Abstract
Objectives:
Cannabis use is proposed as a risk factor for psychosis and is associated with depressive disorders. However, the relationship between recreational cannabis use and its longitudinal implications on anxiety conditions is less studied. The aim of this investigation is to systematically evaluate published literature and perform a meta-analysis of the data.
Methods:
A systematic search was performed of MEDLINE, Embase, and PsychINFO from inception to May 31, 2020, in addition to a hand search. Longitudinal studies that evaluated the relationship of cannabis use and development of anxiety were included. Where applicable, adjusted odds ratios (ORs) were extracted, pooled, and evaluated using random-effects meta-analysis.
Results:
After screening of unique abstracts (n = 6835), the final evaluation included 24 studies, of which 10 reported ORs that were analyzed quantitatively. Cannabis use was significantly associated with increased odds of developing any anxiety conditions (OR = 1.25; 95% CI, 1.01 to 1.54). Cannabis use was not significantly associated with developing generalized anxiety disorder, panic disorder, or social anxiety disorder. Review of studies not reporting OR revealed mixed results but are suggestive of a link between cannabis use and increased rates/severity of anxiety.
Conclusions:
Published evidence suggests that cannabis use is likely associated with increased risk of anxiety in the long term but variability of study designs precludes declaration of a causal relationship. Awareness of this association is of relevance for both clinical practice and mental health policy implementation.
Keywords: cannabis use disorders, cohort study, anxiety, systematic reviews, meta-analysis
Abstract
Objectifs:
L’usage du cannabis est proposé comme facteur de risque de psychose et est associé aux troubles dépressifs. Cependant, la relation entre l’usage récréatif du cannabis et ses implications longitudinales sur les conditions d’anxiété fait moins l’objet d’étude. La présente recherche vise à évaluer systématiquement la littérature publiée et à réaliser une méta-analyse des données.
Méthodes:
Une recherche systématique a été menée dans MEDLINE, Embase et PsychINFO, du début au 31 mai 2020, en plus d’une recherche manuelle. Les études longitudinales qui évaluaient la relation entre l’usage du cannabis et le développement de l’anxiété ont été incluses. Le cas échéant, les rapports de cotes (RC) ajustés ont été extraits, regroupés et évalués à l’aide d’une méta-analyse à effets aléatoires.
Résultats:
Après dépistage des résumés uniques (n = 6 835), l’évaluation finale comprenait 24 études, dont 10 présentaient des RC qui ont été analysés quantitativement. L’usage du cannabis était significativement associé à des probabilités accrues de développer une condition d’anxiété [RC = 1,25; IC à 95% 1,01 à 1,54]. L’usage du cannabis n’était pas significativement associé au développement d’un trouble d’anxiété généralisée, d’un trouble panique ou d’un trouble d’anxiété sociale. L’examen des études qui ne comportaient pas de RC a révélé des résultats mixtes mais suggère un lien entre l’usage du cannabis et des taux d’anxiété plus graves.
Conclusions:
Les données probantes publiées suggèrent que l’usage du cannabis est probablement associé à un risque accru d’anxiété à long terme mais la variabilité des méthodologies des études empêche de déclarer une relation causale. La connaissance de cette association est pertinente tant pour la pratique clinique que pour la mise en œuvre des politiques de santé mentale.
Introduction
In October 2018, Canada became the second country in the world to legalize and regulate cannabis for nonmedical purposes. This has been part of a global movement for the legalization of recreational cannabis production and retail following Uruguay and multiple American states.1 According to the most recent Canadian Tobacco, Alcohol and Drugs Summary in 2017, a survey representing a weighted total of 29.7 million Canadian residents, 12% reported using cannabis over the past year.2 Furthermore, postlegalization, the rate of use was as high as 34.8% among youth aged 18 to 24 years on the National Cannabis Surveys 2019).3 The widespread and increasing cannabis use as well as the changing legal landscape poses unique challenges to clinicians tasked with providing public education and counseling regarding cannabis and its mental health implications.4
Although the Canadian Task Force on Cannabis Legalization and Regulation recognized the risk of psychosis with early and regular use, there are little data on its use and the risk of anxiety conditions, which are said to affect over 2.4 million Canadians over the lifetime.5,6 This issue is particularly salient as cannabis is commonly regarded as an anxiolytic agent and is often used for self-medication, in spite of the lack of systematic evaluations of its long-term impact on the onset and cause of anxiety disorders.7,8
Published literature on cannabis use and prospective development of anxiety symptoms and/or disorders is limited. While a previous narrative review found the common co-occurrence of cannabis use and anxiety symptomatology, it observed the scarcity of prospective studies at the time to determine the relationship of cannabis use and long-term anxiety.9 Other narrative reviews provided mixed findings nestled within much broader study scopes and combined animal-based, cross-sectional and longitudinal data.10–14 In a recent systematic review focused on youth under 25 years, 6 cohort studies on cannabis use and depression and/or anxiety were identified; however, only one of the studies involved anxiety as an independent outcome.14
Among existing meta-analyses, results on cannabis use and prospective anxiety outcomes were either combined with depression and obsessive-compulsive disorder outcomes or based on a small number of cohort studies.15–17 For example, in a meta-analysis with studies published up to 2013, cannabis use was found to be positively associated with anxiety disorders.17 However, the authors recognized that only a small subset of its studies (n = 5) could be used to construe a temporal relationship and noted that limiting the literature search to only 2 databases precluded the inclusion of a more complete set of relevant studies. A subsequent meta-analysis with studies published up to 2016 also found cannabis use to be positively associated with elevated anxiety symptoms in the general population, based on 10 reports.18 However, the single-author design, methodological flaws in data extraction, as well as exclusion of studies of specific anxiety disorders may have led to potential bias in study selection and the findings. Neither review incorporated a systematic review component that would have enabled a synthesis of significant longitudinal data that could not be captured with a meta-analysis design.
Along with the increasing public and scientific interest in cannabis, a flourish of longitudinal studies has been published in the recent years. A thorough synthesis of their findings could strengthen our understanding of the complex interplay between cannabis use and anxiety. This systematic review and meta-analysis aims to summarize and update the literature on cannabis use and its long-term implications on anxiety, using both narrative and quantitative data and methods. Specifically, it focuses on longitudinal investigations to better determine possible temporal associations and optimizes search results by including multiple databases and minimizing search limits. In addition, the association between cannabis use and any specific anxiety-spectrum disorder was explored.
Methods
Search Strategy
A systematic literature search was performed of MEDLINE, Embase, and PsychINFO electronic databases from their inception (1860, 1883, and 1860, respectively) to December 2019. The search was updated on May 31, 2020. All references with either subject headings or keywords involving “cannabis” or “marijuana” or “marihuana” or “cannabinoid”; and “anxiety” or “anxiety disorders” or “phobia” or “panic” were collected. Each keyword was expanded to verify its definition and exploded such that relevant narrower terms were also included in the search. All keywords were searched with possible truncations, for example, “anxiet*,” to account for various suffixes. The search was not restricted to human-based and English language studies nor was it restricted to study design or publication type. The terms “cohort” or “follow-up” or “longitudinal” were not included in the search strategy to maximize search outcomes.
All unique titles and abstracts of identified studies were examined. Full texts of potentially relevant studies were reviewed by S.X. and M.I.H. simultaneously to consider their eligibility of inclusion. Disagreements were resolved by in-depth discussion and consensus. References of included studies were hand searched to identify additional relevant publications. Authors were contacted when a full text could not be obtained through electronic databases.
Inclusion/Exclusion Criteria
Studies were included if they met the following criteria: (1) were original studies published in a peer-reviewed journal; (2) collected population-based data in a longitudinal or prospective design; (3) included cannabis use with or without cannabis use disorder as an exposure variable; and (4) measured anxiety symptoms and/or disorders as outcome variable(s).
Studies were excluded if they: (1) were not longitudinal (e.g., cross-sectional) in design; (2) did not present cannabis use data separately from other psychoactive substances; (3) involved antenatal cannabis exposure; or (4) exclusively involved special patient populations with severe primary psychiatric conditions such as psychotic disorders. Studies of cohorts with depressive symptoms were included, given the high comorbidity and overlap of symptoms—if the anxiety data could be independently extracted. In cases of duplicate studies that drew data from the same cohort in the same time frame, the study using the heaviest cannabis use (e.g., cannabis use disorder) as exposure variable was included.
Outcome Measures
The primary outcome measure was the effect of cannabis on anxiety, as measured by validated rating scales, or diagnostic criteria of Diagnostic and Statistical Manual of Mental Disorders or International Classification of Diseases. If more than one anxiety symptom measure was provided in a particular study, the primary outcome measure for the study was preferred over other measures.
Quality Assessment
Quality of the included studies for meta-analysis was assessed using the National Institute of Health Study Quality Assessment Tools.19 Specifically, the Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies was selected, which outlines 14 criteria, including the specification of study population, participation/attrition rates, and adjustment of confounding variables, that guide to a global rating of either good, fair, or poor. S.X. and M.I.H. independently assessed the studies; ratings were compared and disagreements were resolved by consensus.
Data Extraction
Study characteristics, including year of publication, country of study, age at baseline and at follow-up, measures of cannabis use and anxiety, control variables, and study exclusions were extracted by S.X. and verified by K.W. If available, odds ratios (ORs) and associated 95% confidence interval (95% CI) of developing anxiety based on predetermined cutoff scores or individual anxiety disorder diagnoses, including generalized anxiety disorder (GAD), panic disorder (PD), and social anxiety disorder (SAD), were extracted. Otherwise, efforts were made to calculate ORs based on available data. For studies that report more than one OR, the following rules were applied in a step-wise, hierarchical manner to extract one OR per anxiety outcome per study:
The OR for the longest duration of follow-up was chosen;
The OR for the heaviest/most chronic use subgroup (e.g., daily use or cannabis use disorder) was chosen;
The OR from the model most adjusted for confounder variables (i.e., the most conservative estimate) was chosen; and
The OR accounting for/excluding baseline anxiety was chosen.
Data Analysis
Studies with available ORs were quantitatively synthesized using meta-analysis; other studies were narratively summarized. ORs were pooled using random-effects models, based on the assumption that observed variance is due to heterogeneity among studies in populations and methodologies.20 Heterogeneity across studies was quantified by I2 index.21 Subgroup analyses investigated whether strength of association was modified by early onset of cannabis use and study quality. All analyses were conducted using Review Manager Version 5.3.
Publication bias of studies included in the meta-analyses was assessed by using visual inspection of a funnel plot.22 Sterne and Egger found that it is best to use log OR as the horizontal axis and standard error as the vertical axis. The assumption is that studies of small sample sizes with insignificant results are less likely to get published. When there is no bias, the points in the plot, which show the effect estimates of each study, tend to symmetrically spread around the summary estimate solid line. An asymmetrical spread of the points indicates a publication bias.23
Results
Search Results
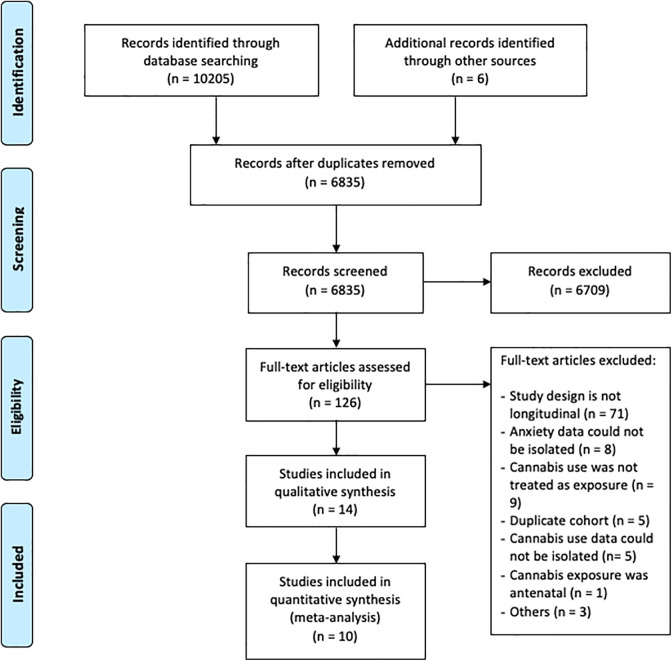
The search strategy yielded n = 10,211 references, of which n = 3,376 were duplicates. The study selection procedure and reasons for exclusion are summarized in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses flowchart (Figure 1). One hundred and twenty-six (n = 126) studies were assessed in full length, and n = 24 studies were included in the final review, of which n = 10 included ORs that could be analyzed quantitatively (total number of subjects = 49,273).
Figure 1.
PRISMA flow chart for literature search process. PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Study Characteristics
Study characteristics are detailed in Table 1. Study settings spanned North America (n = 14), Europe (n = 6), and Australia and Oceania (n = 4). Half of the studies (n = 12) were published after 2013. The majority of the studies (n = 18) enrolled participants in their adolescence (less than or equal to 18 years old) and measured cannabis use at that time point. Length of follow-up ranged from 12 weeks to over 20 years, with half of the studies (n = 12) following participants for 5 years or more.
Table 1.
Characteristics and Main Findings of 24 Included Studies.
| Study and Country | Study Population | n | Baseline Age | Follow-up Length | Cannabis Measure | Anxiety Measure | Control Variables | Main Findings at Last Follow-up | Adjusted OR (95% CI) |
|---|---|---|---|---|---|---|---|---|---|
| Weller and Halikas24; USA | General population | 147 | 18+ | 6 to 7 Years | Cannabis use over 50 times in the past 6 months | Interview similar to DIS | Heavy cannabis use was not associated with greater prevalence of anxiety disorder at follow-up | ||
| Fergusson, et al.25; New Zealand | Birth cohort | 927 | 15 | 1 Year | Self-report and parental reports of lifetime cannabis use | DISC, DIS | Gender, family functioning, association with delinquent or substance using peers, cigarette smoking, family history of alcohol/drug abuse/dependence, alcohol use, offending, conduct/oppositional disorders, childhood conduct problems, truancy, IQ, plans for future secondary education, intention to enter university, baseline anxiety disorders depression and suicidal ideation | Cannabis use was not significantly associated with development of anxiety disorders at age 16 | 1.2 (0.5 to 2.8) |
| Fergusson and Horwood26; New Zealand | Birth cohort | 935 | 15 | 3 Years | Frequency of use between age 15 and 16 | CIDI | Maternal age, family SES, gender, changes of parents, parental history of offending, childhood sexual abuse, IQ, conduct problems, self-esteem, novelty seeking, mood disorder (14 to 16), anxiety disorder (14 to 16) | Frequent cannabis use was significantly associated with anxiety disorder at 16 to 18 but not after covariates were controlled | |
| Brook et al.27; USA | Youth in upstate New York | 698 | 13 (avg) | 6 Years | Self-report converted to light, moderate, and heavy use | DISC-I (Supplemental Material) | Age, gender, adolescent psychiatric disorder | Adolescent cannabis use was not associated with anxiety disorders in young adulthood | 1.16 (1.00 to 1.35) |
| Windle and Wiesner28; USA | High school students | 1,205 | 15 | 5 Years | Self-report converted to trajectory groups | CIDI | Not available | Cannabis trajectory group membership was not associated with lifetime anxiety disorder prevalence in young adulthood | |
| van Laar et al.29; the Netherlands | Adults | 3,854 | 18 to 64 | 3 Years | Lifetime use more than 5 times | CIDI | Age, gender, education, urbanicity, employment, partner status, neuroticism, parental psychiatric history, childhood trauma, lifetime alcohol use disorders or other substance use disorders, lifetime mood disorders, lifetime psychotic symptoms | Cannabis use was not significantly associated with incidence of anxiety disorders | 1.18 (0.71 to 1.97) |
| Cannabis use was not significantly associated with incidence of GAD | 1.83 (0.97 to 3.44) | ||||||||
| Cannabis use was not significantly associated with incidence of PD | 1.29 (0.61 to 2.71) | ||||||||
| Cannabis use was not significantly associated with incidence of SAD | 0.80 (0.36 to 1.79) | ||||||||
| Zvolensky et al.30; USA | High school students | 1,709 | 14 to 18 | 8 Years | Lifetime consumption, abuse, dependence | DSM-IV | Smoking, noncannabis drug dependence comorbidity | Lifetime history of cannabis dependence was not significantly associated with development of PD | 1.6 (0.45 to 5.8) |
| Fröjd et al.31; Finland | High school students | 2,070 | 15 to 16 | 2 Years | Frequency of use (over 5 times) in the past 2 years | Single question for GAD, SPIN | Sex, family structure, parental education levels, baseline depression | Cannabis use was not significantly associated with incidence of GAD | 0.4 (0.1 to 3.3) |
| Cannabis use was not significantly associated with incidence of SAD | 0.7 (0.2 to 2.2) | ||||||||
| Brook et al.32; USA | African American and Puerto Rican youth | 837 | 14 (avg) | 15 Years | Self-report converted to trajectory groups | SCL (items for anxiety) | Sex, ethnicity, differing baseline schools | Chronic use group was significantly associated with anxiety symptoms when compared with non- or low-use groups | 2.3 (1.3 to 4.0) |
| Degenhardt et al.33; Australia | High school students | 1,756 | 14 to 15 (avg) | 15 Years | Frequency of use in the past 6 months, maximum use in the past year, CIDI for DSM-IV | CIDI-Short Form | Sex, school location, low parental education, parental divorce/separation, concurrent alcohol/illicit substances, adolescent anxiety/depression | Weekly cannabis use since adolescence was significantly associated with increased odds of anxiety disorder at 29 years | 3.2 (1.1 to 9.2) |
| Albertella and Norberg34; Australia | Adolescents receiving residential treatment | 132 | 14 to 18 | 3 Months | BTOM items; SDS | BSI | Not available | Reduction of cannabis quantity/frequency was associated with reduction of anxiety symptom | |
| Caldeira et al.35; USA | College students | 973 | 17 to 20 | 6 Years | Self-report converted to trajectory groups | BAI | Baseline BAI score, sex, race, ethnicity, income, alcohol, and tobacco use trajectory group | Chronic use group had more anxiety symptoms than nonuse or low-stable use groups at follow-up | |
| Gage et al.36; UK | Birth cohort | 1,682 | 16 | 2 Years | Frequency of use in the past year | CIS-R | Gender, family history of depression, maternal education, urban living, borderline personality traits, victimization, peer problems, alcohol use, other illicit drug use | Cannabis use was not significantly associated with incidence of SAD | 1.06 (0.73 to 1.53) |
| Bechtold et al.37; USA | Young men | 386 | 12 to 16 | 20+ Years | SUQ converted to trajectory groups | DIS for DSM-IV | SES at age 36; past year use of alcohol, cigarettes, and illicit drugs; health problems at age 14 | Cannabis trajectory group membership was not associated with differences in lifetime anxiety | |
| Danielsson et al.38; Sweden | Adults | 8,598 | 20 to 64 | 3 Years | Ever use of cannabis | SCL (items for anxiety) | Age, sex, ethnicity, other illicit drug use, alcohol use, education, place of upbringing, childhood adverse circumstances | Cannabis use was associated with RR of 1.09 (95% CI, 0.98 to 1.20) for anxiety at follow-up | |
| Feingold et al.39; USA | General population | 34,653 | 18+ | 3 Years | AUDADIS-IV; lifetime cannabis use and past-year use | DSM-IV | Sex, age, educational level, household income, marital status, urbanity, and region | Cannabis dependence was not significantly associated with new diagnosis of any anxiety disorder | 0.99 (0.65 to 1.5) |
| Cannabis dependence was not significantly associated with new diagnosis of GAD | 1.08 (0.61 to 1.93) | ||||||||
| Cannabis dependence was not significantly associated with new diagnosis of PD | 1.69 (0.88 to 3.25) | ||||||||
| Cannabis dependence was not significantly associated with new diagnosis of SAD | 1.75 (0.95 to 3.23) | ||||||||
| Otten et al.40; the Netherlands | Adolescents | 1,424 | 13 | 5 Years | Frequency of use in the last 12 months | YSR Anxiety Problems Scale | Sex, age, alcohol use and tobacco use, baseline anxiety | Cannabis use was significantly associated with higher levels of anxiety at follow-up (significant association was found in short 5-HTTLPR allele carriers but not in noncarriers) | |
| Guttmannova et al.41; USA | Youth from high-crime areas | 808 | 14 | 20 Years | Self-report converted to trajectory groups | DIS for DSM-IV | Gender, ethnicity, childhood poverty, average frequency of tobacco, and alcohol use during adolescence | Chronic cannabis use was significantly associated with increased IRR of 1.57 (95% CI, 1.08 to 2.28) for GAD | |
| Hser et al.42; USA | Adults with cannabis dependence | 302 | 18 to 50 | 12 Weeks | Frequency of use in past 7 days | HADS | Age, sex, race/ethnicity, treatment condition, time-varying tobacco, and alcohol use | Reduction of cannabis use was associated with improvement in anxiety | |
| Thompson, et al.43; Canada | Adolescents | 662 | 12 to 18 | 10 Years | Self-report converted to trajectory groups | BCFPI | Sex, SES, age, and respective assessments at baseline | Chronic cannabis use was associated with higher levels of anxiety symptoms than abstainer and decreaser groups | |
| Hawes et al.44; USA | Adolescents | 401 | 14 to 17 | 2 Years | DUHQ converted to trajectory groups | Computerized DISC-IV symptom count | Sex and race/ethnicity, parental education, general intelligence | Cannabis trajectory membership was not associated with differences in anxiety level at follow-up | |
| Duperrouzel et al.45; USA | Junior high/high school students | 250 | 14- to 17 | 1 Year | Frequency of use in the past 30 days | DASS-21 (anxiety subscale) | Sex, depression, use of alcohol and nicotine | Higher level of cannabis use was associated with more persisting self-reported anxiety at follow-up | |
| Tucker et al.46; USA | Adolescents | 2429 | Grade 6 to 7 | 10 Years | Frequency of use in the past 30 days | GAD-7 | Age, gender, race/ethnicity, mother’s education, intervention group at wave 1 | Cannabis and tobacco couse was associated with higher GAD scores, but not cannabis only use | |
| Hines et al.47; UK | General population | 1,087 | 24 | 1 Year | Self-report of type of cannabis most commonly used in the past year (high/low potency) | CIS-R | Childhood sociodemographic factors, prospective mental health measures, frequency of cannabis use | High potency cannabis use was associated with increased likelihood of GAD | 1.92 (1.11 to 3.32) |
Note. AUDADIS = Alcohol Use Disorder and Associated Disabilities Interview Schedule; Avg = average; BAI = Beck Anxiety Inventory; BCFPI = Brief Child and Family Phone Interview; BSI = Brief Symptom Inventory; BTOM = Brief Treatment Outcome Measure; CI = confidence interval; CIDI = Composite International Diagnostic Interview; CIS-R: Clinical Interview Schedule-Revised; DASS = Depression, Anxiety, Stress Scale; DIS = Diagnostic Interview Schedule; DISC = Diagnostic Interview Schedule for Children; DSM = Diagnostic and Statistical Manual; DUSQ = Drug Use History Questionnaire; GAD = generalized anxiety disorder; HADS = Hospital Anxiety and Depression Scale; IQ = intelligence quotient; IRR = incidence risk ratio; OR= odds ratio; PD = panic disorder; RR = relative risk; SAD = social anxiety disorder; SCL = Symptom Checklist; SES = socioeconomic status; SDS = Severity of Dependence Scale; SPIN = Social Phobia Inventory; SUQ = Substance Use Questionnaire; WISC-R = Wechsler Intelligence Scale for Children-Revised; YSR = Youth Self-Report.
Measures of cannabis exposure were largely based on self-report of use frequency over a defined time period (e.g., past 30 days, past year, lifetime). Two studies considered cannabis dependence, and 1 study considered the type/potency of cannabis most commonly used as the exposure variable. Measures of anxiety outcome were also varied, with 10 (n = 10) studies using rating scales, for example, Beck Anxiety Inventory, Brief Symptom Inventory, and Hospital Anxiety and Depression Scale. The rest (n = 14) used a structured interview that was delivered by either mail, computer, phone, and/or in person.
Of the 10 studies included in the quantitative analysis, 6 were judged to be of high quality (Table 2).
Table 2.
Quality Assessment of 10 Studies Included in Meta-Analyses Based on the National Institute of Health Study Quality Assessment Tool.
Qualitative Analyses
Fourteen studies investigated the longitudinal association of cannabis use and anxiety symptomatology at follow-up but did not report OR or provide sufficient data for its calculation. Their findings are summarized narratively below.24,26-28,34,35,37,38,40–45,47
Cannabis use was found to be significantly linked to increased risk of anxiety in 5 studies. In a U.S. based cohort of 973 college students, cannabis users of the chronic, late-increase and early decline trajectory groups experienced more anxiety symptoms than nonusers or low users 6 years later when adjusted for baseline anxiety and other substance use.35 Cannabis use trajectory groups were also developed in a Canada-based study of 662 adolescents, among whom chronic users reported more anxiety symptoms in young adulthood than all other groups except occasional users.43 Adolescents of greater cannabis use were further found to experience more persisting anxiety level in another U.S. study.45 In a Dutch study of 1,425 adolescents followed over 5 years, cannabis use predicted anxiety levels in a linear regression model (β = 0.08, SE = 0.03; P = 0.01). A parallel process latent growth model indicated that the positive association was present among carriers of the short allele of the 5-HTTLPR gene, which is involved in the regulation of serotonin activation and not noncarriers.40 Regarding specific anxiety disorders, one study of 808 youth from high-crime areas in Seattle reported that adolescence-onset regular cannabis use predicted GAD when assessed at age 33 (incidence risk ratio = 1.57; 95% CI, 1.08 to 2.28).41
The positive association between cannabis use and prospective anxiety lost statistical significance in 2 other studies when adjusted for confounding variables.26,38 In a 3-year longitudinal study of 6,720 Swedish participants, the relative risk of developing anxiety with baseline cannabis use was 1.38 (95% CI, 1.26 to 1.50) when adjusted only for age and sex. It dropped to 1.09 (95% CI, 0.98 to 1.20) when other variables (e.g., illicit drug use and family tension) were included.38 Another New Zealand based study found that frequent cannabis use at age 15 to 16 years was significantly associated with a higher likelihood of anxiety at 3-year follow-up. The association disappeared when the model was adjusted to include confounding factors. Maternal age, childhood sexual abuse, low self-esteem, and presence of mood/anxiety disorders were identified as significant covariates.26
Two studies examined the effect of cannabis use reduction on prospective anxiety.34,42 An improvement in anxiety (β = −0.09, SE = 0.04; P < 0.05) at 12-week follow-up was observed in a group of 152 adults who reduced their cannabis use as part of a randomized controlled trial of N-acetylcysteine as treatment for cannabis use disorder.42 In another study, quantity/frequency of cannabis use and anxiety symptoms significantly reduced among 132 Australian adolescents 3 months after they completed a residential treatment program.34 However, it was thought that the change in mental health symptoms was not significantly associated with the change in cannabis use, and the authors speculated that unmeasured confounding factors may have prevented the finding of a relationship.
Five studies did not find any significant association between cannabis use and anxiety outcomes. Three different U.S. based studies independently found that cannabis use trajectory group status was not predictive of increased anxiety levels or lifetime anxiety diagnosis in adulthood.28,37,44 For instance, in a cohort of 401 adolescents with chronic, escalating, and low cannabis use, anxiety outcome did not differ across groups at 2-year follow-up (χ2 = 0.12, df = 2, P = .94).44 One small study from 1985 focused on the adult population and found 11 out of 97 regular cannabis users were newly diagnosed with anxiety disorders at follow-up 6 to 7 years later, but this increase in prevalence was not considered to be statistically significant.24 In another study of 2,429 U.S. youth, latent growth modeling suggested GAD symptoms at 10-year follow-up were predicted by higher probability of cannabis and tobacco couse, but not cannabis use alone (intercept estimate = −0.01, slope estimate = 0.00, P > 0.05).46
Quantitative Analyses
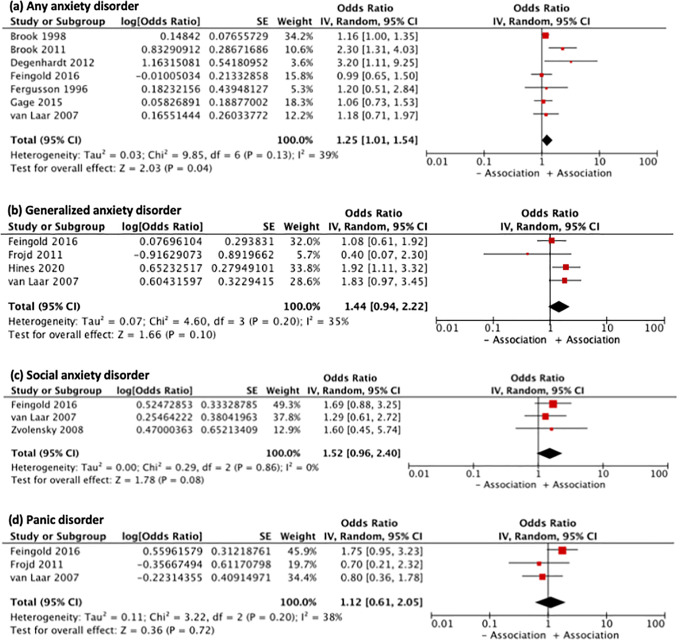
The main meta-analysis included 7 studies that reported ORs of developing any clinically significant anxiety, defined by the individual studies as either meeting cutoff on a questionnaire or meeting criteria of psychiatric diagnoses in the anxiety spectrum.25,27,29,32,33,36,39 Cannabis use was found to be significantly associated with increased odds of developing anxiety on follow-up (OR = 1.25; 95% CI, 1.01 to 1.54; I2 = 39%; Figure 2). The OR was reduced if the analysis was restricted to those using a structured diagnostic interview rather than a self-report questionnaire (OR = 1.15; 95% CI, 1.01 to 1.30). The OR remained positive but did not retain statistical significance if the analysis was restricted to high-quality studies (OR = 1.10; 95% CI, 0.82 to 1.47), or to studies capturing cannabis use prior to 18 years old (OR = 1.32; 95% CI, 0.97 to 1.79), or to studies published after 1999 (OR = 1.36; 95% CI, 0.95 to 1.96).
Figure 2.
Forest plots showing pooled odds ratio of developing (A) any anxiety, (B) generalized anxiety disorder, (C) panic disorder, and (D) social anxiety disorder with baseline cannabis use.
A small number of studies reported ORs of developing specific anxiety disorders: GAD (n = 4), SAD (n = 3), and PD (n = 3).29-31,39,47 Cannabis use was nonsignificantly associated with increased odds of developing GAD (OR = 1.44; 95% CI, 0.94 to 2.22; I2 = 35%), SAD (OR = 1.12; 95% CI, 0.61 to 2.05; I2 = 38%), and PD (OR = 1.52; 95% CI, 0.96 to 2.40; I2 = 0%) at follow-up (Figure 2).
The funnel plot incorporated the effect estimates of the 7 ORs of the main analysis (Figure 3). The symmetrical distribution of points indicated that there was little evidence for publication bias.
Figure 3.
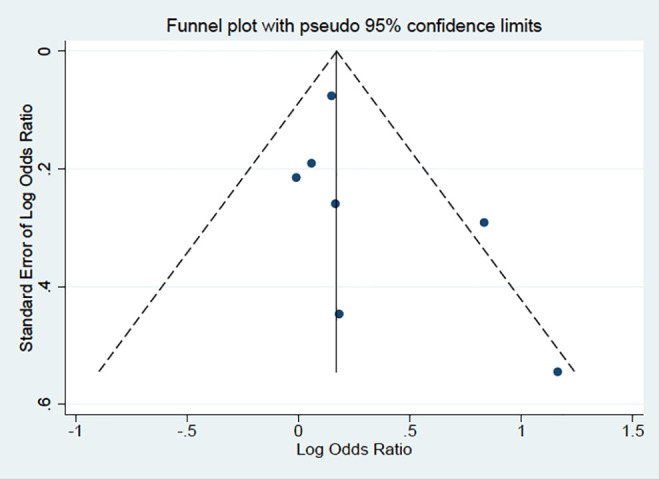
Funnel plot testing for publication bias.
Discussion
Although there exist several publications on the interrelationship between cannabis use and anxiety symptoms, few explored it longitudinally.9 This review included 24 cohort studies and involved participants from 8 countries and 3 continents, and who were followed for a period of up to 20 years.24-47 Furthermore, this is the first review that evaluated the association between cannabis use and development of specific anxiety disorders such as GAD, SAD, and PD.
Meta-analysis of 7 studies published up to May 2020 revealed a pooled OR of 1.25 (95% CI, 1.01 to 1.54) of developing an anxiety disorder among cannabis users. When the analysis was restricted to only high-quality studies and adolescence-onset cannabis use, the pooled OR remained positive but was not statistically significant. This finding reinforces previous meta-analyses, which either included fewer studies (n = 3 to 5) or had significant methodological flaws and reported a positive association between cannabis use and anxiety disorders with pooled ORs between 1.15 and 1.28.15,17,18
Of note, one full text48 included in previous meta-analyses16–18 could not be located in spite of extensive efforts. Should this study be included, the pooled OR of the current meta-analysis would only be minimally increased to OR = 1.28 (95% CI, 1.07 to 1.54). Thus, the addition of the study would not alter the overall finding. Meta-analyses of studies examining specific anxiety disorders revealed pooled ORs between 1.12 and 1.52, also indicating a similar positive yet statistically nonsignificant relationship.
This review also included 14 additional longitudinal studies that would otherwise be excluded from meta-analyses. The studies, most of which were published in the past 2 years, are intended to supplement the quantitative findings and to respond to the call to include more up-to-date literature.49 While the studies reported mixed findings, many are indicative of a positive association. Seven studies supported an association between cannabis use and increased risk of developing an anxiety disorder and/or increased severity of the condition.35,38,40,41,43,45,47 Another study suggested reduction of cannabis use to be associated with decreased severity of anxiety on follow-up.42
The evaluation considering both the quantitative and qualitative data indicates a summative trend that cannabis use may pose an increased risk on anxiety outcomes. However, the results are to be interpreted with caution as subgroup analyses revealed the loss of statistical significance when only high-quality data were included. The findings are also less statistically robust for adolescence-onset cannabis use. It has been argued that much of the observed association between cannabis use and affective outcomes can be explained by confounding variables.16 In one study included in the main meta-analysis, the odds of developing PD from cannabis dependence was reported to be 4.9 (95% CI, 1.7 to 14.0); however, after adjusting for noncannabis drug dependence comorbidity and cigarette smoking, the odds were reduced to 1.6 and became statistically nonsignificant.47 Five individual studies that were qualitatively reviewed also did not find any association between cannabis use and future anxiety,24,28,37,44,46 including the study with the longest period of follow-up, in which subjects aged 12 to 16 years were followed up at age 33 to 39 years.37
The effect sizes from this meta-analysis are less pronounced than that of cannabis on the onset of psychotic disorders (ORs between 1.41 and 3.90) as well as mood disorders (OR up to 1.62 among heavy users).15,16,50–52 Recreational cannabis, used as the exposure variable of all included studies, contains 2 main components: delta-9-tetrahydrocannabinol (THC) and cannabidiol (CBD). Both modulate human anxiety responses in complex manners that are not fully established, though the anxiogenic effect of THC is well-recognized while CBD is suggested to have anxiolytic properties.53 Several mechanisms have been proposed to mediate the neurochemical effects of cannabis including activation of the serotonin 1A receptors (5-HT1A receptors), facilitation of the endocannabinoid signaling, and reduction of glutamate transmission. Furthermore, there is evidence that cannabis may increase adult hippocampal neurogenesis and can modulate the activities of limbic and paralimbic regions.54–59 An increasing number of reviews support the potential application of CBD as a treatment for anxiety.60,61 It is therefore possible that the effect size of this review is moderated by the purported opposing effects of the constituents of cannabis as they relate to anxiety.
The findings from this review should take account of its limitations. There is a large variability of how cannabis use is measured across studies. In order to minimize the variability, only ORs from the heaviest use group from each study were extracted wherever possible. Thus, results of the meta-analysis are not entirely generalizable to rare or occasional cannabis use. Furthermore, the majority of the studies quantify cannabis use in terms of frequency of use and do not factor in quantity, potency, or CBD to THC ratio of the cannabis products. Therefore, even among the heaviest use groups, exposure to cannabis may not be consistent. While the THC content in recreational cannabis has been steadily increasing,62 limiting the main meta-analysis to more recent studies resulted in an OR that was no longer statistically significant. Upon examining studies in the qualitative review, no consistent pattern was identified either between the year of publication and study findings. This review has thus not been able to demonstrate that the year of publication (and indirectly, THC concentration) has an effect on anxiety conditions. Whereas previous reviews explored the association between cannabis use and anxiety outcomes using primarily cross-sectional studies, this review focused on longitudinal studies to better understand the directionality of the relationship. However, the results still do not confirm any causal relationship due to reasons of residual confounding and lack of causal inference methodology in most studies. Another intrinsic limitation to using longitudinal data is attrition, which is up to 36% to 37% in multiple studies.32,40,46 As individuals with higher psychopathology burden at follow-up are less likely to be contacted successfully,63 the meta-analysis may underestimate the true odds of anxiety outcomes. The meta-analysis additionally indicates that the strength of association may be affected by the modality of anxiety measurement, as the OR decreased when studies using self-report questionnaires were excluded. The effect size may also be underestimated as individuals may be more prone to underreport symptoms in interviews.64 Although efforts were made to explode each keyword, the search results could be optimized by including additional search terms that encompass more medicinal cannabis concepts such as nabilone and nabiximols. Although a funnel plot was used to test for publication bias, the number of studies included was less than the liberal criterion of 10.65 Thus, it may not be sufficient to detect a bias should it exists.
To conclude, this systematic review and meta-analysis examined 24 longitudinal studies on baseline cannabis use and anxiety outcomes. We found a general trend that cannabis use may increase the odds of developing an anxiety disorder. This finding should be considered alongside numerous recent prospective cohort studies demonstrating increased levels of anxiety with cannabis use in the life span. With the legalization of recreational cannabis in Canada and beyond, mental health clinicians are increasingly questioned by patients and caregivers about the impacts of cannabis use on mental well-being. Clinicians may use these findings to provide psychoeducation to patients about the potential risk and should consider cannabis use as an exacerbating factor for anxiety, particularly in patients who do not improve with standard treatment such as selective serotonin reuptake inhibitors and cognitive behavioral therapy. Finally, it is essential that public health policy-makers are updated on the accumulating evidence regarding the negative consequences of recreational cannabis on mental health. More longitudinal studies are needed to strengthen the current understanding of cannabis use and prospective anxiety. Future studies are recommended to consider ways to more precisely characterize cannabis exposure, as there may be new possibilities to enroll participants who use medicinal cannabis or those who use retail products with known CBD and/or THC concentrations. Finally, it may be important to consider anxiety as an independent entity from other psychiatric comorbidities and to continue to explore the relationship between cannabis use and specific anxiety disorders.
Supplemental Material
Supplemental Material, NIH_Study_Quality_Assessment_submission.xlsx-CJP-2020-085-SR.R1 for Cannabis Use and Prospective Long-Term Association with Anxiety: A Systematic Review and Meta-Analysis of Longitudinal Studies: Usage du cannabis et association prospective à long terme avec l’anxiété: une revue systématique et une méta-analyse d’études longitudinales by Siqi Xue, M. Ishrat Husain, Haoyu Zhao and Arun V. Ravindran in The Canadian Journal of Psychiatry
Acknowledgments
The authors would like to acknowledge the assistance of the following colleagues at the Centre for Addictions and Mental Health (CAMH): Ms Sarah Bonato for advising on the systematic literature search strategy, Mr Kevin Wang for verifying the extraction of ORs and running preliminary statistical analyses, and Dr Wei Wang for providing guidance on the funnel plot creation. The authors would also like to thank Dr Zohn Rosen and librarian staff at CAMH, Gerstein Science Information Centre and Robarts Library for their assistance in locating original articles. This work was supported in part by an Academic Scholars Award to MIH from the Department of Psychiatry, University of Toronto.
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: MIH is a PI for a trial sponsored by COMPASS Pathways Limited for which he receives salary support. The other authors declare that there is no conflict of interest.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Siqi Xue, MD  https://orcid.org/0000-0002-6937-9552
https://orcid.org/0000-0002-6937-9552
Arun V. Ravindran, MBBS, PhD, FRCP(C)FRCPsych  https://orcid.org/0000-0002-1655-2753
https://orcid.org/0000-0002-1655-2753
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Hammond D, Goodman S, Wadsworth E, Vicki R, Christian B, Wayne H. Evaluating the impacts of cannabis legalization: the international cannabis policy study. Int J Drug Policy. 2020;77:102698. [DOI] [PubMed] [Google Scholar]
- 2. Canadian Tobacco, Alcohol and Drugs Survey (CTADS): Summary of results for 2017. Government of Canada. 2019 [cited 2020 Jan]. https://www.canada.ca/en/health-canada/services/canadian-tobacco-alcohol-drugs-survey/2017-summary.html
- 3. Rotermann M. Analysis of trends in the prevalence of cannabis use and related metrics in Canada. Health Rep. 2019;30(6):3–13. [DOI] [PubMed] [Google Scholar]
- 4. Hall W, Weier M. Has marijuana legalization increased marijuana use among US youth? JAMA Pediatr. 2017;171(2):116–118. [DOI] [PubMed] [Google Scholar]
- 5. McLellan AA, Ware MA, Boyd S, et al. A framework for the legalization and regulation of cannabis in Canada. Government of Canada. 2016 [cited 2019 Nov]. https://www.canada.ca/en/health-canada/services/drugs-medication/cannabis/laws-regulations/task-force-cannabis-legalization-regulation.html?=undefined&wbdisable=true [Google Scholar]
- 6. Pearson C, Janz T, Ali J. Mental and substance use disorders in Canada. Statistics Canada. 2013 [2019 Nov]. https://www150.statcan.gc.ca/n1/pub/82-624-x/2013001/article/11855-eng.pdf
- 7. Wittchen HU, Fröhlich C, Behrendt S, et al. Cannabis use and cannabis use disorders and their relationship to mental disorders: a 10-year prospective-longitudinal community study in adolescents. Drug Alcohol Depend. 2007;88(Suppl 1):S60–S70. [DOI] [PubMed] [Google Scholar]
- 8. Farris SG, Metrik J, Bonn-Miller MO, Christopher WK, Michael JZ. Anxiety sensitivity and distress intolerance as predictors of cannabis dependence symptoms, problems, and craving: the mediating role of coping motives. J Stud Alcohol Drugs. 2016;77(6):889–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Crippa JA, Zuardi AW, Martín Santos R, et al. Cannabis and anxiety: a critical review of the evidence. Hum Psychopharmacol. 2009;24(7):515–523. [DOI] [PubMed] [Google Scholar]
- 10. Vorspan F, Mehtelli W, Dupuy G, Vanessa B, Jean-Pierre L. Anxiety and substance use disorders: co-occurrence and clinical issues. Curr Psychiatry Rep. 2015;17(2):4. [DOI] [PubMed] [Google Scholar]
- 11. Hanna RC, Perez JM, Ghose S. Cannabis and development of dual diagnoses: a literature review. Am J Drug Alcohol Abuse. 2017;43(4):442–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hoch E, Bonnet U, Thomasius R, Florian G, Havemann-Reinecke U, Ulrich WP. Risks associated with the non-medicinal use of cannabis. Dtsch Arztebl Int. 2015;112(16):271–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rubino T, Zamberletti E, Parolaro D. Adolescent exposure to cannabis as a risk factor for psychiatric disorders. J Psychopharmacol. 2012;26(1):177–188. [DOI] [PubMed] [Google Scholar]
- 14. Hosseini S, Oremus M. The effect of age of initiation of cannabis use on psychosis, depression, and anxiety among youth under 25 years. Can J Psychiatry. 2019;64(5):304–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gobbi G, Atkin T, Zytynski T, et al. Association of cannabis use in adolescence and risk of depression, anxiety, and suicidality in young adulthood: a systematic review and meta-analysis. JAMA Psychiatry. 2019;76(4):426–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Moore TH, Zammit S, Lingford-Hughes A, et al. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet. 2007;370(9584):319–328. [DOI] [PubMed] [Google Scholar]
- 17. Kedzior KK, Laeber LT. A positive association between anxiety disorders and cannabis use or cannabis use disorders in the general population-a meta-analysis of 31 studies. BMC Psychiatry. 2014;14(1):136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Twomey CD. Association of cannabis use with the development of elevated anxiety symptoms in the general population: a meta-analysis. J Epidemiol Community Health. 2017;71(8):811–816. [DOI] [PubMed] [Google Scholar]
- 19. Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. National Heart, Lung, and Blood Institute (NIH). 2019. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools [Google Scholar]
- 20. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. [DOI] [PubMed] [Google Scholar]
- 21. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. [DOI] [PubMed] [Google Scholar]
- 22. Egger M, Smith GD, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;135(7109):629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sterne JA, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol. 2001;54(10):1046–1055. [DOI] [PubMed] [Google Scholar]
- 24. Weller RA, Halikas JA. Marijuana use and psychiatric illness: a follow-up study. Am J Psychiatry. 1985;142(7):848–850. [DOI] [PubMed] [Google Scholar]
- 25. Fergusson DM, Lynskey MT, Horwood LJ. The short-term consequences of early onset cannabis use. J Abnorm Child Psychol. 1996;24(4):499–512. [DOI] [PubMed] [Google Scholar]
- 26. Fergusson DM, Horwood LJ. Early onset cannabis use and psychosocial adjustment in young adults. Addiction. 1997;92(3):279–296. [PubMed] [Google Scholar]
- 27. Brook JS, Cohen P, Brook DW. Longitudinal study of co-occurring psychiatric disorders and substance use. J Am Acad Child Adolesc Psychiatry. 1998;37(3):322–330. [DOI] [PubMed] [Google Scholar]
- 28. Windle M, Wiesner M. Trajectories of marijuana use from adolescence to young adulthood: predictors and outcomes. Dev Psychopathol. 2004;16(4):1007–1027. [DOI] [PubMed] [Google Scholar]
- 29. Van Laar M, Van Dorsselaer S, Monshouwer K, De Graaf R. Does cannabis use predict the first incidence of mood and anxiety disorders in the adult population? Addiction. 2007;102(8):1251–1260. [DOI] [PubMed] [Google Scholar]
- 30. Zvolensky MJ, Lewinsohn P, Bernstein A, et al. Prospective associations between cannabis use, abuse, and dependence and panic attacks and disorder. J Psychiatr Res. 2008;42(12):1017–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Fröjd S, Ranta K, Kaltiala-Heino R, Marttunen M. Associations of social phobia and general anxiety with alcohol and drug use in a community sample of adolescents. Alcohol Alcohol. 2011;46(2):192–199. [DOI] [PubMed] [Google Scholar]
- 32. Brook JS, Lee JY, Brown EN, Stephen JF, David WB. Developmental trajectories of marijuana use from adolescence to adulthood: personality and social role outcomes. Psychol Rep. 2011;108(2):339–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Degenhardt L, Coffey C, Romaniuk H, et al. The persistence of the association between adolescent cannabis use and common mental disorders into young adulthood. Addiction. 2012;108(1):124–133. [DOI] [PubMed] [Google Scholar]
- 34. Albertella L, Norberg MM. Mental health symptoms and their relationship to cannabis use in adolescents attending residential treatment. J Psychoact Drugs. 2012;44(5):381–389. [DOI] [PubMed] [Google Scholar]
- 35. Caldeira KM, O’Grady KE, Vincent KB, Amelia MA. Marijuana use trajectories during the post-college transition: health outcomes in young adulthood. Drug Alcohol Depend. 2012;125(3):267–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Gage SH, Hickman M, Heron J, et al. Associations of cannabis and cigarette use with depression and anxiety at age 18: findings from the Avon longitudinal study of parents and children. PloS One. 2015;10(4):e0122896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bechtold J, Simpson T, White HR, Pardini D. Chronic adolescent marijuana use as a risk factor for physical and mental health problems in young adult men. Psychol Addict Behav. 2015;29(3):552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Danielsson AK, Lundin A, Agardh E, Peter A, Yvonne F. Cannabis use, depression and anxiety: a 3-year prospective population-based study. J Affect Disord. 2016;193:103–108. [DOI] [PubMed] [Google Scholar]
- 39. Feingold D, Weiser M, Rehm J. The association between cannabis use and anxiety disorders: results from a population-based representative sample. Eur Neuropsychopharmacol. 2016;26(3):493–505. [DOI] [PubMed] [Google Scholar]
- 40. Otten R, Huizink AC, Monshouwer K, Hanneke EC, Simone O. Cannabis use and symptoms of anxiety in adolescence and the moderating effect of the serotonin transporter gene. Addict Biol. 2017;22(4):1081–1089. [DOI] [PubMed] [Google Scholar]
- 41. Guttmannova K, Kosterman R, White HR, et al. The association between regular marijuana use and adult mental health outcomes. Drug Alcohol Depend. 2017;179:109–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Hser YI, Mooney LJ, Huang D, et al. Reductions in cannabis use are associated with improvements in anxiety, depression, and sleep quality, but not quality of life. J Subst Abuse Treat. 2017;81:53–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Thompson K, Merrin GJ, Ames ME, Bonnie L. Marijuana trajectories in Canadian youth: associations with substance use and mental health. Can J Behav Sci. 2018;50(1):17. [Google Scholar]
- 44. Hawes SW, Trucco EM, Duperrouzel JC, Stefany C, Raul G. Developmental pathways of adolescent cannabis use: risk factors, outcomes and sex-specific differences. Subst Use Misuse. 2019;54(2):271–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Duperrouzel J, Hawes SW, Lopez-Quintero C, Pacheco-Colón I, Jonathan C, Raul G. The association between adolescent cannabis use and anxiety: a parallel process analysis. Addict Behav. 2018;78:107–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Tucker JS, Rodriguez A, Dunbar MS, et al. Cannabis and tobacco use and co-use: trajectories and correlates from early adolescence to emerging adulthood. Drug Alcohol Depend. 2019;204:107499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Hines LA, Freeman TP, Gage SH, et al. Association of high-potency cannabis use with mental health and substance use in adolescence. JAMA Psychiatry. 2020:e201035. doi:10.1001/jamapsychiatry.2020.1035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Brook JS, Rosen Z, Brook DW. The effect of early marijuana use on later anxiety and depressive symptoms. NYS Psychol. 2001;13(1):35–40. [Google Scholar]
- 49. McDonald AJ, Roerecke M, Mann RE. Adolescent cannabis use and risk of mental health problems—the need for newer data. Addiction. 2019;114(10):1889–1890. [DOI] [PubMed] [Google Scholar]
- 50. Marconi A, Di Forti M, Lewis CM, Robin MM, Evangelos V. Meta-analysis of the association between the level of cannabis use and risk of psychosis. Schizophr Bull. 2016;42(5):1262–1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Lev-Ran S, Roerecke M, Le Foll B, George TP, McKenzie K, Rehm J. The association between cannabis use and depression: a systematic review and meta-analysis of longitudinal studies. Psychol Med. 2014;44(4):797–810. [DOI] [PubMed] [Google Scholar]
- 52. Semple DM, McIntosh AM, Lawrie SM. Cannabis as a risk factor for psychosis: systematic review. J Psychopharmacol. 2005;19(2):187–194.15871146 [Google Scholar]
- 53. Turna J, Patterson B, Van Ameringen M. Is cannabis treatment for anxiety, mood, and related disorders ready for prime time? Depress Anxiety. 2017;34(11):1006–1017. [DOI] [PubMed] [Google Scholar]
- 54. Crippa JAS, Derenusson GN, Ferrari TB, et al. Neural basis of anxiolytic effects of cannabidiol (CBD) in generalized social anxiety disorder: a preliminary report. J Psychopharmacol. 2011;25(1):121–130. [DOI] [PubMed] [Google Scholar]
- 55. Russo EB, Burnett A, Hall B, Keith KP. Agonistic properties of cannabidiol at 5-HT1a receptors. Neurochem Res. 2005;30(8):1037–1043. [DOI] [PubMed] [Google Scholar]
- 56. Campos AC, Guimarães FS. Involvement of 5HT1A receptors in the anxiolytic-like effects of cannabidiol injected into the dorsolateral periaqueductal gray of rats. Psychopharmacology (Berl). 2008;199(2):223–230. [DOI] [PubMed] [Google Scholar]
- 57. Guimarães FS, Carobrez AP, De Aguiar JC, Graeff FG. Anxiolytic effect in the elevated plus-maze of the n MDA receptor antagonist Ap7 microinjected into the dorsal periaqueductal grey. Psychopharmacology (Berl). 1991;103:91–94. [DOI] [PubMed] [Google Scholar]
- 58. Esposito G, Scuderi C, Valenza M, et al. Cannabidiol reduces Aβ-induced neuroinflammation and promotes hippocampal neurogenesis through PPARγ involvement. PLoS One. 2011;6(12):e28668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Wolf SA, Bick-Sander A, Fabel K, et al. Cannabinoid receptor CB1 mediates base- line and activity-induced survival of new neurons in adult hippocampal neurogenesis. Cell Commun Signal. 2010;8:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Blessing EM, Steenkamp MM, Manzanares J, Charles RM. Cannabidiol as a potential treatment for anxiety disorders. Neurotherapeutics. 2015;12(4):825–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. White CM. A review of human studies assessing cannabidiol’s (CBD) therapeutic actions and potential. J Clin Pharmacol. 2019;59(7):923–934. [DOI] [PubMed] [Google Scholar]
- 62. ElSohly MA, Mehmedic Z, Foster S, Chandrani G, Suman C, James CC. Changes in cannabis potency over the last 2 decades (1995-2014): analysis of current data in the United States. Biol Psychiatry. 2016;(7):613–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Allott K, Chanen A, Yuen HP. Attrition bias in longitudinal research involving adolescent psychiatric outpatients. J Nerv Ment Dis. 2006;194(12):958–961. [DOI] [PubMed] [Google Scholar]
- 64. Moum T. Mode of administration and interviewer effects in self-reported symptoms of anxiety and depression. Soc Indic Res. 1998;45(1-3):279–318. [Google Scholar]
- 65. Lau J, Ioannidis JP, Terrin N, Christopher HS, Ingram O. The case of the misleading funnel plot. BMJ. 2006;333(7568):597–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, NIH_Study_Quality_Assessment_submission.xlsx-CJP-2020-085-SR.R1 for Cannabis Use and Prospective Long-Term Association with Anxiety: A Systematic Review and Meta-Analysis of Longitudinal Studies: Usage du cannabis et association prospective à long terme avec l’anxiété: une revue systématique et une méta-analyse d’études longitudinales by Siqi Xue, M. Ishrat Husain, Haoyu Zhao and Arun V. Ravindran in The Canadian Journal of Psychiatry