impingement (FAI) is commonly attributed to residual impingement secondary to an inadequate osteochondroplasty, iatrogenic instability, labral pathology, or chondral lesions [1,2]. In the absence of objective imaging or physical examination findings suggestive of residual impingement or instability, determining the underlying source of persistent pain can be difficult. In this report, we present the case of an adolescent boy with persistent, deep, achy hip pain following an adequate osteochondroplasty, labral repair, and routine capsular repair without signs of microinstability or residual impingement. A thorough workup identified his lingering source of pain to be an osteoid osteoma in the ischium. The decision was made to proceed with radiofrequency ablation (RFA), which ultimately relieved his symptoms. At the time of manuscript preparation, the patient was 19 years old. He was informed that data concerning the case would be submitted for publication, and he provided consent.
Case report
A 15-year-old male presented to an outside orthopedic clinic with deep groin pain in the left hip which began 6 months after he fell playing noncontact football. The pain was continuous and increased with deep squatting, sitting, and twisting motions. Occasionally the patient experienced a mild-ache around the left hip at night. Nonsteroidal anti-inflammatory drug (NSAID) provided minimal to no pain relief. Physical examination and plain radiographs were consistent with cam-type FAI (Fig. 1). Additionally, an MR arthrogram demonstrated a labral tear in the anterosuperior region of the labrum. No further osseous abnormalities were observed at this time. After failing nonoperative treatment, he elected to undergo left hip arthroscopy with femoral osteochondroplasty, labral repair, and routine capsular repair. Notable intraoperative findings included a labral tear from 1 to 3 o'clock, softened acetabular cartilage from 12 to 3 o'clock, and pitting in the anterosuperior region of the femoral head-neck junction in the area of the cam deformity. Femoral osteochondroplasty was completed to a depth that provided appropriate clearance on dynamic examination.
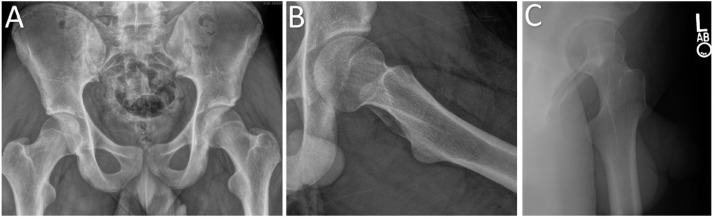
Fig. 1.
Radiographic evaluation prior to hip arthroscopy. Preoperative radiographic evaluation of the left hip in the setting of history and physical examination consistent with femoroacetabular impingement, consistent with CAM-type femoroacetabular impingement. (A) Anteroposterior (AP) pelvis radiograph, (B) Frog-leg lateral radiograph, (C) False profile radiograph.
Three weeks postoperatively the patient was seen in clinic and reported feeling comfortable, stating he felt “really well.” Postoperative radiographs demonstrated an adequate femoral osteochondroplasty with no signs of additional pathology. The patient completed 8 sessions of physical therapy, with the last session occurring at 2 months postoperatively. Throughout the next 5 months the patient began to notice a gradual increase of deep, achy left hip pain; however, during this time period he did not attend any further physical therapy sessions or postoperative clinical visits. At 7 months postoperatively he returned to clinic reporting a poor recovery from his primary hip arthroscopy procedure. His pain was continuous, worst at night, located deep in the hip, and responded partially to NSAIDs. Physical examination found no signs of residual impingement or iatrogenic instability. Radiographs were repeated and again demonstrated an adequate osteochondroplasty (Fig. 2). In order to identify if the source of pain was intra-articular, an ultrasound-guided intra-articular corticosteroid and local anesthetic hip injection was done. The injection provided no pain relief. A repeat MR arthrogram demonstrated normal findings with the exception of edema present in the acetabulum (Fig. 3). An area of nidus formation and surrounding peritumoral edema was appreciated (Fig. 4), which prompted a subsequent computed tomography (CT) scan and consultation with the orthopedic oncology team. In the same region as the MR arthrogram, the CT demonstrated a low density, well-defined, ovoid lesion with a nidus of central calcification and surrounding sclerosis (Fig. 5). These findings were consistent with an osteoid osteoma in the posterior-inferior aspect of the acetabulum.
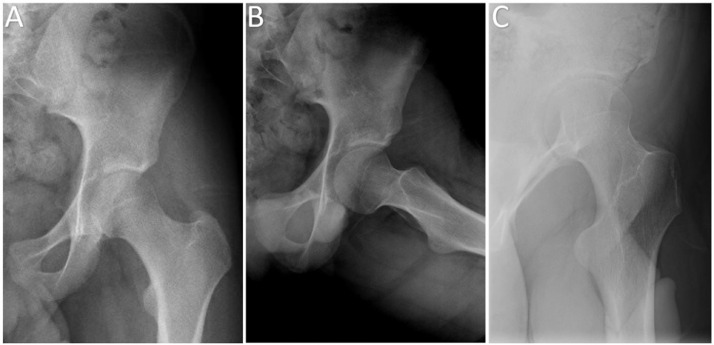
Fig. 2.
Radiographic evaluation 7 months following femoral osteochondroplasty and labral repair. Postoperative radiographic evaluation of the left hip demonstrating adequate femoral osteochondroplasty. (A) Anteroposterior (AP) pelvis radiograph, (B) Frog-leg lateral radiograph, (C) false profile radiograph.
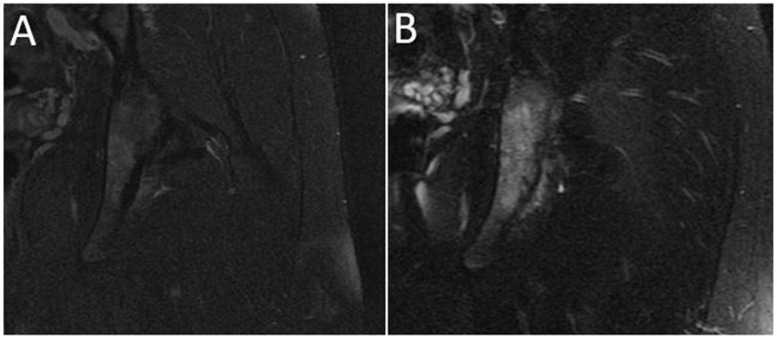
Fig. 3.
Comparison of the posterior-inferior acetabulum on magnetic resonance arthrography prior to and after surgery. Coronal T2-weighted fat saturated magnetic resonance images of the left hip showing the posterior-inferior acetabulum. (A) Magnetic resonance arthrogram obtained one month prior to left hip arthroscopy demonstrating normal findings. (B) Magnetic resonance arthrogram obtained 9 months following left hip arthroscopy demonstrating edema in the posterior-inferior acetabulum extending into the ischial tuberosity.
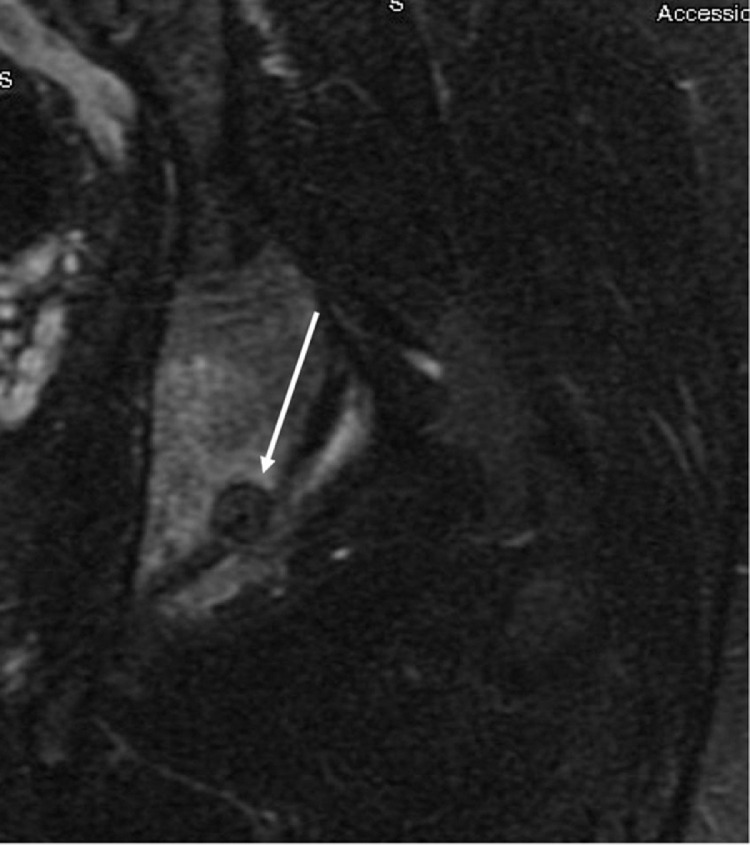
Fig. 4.
Bony lesion visualized on magnetic resonance arthrogram nine months following left hip arthroscopy. Coronal T2-weighted fat saturated magnetic resonance image of the left ischium, demonstrating an area of nidus formation with surrounding peritumoral edema (arrow).
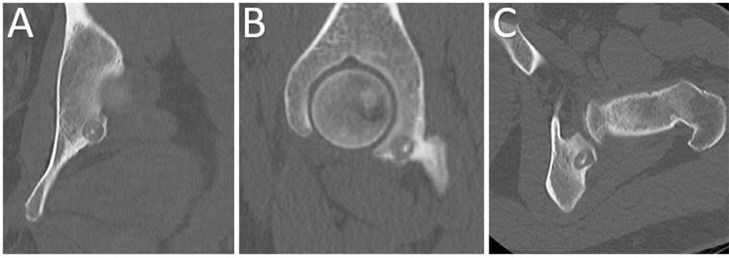
Fig. 5.
Computed tomography of the left hip demonstrating a bony lesion of the ischium. Computed tomography scan of the left hip 10 months following left-sided hip arthroscopy. The osteoid osteoma is apparent in each image in the posterior-inferior acetabulum as a well-defined, lucent lesion with a nidus of central calcification. (A) Coronal slice through the ischium, (B) Sagittal slice through the medial femoral head and acetabulum, (C) Axial slice through the femoral neck and posterior-inferior acetabulum.
After referral to the orthopedic oncology service, the patient elected to undergo percutaneous RFA. The procedure was done in the OR with the orthopedic oncologist, not in the IR suite with the IR team, as is the practice model at our institution. A guide pin was advanced into the lesion under fluoroscopic guidance and its satisfactory position confirmed with intra-operative CT scan (O-arm). The lesion was then over-drilled and the specimen was saved for pathologic assessment. The RFA probe was then advanced into the hole as the drill was removed. Its position was confirmed with the O-arm, and the probe was then used, raising the temperature to 100°C for an effective time of 45 seconds, delivering 120 watts of treatment dose (Fig. 6). Final pathology assessment was consistent with the diagnosis of osteoid osteoma.
Fig. 6.
Radiofrequency ablation of the osteoid osteoma. Radiofrequency ablation probe positioned in the osteoid osteoma lesion of the left ischial tuberosity.
Fifteen months following the patient's initial left-sided arthroscopic hip surgery, he returned to seek treatment for right-sided hip pain. Physical examination and plain radiographs were consistent with right-sided cam-type FAI. A right hip femoral osteochondroplasty, labral repair, and routine capsular closure were performed without complications. At follow up nearly 3 years after the initial hip arthroscopy, the patient was asked to rate his pain at rest, activities of daily living, and during sport activities. He rated his pain in both hips as 2/10 at rest (which he only notices after long periods of rest), 1/10 during activities of daily living, and 0/10 during sport activities. Additionally, the patient was asked his overall satisfaction following his initial left hip arthroscopy and following his left hip RFA surgery. He reported 7/10 following left hip arthroscopy, and 9/10 following his left hip RFA surgery. On Likert Scale (5-point scale: very satisfied, satisfied, neutral, dissatisfied, very dissatisfied), he noted he was very satisfied following each surgery. Finally, he was asked if he were presented with the option of “doing it all over again” would he, and he responded yes.
Discussion
This case report describes an adolescent patient who presented with left-sided hip pain which improved following primary hip arthroscopy with femoral osteochondroplasty, labral repair, and routine capsular closure. While the anterior hip pain consistent with FAI had improved, he continued to experience deep, achy pain in the left hip that was worse at night. Eventually a CT scan revealed a left-sided osteoid osteoma located in the posterior-acetabulum of which there was no evidence on presurgical radiographs or MR arthrogram. This case report is an excellent example of why hip surgeons must maintain a broad differential when considering what might be causing the persistent hip pain following routine hip arthroscopy.
Residual impingement, iatrogenic instability, labral pathology, and chondral lesions are most commonly attributed as causes of persistent pain following hip arthroscopy [1]. If any of these are suspected, revision hip arthroscopy is often considered. In cases without objective findings indicating a revision procedure, it is important to be especially thoughtful before proceeding with a revision procedure that may not be indicated.
After the diagnosis was made on CT scan and in conjunction with pathology assessment of biopsied tissue, we reassessed the imaging that was obtained prior to the original left hip arthroscopy. In retrospect, there were no signs of a tumor or neoplastic process within the acetabulum. Therefore, the osteoid osteoma was not missed or misdiagnosed on initial presurgical imaging; rather, it developed after the original left hip arthroscopy. The first magnetic resonance imaging obtained was sequenced for structural pathology rather than a neoplastic process, thus images were suboptimal for tumor assessment. There was only one non-T1 series. This was a coronal T2, which did have some scattered high intensity signal within the posterior acetabulum, but no area of coalescence to suggest a tumor. Additionally, a sclerotic formation can be appreciated on the AP and frog-leg lateral radiographs obtained 6 months post left hip arthroscopy, however, the posterior acetabulum and ischium were obscured by the local anatomy and slight rotation.
Osteoid osteomas are benign, but active, bone tumors that most commonly affect patients aged 10-30. They are characterized by a constant, deep aching pain, owing to their biology in which the tumor itself constitutively produces prostaglandins. They may be found throughout the skeleton, and often require advanced cross-sectional imaging to narrow the differential diagnosis. Previous case reports and case series have described osteoid osteoma lesions in the femoral neck and acetabulum presenting similarly to FAI, and occasionally hip arthroscopy is used to resect these lesions [3]. One previous case report describes a 52-year-old with FAI and a coexistent osteoid osteoma which was initially overlooked, but was eventually recognized and treated with a NSAID regimen [4]. The present case is unique in that it involves a young, 15-year-old adolescent patient whose anterior hip pain improved following hip arthroscopy for FAI. However, his deep, achy hip pain persisted until a left-sided ischial osteoid osteoma was identified and treated with RFA. Following successful RFA, he had an unrelated right hip arthroscopy for FAI which improved his right-sided impingement pain. At three years follow-up from his initial hip arthroscopy, the patient reported high satisfaction and minimal pain.
Important learning points highlighted by our case are some of the common features in the presentation of osteoid osteomas. Osteoid osteomas present with a deep, constant pain, often noted to worsen at night; NSAIDs provide relief due to their mechanism of action against prostaglandins, but symptoms classically recur immediately, once the therapeutic concentration of the drug drops according to its half-life. They are typically observed on plain radiographs as an ovoid radiolucency with reactive surrounding sclerosis. However, lesions can be difficult to visualize on plain radiographs, particularly in the spine, pelvis, and small bones of the hand [5]. Treatment options include nonsurgical NSAID regimens and operative modalities such as open excision, CT-guided percutaneous excision, CT-guided RFA, and arthroscopic excision.
As shown in the presented case, critical thinking about each patient's complaints and objective findings allows for identification of less likely diagnoses, such as osteoid osteoma of the ischium in a patient with bilateral FAI. The patient had no physical examination or imaging findings suggestive of an inadequate osteochondroplasty, capsular or labral deficiency leading to instability, or chondral pathology. Astute recognition of the unique presentation of residual pain worse at night followed by recognition of nidus formation with surrounding peritumoral edema in the ischium on magnetic resonance imaging led to a timely referral to the orthopedic oncology team and an excellent outcome.
Statement of Informed Consent
The patient was informed that data concerning the case would be submitted for publication, and he provided consent.
References
- 1.Sardana V, Philippon MJ, De Sa D, Bedi A, Ye L, Simunovic N. Revision hip arthroscopy indications and outcomes: a systematic review. Arthroscopy. 2015;31(10):2047–2055. doi: 10.1016/j.arthro.2015.03.039. [DOI] [PubMed] [Google Scholar]
- 2.Wylie JD, Beckmann JT, Maak TG, Aoki SK. Arthroscopic capsular repair for symptomatic hip instability after previous hip arthroscopic surgery. Am J Sports Med. 2016;44(1):39–45. doi: 10.1177/0363546515608162. [DOI] [PubMed] [Google Scholar]
- 3.Spiker AM, Rotter B-Z, Chang B, Mintz DN, Kelly BT. Clinical presentation of intra-articular osteoid osteoma of the hip and preliminary outcomes after arthroscopic resection: a case series. J Hip Preserv Surg. 2018;5(1):88–99. doi: 10.1093/jhps/hnx042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Banga K, Racano A, Ayeni OR, Deheshi B. Atypical hip pain: coexistence of femoroacetabular impingement (FAI) and osteoid osteoma. Knee Surg Sports Traumatol Arthrosc. 2015;23(5):1571–1574. doi: 10.1007/s00167-014-2985-6. [DOI] [PubMed] [Google Scholar]
- 5.Atesok KI, Alman BA, Schemitsch EH, Peyser A, Mankin H. Osteoid osteoma and osteoblastoma. J Am Acad Orthop Surg. 2011;19(11):678–689. doi: 10.5435/00124635-201111000-00004. [DOI] [PubMed] [Google Scholar]