Abstract
Sustained ventricular tachycardia (VT) in the early postoperative period following intracardiac repair for tetralogy of Fallot is rare. In stable VT, amiodarone forms the mainstay of management. However, where amiodarone and other antiarrhythmic drugs are contraindicated, suppressive overdrive atrial pacing can be used as a safe and efficient alternative to maintain cardiac output. We present a case of 1-year 5-month-old child who developed VT with low cardiac output syndrome with deranged hepatic function, who was managed efficiently using suppressive atrial pacing to ameliorate the effects of sustained VT.
Keywords: Atrial overdrive pacing, posttetralogy of Fallot repair, sustained ventricular tachycardia
INTRODUCTION
Arrhythmia is a common phenomenon in the early postoperative period following congenital heart surgeries (CHSs), and its management sometimes imposes a great challenge. Right ventriculotomy and muscle resection during tetralogy of Fallot (TOF) repair predispose to arrhythmias – most commonly being junctional ectopic tachycardia. However, ventricular tachycardia (VT) is rare. Usually, amiodarone is the best available therapeutic option besides various general measures to control any form of arrhythmias. Although overdrive pacing is well established in atrial arrhythmias, its application in ventricular arrhythmias (VAs) is not well explored, especially in CHS. Patients where established pharmacotherapy is not feasible, suppressive overdrive atrial pacing is a safe and effective alternative.
CASE REPORT
A 1-year 5-month-old cyanosed female child with a diagnosis of TOF underwent intracardiac repair with transannular patch. The child had high left atrial pressure (LAP) while coming off cardiopulmonary bypass, and hence, sternum was stented electively followed by delayed sternal closure on the postoperative day (POD) 1. Postextubation, the child was reintubated on POD5 following tachypnea with poor gas exchange. ECHO imaging revealed severe right ventricular (RV) diastolic dysfunction, leading to congestive hepatopathy. The high LAP also added onto the insult. Serum bilirubin was 8.2 mg%, and serum glutamic oxaloacetic transaminase and serum glutamic pyruvic transaminase were 2840 and 2120 U/L, respectively. She was on inotropic supports of adrenaline, noradrenaline, and milrinone infusion of 0.05 miC/kg/min.
Frequent nonsustained VT developed on the POD6. The possible correctable causes were evaluated for and arrhythmogenic nature of the inotropes being concluded as the cause, were replaced with levosimendan infusion. Transient initial success was achieved with intermittent boluses of MgSO4 and xylocaine injection. With progression, the VT became more frequent and resistant to medical therapy. Amiodarone could not be used in view of deranged liver function, and options of using beta-blocker and calcium channel blockers were ruled out in view of persistent ventricular dysfunction. A 12-lead electrocardiogram showed peaked, nonnotched, tall QRS in the inferior leads with qS in the lead aVL characteristically seen with ventricular premature complexes (VPCs), arising from anterosuperior portion of septal aspect of RV outflow [Figure 1].
Figure 1.
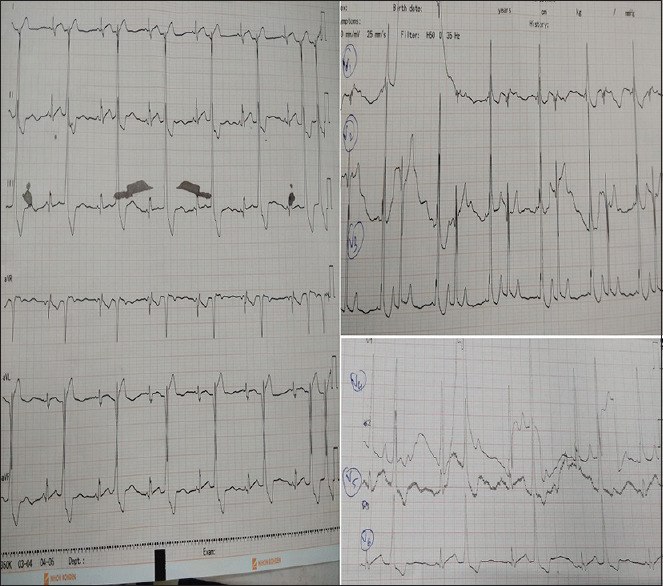
A 12-lead electrocardiogram showing the morphology of QRS complex of ventricular bigeminy (qS in aVL)
On POD7, rhythm worsened to ventricular bigeminy degenerating to sustained monomorphic stable VT with borderline hemodynamics [Figure 2]. Atrial electrogram performed during tachycardia showed VA dissociation. Overdrive atrial pacing was established at 160 bpm above the rate of VT with intraoperatively placed epicardial leads [Figure 3]. Cardiac output improved with atrial pacing with disappearance of VT. This beneficial effect was only observed when paced at a rate higher than VT along with the added advantage of the atrial kick.
Figure 2.
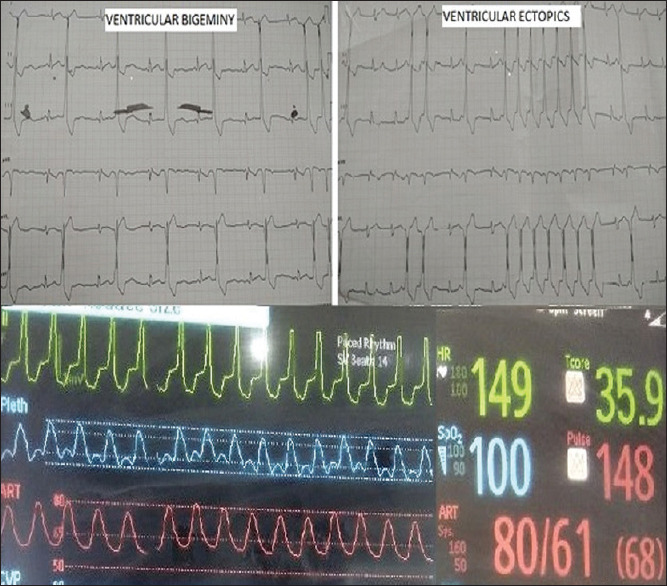
Varying rhythms with ventricular bigeminy, short VT runs, and sustained VT. VT: Ventricular tachycardia
Figure 3.

Atrial overdrive pacing suppressing VT. VT: Ventricular tachycardia
Within hours, rhythm reverted to ventricular bigeminy followed by infrequent ventricular ectopics. Pacing was readjusted to 140 bpm to maintain optimal hemodynamics. The child reverted to normal sinus rhythm with the improvement of cardiac function in the following 24 h.
DISCUSSION
Overdrive pacing has been well documented to revert rhythm in re-entrant arrhythmia in adults.[1] VA, though rare in the early postoperative period, are deleterious to the recovering myocardium.[2] The patient's QRS morphology clearly favored VPC's as wide QRS was not preceded byPwaves and PP interval continued unaltered. We presumed that this arrhythmia had a nonre-entrant mechanism with either an automaticity or triggered activity. The location of outflow, induction with isoprenaline infusion, and the fixed coupling interval of VPCs favors triggered activity as the most common mechanism of idiopathic RVOT ectopics which might have been provoked by the adrenergic state.
Normally, sustained VT with rates <150 bpm is well tolerated in the postoperative period in the absence of ventricular dysfunction. At higher rates, opposing effect is observed as diastolic filling time is affected. Patients with hypertrophied ventricles having diastolic dysfunctions responds poorly to the loss of AV synchrony and results in low cardiac output even with a lower ventricular rate. Moreover, RV output remains fixed in RV dysfunction.
Overdrive pacing with desirable effect is limited to VT between 140 and 170 bpm because AV node should conduct with desirable hemodynamic changes. The patient's rate <150 bpm with effective 1:1 AV conduction with regular QRS intervals was sufficient enough to overdrive.
Although ventricular overdrive pacing is an established management modality of VT, it can result in interventricular dys-synchrony, hypotension, and at times degeneration of arrhythmia to ventricular fibrillation. On the contrary, atrial pacing results in better synchronous ventricular contraction due to narrow QRS. This emphasizes the need for epicardial atrial leads, especially in such cases or cases where VA is expected such as ASO and ALCAPA repair.
The decision to treat an arrhythmia should be based on hemodynamic necessity and not just for reverting rhythm to normal. Amiodarone is a drug of choice in cases of hemodynamically stable VT.[3]
CONCLUSION
Suppressive atrial overdrive pacing can be used alone or as a hybrid to pharmacotherapy to control VT in the early postoperative period. However, this beneficial effect of overdrive atrial pacing losses its advantage at higher rates. Further studies with varied subsets of diagnosis are required to incorporate this beneficial effect as a management modality for VT.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Hamer AW, Zaher CA, Rubin SA, Peter T, Mandel WJ. Hemodynamic benefits of synchronized 1:1 atrial pacing during sustained ventricular tachycardia with severely depressed ventricular function in coronary heart disease. Am J Cardiol. 1985;55:990–4. doi: 10.1016/0002-9149(85)90732-5. [DOI] [PubMed] [Google Scholar]
- 2.Walsh EP. Improved understanding of ventricular tachycardia in patients with tetralogy of Fallot. Eur Heart J. 2017;38:277–9. doi: 10.1093/eurheartj/ehw167. [DOI] [PubMed] [Google Scholar]
- 3.Hernández-Madrid A, Paul T, Abrams D, Aziz PF, Blom NA, Chen J, et al. Arrhythmias in congenital heart disease: A position paper of the European Heart Rhythm Association (EHRA), Association for European Paediatric and Congenital Cardiology (AEPC), and the European Society of Cardiology (ESC) Working Group on Grown-up Congenital heart disease, endorsed by HRS, PACES, APHRS, and SOLAECE. Europace. 2018;20:1719–53. doi: 10.1093/europace/eux380. [DOI] [PubMed] [Google Scholar]


