Summary
Lumbar epidurals are frequently inserted for women in labour as they provide excellent analgesia. One of the more common procedural complications is post‐dural puncture headache which can be associated with auditory symptoms such as hearing loss and tinnitus and can be treated with an epidural blood patch. Sphenopalatine ganglion blocks have also been used to treat post‐dural puncture headache but have not been previously shown to resolve the associated tinnitus. We report a case where postural neck pain and tinnitus from an accidental dural puncture during lumbar epidural insertion for labour analgesia was treated successfully with a sphenopalatine ganglion block. Further, we explore the literature on the cause of tinnitus in post‐dural puncture headache and the possible mechanism by which a sphenopalatine ganglion block relieves both post‐dural puncture headache and the associated tinnitus.
Keywords: dural puncture, epidural, headache, sphenopalatine ganglion block, tinnitus
Introduction
Lumbar epidurals are commonly inserted in parturients as they have the best analgesic profile among the labour analgesia options available. Post‐dural puncture headache (PDPH) is a known complication of epidural insertion with an incidence of approximately 1% [1]. According to the International Headache Society, PDPH is an orthostatic headache commonly associated with neck pain, tinnitus, changes in hearing, photophobia and/or nausea [1]. Timely management of PDPH reduces morbidity and mortality. An epidural blood patch is the only proven intervention that relieves severe and intractable PDPH. However, it is invasive and may be associated with significant complications [1].
The sphenopalatine ganglion, also known as Meckel’s ganglion, is located extracranially in the pterygopalatine fossa and has sympathetic, parasympathetic and somatic innervation [2]. Sphenopalatine ganglion block has been used to treat chronic headache syndromes like migraine, cluster headache and trigeminal neuralgia [3]. There is promising support emerging in the literature for the use of sphenopalatine ganglion block as a less invasive treatment for PDPH [3, 4]. However, there are no documented cases of sphenopalatine ganglion block alleviating both PDPH and associated tinnitus. We report a case of a patient with severe neck pain and bilateral tinnitus after an accidental dural puncture who was treated successfully with a sphenopalatine ganglion block.
Report
A 34‐year‐old, ASA physical status 1, primigravida woman developed PDPH which manifested as severe orthostatic neck pain with bilateral tinnitus after an accidental dural puncture during the insertion of a lumbar epidural for labour analgesia. Two attempts were made using a loss of resistance to saline technique with an 18‐G Tuohy needle at the L3/4 interspace with the patient in the sitting position. During the first attempt, no loss of resistance was obtained despite being at an insertion depth of 6 cm. On the second attempt, a convincing loss of resistance to saline was obtained at a depth of 4.5 cm, and the catheter was threaded into the epidural space and secured at 5 cm at the skin. The labour epidural was effective with no indication of a dural breach throughout labour. The patient had an uneventful vaginal delivery a few hours later.
Twenty‐four hours following epidural insertion, the patient reported severe neck pain associated with bilateral tinnitus. The patient rated her neck pain at 10/10 on the numeric pain rating scale. The pain was orthostatic in nature and improved on recumbency to 6/10. A full neurological examination was unremarkable, with normal Rinne and Weber tests. Conservative management strategies were instituted including intravenous hydration, oral analgesics (paracetamol 1 g four times a day; mefenamic acid 500 mg three times a day; tramadol 50 mg three times a day as required) and bed rest. When these strategies did not improve her pain, which was still 9/10, nor her bilateral tinnitus (which resulted in poor sleep quality and emotional distress), we performed a trial of a transnasal sphenopalatine ganglion block 48 hours later [3].
Two long cotton‐tip applicators were immersed in a solution containing 2% lidocaine and 0.5% ropivacaine. The patient was positioned supine with her neck extended and both nostrils facing superiorly. Each cotton‐tip applicator was then inserted into each naris parallel to the floor of the nose until resistance was encountered, corresponding to the position of the sphenopalatine ganglion which is at the posterior wall of the nasopharynx and superior to the middle concha. The applicators were left in‐situ for 10 min (Fig. 1) [2, 3]. The patient tolerated the procedure well and was advised to remain supine for at least 30 min.
Figure 1.
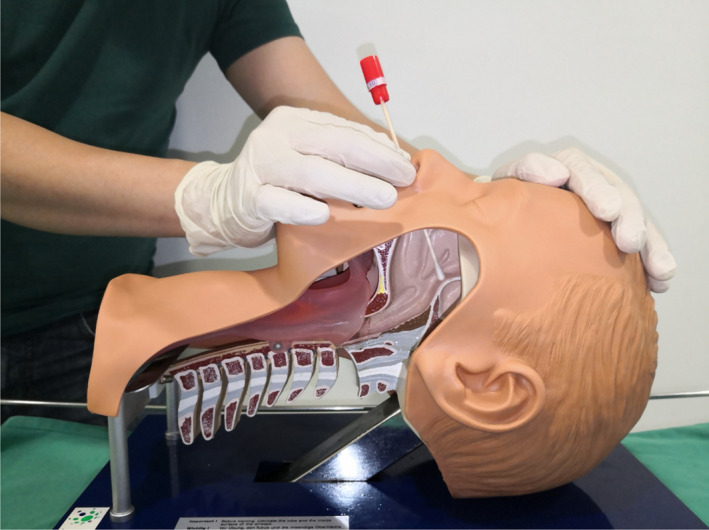
Anatomical illustration of how the transnasal sphenopalatine ganglion block is performed.
When the patient was reviewed 90 min after the sphenopalatine ganglion block she reported significant reduction in her neck pain (from 10/10 to 6/10) and she was able to sit up at an incline of 30°. Her bilateral tinnitus was unchanged. However, 6 h later, her neck pain further improved to 2/10 and her tinnitus completely resolved. On the morning of day 3 following the dural puncture, her pain score was 0–1/10 and she denied any tinnitus. She was discharged on day 4 following the dural puncture with subsequent daily phone follow‐up. She reported one episode of breakthrough neck pain of 8/10 on day 6 after the dural puncture which was alleviated with a dose of oral tramadol. Her pain decreased in intensity daily thereafter, requiring no analgesia by day 9. Of significance, there was no recurrence of bilateral tinnitus following the block. She remained completely asymptomatic 1 month after the sphenopalatine ganglion block and was satisfied with the treatment received.
Discussion
Post‐dural puncture headache, if left untreated, usually lasts for 7 days, although severe cases can take months or years to resolve. Accompanying auditory symptoms such as tinnitus and sensorineural hearing loss are usually transient but have been reported to last for several months and even years [5]. Sensorineural hearing loss secondary to a dural puncture is a known complication and occurs commonly in cases involving spinal anaesthesia. Post‐dural puncture tinnitus from epidural analgesia has been reported with a much lower incidence restricted to a few case reports [5, 6]. Indeed, despite being an incapacitating symptom associated with low mood and sometimes suicide, tinnitus remains a rare but potentially long‐lasting side‐effect of a dural puncture.
While the pathophysiology of PDPH is attributed to cerebrospinal fluid loss leading to a compensatory cerebral vasodilatation which manifests as a postural headache, the mechanism of tinnitus is still unclear [4]. Two theories have been postulated. The first is that a cerebrospinal fluid leak through the dural lesion causes a decrease in cerebrospinal fluid pressure and consequently a reduction in intralabyrinth pressure. This occurs as perilymph content is similar to that of cerebrospinal fluid and a direct connection exists between the subarachnoid space and the cochlea via the cochlear aqueduct. Therefore, the pressure differential between perilymph and endolymph can disrupt both the vestibular membrane and the basilar membrane within the cochlea [7]. This leads to displacement of inner ear hair cells resulting in tinnitus [8]. Another theory is neuropraxia of the vestibulocochlear nerve resulting from stretching caused by cerebrospinal fluid hypotension as the nerve traverses the posterior cranial fossa [6]. The nerve is prone to stretch injury because the internal acoustic meatus it eventually enters is a tight space [5].
The underlying mechanism for the analgesic effect of sphenopalatine ganglion block is proposed to be related to the reversal of the cerebral vasodilatation responsible for PDPH. The sphenopalatine ganglion has both somatic and autonomic nerve supplies. Local anaesthetic blocks this ganglion which reduces the release of vaso‐active mediators such as acetylcholine, nitric oxide and vaso‐active intestinal peptide. The resultant cerebral vasoconstriction alleviates the headache [4].
Regarding PDPH‐associated tinnitus, there are case reports where an epidural blood patch resulted in complete resolution [6]. However, reports of sphenopalatine ganglion block relieving tinnitus are scarce, with only one case where a young woman with a 1‐year history of tinnitus and bilateral ear itching experienced resolution of both symptoms after cocaine was applied to the sphenopalatine ganglion [9].
We acknowledge some limitations with this report. The placebo effect of this intervention for neck pain cannot be excluded, as highlighted by Jespersen et al., who conducted a randomised trial of 40 patients with PDPH who received sphenopalatine ganglion block with either a mixture of lidocaine 4%/ropivacaine 0.5% or with saline [10]. Although there was no significant difference in pain scores between both groups, Jespersen et al.’s study had limitations, including the possibility of unblinding due to the contrast in taste between local anaesthetic and saline; the blind administration of the block which led to the possibility of wrongly placed and therefore failed blocks; the heterogeneous nature of the study population; the small sample size; and the absence of a group which received no treatment. Moreover, Jespersen et al.’s primary outcome was pain scores, and the incidence of tinnitus was not mentioned in this study. Tinnitus is a distressing symptom and complete resolution in this patient is unlikely to be accounted for by the placebo effect. The prompt resolution of her tinnitus which did not recur suggests that there is likely another relevant treatment effect.
This case provides promising evidence that sphenopalatine ganglion block can be used to treat not only the pain component of PDPH but the associated tinnitus as well. This should be evaluated in future studies. An epidural blood patch is effective for treating PDPH and its associated tinnitus but is an invasive procedure with risks including dural puncture; bleeding; neurological symptoms (back pain or radicular pain); infection; and subdural haemorrhage [3, 4]. In contrast, a transnasal sphenopalatine ganglion block is less invasive, has a faster onset of headache relief and a better risk profile. Self‐limiting side‐effects include a taste of bitterness, burning sensation in the nostrils and numbness in the oropharyngeal region [4]. Despite this, it is prudent to note that sphenopalatine ganglion block does not reduce the rare risk of subdural haematoma as the cerebrospinal fluid leaks through the dural lesion, which can lead to cerebrospinal fluid hypotension and consequent shearing of bridging veins [1]. As such we recommend a period of follow‐up for patients who have had a sphenopalatine ganglion block so that red flag symptoms, such as a headache which is non‐orthostatic and associated with other neurological deficits, can be detected and acted upon promptly. In our institution, after discharge, patients receive daily phone follow‐up until they are headache‐free for 2 consecutive days, then contacted again at 1 week and 1 month.
In conclusion, this report shows the use of a transnasal sphenopalatine ganglion block as a treatment for both PDPH and the associated tinnitus. As the block is less invasive and has lower morbidity, it can be used for the treatment of PDPHs with a tinnitus component instead of an epidural blood patch if similar results are shown in future studies.
Acknowledgements
Published with the written consent of the patient. No external funding or competing interests declared.
References
- 1. Sachs A and Smiley R. Post‐dural puncture headache: the worst common complication in obstetric anesthesia. Seminars in Perinatology 2014; 38: 386–94. [DOI] [PubMed] [Google Scholar]
- 2. Nair A and Rayani B. Sphenopalatine ganglion block for relieving postdural puncture headache: technique and mechanism of action of block with a narrative review of efficacy. Korean Journal of Pain 2017; 30: 93–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kent S and Mehaffey G. Transnasal sphenopalatine ganglion block for the treatment of postdural puncture headache in the ED. American Journal of Emergency Medicine 2015; 33: e1–2. [DOI] [PubMed] [Google Scholar]
- 4. Cohen S, Levin D, Mellender S, et al. Topical sphenopalatine ganglion block compared with epidural blood patch for postdural puncture headache management in postpartum patients. Regional Anesthesia and Pain Medicine 2018; 43: 880–4. [DOI] [PubMed] [Google Scholar]
- 5. Wong A, Irwin M. Postdural puncture tinnitus. British Journal of Anaesthesia 2003; 91: 762–3. [DOI] [PubMed] [Google Scholar]
- 6. Jia W and Fadhlillah F. Blood patch for the treatment of post‐dural puncture tinnitus. SAGE Open Medical Case Reports 2018; 6: 2050313X1875944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lybegker H, Andersen T. Repetitive hearing loss following dural puncture treated with autologous epidural blood patch. Acta Anaesthesiologica Scandinavica 1995; 39: 987–9. [DOI] [PubMed] [Google Scholar]
- 8. O'Shaughnessy S, Fitzgerald C, Katiri R, Kieran S, Loughrey J. Permanent hearing loss and tinnitus following epidural analgesia complicated by accidental dural puncture. International Journal of Obstetric Anesthesia 2020; 43: 9–12. [DOI] [PubMed] [Google Scholar]
- 9. Ruskin S. The nasal (sphenopalatine) ganglion: In relation to itching in the auditory canal and to tinnitus aurium. Archives of Otolaryngology ‐ Head and Neck Surgery 1925; 2: 269–70. [Google Scholar]
- 10. Jespersen M, Jaeger P, Ægidius K, et al. Sphenopalatine ganglion block for the treatment of postdural puncture headache: a randomised, blinded, clinical trial. British Journal of Anaesthesia 2020; 124: 739–47. [DOI] [PubMed] [Google Scholar]


