Abstract
Objective:
Patients with depression frequently experience persistent residual symptoms even with optimal interventions. These patients often use complementary treatments, including yoga, as a preferred alternative or adjunctive treatment. There is evidence for the benefit of yoga for depression, but this has not been rigorously evaluated, particularly in bipolar depression. We aimed to determine the feasibility and benefit of manualized breathing-focused yoga in comparison to psychoeducation as augmentation to pharmacotherapy for improving residual symptoms of depression in unipolar and bipolar patients.
Methods:
Using a randomized single-blind crossover design, 72 outpatients with unipolar or bipolar depression were augmented with the two 8-week interventions at separate times, as add-ons to current first-line antidepressants and mood stabilizers. The primary outcome measure was the Montgomery-Åsberg Depression Rating Scale (MADRS). Due to the high dropout of participants after crossover at Week 8, analysis focused on between-group comparisons of yoga and psychoeducation during the initial 8 weeks of the study.
Results:
There was a significant decline in depressive symptoms, as measured by the MADRS, following 8 weeks of yoga. However, there was no significant difference in MADRS ratings between intervention groups. Similar improvements in self-rated depressive symptoms and well-being were also observed across time.
Conclusions:
Both yoga and psychoeducation may improve residual symptoms of unipolar and bipolar depression as add-on to medications. In-class group sessions and long study durations may reduce feasibility for this population. Larger trials with parallel group design and shorter duration may be more feasible.
Keywords: breathing-focused yoga, yoga, psychoeducation, depression, unipolar, bipolar, augmentation
Abstract
Objectif:
Les patients souffrant de dépression sont souvent aux prises avec des symptômes résiduels persistants même avec des interventions optimales. Ces patients ont souvent recours à des traitements complémentaires, notamment le yoga, comme solution de rechange préférée ou comme traitement d’appoint. Des données probantes vantent l’avantage du yoga pour la dépression, mais cela n’a pas été rigoureusement évalué, particulièrement pour la dépression bipolaire. Nous visions à déterminer la faisabilité et l’avantage du yoga axé sur la respiration (YAR) d’après un manuel comparativement à la psychoéducation comme augmentation à la pharmacothérapie pour améliorer les symptômes résiduels de la dépression chez les patients unipolaires et bipolaires.
Méthodes:
À l’aide d’une méthode randomisée croisée à simple insu, 72 patients ambulatoires souffrant de dépression unipolaire ou bipolaire ont été augmentés par 2 interventions de 8 semaines à des moments distincts, comme ajouts aux antidépresseurs et psychorégulateurs actuels de première intention. La principale mesure des résultats était l’échelle de dépression de Montgomery-Åsberg (MADRS). En raison du taux élevé d’abandons des participants après le croisement à 8 semaines, l’analyse s’est concentrée sur les comparaisons entre les groupes de yoga et de psychoéducation durant les 8 semaines initiales de l’étude.
Résultats:
Il y avait une baisse significative des symptômes dépressifs, comme ils ont été mesurés par la MADRS, après 8 semaines de yoga. Il n’y avait toutefois aucune différence significative des scores à la MADRS entre les groupes d’intervention. Des améliorations semblables des symptômes dépressifs auto-évalués et du bien-être ont aussi été observées avec le temps.
Conclusions:
Le yoga et la psychoéducation peuvent améliorer les symptômes résiduels de la dépression unipolaire et bipolaire comme ajout aux médications. Les séances de groupe en classe et la longue durée de l’étude peuvent réduire la faisabilité pour cette population. Des essais plus vastes avec une méthode à groupes parallèles et une durée plus courte peuvent être plus faisables.
Introduction
Depression is a common mental disorder, with a lifetime prevalence between 7% and 21%.1 With significant morbidity, it is a leading cause of global disease burden and manifests as unipolar and bipolar forms.2 The societal cost of these conditions combined is estimated to exceed US$200 billion per year, mostly due to reduced worker productivity and increased utilization of health care resources.3
Treatments for unipolar and bipolar depression include a wide range of pharmacological agents, including antidepressants and mood stabilizers,4 as well as psychological treatments (e.g., cognitive behavioral therapy and psychoeducation).5,6 However, the limitations of these first-line treatments are well-recognized as patients often discontinue medications due to adverse side effects.7 Although effective and often preferred by patients, psychotherapy also has its own challenges, including access (e.g., long wait-lists), costs, and a lack of trained professionals.8,9 Dropout rates for both psychotherapy and pharmacotherapy are similar although the reasons for discontinuation may vary between patient groups.10
Even after appropriate first-line treatments, about one third of patients with depression do not remit and report significant subsyndromal symptoms with functional impairment.11,12 It is well-documented that such residual symptoms of depression are associated with an increased likelihood of relapse, poorer quality of life, impaired function, and increased mortality rates.13
Complementary and Alternative Treatments for Unipolar and Bipolar Depression
Complementary and alternative medicine (CAM) treatments include physical therapies (e.g., yoga, acupuncture), nutraceuticals (i.e., nutritional supplements such as vitamins and minerals), and herbal remedies (i.e., plants and plant extracts).14 Depressed patients are often seeking these options, partly due to poor access to conventional treatments, but in addition, they often perceive CAMs as safer, accessible, more tolerable, and easily acceptable compared to pharmaceuticals.15 It has been estimated that 10% to 30% of depressed patients use CAM therapies, often in tandem with conventional treatments and frequently without the knowledge of their physician. This percentage is even higher amongst those with bipolar disorder (up to 50%) and in clinic populations (up to 86%).16
There is preliminary evidence supporting the effectiveness of CAMs, including yoga, for unipolar depression,14 which needs more rigorous evaluations and data. However, information on the benefits of CAMs for bipolar depression is even more sparse.17
Yoga for Depression
Yoga was born out of the centuries-old sociocultural tradition of India but now accepted as a secular practice worldwide.18 Modern Western yoga disciplines usually focus on three main components—asanas (postures), pranayamas (breathing exercises), and dhyana (meditation). Forms of yoga differ in their degree of focus on one or more of these components but usually incorporate all three.
Several randomized controlled trials (RCTs) and open studies have found yoga to be beneficial in treating unipolar depression.19–22 On its own or as an adjunct to medication, yoga has been shown to alleviate symptoms of mild to moderate depression.23 Preliminary evidence suggests that it may even benefit more severe depression and even alleviate suicidal ideation.24 It is noted to be well tolerated, with only mild and infrequent adverse events linked to physical fitness being reported,24 and evidence for sustained benefit 3 to 6 months postintervention.25 In contrast, the role of yoga in the treatment of bipolar depression is significantly understudied. Preliminary observations suggest that yoga improves psychological, physical, and cognitive function warranting further investigation.26,27
Although early results are promising, their reliability and generalizability are limited by the paucity of studies and methodological constraints, including small sample sizes, variations in clinical measurements, blinding methods, and patient selection.20,28 Moreover, there are considerable differences in the forms of yoga employed, with many yoga publications not including the key components of yoga in the intervention.29 This is an important limitation, given the distinct physiological and psychological impacts and outcomes noted among types of yoga practices.30 As well, most RCTs did not employ comparators or assessed yoga against less rigorous control conditions (e.g., no treatment, wait-list). There are few well conducted comparative studies versus established treatments.20
The Mechanisms Mediating the Antidepressant Effects of Yoga
Although the mechanisms underlying therapeutic benefit of yoga have not been fully elucidated, it has been suggested that its benefit may be due to normalization of hypothalamic pituitary adrenal axis activity and autonomic nervous system functioning after stress reactivity.31,32 The component of breath control (referred to as pranamaya) is thought to play a key role in such normalization after stress response. It has been shown that several neuroendocrine and autonomic changes associated with depression, including hypercortisolemia, cytokine expression, and heart rate variability, among others, have been shown to normalize with yoga practice, specifically with breath control.33 Neurophysiological models propose that yogic breathing may have a positive impact on regulation of emotion and stress responsivity through activation of vagal afferents to autonomic, neuroendocrine, and limbic circuits.32
Rationale for This Study
Medication treatments for unipolar and bipolar depression have their own limitations, including adverse effects and poor adherence,29 while psychological treatments are costly and often not accessible, thus increasing the risk of relapse and negative long-term outcomes. As such, new, effective, accessible, and patient-preferred treatment options would greatly enhance current treatments for depression.
Given the popularity and frequent use of CAM therapies by patients with depression and anxiety,14 there is a need to systematically evaluate their benefits in this population. Yoga is widely seen as an accessible, adaptable, cost-effective, and noninvasive intervention that also improves physical fitness. All these qualities likely increase patient preference and adherence.
Although there is a growing body of literature on the utility of yoga in depression, variabilities in study design, methodology, and yoga practice protocols limit generalizability in clinical settings. This study addressed several such gaps by evaluating the feasibility and potential benefit of a manualized yoga protocol in unipolar and bipolar depressed patients with significant residual symptoms. Yoga was compared to another established intervention for depression, psychoeducation, and both were evaluated as augmentation in patients who showed only partial response to medication.
Psychoeducation was chosen as the comparator for its benefits in acute unipolar depression,34 as well as its utility in maintenance treatment and prophylaxis of bipolar depression.35 Furthermore, it can be manualized and structured for the same duration and frequency of delivery as yoga. Similar to yoga, it is a nonpharmacological intervention with at least one published comparative study of the two interventions in unipolar depression.36
The aim of this study was to determine the feasibility and identify any signals of benefit of a manualized yoga protocol in participants with unipolar and bipolar depression. The primary hypothesis was that while both interventions will improve residual symptoms of depression (measured by Montgomery-Åsberg Depression Rating Scale [MADRS]), yoga would be associated with a significantly greater improvement, including among secondary measures of well-being, given its potentially beneficial effect on psychological and physical functioning.22
Methods
Study Design
The investigation was a 16-week, single-blind, randomized, controlled, rater-blinded, crossover study conducted after approval by the institutional ethics board and in a tertiary care teaching hospital in the outpatient setting. Patients were randomized to receive 8 weeks of yoga, followed by 8 weeks of psychoeducation, or 8 weeks of psychoeducation, followed by yoga for equal duration. Treatment sessions were conducted twice a week for 1.5 hours per session.
While the study was initially designed and implemented as noted above, there were high dropouts after crossover at 8 weeks, that were often attributed to the length of the RCT. Thus, it was decided that a direct between-group comparison would be conducted between those who received yoga versus psychoeducation for 8 weeks.
Study Treatments
Yoga
The yoga protocol was developed specifically for this study and in consultation with a Centre of Excellence for Yoga at the National Institute of Mental Health and Neurosciences (NIMHANS) in Bangalore, India. Based on published evidence, the manualized yoga practice focused on cyclical breathing and breathe control (pranayamas) as the key component of the yoga protocol. These breathing practices included Ujjayi and Kapalabhati techniques. Cyclical breathing refers to rapid cycle breathing where individuals begin by breathing 40 to 60 breaths per minute, followed by 60 to 80 breaths per minute, and finish with 80 to 100 breaths per minute. This is repeated 3 times to complete 1 round. A full cyclical breathing program consists of 5 rounds. In the study protocol, participants gradually worked their way up to 5 rounds.
Other components of the yoga intervention included postures and guided meditation that allowed some flexibility for participants with different ability levels to acquire the yoga technique. The yoga protocol was standardized for subjects to learn the practice in the same regulated sequence and pace to maintain fidelity of practice and taught by an instructor trained in Bangalore, India. When necessary, minor modifications were allowed to accommodate varying physical abilities. Treatment sessions were conducted twice a week for 1.5 hours per session. Participants were also encouraged to practice at home and to document it.
Psychoeducation
The psychoeducation protocol for unipolar and bipolar depression was adopted from a manualized protocol previously developed and validated at the institution of the current study. It incorporated education on symptoms and treatments for unipolar and bipolar depression, interpersonal communication, stress and problem management, coping strategies, community resources, dealing with the medical and legal systems, and relapse prevention. The weekly sequence and delivery of content was standardized, with some flexibility allowed for different rates of learning and discussion. It was taught by a trained clinician who also led the clinical group that developed the psychoeducation protocol. Treatment sessions were conducted twice a week for 1.5 hours per session.
During the study, psychotropic medications were permitted; however, only patients who were on stable doses for at least 2 weeks prior to randomization were included and no increases in psychotropic medications were allowed. Concomitant medications for anxiety and insomnia (e.g., low-dose lorazepam and zopiclone) were allowed on an as-needed basis, except on the days of intervention and assessments.
Subjects
The study was conducted between 2007 and 2011 and registered at ClinicalTrials.gov (Identifier: NCT00482482). Following ethics approval from the Centre for Addiction and Mental Health (CAMH; Toronto, Canada; #308/2006) and written informed consent, patients (age range 18 to 70 years) who met DSM-IV criteria for major depression, dysthymia, or bipolar disorder37 and scoring ≥12 and ≤24 on the MADRS38 were recruited at CAMH. The diagnosis was confirmed and comorbidities excluded by a standardized, semi-structured interview, the Mini International Neuropsychiatric Interview.39
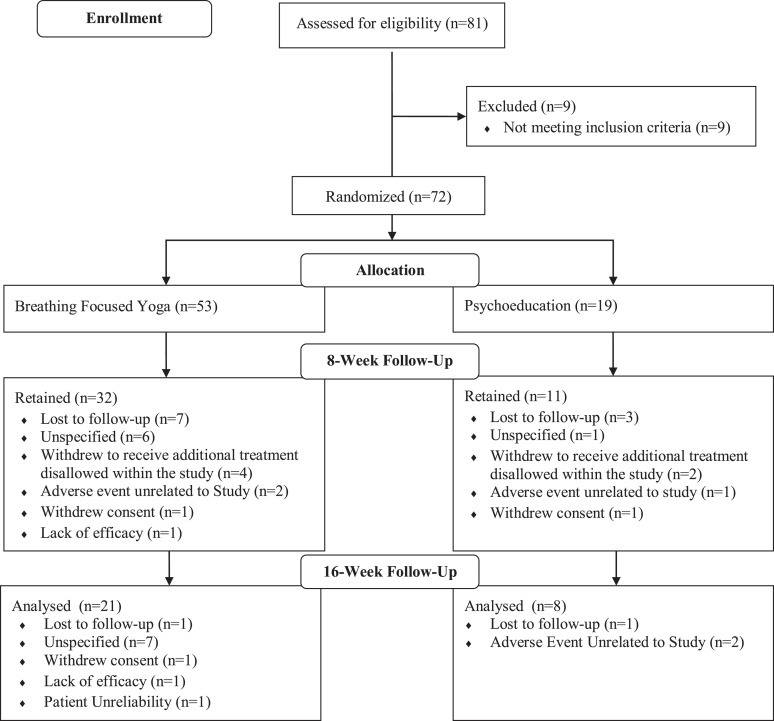
Exclusion criteria included current manic/hypomanic/mixed state, history of nonmood psychosis (e.g., schizophrenia, schizoaffective disorders), substance dependence within the previous 6 months, initiation of structured psychotherapy within the previous 3 months, existing yoga practice (see Note 1), risk of suicidality, and presence of medical conditions or physical limitations that would affect ability to participate in the study. It was initially proposed that participants who missed ≥ 6 yoga sessions or ≥ 3 psychoeducation sessions would be withdrawn from the study by researchers, though this did not apply to any study participants. Participants made the choice to withdraw for other reasons as outlined in Figure 1.
Figure 1.
Consolidated Standards of Reporting Trials diagram.
As this was a feasibility and signal detecting trial, we did not determine sample size a priori but tried to recruit as many participants as possible. In light of the evidence for patient preference of yoga, the benefits associated with yoga practice, and to facilitate recruitment, participants were randomly assigned by a blinded investigator to receive yoga first (N = 53) or psychoeducation first (N = 19), using a 2:1 randomization method, which was accomplished via a computerized number generator.
Efficacy and Safety Evaluation
Patients were evaluated at screening, baseline, Week 8 (end of first intervention), and Week 16 (end of second intervention). Clinician-rated measures included the MADRS,38 the Hamilton Depression Rating Scale (HAMD),40 and the Clinical Global Impression (CGI) Scale.41 Patient-rated measures included the Beck Depression Inventory (BDI),42 the Perceived Stress Scale (PSS),43 and the Quality of Life Satisfaction and Enjoyment Scale (QLESQ).44
For the primary efficacy variable, the MADRS, response was defined as a ≥50% decrease in score from baseline. Remission was defined as a score ≤10.
Statistical Analysis
We conducted an intent-to-treat (ITT) analysis assessing mean changes (MC) from baseline to 8 weeks for each intervention and mean differences (MD) between yoga and psychoeducation on all primary (MADRS) and secondary outcome measures (HAMD, CGI, BDI, QLESQ, PSS). To complete the ITT analysis, we carried forward the last observation for participants who withdrew. A separate analysis for completers of the first trial arm was also conducted. MC between time points were determined using paired t tests. MD between interventions were assessed using analysis of covariance with Bonferroni adjusted post hoc comparisons while controlling for baseline. Confidence intervals (CI) for each estimate are included in Table 1. Generally, criteria for linearity, homogeneity of regression slopes, normality, homoscedasticity, and equality of variances were met. There were a few minor deviations in normality for MADRS, CGI, and BDI scales, though both statistical tests used in the present analysis are considered robust to such deviations and thus no data modifications were made. In an exploratory analysis, these tests were also conducted for all participants and completers of the second arm of the trial and their results can be found in the Appendix (Table A1).
Table 1.
Mean Change from Baseline to 8 Weeks and Mean Difference between Yoga and Psychoeducation at 8 Weeks for All Participants and Completers of the First Trial Arm.
| Outcome | Mean Change (95% CI) from Baseline to 8 Weeks, Yoga First | Mean Change (95% CI) from Baseline to 8 Weeks, Psychoeducation First | Mean Difference (95% CI) between Yoga vs. Psychoeducation at 8 Weeks | |||
|---|---|---|---|---|---|---|
| ITTa | Completers | ITTa | Completers | ITTa | Completers | |
| MADRS | −3.11 (−5.19 to −1.04)*** | −4.15 (−6.86 to −1.44)*** | −2.25 (−5.24 to 0.74) | −3.60 (−8.50 to 1.30) | −0.65 (−4.42 to 3.11) | −1.26 (−6.75 to 4.23) |
| HAMD | −2.00 (−4.82 to 0.82) | −2.67 (−6.45 to 1.11) | −0.75 (−3.80 to 2.30) | −1.2 (−6.45 to 4.05) | −0.65 (−5.47 to 4.17) | −2.27 (−9.24 to 4.71) |
| CGI | −0.46 (−0.75 to −0.16)*** | −0.61 (−0.99 to −0.22)*** | −0.37 (−0.80 to 0.05) | −0.60 (−1.29 to 0.09) | −0.11 (−0.66 to 0.43) | −0.12 (−0.94 to 0.71) |
| BDI | −6.83 (−8.87 to −4.79)*** | −8.30 (−10.54 to −6.07)*** | −1.79 (−4.20 to 0.62) | −2.50 (−5.94 to 0.94) | −5.18 (−8.90 to −1.46)*** | −6.36 (−10.82 to −1.91)*** |
| QLESQ | 4.67 (2.30 to 7.05)*** | 5.53 (2.68 to 8.38)*** | 1.66 (−1.99 to 5.33) | 2.5 (−3.30 to 8.30) | 2.79 (−1.57 to 7.15) | 3.71 (−2.00 to 9.44) |
| PSS | −2.37 (−4.07 to −0.66)** | −2.73 (−4.80 to −0.65)** | 0.67 (−1.45 to 2.79) | 1.00 (−2.40 to 4.40) | −2.87 (−5.77 to 0.03) | −4.46 (−8.08 to −0.84)a |
Note. MADRS = Montgomery-Åsberg Depression Rating Scale; HAMD = Hamilton Depression Rating Scale; CGI = Clinical Global Impression Scale; BDI = Beck Depression Inventory; PSS = Perceived Stress Scale; QLESQ = Quality of Life Satisfaction and Enjoyment Scale; ITT = intent-to-treat.
a Last (i.e., baseline) observation carried forward.
**P < 0.05.***P < 0.01.
Results
Patient Characteristics
Seventy-two participants (age range 18 to 70 years) were enrolled in the study (bipolar, N = 17; unipolar, N = 55). Nine participants were considered screen failures, and 29 participants withdrew or were lost to follow up for several reasons during the first 8 weeks of the study (see Figure 1). Demographic information and clinical features are presented in Table 2. The flow of participants through the study is presented in Figure 1.
Table 2.
Demographics and Medications Taken by Participants in First Trial Arm.
| Demographics | Participants Receiving Yoga First | Participants Receiving Psychoeducation First | All Participants |
|---|---|---|---|
| Mean age (SD) | 39.36 (11.69) | 40.58 (12.72) | 39.68 (11.89) |
| Gender N (%) | |||
| Female | 43 (81.10) | 14 (73.70) | 57 (79.20) |
| Male | 10 (18.90) | 5 (26.30) | 15 (20.80) |
| Mood diagnosis N (%) | |||
| Unipolar | 44 (83.0) | 11 (57.90) | 55 (76.40) |
| Bipolar | 9 (17.0) | 8 (42.10) | 17 (23.60) |
| Mean baseline MADRS score (SD) | 19.18 (5.91) | 18.42 (5.66) | 18.97 (5.81) |
| Mean duration of illness years (SD) | 9.82 (9.12) | 12.05 (9.80) | 10.41 (9.29) |
| Comorbid diagnosis N (%) | 26 (49.1) | 10 (52.60) | 36 (50.0) |
| Family history of psychiatric disorder N (%) | 47 (88.70) | 13 (68.40) | 60 (83.30) |
| Receiving psychotropic medication N (%) | 52 (98.1) | 18 (94.70) | 70 (97.20) |
| Marital status N (%) | |||
| Married | 6 (11.30) | 3 (15.80) | 9 (12.50) |
| Single | 16 (30.20) | 7 (36.80) | 23 (31.90) |
| In long-term relationship | 10 (18.90) | 4 (21.10) | 14 (19.40) |
| Divorced | 10 (18.90) | 2 (10.50) | 12 (16.70) |
| Widowed | 2 (3.80) | 1 (5.30) | 3 (4.20) |
| Employment status N (%) | |||
| Full-time | 5 (9.40) | 2 (10.50) | 7 (9.70) |
| Part-time | 13 (24.50) | 1 (5.30) | 14 (19.40) |
| Not currently working | 29 (54.70) | 13 (68.40) | 42 (58.30) |
| Student | 2 (3.80) | 1 (5.30) | 3 (4.20) |
| Education level N (%) | |||
| High school | 4 (7.60) | 2 (10.50) | 6 (8.30) |
| College | 6 (11.30) | 6 (31.60) | 12 (16.70) |
| University | 37 (69.80) | 7 (36.80) | 44 (61.10) |
| Graduate studies | 5 (9.40) | 4 (21.10) | 9 (12.50) |
| Medication type N (%) | |||
| SSRI | 23 (48.9) | 7 (38.9) | 30 (46.2) |
| SNRI | 23 (48.9) | 7 (38.9) | 30 (46.2) |
| Tricyclic | 2 (4.3) | 2 (11.1) | 4 (6.2) |
| Atypical antipsyhcotic | 11 (23.4) | 8 (44.4) | 19 (29.2) |
| Mood stabilizer | 9 (19.1) | 6 (33.3) | 15 (23.1) |
| Benzodiazepine | 13 (27.7) | 4 (22.2) | 17 (26.2) |
| Other (stimulant, sleep aid) | 6 (12.8) | 4 (22.2) | 10 (15.4) |
Note. N = 72.
The majority of participants (90.3%) were receiving psychotropic medication for the treatment of a mood disorder. The mean number of medications taken by participants was 2.04 (SD = 1.28) and frequencies of medication types are presented in Table 2.
Participant attendance was relatively similar in both arms for yoga and psychoeducation, with an average of 79.04% to 81.25% of classes attended. Approximately 40% of participants dropped out of the study between baseline and Week 8.
Three participants did not incorporate yoga into their daily routine at home, while the remainder reportedly practiced at least some components of the yoga protocol off-site. Finally, an insufficient number of participants with bipolar disorder completed the study to allow for a meaningful statistical analysis (N = 5). They are included in the analysis presented here, although, it is worth noting that removing these participants from the analysis did not change the results. Mean scores on clinician- and patient-rated measures for all patients and completers of each trial arm can be found in Table 3.
Table 3.
Mean Scores for Clinician- and Patient-rated Measures across Time for Each Trial Arm.
| Outcome | Mean Score (SD), Yoga First | Mean score (SD), Psychoeducation First | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline N = 53 |
8 Weeks ITTa |
N = 32 | 16 Weeks ITTa |
N = 21 | Baseline N = 19 |
8 Weeks ITTa |
N = 11 | 16 Weeks ITTa |
N = 9 | |
| MADRS | 20.18 (5.55) | 17.07 (8.02) | 16.27 (8.36) | 17.16 (8.98) | 16.27 (9.11) | 19.38 (5.66) | 17.13 (6.13) | 19.00 (6.68) | 15.81 (6.62) | 14.14 (6.96) |
| HAMD | 21.77 (7.28) | 19.77 (9.96) | 18.94 (10.62) | 19.73 (10.89) | 17.81 (10.02) | 20.06 (6.84) | 19.31 (7.43) | 22.00 (7.56) | 16.63 (7.29) | 15.14 (7.97) |
| CGI | 3.64 (.53) | 3.18 (1.08) | 3.06 (1.20) | 3.14 (1.21) | 3.00 (1.27) | 3.75 (.68) | 3.38 (.72) | 3.50 (.85) | 3.12 (.96) | 2.71 (1.11) |
| BDI | 25.59 (11.39) | 18.76 (12.14) | 17.39 (11.62) | 20.37 (12.91) | 18.00 (11.75) | 27.36 (10.55) | 25.57 (11.18) | 28.50 (9.71) | 22.50 (11.00) | 20.14 (8.78) |
| QLESQ | 40.37 (8.87) | 45.04 (10.56) | 45.71 (10.02) | 44.61 (11.63) | 45.64 (10.57) | 41.67 (11.40) | 43.33 (11.13) | 40.20 (9.63) | 44.53 (13.60) | 46.43 (14.85) |
| PSS | 35.17 (8.92) | 32.80 (8.74) | 32.27 (7.77) | 32.17 (9.30) | 30.68 (7.77) | 34.33 (6.87) | 35.00 (6.68) | 38.10 (4.22) | 32.07 (7.21) | 31.14 (7.20) |
Note. MADRS = Montgomery-Åsberg Depression Rating Scale; HAMD = Hamilton Depression Rating Scale; CGI = Clinical Global Impression Scale; BDI = Beck Depression Inventory; PSS = Perceived Stress Scale; QLESQ = Quality of Life Satisfaction and Enjoyment Scale; ITT = intent-to-treat.
aLast (i.e., baseline) observation carried forward.
Response and Remission
At 8 weeks, 37% of participants were considered to be responders as defined by our protocol (≥50% decrease in MADRS score), while 27.9% of participants were in remission (MADRS score of ≤10).
Primary Outcome
As shown in Table 1, the ITT analysis revealed a significant decrease in MADRS-rated depressive symptoms after yoga (MC = −3.11, CI = −5.19 to −1.04), but not after psychoeducation (MC = −2.25, CI = −5.24 to 0.74). However, there was no significant difference in MADRS scores between yoga and psychoeducation at Week 8 (MD = −0.65, CI = −4.42 to 3.11).
Secondary Outcomes
Across time and between interventions, there were no significant differences in HAMD ratings of depressive symptoms (yoga first, MC = −2.00, CI = −4.82 to 0.82; psychoeducation first, MC = −0.75, CI = −3.80 to 2.30; MD = −0.65, CI = −5.47 to 4.17). In contrast, following yoga, illness severity (CGI, MC = −0.46, CI = −0.75 to −0.16), self-rated depressive symptoms (BDI, MC = −6.83, CI = −8.87 to −4.79), and perceived stress (PSS, MC = −2.37, CI = −4.07 to −0.66) significantly decreased from baseline, while quality of life significantly improved (QLESQ, MC = 4.67, CI = 2.30 to 7.05). There were no meaningful changes in these measures following psychoeducation (CGI, MC = −0.37, CI = −0.80 to 0.05; BDI, MC = −1.79, CI = −4.20 to 0.62; PSS, MC = 0.67, CI = −1.45 to 2.79; QLESQ, MC = 1.66, CI = −1.99 to 5.33). Interestingly, compared to psychoeducation, participants in the yoga group reported significantly lower BDI scores (MD = −5.18, CI = −8.90 to −1.46). However, there were no between-group differences for CGI (MD = −0.11, CI = −0.66 to 0.43), PSS (MD = −2.87, CI = −5.77 to 0.03), and QLESQ (MD = 2.79, CI = −1.57 to 7.15). See Table 1 for the complete analysis.
Safety and Tolerability
A small subgroup of subjects in the first (N = 5) and second trial arm (N = 2) reported side effects of sweating, shortness of breath, and/or hot flushes and all were mild and temporary, occurring after the cyclical breathing. Subjects opted to continue the practice, and there were no dropouts in the yoga group due to adverse effects. None of the subjects reported adverse effects with psychoeducation.
Discussion
This crossover RCT evaluated the benefits of augmentation of medications with yoga or psychoeducation in depressed patients with mild to moderate residual symptoms of depression. We did not find a significant difference in MADRS scores between interventions at 8 weeks posttreatment, which is contrary to the initial hypothesis. There were, however, positive changes in well-being over time for both interventions, as determined by other clinician- and self-rated measures. This was especially true for yoga. Indeed, there were between-group differences for BDI scores—patients rated a much higher magnitude of perceived improvement in symptoms following yoga compared to psychoeducation. While it may seem contradictory that self-reported improvement would be higher than that measured by clinicians, one possible explanation for this finding is that yoga involves more “active” components (i.e., poses, meditation) that encourage patient engagement and generally require greater physical and mental effort compared to psychoeducation. The effort justification paradigm proposes that individuals tend to attribute greater value to an outcome that requires more effort to achieve45; this may have influenced participants’ perceptions of the efficacy of yoga.
These findings do not suggest that yoga is superior to psychoeducation, but they do provide support for its benefit in improving residual symptoms of depression, along with other proven interventions including psychoeducation.34,35 In light of the overall improvement in symptoms and function, it is suggested that yoga may be at least as effective as psychoeducation and as adjunctive to medications for mild to moderate depression. In a similar investigation comparing adjunctive yoga and health education in depressed patients, yoga was found to be superior after a 6-month follow-up, but not in the active treatment phase,25 suggesting duration of intervention may influence the magnitude of benefits of the two interventions.
There are several limitations to this investigation. First, it employed a crossover design in which patients served as their own controls with maximum benefits obtained if they completed both arms of the study. This design is somewhat inflexible and presented unique recruitment and attendance challenges for this patient population, which likely contributed to the high dropout rate. Second, as the design of this study was single-blind (with blinding of the raters), it is conceivable that participant bias could have influenced the measurements. Third, there was substantial variability in depression severity across the sample, with baseline severity ranging from mild to moderate. The fact that the majority of participants were in the mild to mild-moderate range at baseline may have also produced a floor effect such that, if participants responded differentially to yoga versus psychoeducation, the difference between pre- and posttreatment scores may not have been large enough to detect via statistical testing. Fourth, the relatively modest sample size limits generalizability, decreases power, and the ability to detect meaningful differences between groups. Finally, while there are past reports of mild and transient side effects with cyclical breathing, only 10% reported such experiences in this study. They were rated as not troublesome, and there were no dropouts due to these adverse effects.
There were several feasibility issues that were encountered and not anticipated. These occurred due to the novel nature of the intervention and lack of clinical trial experience with its use and evaluation. In hindsight, it was realized that the crossover design may have several disadvantages, including carryover effects and cyclical intake for groups, adding to participant time and commitment to the study. The high dropout rate is likely the result of the long duration of study with multiple interventions inherent to crossover designs. It has been observed that dropout rates often increase with number of treatment sessions in nonmedication intervention trials.46 Thus, a parallel group design of shorter duration may have been a more feasible option in spite of larger number of subjects needed for meaningful comparisons of interventions.
Conclusions
Findings suggest that yoga, similar to psychoeducation, may be helpful as an adjunctive intervention in reducing symptoms and improving function in depression of mild to moderate severity. The type of design and long duration of study likely contributed to high dropout rates and call into question the feasibility of a crossover design for this type of treatment and population. However, in spite of its shortcomings, the data from the investigation provide evidence supporting yoga as a viable adjunctive treatment for depression.
Acknowledgments
We wish to acknowledge the contribution of Jonathan Jin in the drafting and editing of the manuscript and Dr. Nisha Ravindran for assessment and recruitment of patients.
Appendix
Table A1.
Mean Change from 8 to 16 Weeks and Mean Difference between Yoga and Psychoeducation at 16 weeks for All Participants and Completers of the Second Trial Arm.
| Outcome | Mean Change (95% CI) from 8 to 16 Weeks, Yoga First | Mean Change (95% CI) from 8 to 16 Weeks, Psychoeducation First | Mean Difference (95% CI) between Yoga vs. Psychoeducation at 16 Weeks | |||
|---|---|---|---|---|---|---|
| ITTa | Completers | ITTa | Completers | ITTa | Completers | |
| MADRS | 0.09 (−2.31 to 2.49) | 0.18 (−4.82 to 5.19) | −1.31 (−4.18 to 1.55) | −3.00 (–10.55 to 4.55) | −1.38 (−5.41 to 2.65) | −2.22 (−10.11 to 5.66) |
| HAMD | −0.04 (−2.74 to 2.65) | −0.09 (−5.72 to 5.54) | −2.68 (−7.60 to 2.22) | −6.14 (−18.82 to 6.53) | −2.87 (−7.67 to 2.04) | −2.23 (−11.18 to 6.53) |
| CGI | −0.04 (−0.38 to 0.29) | −0.09 (−0.78 to 0.61) | −0.26 (−0.66 to 0.16) | −0.57 (−1.62 to 0.48) | −0.14 (−0.70 to 0.43) | −0.31 (−1.4 to 0.81) |
| BDI | 1.61 (−0.85 to 4.07) | 3.00 (−1.68 to 7.68) | −3.07 (−6.41 to 0.27) | −6.14 (−12.71 to 0.43) | −3.71 (−8.34 to 0.92) | −5.26 (−14.94 to 4.42) |
| QLESQ | −0.43 (−0.289 to 2.03) | −0.80 (−5.56 to 3.96) | 1.20 (−2.54 to 4.94) | 2.57 (−6.79 to 11.94) | 1.45 (−.3.12 to 6.02) | 2.52 (−6.89 to 11.92) |
| PSS | −0.63 (−2.19 to 0.92) | −1.18 (−4.18 to 1.81) | −2.93 (−5.44 to −0.43) | −6.29 (−10.74 to −1.83) | −2.07 (−5.00 to 0.86) | −3.57 (−9.56 to 2.43) |
Note. MADRS = Montgomery-Åsberg Depression Rating Scale; HAMD = Hamilton Depression Rating Scale; CGI = Clinical Global Impression Scale; BDI = Beck Depression Inventory; PSS = Perceived Stress Scale; QLESQ = Quality of Life Satisfaction and Enjoyment Scale; ITT = intent-to-treat.
a Last (i.e., baseline) observation carried forward.
Note
Participants were asked about their current yoga practice, if any, and if it included specific breath-focused practices as outlined in protocol manual, they would be excluded from the study. However, no participants reported regular yoga practices that involved specific breath-focused element, and therefore, no participants were excluded for this reason.
Authors’ Note: Data cannot be accessed due to participant privacy agreements.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Partial funding toward the cost of yoga therapy was provided by the family of a patient (Mr. AW) with depression who benefited from participation but wished to remain anonymous.
ORCID iD: Arun V. Ravindran, MB, PhD, FRCP(C), FRCPsych  https://orcid.org/0000-0002-1655-2753
https://orcid.org/0000-0002-1655-2753
References
- 1. Bromet E, Andrade LH, Hwang I, et al. Cross-national epidemiology of DSM-IV major depressive episode. BMC Med. 2011;9(1):90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ferrari AJ, Charlson FJ, Norman RE, et al. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Med. 2013;10(11):e1001547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Greenberg PE, Fournier AA, Sisitsky T, et al. The economic burden of adults with major depressive disorder in the United States (2005 and 2010). J Clin Psychiatry. 2015;76(2):155–162. [DOI] [PubMed] [Google Scholar]
- 4. Kennedy SH, Lam RW, McIntyre RS, et al. Canadian network for mood and anxiety treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: section 3. pharmacological treatments. Can J Psychiatry. 2016;61(9):540–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kolovos S, Kleiboer A, Cuijpers P. Effect of psychotherapy for depression on quality of life: meta-analysis. Br J Psychiatry. 2016;209(6):460–468. [DOI] [PubMed] [Google Scholar]
- 6. Parikh SV, Quilty LC, Ravitz P, et al. Canadian network for mood and anxiety treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: section 2. psychological treatments. Can J Psychiatry. 2016;61(9):524–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Maund E, Dewar-Haggart R, Williams S, et al. Barriers and facilitators to discontinuing antidepressant use: a systematic review and thematic synthesis. J Affect Disord. 2019;245:38–62. [DOI] [PubMed] [Google Scholar]
- 8. Kazdin AE, Rabbitt SM. Novel models for delivering mental health services and reducing the burdens of mental illness. Clin Psychol Sci. 2013;1(2):170–191. [Google Scholar]
- 9. Mira A, Soler C, Alda M, et al. Exploring the relationship between the acceptability of an internet-based intervention for depression in primary care and clinical outcomes: secondary analysis of a randomized controlled trial. Front Psychiatry. 2019;10:325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Swift JK, Greenberg RP, Tompkins KA, Susannah RP. Treatment refusal and premature termination in psychotherapy, pharmacotherapy, and their combination: a meta-analysis of head-to-head comparisons. Psychotherapy. 2017;54(1):47. [DOI] [PubMed] [Google Scholar]
- 11. De Carlo V, Calati R, Serretti A. Socio-demographic and clinical predictors of non-response/non-remission in treatment resistant depressed patients: a systematic review. Psychiatry Res. 2016;240:421–430. [DOI] [PubMed] [Google Scholar]
- 12. Lex H, Ginsburg Y, Sitzmann AF, et al. Quality of life across domains among individuals with treatment-resistant depression. J Affect Disord. 2019;243:401–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Johnston KM, Powell LC, Anderson IM, et al. The burden of treatment-resistant depression: a systematic review of the economic and quality of life literature. J Affect Disord. 2019;242:195–210. [DOI] [PubMed] [Google Scholar]
- 14. Ravindran AV, Balneaves LG, Faulkner G, et al. Canadian network for mood and anxiety treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: section 5. complementary and alternative medicine treatments. Focus. 2018;16(1):85–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ravindran AV, da Silva TL. Complementary and alternative therapies as add-on to pharmacotherapy for mood and anxiety disorders: a systematic review. J Affect Disord. 2013;150(3):707–719. [DOI] [PubMed] [Google Scholar]
- 16. Solomon D, Adams J. The use of complementary and alternative medicine in adults with depressive disorders. a critical integrative review. J Affect Disord. 2015;179:101–113. [DOI] [PubMed] [Google Scholar]
- 17. Andreescu C, Mulsant BH, Emanuel JE. Complementary and alternative medicine in the treatment of bipolar disorder—a review of the evidence. J Affect Disord. 2008;110(1-2):16–26. [DOI] [PubMed] [Google Scholar]
- 18. Brown RP, Gerbarg PL. Sudarshan Kriya Yogic breathing in the treatment of stress, anxiety, and depression. part II—clinical applications and guidelines. J Altern Complement Med. 2005;11(2):711–717. [DOI] [PubMed] [Google Scholar]
- 19. Bridges L, Sharma M. The efficacy of yoga as a form of treatment for depression. J Evid Based Complement Alternat Med. 2017;22(4):1017–1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cramer H, Anheyer D, Lauche R, et al. A systematic review of yoga for major depressive disorder. J Affect Disord. 2017;213:70–77. [DOI] [PubMed] [Google Scholar]
- 21. da Silva TL, Ravindran LN, Ravindran AV. Yoga in the treatment of mood and anxiety disorders: a review. Asian J Psychiatr. 2009;2(1):6–16. [DOI] [PubMed] [Google Scholar]
- 22. Meister KK, Juckel G. A systematic review of mechanisms of change in body-oriented yoga in major depressive disorders. Pharmacopsychiatry. 2017;51(3):73–81. [DOI] [PubMed] [Google Scholar]
- 23. Prathikanti S, Rivera R, Cochran A, Jose Gabriel T, Nima F, Eva W. Treating major depression with yoga: a prospective, randomized, controlled pilot trial. PLoS One. 2017;12(3):1–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Nyer M, Gerbarg PL, Silveri MM, et al. A randomized controlled dosing study of Iyengar yoga and coherent breathing for the treatment of major depressive disorder: impact on suicidal ideation and safety findings. Complement Ther Med. 2018;37(1):136–142. [DOI] [PubMed] [Google Scholar]
- 25. Uebelacker LA, Tremont G, Gilette LT, et al. Adjunctive yoga v. health education for persistent major depression: a randomized controlled trial. Psychol Med. 2017;47(12):2130–2142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Uebelacker LA, Weinstock LM, Kraines MA. Self-reported benefits and risks of yoga in individuals with bipolar disorder. J Psychiatr Pract. 2014;20(5):345–352. [DOI] [PubMed] [Google Scholar]
- 27. Weinstock LM, Broughton MK, Tezanos KM, et al. Adjunctive yoga versus bibliotherapy for bipolar depression: a pilot randomized controlled trial. Mental Health Physical Activity. 2016;11:67–73. [Google Scholar]
- 28. Pilkington K, Kirkwood G, Rampes H, et al. Yoga for depression: the research evidence. J Affect Disord, 2005;89(1-3):13–24. [DOI] [PubMed] [Google Scholar]
- 29. Vollbehr NK, Bartels-Velthuis AA, Nauta MH, et al. Hatha yoga for acute, chronic and/or treatment-resistant mood and anxiety disorders: a systematic review and meta-analysis. PLoS One. 2018;13(10):e0204925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Schmalzl L, Powers C, Zanesco AP, et al. The effect of movement-focused and breath-focused yoga practice on stress parameters and sustained attention: a randomized controlled pilot study. Conscious Cogn. 2018;65:109–125. [DOI] [PubMed] [Google Scholar]
- 31. Cahn BR, Goodman MS, Peterson CT, Raj M, Paul JM. Yoga, meditation and mind-body health: Increased BDNF, cortisol awakening response, and altered inflammatory marker expression after a 3-month yoga and meditation retreat. Front Hum Neurosci. 2017;11:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Streeter CC, Gerbarg PL, Saper RB, Ciraulo DA, Brown RP, et al. Effects of yoga on the autonomic nervous system, gamma-aminobutyric-acid, and allostatis in epilepsy, depression, and post-traumatic stress disorder. Med Hypotheses. 2012;78(5):571–579. [DOI] [PubMed] [Google Scholar]
- 33. Pascoe MC, Bauer IE. A systematic review of randomised control trials on the effects of yoga on stress measures and mood. J Psychiatr Res. 2015;68(5):270–282. [DOI] [PubMed] [Google Scholar]
- 34. Donker T, Griffiths KM, Cuijpers P, Christensen H. Psychoeducation for depression, anxiety and psychological distress: a meta-analysis. BMC Med. 2009;7:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Oud M, Mayo-Wilson E, Braidwood R, et al. Psychological interventions for adults with bipolar disorder: systematic review and meta-analysis. Br J Psychiatry. 2016;208(3):213–222. [DOI] [PubMed] [Google Scholar]
- 36. Butler LD, Waelde LC, Hastings TA, et al. Meditation with yoga, group therapy with hypnosis, and psychoeducation for long-term depressed mood: a randomized pilot trial. J Clin Psychol. 2008;64(7): 806–820. [DOI] [PubMed] [Google Scholar]
- 37. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: (DSM-IV-TR). Revised 4th ed. Washington (DC): American Psychiatric Association; 2000. [Google Scholar]
- 38. Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134(7):382–389. [DOI] [PubMed] [Google Scholar]
- 39. Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- 40. Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clinic Psychol. 1967;6(3):278–296. [DOI] [PubMed] [Google Scholar]
- 41. Guy W. Clinical global impressions. In: Guy W, editor. ECDEU Assessment manual for psychopharmacology (338). Rockville (MD): U.S. Department of Health, Education, and Welfare, Department of Health Education & Welfare; 1976. [Google Scholar]
- 42. Beck AT, Ward CH, Mendelson M, Mockb J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. [DOI] [PubMed] [Google Scholar]
- 43. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(1):385–396. [PubMed] [Google Scholar]
- 44. Endicott J, Nee J, Harrison W, Blumenthal R, et al. Quality of life enjoyment and satisfaction questionnaire: a new measure. Psychopharmacol Bull. 1993;29(2):321–326. [PubMed] [Google Scholar]
- 45. Festinger L. A theory of cognitive dissonance. Stanford (CA): Stanford University Press; 1957. [Google Scholar]
- 46. Fernandez E, Salem D, Swift JK, Ramtahal N. Meta-analysis of dropout from cognitive behavioral therapy: magnitude, timing, and moderators. J Consult Clin Psychol. 2015;83(6):1108. [DOI] [PubMed] [Google Scholar]