Abstract
Introduction
Frontline healthcare providers are redeployed to areas outside their clinical expertise and assigned high-loading workload to address the surge of patients with each coronavirus outbreak. Their importance in crisis is not in doubt. However, they experienced considerable physical distress and psychological stressors, even leading to psychological illness and infection in this environment. There is an urgent need to accurately, comprehensively and objectively understand their experiences, perceptions and current situation of burnout, post-traumatic stress disorder (PTSD), anxiety, depression, insomnia and coronavirus infection. Therefore, this protocol is to conduct a mixed-methods systematic review to summarise the evidence on the experiences of healthcare providers and impacts of the coronavirus on their psychological status and infection during the pandemics.
Methods
Published studies on experience, perspective, impact, burnout, PTSD, anxiety, depression, insomnia, and infection of healthcare providers with SARS, Middle East respiratory syndrome and COVID-19, and written in English and Chinese will be accepted. Databases (MEDLINE, EMBASE, CENTRAL, Web of Science, PubMed, Psychology Information, WanFang and SinoMed) from inception until 30 July 2020 will be searched. Two reviewers will select, screen, extract data and assess the risk of bias independently. Risk of bias of results will be using the Mixed-Methods Appraisal Tool. Using a convergent integrated approach on qualitative/quantitative studies, we will synthesise qualitative and quantitative data separately. The incidence and number of cases about burnout, PTSD, anxiety, depression, insomnia and coronavirus infection among medical staff will be extracted. Then we will transform quantitative data to synthesise narrative findings. This protocol will be reported per the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols guidelines.
Ethics and dissemination
Ethical assessment is not required due to the nature of the proposed systematic review. Findings of our research will be disseminated at conferences related to this field and through publication in peer-reviewed journals.
PROSPERO registration number
CRD42020198506.
Keywords: COVID-19, health & safety, epidemiology, health policy, anxiety disorders, depression & mood disorders
Strengths and limitations of this study.
This is the first mixed-methods systematic review that assesses the experience of healthcare providers and the impact of the coronavirus on them during the outbreak.
We will comprehensively understand the healthcare providers’ real experiences and the coronavirus’ impacts when their lives and security are threatened. This is also stronger evidence in clinical practice of sustained and comprehensive support policies and measures adopted to improve their physical and mental feelings, and health.
This study will include only English and Chinese, and similar topics in other languages were ignored.
The type of research included in the study is limited by the type of published original research, and the definition of first-line healthcare workers is non-standardised.
Introduction
Coronaviruses are a kind of single-stranded, positive-sense RNA viruses, enveloped and non-segmented, which exist in nature widely.1 These host-specific viruses infect other mammals, birds and even humans frequently, and lead to diverse clinical syndromes in humans, including respiratory, digestive, liver and neurological disorders.2 Two of the six coronaviruses that have been identified, SARS-CoV and Middle East respiratory syndrome coronavirus (MERS-CoV), are characterised by zoonosis and highly pathogenic, increasing the risk of deaths.3
Coronavirus which is highly pathogenic has been spread in humans for hundreds of years through contact, droplets, aerosols and so on. The number of deaths due to infection of SARS-CoV-2–4 and MERS-CoV far exceeded 10 000 in the past two decades.4 Every outbreak of coronavirus has a tremendous impact on human life and health. The WHO confirmed 8098 cases and 774 (9.6%) deaths during the SARS outbreak in 2002. Similarly, 2494 infections and 34.4% deaths were confirmed during the MERS epidemic from 2012 to 2018. Because of the high infection rate and widespread of coronaviruses, their infection poses a constant threat to human health.
COVID-19 infection is the third outbreak of coronavirus cross-species transmission of sudden public health events after SARS and MERS. It was first reported in the late December 2019, and an ongoing outbreak has been widespread all across the world. As of 16 July 2020, there have been 13 378 853 confirmed cases of COVID-19 globally, including 580 045 deaths, already circulating in 216 countries.5 The WHO declared a state of emergency and could confront long-term challenges worldwide.6
Every outbreak of a new disease, the demand for resources, especially healthcare providers and medical supplies, has increased greatly around the world. In order to resolve this situation, most hospitals have to rapidly reconfigure clinical spaces and restructure clinical teams. Therefore, many healthcare providers are redeployed to areas outside their clinical expertise and are assigned high-loading workload to address the surge of patients with COVID-19. The importance of healthcare providers in this crisis is not in doubt.6 Their health and safety can affect the effectiveness of patients’ treatment and care, and can even determine the control of any outbreak.7 However, they also face great challenges.8
Healthcare providers experienced considerable physical distress when working with patients diagnosed with SARS, MERS and COVID-19.9 10 They were exhausted owing to the intensive care they provided during long shifts in protective suits without toilet breaks. The combination of heavy protective clothing and the hot environmental conditions made them awkward to move, difficult to breathe, hard to hear and covered with sweat they were unable to wipe off.11
Healthcare providers also experienced significant psychological stressors. Recent evidence suggests that even someone who is non-symptomatic can spread COVID-19 with high efficiency. At the same time, little was known about the new virus, including its lethality or how to best care for these patients.12 And they always witness the death of infected people. Hence, they experienced fear of getting infected themselves and spreading infection to their family members. The families, neighbours and community residents who fear exposing themselves13 14 tried to prevent the medical staff from going home after finishing work, which makes the staff socially stressed. Moreover, some environmental stress, such as cultural differences of medical staff between different regions, lack of supplies and temporary workplaces, raised the healthcare workers’ sense of helplessness and frustration.15
It is worth noting that healthcare professionals who take care of patients with coronavirus are more prone to psychological disorders and illnesses, such as burnout, post-traumatic stress disorder (PTSD), anxiety, depression and insomnia. Stress reaction symptoms have been reported in about 10% of healthcare workers in the course and in the aftermath of previous outbreaks of SARS and MERS.16 17 Similar challenges have arisen in the USA, Canada, Taiwan and Hong Kong.18–22 In a cross-sectional survey of 1257 healthcare workers in China during the COVID-19 pandemic, over 70% reported distress, with 50% reporting depression and 34% insomnia.23 But the unexpected findings of one study suggest that the frequency of burnout is significantly smaller in frontline workers than that of healthcare providers in their usual ward.24
In addition, health professionals have become the most vulnerable population to contract the coronavirus. Earlier studies reported that infected healthcare providers accounted for 51% of the SARS cases.25 However, the prevalence of infection with COVID-19 among healthcare workers was only 6% in the Netherlands.26 Similarly, on 7 February the proportion of Chinese medical staff infected grew to 26% in 2020, up from 3% on 1 January 2020.27 28
Although many studies have reported psychological changes and incidence of coronavirus infection among medical staff, the sample size of studies is different and the results provide visible differences. Therefore, there is an urgent need for a systematic review of quantitative research to accurately and objectively understand the current situation of psychology and coronavirus infection for healthcare providers in their industry during outbreaks.
However, some of the studies found that healthcare providers showed great strength and resilience in the face of various challenges. Meanwhile, they had an extraordinary sense of responsibility and a strong spirit of teamwork when treating patients with coronavirus.23 Several studies have discussed the experience of healthcare providers in the face of the epidemic. In this case, systematic review of qualitative study can improve the reliability, generality and policy reference of qualitative research results. In this way, the experiences or perceptions of medical staff are more comprehensively described during an outbreak.
The main aim of the present protocol is to conduct a mixed-methods systematic review to summarise the evidence on the experiences of healthcare providers and impacts on their psychological status and infection during the coronavirus pandemics.
Methods
Protocol registration
This mixed-methods systematic review is reported according to the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) guidelines.29 The protocol has been registered in the International Prospective Register of Systematic Review (PROSPERO) (https://www.crd.york.ac.uk).
Patient and public involvement
This is a systematic review study and therefore does not require patient and/or public involvement.
Design
The mixed-methods systematic review incorporating quantitative and qualitative data is conducted. The qualitative component is undertaken first to comprehensively explore the experience of healthcare providers and the impact of the coronavirus on them during the pandemic. Then the quantitative component of the psychological status and infected condition of caregivers is used to generalise or prove the qualitative results that caregivers are significantly affected during outbreaks. This review used the convergent integrated approach. First, quantitative results are translated into qualitative topics, and then all qualitative studies results are integrated simultaneously30 (see figure 1 for design process).
Figure 1.
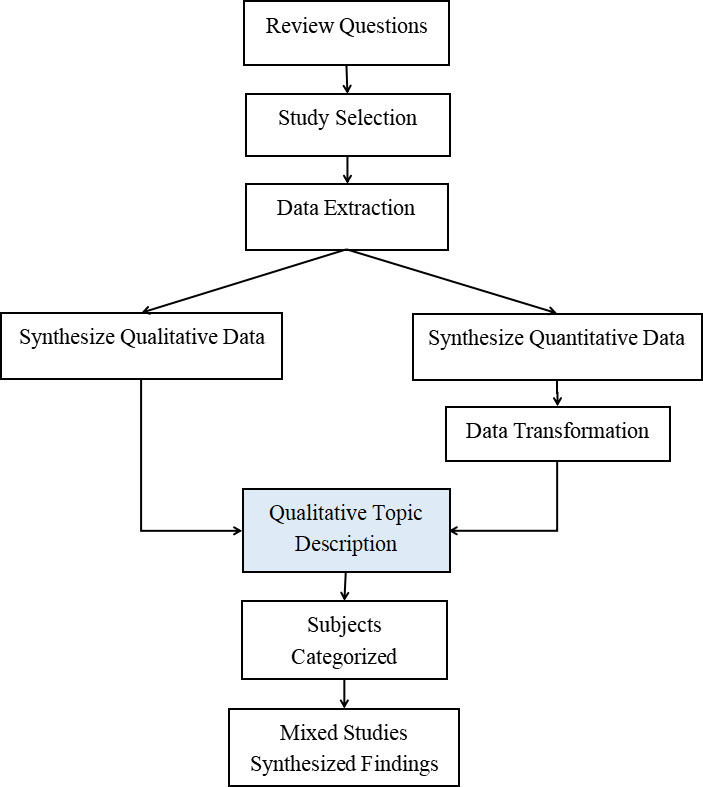
The design process of systematic review.
Data sources and searches
The literature searches have been conducted in electronic bibliographical databases, including MEDLINE, EMBASE, the Cochrane Library (CENTRAL), Web of Science, PubMed, Psychology Information, WanFang data and SinoMed, from inception until 30 July 2020.
An initial search of PubMed has started the original research and review, followed by the identification of keywords found in each title and abstract.We enter these keywords into ‘Medical Subject Headings terms (MeSH)’ box for advanced search in the Cochrane Library, and further search more synonymous terms. After that, we add terms through 10 registered unpublished protocols of the systematic review in PROSPERO. Ultimately, the following search terms in table 1 are used to perform the search. The search terms will use a combination of MeSH terms, free-text words and Boolean operators. The reference section of the included studies will be hand searched for additional relevant studies. The detailed search strategy in PubMed is shown in the PDF document (see online supplemental file 1).
Table 1.
Search terms
| Entries | Theme | Search terms | |
| #1 | Participants | Healthcare providers | (Healthcare Provider) OR (Healthcare Worker) OR (Health Care Provider) OR (health personnel) OR (health professional) OR (Medical staff) OR (Medical worker) OR (Physician) OR (Clinician) OR (Doctor) OR(Nurse) OR (Nursing Staff) OR (Healthcare employee) OR (Paramedic) |
| #2 | Phenomenon/outcome of interest | Experience and impact | Experience OR perception OR Attitude OR Opinion OR Impact OR Affect OR Emotion OR Mood OR Mental OR (Burn out) OR Burnout OR Burn-out OR (Stress Disorders, Post-Traumatic) OR (Post Traumatic Stress Disorder) OR (Post-Traumatic Stress Disorder) OR (Posttraumatic Stress Disorder) OR PTSD OR (Stress Psychological) OR (Psychological Distress) OR (Affective Symptoms) OR Suffering OR anxiety OR Nervousness OR depression OR insomnia OR (sleep disorder) OR (stress levels) OR infection OR incidence OR morbidity |
| #3 | Context | Coronavirus | Coronavirus OR COVID-19 OR SARSCOV2 OR 2019-nCov OR (COVID-19 Ncov) OR (2019 coronavirus) OR (novel coronavirus) OR (new coronavirus) OR (nouveau coronavirus) OR (COVID-19) OR (2019-severe acute respiratory syndrome coronavirus 2) OR (SARS-2) OR (Wuhan seafood market pneumonia virus) OR (SARS) OR SARS-CoV OR (SARS VIRUS) OR (severe acute respiratory syndrome) OR (MERS) OR (MERS-VIRUS) OR (Middle East Respiratory Syndrome) OR (Middle East respiratory syndrome related coronavirus) OR (MERS-CoV) |
| #4 | Types of studies | Cross-sectional, cohort studies and qualitative studies | (cohort study) OR (Incidence Study) OR (Cohort Analysis) OR (Cohort Analyses) OR (Concurrent Study) OR (Closed Cohort Study) OR (Historical Cohort Study) OR (Prevalence Study) OR (Disease Frequency Survey) OR (Cross-Sectional) OR (Cross Sectional) OR (Empirical Research) OR (qualitative study) OR (qualitative Research) OR (Qualitative description) OR (phenomenological study) OR (Grounded Theory) OR (ethnography) OR (Anthropology) OR (Behavioral Research) OR (action research) OR (mixed method) OR (mixed-method) OR (Investigative research) OR (Investigative study) |
| Number of articles #1=1,811,427 #2=10,519,278 #3=73 347 #4=6,302,298 #1 AND #2 AND #3 AND #4=2380 (31 July 2020-PubMed) | |||
bmjopen-2020-043686supp001.pdf (133.7KB, pdf)
Inclusion and exclusion criteria
Only published studies are original articles, and studies that reported the experience, perspective, burnout, PTSD, anxiety, depression, insomnia and infection rates of healthcare providers who took care of patients with SARS, MERS and COVID-19 will be accepted in this study. For language restrictions, only studies in English and Chinese will be accepted.
Types of participants
This review will include studies where participants are healthcare providers who treat and cure the patients diagnosed with coronavirus infection, working in designated hospital and having a close contact with infected patients. The gender, age and major field of participants will not be limited. But medical students or trainees will be excluded.
Phenomenon of interest
Our phenomenon of interest will focus on studies that the experience and perspective of healthcare providers who took care of patients, as well as the impact of the coronavirus on them, will be all considered in qualitative review. The terms ‘experience’ and ‘perspective’ consisted of all factors— impact on the feeling and mood of providers from coronavirus. The term ‘impact’ was defined as what healthcare providers perceive the impact on themselves, whether physical, psychological or lifestyle habits.
Outcome of interest
This review will consider quantitative studies about the impact of coronaviruses on the physical and mental health of healthcare providers during the SARS, MERS and COVID-19 pandemic. The quantitative outcomes will include two subsystems. One is included proportions, prevalence and counts of psychological distress and illness (including the incidence of burnout, PTSD, anxiety, depression, insomnia), and the other one is the incidence and number of coronavirus infection. The results must include one or more outcomes. The measurement tool must be an international scale, and a self-made scale will not be considered.
Context
This review will consider studies that were in the context of a pandemic caused by coronavirus, including SARS, MERS and COVID-19. Coronavirus diagnosis was in accordance with the WHO.
Types of studies
We will include studies that use quantitative (including cross-sectional, cohort studies), qualitative (including but not limited to, designs such as phenomenology, grounded theory, ethnography, action research, qualitative description) and mixed-methods methodologies. We will exclude case reports and articles, such as conference abstracts, editorials, letters, reviews and commentaries. Systematic reviews and meta-analyses will not be included, but we will be looking for articles in the systematic review or other types of review in order to identify more articles for this systematic review.
Exclusion criteria
Studies that did not report incidence rate of burnout, PTSD, anxiety, depression or infection rates for healthcare providers in pandemics, and studies that did not state the number of patients will be excluded. Studies that analysed mental and behavioural disorders due to the use of an existing primary disease, alcohol and other drugs will not be included. Studies that measure burnout, PTSD, anxiety, depression and insomnia but do not use the universal international scale will be excluded.
Data collection and analysis
Data management
Covidence systematic review management software, EndNote V.X9, will be used to assist with further data management.31 All identified references following the search will be uploaded and collated into EndNote and duplicates will be removed from the list.
Selection of studies
In phase one, the title and the abstract of each identified study will be independently screened according to the established inclusion criteria by each of the two review authors (NX and TL) to determine which should be assessed further. Full texts for the eligible titles and/or abstracts including those uncertain will be obtained for further assessment on whether to include or not in the study at the second stage.
In order for two reviewers to use consistent evaluation criteria for all retrieved results, we will conduct step-by-step calibration exercises for 30 studies before screening.32 In case 80% agreement is not reached, we will refine the inclusion and exclusion criteria and the calibration will be repeated until the threshold is reached. Disagreement between the two authors will be resolved through discussion, and when needed, there will be arbitration by a third reviewer (MH). Reasons for excluding full-text studies will be recorded.
Data extraction
A standardised form based on previous studies33–35 will be used for data extraction. The form will be created by using a specially developed tool in a Microsoft Excel (V.2016) spreadsheet. In this systematic review, the key data to be extracted are as follows:
Research information: first author, year of publication, country of the study.
Demographic information: populations (doctors, nurses and others), hospital level, sample size, age.
Qualitative studies: study methods, contexts, culture and outcomes of interest (the experiences and perspectives of healthcare providers, and the impacts of coronavirus on them).
Quantitative studies: study design will be extracted. The incidence, proportions or prevalence and number of cases about burnout, PTSD, anxiety, depression, insomnia and coronavirus infection among medical staff will be extracted.
The extracted information from each paper will be checked for congruency and agreed by two reviewers. If additional information or data are required, we will contact the authors of the original studies through email for clarification or addition.
Data synthesis and integration
We will use a convergent integrated approach in accordance with Joanna Briggs Institute (JBI) methodology for conducting a mixed-methods systematic review.35
In the first part, we will synthesise qualitative data by means of thematic synthesis using JBI-QARI software systems. Under the premise of understanding the philosophical thought and methodology of various qualitative studies, two reviewers (NX and TL) repeatedly read, understand, analyse and explain the experiences and perspectives of medical workers and the impacts of coronavirus, and combine similar results to form new categories. Then, the new categories are summed up as an integrated result to form new concepts or interpretations. Two reviewers will independently analyse the extracted data and provide thematic codes. In order to derive a matrix structure, both reviewers will discuss coding and identify thematic issues and categories.
In the second part, we will synthesise quantitative data and perform meta-analysis. Statistical analysis will be conducted using Revman V.5.3. Proportion and SE will be used to analyse the incidence of burnout, PTSD, anxiety, depression, insomnia and infection. Between-study heterogeneity will be assessed using the χ2 test on Cochrane’s Q statistic, and quantified by calculating the I2 statistic (with values of 25%, 50% and 75% as representatives of the low, medium and high heterogeneity, respectively). There will be a methodological heterogeneity between studies included in this study because different scales are used to evaluate. We will use a random-effects meta-analysis to estimate the burnout, PTSD, anxiety, depression, insomnia and coronavirus infection among medical staff. Results will be reported as proportions with corresponding 95% CIs (n% (95% CI (a% to b%))).
The next step is data transformation.34 According to the JBI convergent integrated approach, quantitative data will be converted to ‘qualitative data’ and be transfigured to textual or narrative interpretations to answer the review question.
In a final step, we will extract themes and subtopics in shape of qualified textual description from qualitative results, whether untransformed or transformed, and collate and categorise them according to consistencies of content. These categories will then be subjected to a synthesis to produce a single comprehensive set of synthesised findings that can be used as a basis for evidence-based practice.
Subgroup analysis
The doctors, nurses and other medical staff are all working together to combat the coronavirus pandemic, but they have different duties and their experience may vary from each other. Hence, we plan to conduct subgroup analyses to examine whether a profession has different experiences and impacts. For qualitative data, we will label the results of articles that are only included in a class of research objects when extracting the results of qualitative studies. If the experience of different occupations is the same, we will integrate the results and not report according to different occupations. If people in different occupations do have differences in experience, we will report it in the results. For quantitative data, the subgroup analysis of different occupations (doctors, nurses and other medical workers) can be performed using a mixed-effect model to reduce the heterogeneity of the study and to distinguish the psychological and infection conditions of different occupations during the outbreak of the epidemic.
Moreover, in order to reduce the heterogeneity across quantitative studies, the subgroup analysis could classify countries by economic income group according to the World Bank list of economies (high income/upper middle income/lower middle income).36 37 We will also try to do subgroup analysis by gender (female/male) and measuring instruments (various scales and equipment) if data allow.
Sensitivity analysis
If the available data allow, we will conduct the sensitivity analyses that exclude studies at high risk of bias in order to determine its impact.
Assessment of reporting biases
The presence of publication bias will be assessed using Egger’s test and funnel plots. P value of <0.10 on the Egger’s test will be considered statistically significant for publication bias.
Assessment of risk and quality
Assessment of risk of bias in included studies
To assess the risk of bias and quality of all articles selected, the methodological quality criteria, Mixed-Methods Appraisal Tool (MMAT), V.2018 will be used.38 This document comprises two parts: checklist (part I) and explanation of the criteria (part II). Each part is divided into five smaller sections according to the category of research designs, and each category includes five items, respectively. All items from the MMAT will be rated as ‘Yes’, ‘No’ or ‘Can’t tell’.39
One reviewer (NX) will apply the MMAT criteria and a second reviewer (TL) will verify the assessments independently. Any disputes will be resolved through discussion or a third reviewer (MH). Regardless of the research quality, all studies will undergo extraction and synthesis where possible.
Assessing confidence in the findings
In order to determine the strength of gathered evidence, the CERQual (Confidence in the Evidence from Reviews of Qualitative Research) approach will be used.40 The CERQual approach is based on four aspects: (1) methodological limitations component, (2) relevance component, (3) coherence component and (4) adequacy component. By synthesising the evaluation results of four parts, the confidence in the evidence for each review finding was assessed as high, moderate, low or very low.
Timeline for review
At the time of submitting this protocol, we have completed the electronic searches and piloted the study selection process. This systematic review is scheduled to finish in July 2021.
Discussion
This protocol was registered and reported according to PRISMA-P guidelines. The PRISMA flow diagram in figure 2 will be used to record the review process in different phases.41
Figure 2.
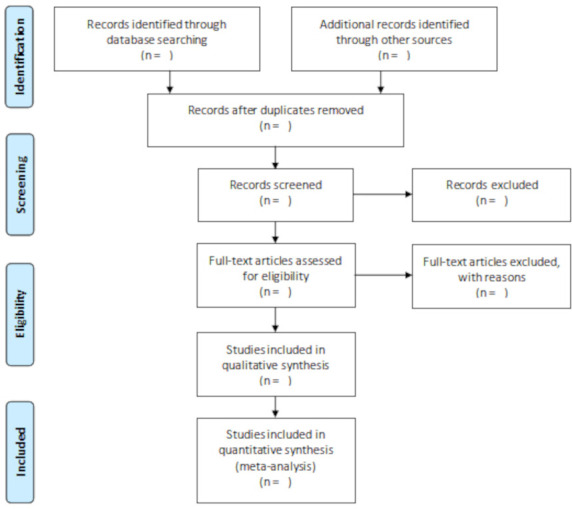
Flow chart diagram that shows the selection of articles for systemic review.
Healthcare providers face a variety of unpredictable challenges in caring for infected patients in the context of coronavirus outbreaks. To our knowledge, there are few systematic reviews that assess the experience of healthcare providers and the impact of coronavirus on them during the outbreak. Comprehensive understanding of what their real experiences and impacts will have a significant meaning when their lives and security are threatened. Meanwhile, this is also stronger evidence in clinical practice of sustained and comprehensive support measures to healthcare providers.
Ethics and dissemination
Ethical assessment is not required due to the nature of the proposed systematic review. Findings of our research will be disseminated at conferences related to this field and through publication in peer-reviewed journals.
Supplementary Material
Footnotes
Contributors: NX and AL conceived and designed the initial study. NX and TL drafted the initial protocol. XL, MH and YS were responsible for the revision of the draft and provided general advice on the protocol. All authors contributed to the development of the selection criteria, the risk of bias assessment strategy and data extraction criteria. AL is the guarantor of the review. All authors read, provided feedback and approved the final protocol before submission of the journal.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
References
- 1.DD R, RJ W, FG H. Clinical virology. 4th edn. Washington: ASM Press, 2016. [Google Scholar]
- 2.Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med Overseas Ed 2020;382:727–33. 10.1056/NEJMoa2001017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Su S, Wong G, Shi W, et al. Epidemiology, genetic recombination, and pathogenesis of coronaviruses. Trends Microbiol 2016;24:490–502. 10.1016/j.tim.2016.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kuiken T, Fouchier RAM, Schutten M, et al. Newly discovered coronavirus as the primary cause of severe acute respiratory syndrome. Lancet 2003;362:263–70. 10.1016/S0140-6736(03)13967-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO . Coronavirus disease (COVID-19) pandemic, 2020. Available: https://www.who.int/emergencies/diseases/novel-coronavirus-2019
- 6.Xiong Y, Peng L. Focusing on health-care providers' experiences in the COVID-19 crisis. Lancet Glob Health 2020;8:e740–1. 10.1016/S2214-109X(20)30214-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chang D, Xu H, Rebaza A, et al. Protecting health-care workers from subclinical coronavirus infection. Lancet Respir Med 2020;8:e13. 10.1016/S2213-2600(20)30066-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO . Coronavirus disease (COVID-19) outbreak: rights, roles and responsibilities of health workers, including key considerations for occupational safety and health, 2020. Available: https://apps.who.int/iris/handle/10665/331510 [Accessed 16 Apr 2020].
- 9.Chou T-L, Ho L-Y, Wang K-Y, et al. Uniformed service nurses' experiences with the severe acute respiratory syndrome outbreak and response in Taiwan. Nurs Clin North Am 2010;45:179–91. 10.1016/j.cnur.2010.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim Y. Nurses' experiences of care for patients with middle East respiratory syndrome-coronavirus in South Korea. Am J Infect Control 2018;46:781–7. 10.1016/j.ajic.2018.01.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Urooj U, Ansari A, Siraj A, et al. Expectations, fears and perceptions of doctors during Covid-19 pandemic. Pak J Med Sci 2020;36:S37–42. 10.12669/pjms.36.COVID19-S4.2643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee JY, Hong JH, Park EY. Beyond the fear: nurses' experiences caring for patients with Middle East respiratory syndrome: A phenomenological study. J Clin Nurs 2020;29:3349–62. 10.1111/jocn.15366 [DOI] [PubMed] [Google Scholar]
- 13.Chen Q, Liang M, Li Y, et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry 2020;7:e15–16. 10.1016/S2215-0366(20)30078-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.HH P, CK C, CP C. Stress and coping behaviors of nurses caring for patients with SARS: an exploratory descriptive study. Journal of Taiwan Nephrology Nursing Association 2003;2:120–8. [Google Scholar]
- 15.Liu Q, Luo D, Haase JE, et al. The experiences of health-care providers during the COVID-19 crisis in China: a qualitative study. Lancet Glob Health 2020;8:e790–8. 10.1016/S2214-109X(20)30204-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mak IWC, Chu CM, Pan PC, et al. Long-Term psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry 2009;31:318–26. 10.1016/j.genhosppsych.2009.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bai Y, Lin C-C, Lin C-Y, et al. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr Serv 2004;55:1055–7. 10.1176/appi.ps.55.9.1055 [DOI] [PubMed] [Google Scholar]
- 18.Park BJ, Peck AJ, Kuehnert MJ, et al. Lack of SARS transmission among healthcare workers, United States. Emerg Infect Dis 2004;10:217–24. 10.3201/eid1002.030793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maunder R, Hunter J, Vincent L, et al. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ 2003;168:1245–51. [PMC free article] [PubMed] [Google Scholar]
- 20.Lu Y-C, Shu B-C, Chang Y-Y, et al. The mental health of hospital workers dealing with severe acute respiratory syndrome. Psychother Psychosom 2006;75:370–5. 10.1159/000095443 [DOI] [PubMed] [Google Scholar]
- 21.Lee AM, Wong JGWS, McAlonan GM, et al. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can J Psychiatry 2007;52:233–40. 10.1177/070674370705200405 [DOI] [PubMed] [Google Scholar]
- 22.Chua SE, Cheung V, Cheung C, et al. Psychological effects of the SARS outbreak in Hong Kong on high-risk health care workers. Can J Psychiatry 2004;49:391–3. 10.1177/070674370404900609 [DOI] [PubMed] [Google Scholar]
- 23.Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open 2020;3:e203976–88. 10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wu Y, Wang J, Luo C, et al. A comparison of burnout frequency among oncology physicians and nurses working on the frontline and usual wards during the COVID-19 epidemic in Wuhan, China. J Pain Symptom Manage 2020;60:e60–5. 10.1016/j.jpainsymman.2020.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Booth CM, Matukas LM, Tomlinson GA, et al. Clinical features and short-term outcomes of 144 patients with SARS in the greater Toronto area. JAMA 2003;289:2801–9. 10.1001/jama.289.21.JOC30885 [DOI] [PubMed] [Google Scholar]
- 26.Kluytmans-van den Bergh MFQ, Buiting AGM, Pas SD, et al. Prevalence and clinical presentation of health care workers with symptoms of coronavirus disease 2019 in 2 Dutch hospitals during an early phase of the pandemic. JAMA Netw Open 2020;3:e209673. 10.1001/jamanetworkopen.2020.9673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med 2020;382:1199–207. 10.1056/NEJMoa2001316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020;323:1061. 10.1001/jama.2020.1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;349:7647:g7647. 10.1136/bmj.g7647 [DOI] [PubMed] [Google Scholar]
- 30.Lizarondo LSC, Carrier J, Godfrey C. Chapter 8: Mixed methods systematic reviews. In: Aromataris E, Munn Z, eds. JBI manual for evidence synthesis, 2020. https://synthesismanual.jbi.global [Google Scholar]
- 31.Innovation VH . Covidence systematic review software. Melbourne: Veritas Health Innovation, 2017. [Google Scholar]
- 32.Browne RH. On the use of a pilot sample for sample size determination. Stat Med 1995;14:1933–40. 10.1002/sim.4780141709 [DOI] [PubMed] [Google Scholar]
- 33.Bishop FL, Holmes MM. Mixed methods in CAM research: a systematic review of studies published in 2012. Evid Based Complement Alternat Med 2013;2013:1–12. 10.1155/2013/187365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Issac H, Moloney C, Taylor M, et al. Mapping of modifiable barriers and facilitators with interdisciplinary chronic obstructive pulmonary disease (COPD) guidelines concordance within hospitals to the theoretical domains framework: a mixed methods systematic review protocol. BMJ Open 2020;10:e036060. 10.1136/bmjopen-2019-036060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gonzalez-Gonzalez AI, Schmucker C, Nothacker J, et al. End-Of-Life care preferences of older patients with multimorbidity: protocol of a mixed-methods systematic review. BMJ Open 2020;10:038682. 10.1136/bmjopen-2020-038682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.World Bank list of economies . World Bank website. Available: databank.worldbank.org
- 37.Schreiber PW, Sax H, Wolfensberger A, et al. The preventable proportion of healthcare-associated infections 2005-2016: systematic review and meta-analysis. Infect Control Hosp Epidemiol 2018;39:1277–95. 10.1017/ice.2018.183 [DOI] [PubMed] [Google Scholar]
- 38.Pluye P, Hong QN. Combining the power of stories and the power of numbers: mixed methods research and mixed studies reviews. Annu Rev Public Health 2014;35:29–45. 10.1146/annurev-publhealth-032013-182440 [DOI] [PubMed] [Google Scholar]
- 39.Pluye P, Hong QN. Combining the power of stories and the power of numbers: mixed methods research and mixed studies reviews. Annu Rev Public Health 2014;35:29–45. 10.1146/annurev-publhealth-032013-182440 [DOI] [PubMed] [Google Scholar]
- 40.GRADE-CERQual Project Group . What is the CERQual approach? 2020. Available: https://www.cerqual.org/what-is-the-grade-cerqual-approach2/
- 41.Hutton B, Catalá-López F, Moher D. [The PRISMA statement extension for systematic reviews incorporating network meta-analysis: PRISMA-NMA]. Med Clin 2016;147:262–6. 10.1016/j.medcle.2016.10.003 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-043686supp001.pdf (133.7KB, pdf)


