Abstract
Mechanical circulatory support (MCS) devices are effective tools in managing refractory cardiogenic shock (CS). Data comparing veno-arterial extracorporeal membrane oxygenation (VA-ECMO) and IMPELLA® are however scarce. We aimed to assess outcomes of patients implanted with these two devices and eligible to both systems. From 2004 to 2020, we retrospectively analyzed 128 patients who underwent VA-ECMO or IMPELLA® in our institution for refractory left ventricle (LV) dominant CS. All patients were eligible to both systems: 97 patients were first implanted with VA-ECMO and 31 with IMPELLA®. The primary endpoint was 30-day all-cause death. VA-ECMO patients were younger (52 vs. 59.4, p = 0.006) and had a higher lactate level at baseline than those in the IMPELLA® group (6.84 vs. 3.03 mmol/L, p < 0.001). Duration of MCS was similar between groups (9.4 days vs. 6 days in the VA-ECMO and IMPELLA® groups respectively, p = 0.077). In unadjusted analysis, no significant difference was observed between groups in 30-day mortality: 43.3% vs. 58.1% in the VA-ECMO and IMPELLA® groups, respectively (p = 0.152). After adjustment, VA-ECMO was associated with a significant reduction in 30-day mortality (HR = 0.25, p = 0.004). A higher rate of MCS escalation was observed in the IMPELLA® group: 32.3% vs. 10.3% (p = 0.003). In patients eligible to either VA-ECMO or IMPELLA® for LV dominant refractory CS, VA-ECMO was associated with improved survival rate and a lower need for escalation.
Keywords: IMPELLA®, extracorporeal membrane oxygenation, mechanical circulatory support, cardiogenic shock
1. Introduction
Despite improvements in heart failure (HF) pharmacological therapies and widespread use of timely reperfusion in acute myocardial infarction (MI), cardiogenic shock (CS) is still associated with a dismal prognosis and major resource utilization [1]. Standard of care and current guidelines support the use of vasoactive agents (inotropes and/or vasopressors) to maintain adequate cardiac output [2]. This strategy however exposes the patients to increased afterload, increased myocardial oxygen demand and higher risk of arrhythmias that could lead at the end to impaired perfusion, further clinical deterioration and death [3].
Mechanical circulatory support (MCS) devices could overcome these pitfalls and restore cardiac output, improve systemic hemodynamic and subsequently reduce mortality [4,5]. Despite the lack of robust evidences, use of these devices significantly rose in the past decade but may also be associated with potential life-threatening complications [6]. Therefore, a careful multimodal evaluation by a dedicated Shock Team (critical care physicians, cardiac intensivists, interventional cardiologists, cardio-thoracic surgeons, advanced heart failure specialists, and anesthesiologist) is recommended to ensure correct CS phenotyping, therefore allowing tailored and early interventions with adequate MCS selection.
Currently, in most tertiary European cardiac centers, veno-arterial extracorporeal membrane oxygenation (VA-ECMO) and IMPELLA® are the most frequently devices implanted for refractory CS patients. Patients with a left ventricle (LV) dominant CS and without severe hypoxemia could be supported either with VA-ECMO or with IMPELLA®. Both have however different hemodynamic properties, with specific advantages/disadvantages and level of support. To date, direct comparison of these two devices is however limited and obviously highly challenging. Indeed, whether the choice would affect outcomes is poorly described.
Thus, we aimed in the present analysis to compare the characteristics and outcomes of patients implanted with VA-ECMO vs. IMPELLA® for refractory LV dominant CS, depending on the first implanted device in a selected CS population eligible to both devices.
2. Materials and Methods
2.1. Population and Design
The present study is a single-center, retrospective, observational registry conducted at the Heart and Lung Institute, University Hospital of Lille, France. Between April 2004 and March 2020, all patients requiring MCS using either IMPELLA® or VA-ECMO (irrespective of the first chosen device) for LV dominant refractory CS were included in the present registry (n = 262). All patients received standard CS therapies (adequate filling status, vasoactive drug use, and correction of the underlying cause) according to CS guidelines and local protocols.
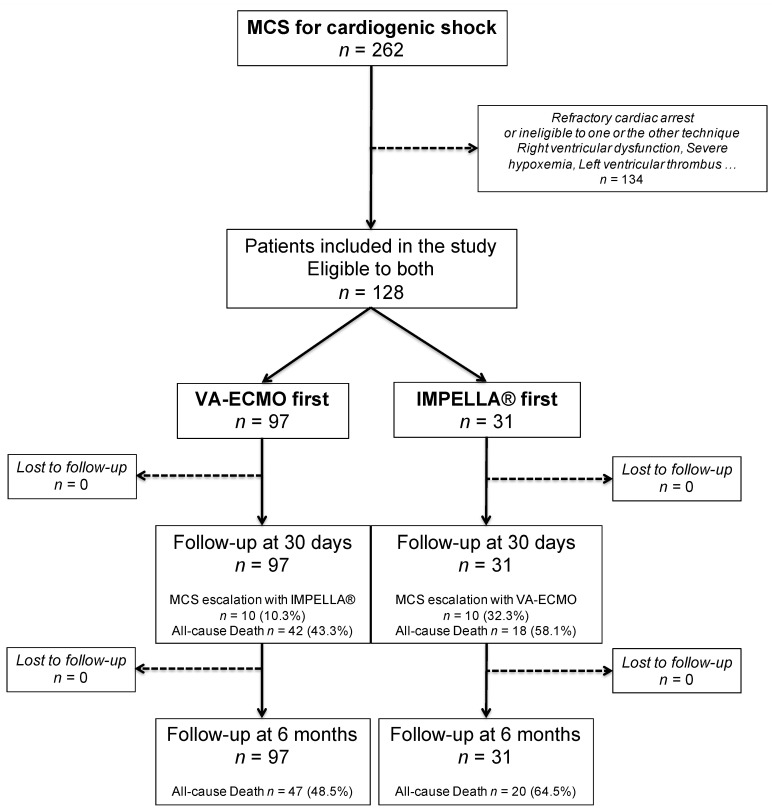
The present analysis aimed to compare patients who were first implanted with the IMPELLA® device (n = 31) to those first implanted with VA-ECMO (n = 97) as MCS device (Figure 1). For that purpose, we restrained the population to patients eligible to both devices (n = 128). Therefore, patients with severe hypoxemia (not related to acute heart failure), concomitant significant right ventricle (RV) failure, LV thrombus, and/or presenting with refractory cardiac arrest were excluded (n = 134).
Figure 1.
Flow chart of the study. MCS = mechanical circulatory support; VA-ECMO = veno-arterial extracorporeal membrane oxygenation; LV = left ventricle.
For each specific case, a dedicated Shock Team was activated and discussed timing and choice of MCS insertion based on a local protocol of refractory cardiogenic shock management (Figure S1). Data were entered into a comprehensive database.
2.2. CS Definition
CS was defined by a combination of impaired hemodynamic from cardiac origin (systolic blood pressure (SBP) < 90 mmHg for > 30 min or use of catecholamines to maintain SBP > 90 mmHg; cardiac index < 1.8 L/min/m2 without support or < 2.2 L/min/m2 with support), pulmonary congestion and impaired end-organ perfusion (confusion, cold/clammy skin and extremities, urine output < 30 mL/h, or lactate > 2 mmol/L).
RV failure was defined by a TAPSE (Tricuspid Annular Plane Systolic Excursion) < 15 and/or S (tissular Doppler) < 9 cm/s on transthoracic echocardiography (TTE).
2.3. Devices Implantation and CS Management
Experienced physicians implanted all devices. VA-ECMO was inserted surgically or percutaneously when possible (stable condition and suitable vascular access). At first, VA-ECMO was central in 6 cases. All the remaining patients underwent peripheral VA-ECMO (n = 91).
A centrifugal pump was combined with an oxygenator and limb reperfusion was routinely implanted. VA-ECMO flow was adapted to residual cardiac function and macro/microcirculatory parameters (mean arterial pressure (MAP), lactate, and central venous oxygen saturation (ScvO2)), and for an optimal right ventricular unloading. Implantation was performed with the assistance of experienced perfusionists and cardio-thoracic surgeons at the bedside, in the catheterization laboratory or operating room depending on the context and patient’s hemodynamic conditions.
IMPELLA® pumps were inserted percutaneously for CP devices (n = 26, 84%), or with an axillary surgical approach (arteriotomy and vascular graft) for 5.0 devices (n = 5, 16%). Choice was based on hemodynamic parameters, level of support needed and arterial access feasibility. All pumps were intended to run on the highest possible program level to achieve the best LV unloading and/or hemodynamic performance. Chest radiography and trans-thoracic echocardiography (TTE) was performed at implantation and repeated daily to ensure correct device position.
All patients without contraindications received unfractionated heparin to target an anti-Xa between 0.2 and 0.4 U/mL, modulated by pump flow and presence of bleeding or thrombotic complications. General medications including vasoactive drugs were in accordance to current CS recommendations.
2.4. Endpoints
The primary end-point was 30-day all-cause death. Secondary endpoints were 6-month all-cause mortality, 30-day and 6-month need for long-term LV assist device (LVAD), and/or heart transplantation. We also assessed a composite endpoint of all-cause death, LVAD implantation or heart transplant at 30 days and 6 months.
MCS escalation: In the IMPELLA® group, refractory CS that required implantation of VA-ECMO on top of IMPELLA® defined MCS failure because of persistent tissue hypoperfusion despite appropriate medical therapy and supposed from a cardiac origin. In the VA-ECMO group, MCS escalation was defined as insufficient LV unloading during VA-ECMO therapy leading to IMPELLA® insertion, characterized by a combination of clinical (arterial pulsatility loss), radiological (pulmonary oedema), echocardiographic criteria (LV distension, severe mitral insufficiency, stasis and/or LV thrombosis), or an elevated pulmonary capillary wedge pressure despite usual measures. In addition, 1 patient was unloaded with fenestration and one with intra-aortic balloon pump (IABP) insertion. Although these 2 cases could be considered as MCS failure, they were not considered as MCS escalation in this analysis.
Cardiac recovery was defined by a durable improvement of myocardial parameters allowing definite MCS weaning without the need for LVAD or heart transplantation during follow-up.
Specific MCS devices adverse events were in accordance with a recent consensus statement endorsed by the MCS academic research consortium [7]. Finally, major bleeding events, stroke and sepsis were also evaluated at 6 months. Stroke and sepsis were defined in line with current definitions [8,9]. Bleeding events were based on the Bleeding Academic Research Consortium (BARC) standardized definitions and major bleeding was defined by a BARC > 2 [10].
2.5. Statistical Analysis
Qualitative categorical variables are presented as numbers (percentages) and were compared using Chi-2 or Fisher tests as appropriate. Quantitative continuous variables are presented as mean (±standard deviation (SD)) and compared using Student’s t-test. Survival analyses were performed using the Kaplan–Meier method and were compared by a log-rank test. For multivariable analysis, in the primary analysis (model 1), multivariate Cox analyses were used to determine the association between variables of interest (based on previous literature) and 30-day and 6-month mortalities after adjusting for age, sex, diabetes, acute myocardial infarction at admission, left ventricle ejection fraction (LVEF) at admission, lactate level, creatinine level, hemoglobin level at admission and VA-ECMO first group. A second model (model 2) was also performed using a different approach. In the model 2, all variables significantly (p < 0.05) different between the 2 groups (VA-ECMO vs. IMPELLA®) at 30 days and at 6 months were selected as covariables. For both models, hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated. The proportional hazards assumption was tested and satisfied for all variables. Collinearity was excluded by constructing a correlation matrix between candidate predictors. A p value < 0.05 was considered as statistically significant. All statistical analyses were performed using SPSS 25.0 software (IBM Company, Armonk, New York, NY, USA).
The authors are solely responsible for the design of this study, all analyses, the editing of the paper and its final content. Our study complied with the “Declaration of Helsinki”.
3. Results
3.1. Baseline Characteristics
During the study period, 262 patients were implanted in our tertiary center (University hospital of Lille, France) with a MCS device for refractory CS. Among these, 128 patients were judged eligible to both MCS devices, either VA-ECMO or IMPELLA® (Supplemental Figure S1). VA-ECMO was used as first MCS device in 97 patients and IMPELLA® in 31 patients (mostly IMPELLA-CP®, 84%).
Baseline characteristics of the population are summarized in Table 1. Mean age was 53.8 ± 13.1 year-old and 72.7% of the patients were male. Altogether, 19.5% of the patients had diabetes mellitus. Patients who underwent VA-ECMO as the first MCS device were significantly younger than those who underwent IMPELLA®: 52 ± 12.4 vs. 59.4 ± 13.8 (p = 0.006).
Table 1.
Baseline characteristics of the population.
| Total Population n = 128 |
VA-ECMO First n = 97 |
IMPELLA® First n = 31 |
p | |
|---|---|---|---|---|
| Demographics and Medical History | ||||
| Age (years) | 53.8 ± 13.1 | 52 ± 12.4 | 59.4 ± 13.8 | 0.006 |
| Sex (male), n (%) | 93 (72.7%) | 70 (72.2%) | 23 (74.2%) | 0.825 |
| Body mass index (Kg/m2) | 27 ± 4.9 | 27 ± 5.1 | 26.7 ± 4.3 | 0.735 |
| Diabetes, n (%) | 25 (19.5%) | 18 (18.6%) | 7 (22.6%) | 0.660 |
| History of coronary artery disease, n (%) | 34 (26.6%) | 26 (26.8%) | 8 (25.8%) | 0.913 |
| History of stroke, n (%) | 4 (3.1%) | 2 (2.1%) | 2 (6.5%) | 0.260 |
| Peripheral artery disease, n (%) | 3 (2.3%) | 1 (1%) | 2 (6.5%) | 0.154 |
| Renal failure before admission, n (%) | 7 (5.5%) | 5 (5.2%) | 2 (6.5%) | 0.999 |
| Admission | ||||
| Acute myocardial infarction, n (%) | 72 (56.3%) | 51 (52.6%) | 21 (67.7%) | 0.138 |
| Left ventricular ejection fraction (LVEF,%) | 21.8 ± 15.5 | 19.1 ± 13.8 | 27.2 ± 17.6 | 0.017 |
| Creatinine (mg/L) | 18 ± 10.1 | 18.5 ± 10.3 | 16.5 ± 9.6 | 0.353 |
| Hemoglobin (g/dL) | 11.9 ± 2.6 | 11.3 ± 2.4 | 13.5 ± 2.6 | <0.001 |
| Lactate (mmol/L) | 5.82 ± 4.93 | 6.84 ± 5.33 | 3.03 ± 1.57 | <0.001 |
| ASAT (IU/L) | 460 ± 749 | 498.3 ± 835 | 348.8 ± 397.9 | 0.340 |
| ALAT (IU/L) | 269.5 ± 552.1 | 325.6 ± 627.5 | 104.8 ± 101.9 | 0.054 |
| PT (%) | 63.2 ± 31.2 | 61.7 ± 33.9 | 69 ± 17 | 0.322 |
| Bilirubin (mg/L) | 13.2 ± 14.5 | 14 ± 15.2 | 10.3 ± 11.7 | 0.289 |
| CRP-us (mg/L) | 68.7 ± 75.9 | 68.2 ± 71.7 | 70.3 ± 88.7 | 0.903 |
| Mechanical support | ||||
| VA-ECMO, n (%) | 107 (83.6%) | 97 (100%) | 10 (32.3%) | - |
| IMPELLA®, n (%) | 41 (32%) | 10 (10.3%) | 31 (100%) | - |
| IMPELLA-CP®, n (%) | 34 (26.6%) | 7 (7.2%) | 27 (87.1%) | - |
| VA-ECMO as first device, n (%) | 97 (75.8%) | 97 (100%) | - | - |
| IMPELLA® as first device, n (%) | 31 (24.2%) | - | 31 (100%) | - |
| Duration of MCS (days) | 8.6 ± 9.2 | 9.4 ± 10.1 | 6 ± 5 | 0.077 |
ASAT = aspartate aminotransferase; ALAT = alanine aminotransferase; PT = prothrombin time; CRP = C-reactive protein; VA-ECMO = veno-arterial membrane oxygenation; MCS = mechanical circulatory support.
At admission, CS was mainly the consequence of acute myocardial infarction (56.3%). LVEF was significantly lower in patients who underwent VA-ECMO as the first MCS device: 19.1 ± 13.8 vs. 27.2 ± 17.6 (p = 0.017). Lactate level was higher: 6.84 ± 5.33 vs. 3.03 ± 1.57 mmol/L (p < 0.001) and hemoglobin level was lower 11.3 ± 2.4 vs. 13.5 ± 2.6 g/dL (p < 0.001) in VA-ECMO first patients. There was no difference for other baseline characteristics.
3.2. Outcomes
Duration of MCS was similar between both groups, respectively 9.4 ± 10.1 days in the VA-ECMO group and 6 ± 5 days in the IMPELLA® group (p = 0.077).
Outcomes are summarized in Table 2. In our study, 30-day (primary endpoint) and 6-month mortality rates were 46.9% and 52.3%, respectively. The composite of all-cause death, LVAD or heart transplantation was of 68.8% at 30 days and 73.4% at 6 months. At 6 months, recovery was observed in 38 patients (29.7%).
Table 2.
30-day and 6-month outcomes.
| Total Population n = 128 |
VA-ECMO First n = 97 |
IMPELLA First n = 31 |
p | |
|---|---|---|---|---|
| 30-Day Outcomes | ||||
| 30-day mortality, n (%) | 60 (46.9%) | 42 (43.3%) | 18 (58.1%) | 0.152 |
| Bridge to left ventricular assist device (LVAD, n %) | 18 (14.1%) | 14 (14.4%) | 4 (12.9%) | 0.831 |
| Bridge to transplantation, n (%) | 14 (10.9%) | 14 (14.4%) | 0 | 0.025 |
| Composite of all-cause death, LVAD, transplantation, n (%) | 88 (68.8%) | 67 (69.1%) | 21 (67.7%) | 0.889 |
| Need for MCS escalation, n (%) | 20 (15.6%) | 10 (10.3%) | 10 (32.3%) | 0.003 |
| Time between first MCS and escalation (Days) | 3.1 ± 4 | 5 ± 5 | 1.1 ± 0.9 | 0.026 |
| Stroke, n (%) | 15 (11.7%) | 13 (13.4%) | 2 (6.5%) | 0.295 |
| Sepsis, n (%) | 46 (35.9%) | 39 (40.2%) | 7 (22.6%) | 0.075 |
| Renal replacement therapy, n (%) | 60 (46.9%) | 43 (44.3%) | 17 (54.8%) | 0.307 |
| Major bleeding, n (%) | 48 (37.5%) | 39 (40.2%) | 9 (29%) | 0.263 |
| Vascular complication related to MCS insertion, n (%) | 21 (16.5%) | 15 (15.5%) | 6 (19.4%) | 0.627 |
| Myocardial recovery, n (%) | 37 (28.9%) | 29 (29.9%) | 8 (25.8%) | 0.662 |
| Six-Month Outcomes | ||||
| 6-month mortality | 67 (52.3%) | 47 (48.5%) | 20 (64.5%) | 0.119 |
| Bridge to LVAD, n (%) | 20 (15.6%) | 15 (15.5%) | 5 (16.1%) | 0.999 |
| Bridge to transplantation, n (%) | 16 (12.5%) | 16 (16.5%) | 0 | 0.016 |
| Composite of all-cause death, LVAD, transplantation | 94 (73.4%) | 71 (73.2%) | 23 (74.2%) | 0.913 |
| Need for MCS escalation, n (%) | 20 (15.6%) | 10 (10.3%) | 10 (32.3%) | 0.003 |
| Time between first MCS and escalation (Days) | 3.1 ± 4 | 5 ± 5 | 1.1 ± 0.9 | 0.026 |
| Stroke, n (%) | 16 (12.5%) | 14 (14.4%) | 2 (6.5%) | 0.353 |
| Sepsis, n (%) | 53 (41.4%) | 43 (44.3%) | 10 (32.3%) | 0.089 |
| Renal replacement therapy, n (%) | 63 (49.2%) | 44 (45.4%) | 19 (61.3%) | 0.279 |
| Major bleeding, n (%) | 52 (40.6%) | 40 (41.2%) | 12 (38.7%) | 0.771 |
| Vascular complication related to MCS insertion, n (%) | 21 (16.5%) | 15 (15.5%) | 6 (19.4%) | 0.627 |
| Myocardial recovery, n (%) | 38 (29.7%) | 30 (30.9%) | 8 (25.8%) | 0.587 |
MCS = mechanical circulatory support.
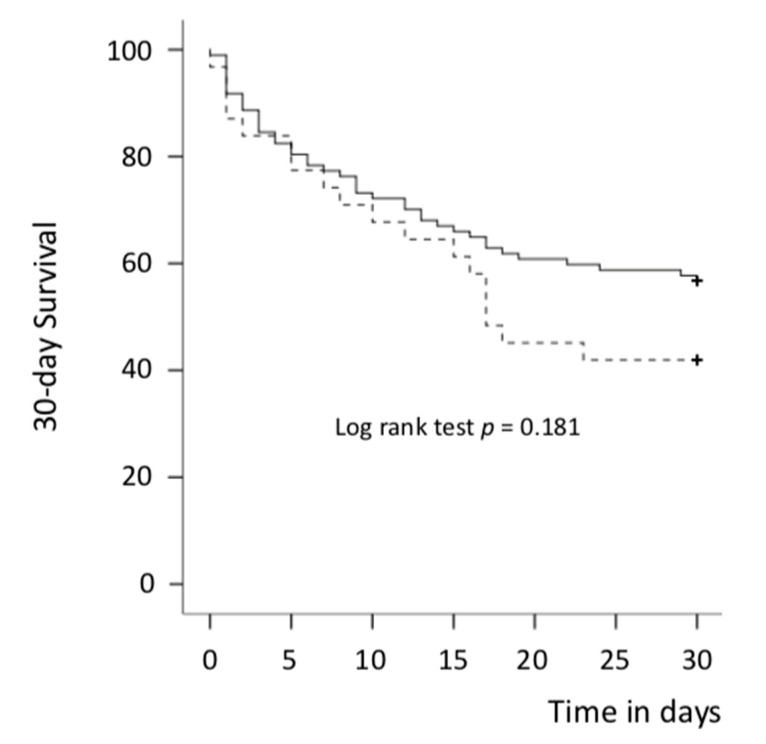
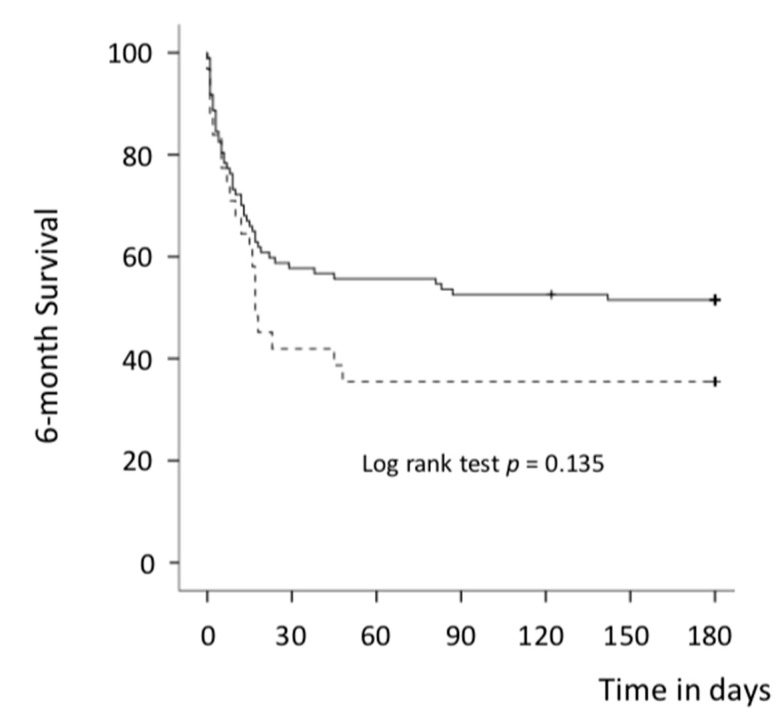
In the univariate analysis, there was overall no significant difference between the VA-ECMO first group and IMPELLA® first group in 30-day (primary endpoint) and 6-month mortality rates (43.3 % vs. 58.1%, p = 0.152 and 48.5% vs. 64.5%, p = 0.119) (Table 3 and Table S1, Figure 2 and Figure 3). After adjustment (multivariate Cox analysis, model 1), VA-ECMO as the first MCS device implanted was significantly associated with better survival at 30 days and 6 months: HR = 0.25 (0.10–0.65) (p = 0.004) and 0.27 (0.11–0.64) (p = 0.001), respectively (Table 4 and Table S2). Results were highly concordant with the model 2 (Tables S3 and S4). The composite of all-cause death, LVAD or heart transplantation was similar between both groups at 30 days and 6 months: 69.1% vs. 67.7%, p = 0.889 and 73.2% vs. 74.2%, p = 0.913, respectively. No difference was observed between both groups in other endpoints studied (Table 2) except for a lower rate of heart transplantation in the IMPELLA® first group.
Table 3.
Variables associated with 30-day mortality after adjustment (univariate analysis).
| Total Population n = 128 |
Alive at 30 Days n = 68 |
Dead at 30 Days n = 60 |
p | |
|---|---|---|---|---|
| Demographics and Medical History | ||||
| Age (years) | 53.8 ± 13.1 | 51 ± 13.6 | 56.9 ± 11.8 | 0.011 |
| Sex (male), n (%) | 93 (72.7%) | 43 (63.2%) | 50 (83.3%) | 0.011 |
| Body mass index (Kg/m2) | 27 ± 4.9 | 26.6 ± 4.8 | 27.4 ± 5 | 0.404 |
| Diabetes, n (%) | 25 (19.5%) | 10 (14.7%) | 15 (25%) | 0.118 |
| History of coronary artery disease, n (%) | 34 (26.6%) | 18 (26.5%) | 16 (26.7%) | 0.980 |
| History of stroke, n (%) | 4 (3.1%) | 0 | 4 (6.7%) | 0.042 |
| Peripheral artery disease, n (%) | 3 (2.3%) | 0 | 3 (5%) | 0.089 |
| Renal failure before admission, n (%) | 7 (5.5%) | 5 (7.4%) | 2 (3.3%) | 0.456 |
| Admission | ||||
| Acute myocardial infarction, n (%) | 72 (56.3%) | 32 (47.1%) | 40 (66.7%) | 0.026 |
| LVEF (%) | 21.8 ± 15.5 | 20.8 ± 14 | 23.1± 17.4 | 0.472 |
| Creatinine (mg/L) | 18 ± 10.1 | 16.1± 8.3 | 20.2 ± 11.6 | 0.021 |
| Hemoglobin (g/dL) | 11.9 ± 2.6 | 11.7 ± 2.6 | 12.1 ± 2.6 | 0.503 |
| Lactate (mmol/L) | 5.82 ± 4.93 | 4.83 ± 3.48 | 7.09 ± 6.12 | 0.013 |
| ASAT (IU/L) | 460 ± 749 | 442.3 ± 878.9 | 482.7 ± 546.3 | 0.770 |
| ALAT (IU/L) | 269.5 ± 552.1 | 209.6 ± 484.6 | 340.1 ± 619.3 | 0.194 |
| PT (%) | 63.2 ± 31.2 | 67.9 ± 36.5 | 57.1 ± 21.4 | 0.070 |
| Bilirubin (mg/L) | 13.2 ± 14.5 | 11.2 ± 11.4 | 15.9 ± 17.7 | 0.098 |
| CRP-us (mg/L) | 68.7 ± 75.9 | 57.7 ± 83.9 | 83.9 ± 86.1 | 0.086 |
| Mechanical Support | ||||
| VA-ECMO, n (%) | 107 (83.6%) | 57 (83.8%) | 50 (83.3%) | 0.940 |
| IMPELLA®, n (%) | 41 (32%) | 16 (23.5%) | 25 (41.7%) | 0.028 |
| IMPELLA-CP®, n (%) | 34 (26.6%) | 15 (22.1%) | 19 (31.7%) | 0.141 |
| VA-ECMO as first device, n (%) | 97 (75.8%) | 55 (80.9%) | 42 (70%) | 0.152 |
| IMPELLA® as first device, n (%) | 31 (24.2%) | 13 (19.1%) | 18 (30%) | 0.152 |
| Duration of MCS (Days) | 8.6 ± 9.2 | 9.5 ± 11.1 | 7.5 ± 6.4 | 0.230 |
Abbreviations = cf. Table 1.
Figure 2.
Thirty-day survival curves for all-cause death (Kaplan–Meier curves) in both groups. Solid line: VA-ECMO first group and dotted line: IMPELLA® first group; VA-ECMO = veno-arterial extracorporeal membrane oxygenation. + = patient censored.
Figure 3.
Six-month survival curves for all-cause death (Kaplan–Meier curves) in both groups. Solid line: VA-ECMO first group and dotted line: IMPELLA® first group; VA-ECMO = veno-arterial extracorporeal membrane oxygenation; + = patient censored.
Table 4.
Variables associated with 30-day mortality after adjustment (Cox multivariate analysis, model 1).
| Hazard Ratio | 95% Confidence Interval | p | |
|---|---|---|---|
| Age (per year) | 1.03 | 0.99–1.07 | 0.073 |
| Sex male | 5.70 | 1.85–17.51 | 0.002 |
| Diabetes | 1.51 | 0.68–3.56 | 0.309 |
| Acute myocardial infarction at admission | 2.79 | 1.29–6.03 | 0.009 |
| LVEF (per %) | 0.99 | 0.97–.01 | 0.349 |
| Lactate level (per one unit) | 1.17 | 1.10–1.25 | <0.001 |
| Creatinine level (per one unit) | 1.04 | 1.01–1.08 | 0.026 |
| Hemoglobin level (per one unit) | 0.92 | 0.81–1.05 | 0.236 |
| VA-ECMO first | 0.25 | 0.10–.65 | 0.004 |
Cox model: age, sex, diabetes, acute myocardial infarction at admission, left ventricle ejection fraction, lactate level, creatinine level, hemoglobin level, VA-ECMO first; variables of interest were selected based on the previous literature. LVEF = left ventricular ejection fraction; VA-ECMO = veno-arterial membrane oxygenation.
Of note, during follow-up, 15.6% of the patients (n = 20) required MCS escalation. The rate of MCS escalation was significantly lower in the VA-ECMO first group: 10.3% of the VA-ECMO first patients were unloaded with IMPELLA® combination and 32.3% of the IMPELLA® first patients were upgraded with VA-ECMO to ensure adequate perfusion (p = 0.003). In addition, MCS escalation was required earlier after first MCS implantation in the IMPELLA® first group: 1.1 ± 0.9 vs. 5 ± 5 days (p = 0.026). Thirty-day and 6-month mortalities were higher in patients requiring MCS escalation during follow-up: 41.7% vs. 75% at 30 days and 47.2% vs. 80% at 6 months. Mortality was however similar between groups in those patients who required escalation: 70% vs. 80% (p = 0.999) at 30 days and 70% vs. 90% (p = 0.582) at 6 months in the IMPELLA® and VA-ECMO group, respectively.
4. Discussion
In our selected population (patients eligible to both type of devices), IMPELLA® devices were used in less severe patients as illustrated by a higher baseline LVEF and lower lactate level. All-cause 30-day and 6-month mortality rates were 46.9% and 52.3% respectively in the overall population and comparable with previous literature [11,12,13,14,15,16,17]. In the univariate analysis, VA-ECMO tends to be associated with better outcomes (not significant). Importantly, after adjustment, VA-ECMO first patients showed however significantly better 30-day and 6-month outcomes as compared to IMPELLA® first patients (HR = 0.25 for 30-day mortality, p = 0.004). In addition, a 3-fold lower need for MCS escalation was observed in the VA-ECMO group.
To date, head-to-head comparison of IMPELLA® versus VA-ECMO is limited since only a few studies focused on this topic in the literature [11,12,13,14,15,16,17]. In summary, all of these show similar outcomes between groups. Importantly, it should however be acknowledged that in these previous studies, heterogeneous patients were included with a high rate of patients with cardiac arrest (from 23% to 63%). By contrast, patients with cardiac arrest were excluded from our analysis since prognosis was rather related to neurological than cardiac disorders in this subset of patients. In addition, patients with right ventricle failure and/or severe hypoxemia were often not excluded in the previous literature. As a matter of fact, these previous studies did not select patients eligible to both strategies as we did and patient characteristics therefore largely differed between groups, even more than what we had observed in our analysis (biases difficult to account for even after adjustment or propensity score matching). In addition, the size of some of these studies did not allow statistical adjustment between groups.
An elegant recent animal study aimed to address hemodynamic properties of IMPELLA® and VA-ECMO under similar hemodynamic conditions at equal flow rates (P8 for IMPELLA® CP and pump flow at 3.2 L/min for VA-ECMO) in 12 swine females with induced acute myocardial infarction-CS [18]. At baseline, MAP and arterial lactate were similar in IMPELLA® and VA-ECMO groups (31 vs. 34 mmHg, p = 0.47 and 3.8 vs. 3.0 mmol/L, p = 0.26 respectively). After 60 min of support, both devices restored lactate levels (1.7 mmol/L for IMPELLA® group vs. 2.4 for VA-ECMO group, p = 0.75). Better unloading was achieved with IMPELLA® (pressure volume area 2456 vs. 7101 mmHg.mL−1, p = 0.004) but a greater improvement in venous oxygen saturation was observed in the VA-ECMO group (venous O2 cerebral saturation 33 vs. 69%, p = 0.04). In this model, results highlight similar performance of IMPELLA® and VA-ECMO to normalize tissular perfusion. Translation of these hemodynamic data into clinical practice and patient’s outcomes is however challenging: in this study, MCS was started immediately after CS initiation, a situation rarely encountered in a real-life setting.
MCS escalation should be regarded as the failure of the first chosen device. In our study, support upgrade was significantly more frequent in the IMPELLA® first group. This point may be of main importance in daily practice since close to 1/3 of the patients in the IMPELLA® first group required escalation (as compared to only 10% in the VA-ECMO group). Akanni et al. [17] reported their experience with MCS escalation, whether it was related to insufficient perfusion or refractory LV distension management. As expected, adding IMPELLA® to VA-ECMO significantly reduced pulmonary artery pressures and adding VA-ECMO to on-going IMPELLA® support significantly improved perfusion indices (lactate, ScvO2) and oxygenation (P/F ratio). In their prospective study, Garan et al. [14] noted that, overall, 47% of their patients were upgraded with almost a 3-fold higher rate in the IMPELLA® first group (64.5% vs. 25%) similarly to our study. The question is: insufficient perfusion (reason for upgrade in the IMPELLA® group) worse than the need for LV unloading (reason for upgrade in the VA-ECMO group) in terms of patient outcomes? The answer is not easy and observational data showed conflicting results. If VA-ECMO upgrade in IMPELLA® patients were associated with better survival in the study of Mourad et al. (50% vs. 33% at discharge) [16], the opposite effect was observed in the study of Garan et al. [14] with a survival rate to discharge 75% of VA-ECMO first patients versus 50% for IMPELLA® first patients. In our study, as expected, 30-day and 6-month mortalities were higher in upgraded patients; but this increase was not significantly influenced by the group (30-day mortality of 70% in VA-ECMO first vs. 80% in IMPELLA® first patients, p = non-significant). Of note, we observed that time between first MCS implantation and need for escalation was significantly shorter for IMPELLA® first patients (1.1 ± 0.9 days vs. 5 ± 5 days, p = 0.026). Timing of MCS upgrade was not available in previous studies on combined support since most of them mixed concomitant implantation of both devices, IMPELLA® first/VA-ECMO staged, and VA-ECMO/IMPELLA® staged [19]. Noteworthy, it is important to note that an intentional early combination of support devices (a situation very different from the need for MCS escalation) holds promise (despite a higher risk of complications), and recent studies suggest a potential mortality benefit of an early VA-ECMO and IMPELLA® association [20,21] to fulfill essential conditions (adequate perfusion, LV unloading) for improving CS mortality.
Sepsis, major bleeding, vascular complication, or stroke are serious concerns that increase mortality in CS patients and could even compromise durable HF therapy candidacy (LVAD/heart transplantation) [22]. It is very difficult to reliably appreciate the safety profile of MCS because standard definitions were lacking before a recent expert consensus statement publication [7]. In our study, as compared to the most previous literature, rates of major complications were similar between both groups. In contrast to our results and those of Garan et al. [14] and Mourad et al. [16], Karami et al. [15] however observed more device-related vascular complications in the VA-ECMO group (39.5% vs. 16.7%, p = 0.001).
Our study (highly selected population) emphasizes the fact that after adjustment, VA-ECMO was associated with better outcome and a less frequent need for MCS escalation. Therefore, our results suggest that IMPELLA® use (a quick, easy, and less invasive technique as compared to VA-ECMO) should be restricted to the less severe patients and at the very early phase of the CS depending on local facilities. Indeed, CS patients are initially often referred to PCI-capable hospitals but without advanced MCS capabilities. From a pathophysiological view, transvalvular devices are very attractive by solving the CS hemodynamic equation (systemic and coronary perfusion, ventricular and hepatorenal unloading) especially for AMI-CS patients without major organ failure or profound hypoperfusion. IMPELLA® devices could find a real central place for preshock or mild CS management and probably before primary percutaneous coronary intervention (PCI) [23,24]. Current studies are underway to solve these major issues and better define the role and timing of MCS deployment for this subset of patients.
5. Strengths and Limitations
In our study, excluding RV failure, cardiac arrest, LV thrombus, or severe hypoxemia offers a homogeneous population regarding the CS phenotype with eligibility for either VA-ECMO or IMPELLA®. It therefore allows a fair comparison of both devices. However, the retrospective design has important limitations with inherent biases. This is a single center study that only reflects practices in our institution, which may not be generalizable worldwide. Finally and unfortunately, detailed hemodynamic data were not available for our patients, and MCS escalation effects cannot be precisely assessed.
6. Conclusions
In our study, as consistently observed in the literature in the field, VA-ECMO implanted patients for refractory CS showed more severe hemodynamic compromise as compared to IMPELLA® patients. In a restricted population eligible for both devices and after adjustment, VA-ECMO was associated with improved survival rate and a lower need for MCS escalation. In advanced stages of CS, VA-ECMO should be preferred and promptly started to ensure adequate perfusion in critical settings. IMPELLA® device, by its attractive properties, could be considered in less severe situations to promote myocardial recovery and reverse the downward spiral of CS. Randomized data are needed to confirm our findings.
Acknowledgments
Authors are thankful for all nurse staffs from the CICU, cardiac surgery and interventional cardiology departments.
Supplementary Materials
The following are available online at https://www.mdpi.com/2077-0383/10/4/759/s1, Figure S1: Local protocol for refractory CS management, Table S1: Variables associated with 6-month mortality after adjustment (univariate analysis), Table S2. Variables associated with 6-month mortality after adjustment (Cox multivariate analysis, model 1), Table S3. Variables associated with 30-day mortality after adjustment (Cox multivariate analysis, model 2), Table S4. Variables associated with 6-month mortality after adjustment (Cox multivariate analysis, model 2).
Author Contributions
Conceptualization G.S., N.R. and G.L.; Methodology: O.S., F.V., G.L.; Software: O.S.; Validation: A.V., M.D.M., G.L.; Formal analysis: G.L.; Investigation: N.R., O.S., V.B., G.L.; Resources: E.R., E.V.B., S.P., A.C., F.J., M.D.M., B.V., L.B., C.D. (Clément Delmas), C.D. (Cédric Delhaye), F.V., E.P., N.A.; Data curation: G.S., O.S., N.R., V.B., M.D.M., E.R., A.V., F.V., G.L.; Writing-original draft preparation: G.S., N.R., G.L.; Writing-review and editing: G.S., N.R., A.V., F.V., N.L., G.L.; Visualization: G.L.; Supervision: G.L.; Project administration: G.L.; Funding acquisition: G.L. All authors have read and agreed to this manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
All authors have disclosed that they do not have any conflicts of interest in direct connection with this article.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Aissaoui N., Puymirat E., Delmas C., Ortuno S., Durand E., Bataille V., Drouet E., Bonello L., Bonnefoy-Cudraz E., Lesmeles G., et al. Trends in cardiogenic shock complicating acute myocardial infarction. Eur. J. Heart Fail. 2020;22:664–672. doi: 10.1002/ejhf.1750. [DOI] [PubMed] [Google Scholar]
- 2.Thiele H., Ohman E.M., De Waha-Thiele S., Zeymer U., Desch S. Management of cardiogenic shock complicating myocardial infarction: An update 2019. Eur. Hear. J. 2019;40:2671–2683. doi: 10.1093/eurheartj/ehz363. [DOI] [PubMed] [Google Scholar]
- 3.Rao P., Khalpey Z., Smith R., Burkhoff D., Kociol R.D. Venoarterial Extracorporeal Membrane Oxygenation for Cardiogenic Shock and Cardiac Arrest. Circ. Heart Fail. 2018;11:e004905. doi: 10.1161/CIRCHEARTFAILURE.118.004905. [DOI] [PubMed] [Google Scholar]
- 4.Stretch R., Sauer C.M., Yuh D.D., Bonde P. National Trends in the Utilization of Short-Term Mechanical Circulatory Support. J. Am. Coll. Cardiol. 2014;64:1407–1415. doi: 10.1016/j.jacc.2014.07.958. [DOI] [PubMed] [Google Scholar]
- 5.Schurtz G., Laine M., Delmas C., Kerbaul F., Puymirat E., Lemesle G., Bonello L. Mechanical Support in Cardiogenic Shock Complicating Acute Coronary Syndrome: Ready for Prime Time? Curr. Vasc. Pharmacol. 2018;16:418–426. doi: 10.2174/1570161116666180116165544. [DOI] [PubMed] [Google Scholar]
- 6.Dhruva S.S., Ross J.S., Mortazavi B.J., Hurley N.C., Krumholz H.M., Curtis J.P., Berkowitz A., Masoudi F.A., Messenger J.C., Parzynski C.S., et al. Association of Use of an Intravascular Microaxial Left Ventricular Assist Device vs Intra-aortic Balloon Pump with In-Hospital Mortality and Major Bleeding Among Patients with Acute Myocardial Infarction Complicated by Cardiogenic Shock. JAMA. 2020;323:734. doi: 10.1001/jama.2020.0254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kormos R.L., Antonides C.F.J., Goldstein D.J., Cowger J.A., Starling R.C., Kirklin J.K., Rame J.E., Rosenthal D., Mooney M.L., Caliskan K., et al. Updated definitions of adverse events for trials and registries of mechanical circulatory support: A consensus statement of the mechanical circulatory support academic research consortium. J. Heart Lung Transpl. 2020;39:735–750. doi: 10.1016/j.healun.2020.03.010. [DOI] [PubMed] [Google Scholar]
- 8.Hicks K.A., Mahaffey K.W., Mehran R., Nissen S.E., Wiviott S.D., Dunn B., Solomon S.D., Marler J.R., Teerlink J.R., Farb A., et al. 2017 Cardiovascular and Stroke Endpoint Definitions for Clinical Trials. Circulation. 2018;137:961–972. doi: 10.1161/CIRCULATIONAHA.117.033502. [DOI] [PubMed] [Google Scholar]
- 9.Singer M., Deutschman C.S., Seymour C.W., Shankar-Hari M., Annane D., Bauer M., Bellomo R., Bernard G.R., Chiche J.-D., Coopersmith C.M., et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016;315:801–810. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mehran R., Rao S.V., Bhatt D.L., Gibson C.M., Caixeta A., Eikelboom J., Kaul S., Wiviott S.D., Menon V., Nikolsky E., et al. Standardized Bleeding Definitions for Cardiovascular Clinical Trials. Circulation. 2011;123:2736–2747. doi: 10.1161/CIRCULATIONAHA.110.009449. [DOI] [PubMed] [Google Scholar]
- 11.Karatolios K., Chatzis G., Markus B., Luesebrink U., Ahrens H., Divchev D., Syntila S., Jerrentrup A., Schieffer B. Comparison of mechanical circulatory support with venoarterial extracorporeal membrane oxygenation or Impella for patients with cardiogenic shock: A propensity-matched analysis. Clin. Res. Cardiol. 2020:1–8. doi: 10.1007/s00392-020-01777-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schiller P., Hellgren L., Vikholm P. Survival after refractory cardiogenic shock is comparable in patients with Impella and veno-arterial extracorporeal membrane oxygenation when adjusted for SAVE score. Eur. Heart J. Acute Cardiovasc. Care. 2017;8:329–337. doi: 10.1177/2048872618799745. [DOI] [PubMed] [Google Scholar]
- 13.Lamarche Y., Cheung A., Ignaszewski A., Higgins J., Kaan A., Griesdale D.E., Moss R. Comparative outcomes in cardiogenic shock patients managed with Impella microaxial pump or extracorporeal life support. J. Thorac. Cardiovasc. Surg. 2011;142:60–65. doi: 10.1016/j.jtcvs.2010.07.075. [DOI] [PubMed] [Google Scholar]
- 14.Garan A.R., Takeda K., Salna M., Vandenberge J., Doshi D., Karmpaliotis D., Kirtane A.J., Takayama H., Kurlansky P. Prospective Comparison of a Percutaneous Ventricular Assist Device and Venoarterial Extracorporeal Membrane Oxygenation for Patients with Cardiogenic Shock Following Acute Myocardial Infarction. J. Am. Heart Assoc. 2019;8:e012171. doi: 10.1161/JAHA.119.012171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Karami1 M., den Uil C.A., Ouweneel D.M., Scholte N.T.B., Engström A.E., Akin S., Lagrand W.K., Vlaar A.P.J., Jewbali L.S., Henriques J.P.S. Mechanical circulatory support in cardiogenic shock from acute myocardial infarction: Impella CP/5.0 versus ECMO. Eur. Heart J. Acute Cardiovasc. Care. 2019;33 doi: 10.1177/2048872619865891. [DOI] [PubMed] [Google Scholar]
- 16.Mourad M., Gaudard P., De La Arena P., Eliet J., Zeroual N., Rouvière P., Roubille F., Albat B., Colson P.H. Circulatory Support with Extracorporeal Membrane Oxygenation and/or Impella for Cardiogenic Shock during Myocardial Infarction. ASAIO J. 2018;64:708–714. doi: 10.1097/MAT.0000000000000704. [DOI] [PubMed] [Google Scholar]
- 17.Akanni O.J., Takeda K., Truby L.K., Kurlansky P.A., Chiuzan C., Han J., Topkara V.K., Yuzefpolskaya M., Colombo P.C., Karmpaliotis D., et al. EC-VAD: Combined Use of Extracorporeal Membrane Oxygenation and Percutaneous Microaxial Pump Left Ventricular Assist Device. ASAIO J. 2019;65:219–226. doi: 10.1097/MAT.0000000000000804. [DOI] [PubMed] [Google Scholar]
- 18.Møller-Helgestad O.K., Hyldebrandt J.A., Banke A., Rud C.S., Udesen N.L., Linde L., Okkels-Jensen L., Schmidt H., Ravn H.B., Møller J.E. Impella CP or VA-ECMO in profound cardiogenic shock: Left ventricular unloading and organ perfusion in a large animal model. EuroIntervention. 2019;14:e1585–e1592. doi: 10.4244/EIJ-D-18-00684. [DOI] [PubMed] [Google Scholar]
- 19.Schrage B., Burkhoff D., Rübsamen N., Becher P.M., Schwarzl M., Bernhardt A., Grahn H., Lubos E., Söffker G., Clemmensen P., et al. Unloading of the Left Ventricle during Venoarterial Extracorporeal Membrane Oxygenation Therapy in Cardiogenic Shock. JACC Heart Fail. 2018;6:1035–1043. doi: 10.1016/j.jchf.2018.09.009. [DOI] [PubMed] [Google Scholar]
- 20.Schrage B., Becher P.M., Bernhardt A., Bezerra H., Blankenberg S., Brunner S., Colson P., Deseda G.C., Dabboura S., Eckner D., et al. Left Ventricular Unloading Is Associated with Lower Mortality in Patients with Cardiogenic Shock Treated with Venoarterial Extracorporeal Membrane Oxygenation. Circulation. 2020;142:2095–2106. doi: 10.1161/CIRCULATIONAHA.120.048792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tongers J., Sieweke J.-T., Kühn C., Napp L.C., Flierl U., Röntgen P., Schmitto J.D., Sedding D.G., Haverich A., Bauersachs J., et al. Early Escalation of Mechanical Circulatory Support Stabilizes and Potentially Rescues Patients in Refractory Cardiogenic Shock. Circ. Heart Fail. 2020;13:e005853. doi: 10.1161/CIRCHEARTFAILURE.118.005853. [DOI] [PubMed] [Google Scholar]
- 22.Freund A., Jobs A., Lurz P., Feistritzer H.-J., De Waha-Thiele S., Meyer-Saraei R., Montalescot G., Huber K., Noc M., Windecker S., et al. Frequency and Impact of Bleeding on Outcome in Patients with Cardiogenic Shock. JACC Cardiovasc. Interv. 2020;13:1182–1193. doi: 10.1016/j.jcin.2020.02.042. [DOI] [PubMed] [Google Scholar]
- 23.Basir M.B., Schreiber T.L., Grines C.L., Dixon S.R., Moses J.W., Maini B.S., Khandelwal A.K., Ohman E.M., O’Neill W.W. Effect of Early Initiation of Mechanical Circulatory Support on Survival in Cardiogenic Shock. Am. J. Cardiol. 2017;119:845–851. doi: 10.1016/j.amjcard.2016.11.037. [DOI] [PubMed] [Google Scholar]
- 24.Bonello L., Delmas C., Schurtz G., Leurent G., Bonnefoy E., Aissaoui N., Henry P. Mechanical circulatory support in patients with cardiogenic shock in intensive care units: A position paper of the ‘‘Unité de Soins Intensifs de Cardiologie’’ group of the French Society of Cardiology, endorsed by the “‘Groupe Athérome et Cardiologie Interventionnelle’” of the French Society of Cardiology. Arch. Cardiovasc. Dis. 2018;111:601–612. doi: 10.1016/j.acvd.2018.03.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.