INTRODUCTION
Alcohol is a teratogen, a leading preventable cause of intellectual disability in the U.S., and the cause of fetal alcohol spectrum disorders.1 The prevalence of these disorders ranges from 1.1% to 5.0% among first graders in 4 U.S. communities.2 Alcohol use has been increasing among reproductive-aged women.3 This study investigates increased alcohol use during pregnancy using national data from 2011 to 2018.
METHODS
Data were from the Behavioral Risk Factor Surveillance System (BRFSS) 2011–2018, restricted to self-reported pregnant women aged 18–44 years. BRFSS is a representative, landline/cellular telephone survey of non-institutionalized adults from 50 states and the District of Columbia. The annual median response rate ranged from 45.2% to 49.9%. Pregnancy status was based on responses to: To your knowledge, are you now pregnant? Investigators examined 4 measures of alcohol consumption in the past 30 days: (1) current drinking (at least 1 drink of any alcoholic beverage), (2) binge drinking (4 or more drinks on an occasion), (3) quantity (average number of drinks consumed on the days one drank, among current drinkers), and (4) frequency (number of days having at least 1 drink of any alcoholic beverage, among current drinkers). The authors estimated the weighted age (18–24, 25–29, 30–34, and 35–44 years), ethnicity/ethnicity (White, non-Hispanic; Black, non-Hispanic; Hispanic; and other, non-Hispanic), standardized annual prevalence, and 95% CIs. The standard population weights were based on the age and racial/ethnic distribution of pregnant women in the 2011 BRFSS. This study investigated trends in the annual prevalence of current and binge drinking using logistic regression, and quantity and frequency using linear regression, with drinking pattern as the dependent variable and year, age, and race/ethnicity as the covariates. A p-value<0.05 was considered statistically significant. Analyses were conducted in 2019 with SUDAAN, release 11.0.1.
RESULTS
There were 20,736 pregnant women aged 18–44 for analysis. The weighted age distribution was 29.6% aged 18–24 years, 27.3% aged 25–29 years, 27.1% aged 30–34 years, and 16.0% aged 35–44 years. The weighted racial/ethnic distribution was 51.8% White, non-Hispanic; 13.2% Black, non-Hispanic; 25.2% Hispanic; and 9.7% other, non-Hispanic. The weighted prevalence of current drinking increased significantly from 9.2 (95% CI=7.5, 11.3) in 2011 to 12.9 (95% CI=11.0, 15.2) in 2013, decreased significantly to 8.9 (95% CI=7.2, 11.0) in 2014, and then slightly increased to 11.3 (95% CI=9.1, 13.9) in 2018 (Figure 1). The weighted prevalence of binge drinking increased slightly from 2.5 (95% CI=1.8, 3.6) in 2011 to 3.9 (95% CI=2.9, 5.2) in 2013, decreased significantly to 2.2 (95% CI=1.5, 3.4) in 2014, and then slightly increased to 4.0 (95% CI=2.6, 6.2) in 2018. From 2011 to 2018, trends increased, albeit narrowly, for current drinking (p=0.0497) and binge drinking (p=0.045). The average quantity increased from 2.1 (95% CI=1.8, 2.4) in 2011 to 2.2 (95% CI=1.8, 2.6) in 2018, and the average frequency increased from 5.8 (95% CI=4.4, 7.2) in 2011 to 7.0 (95% CI=5.9, 8.1) in 2018, neither significantly.
Figure 1.
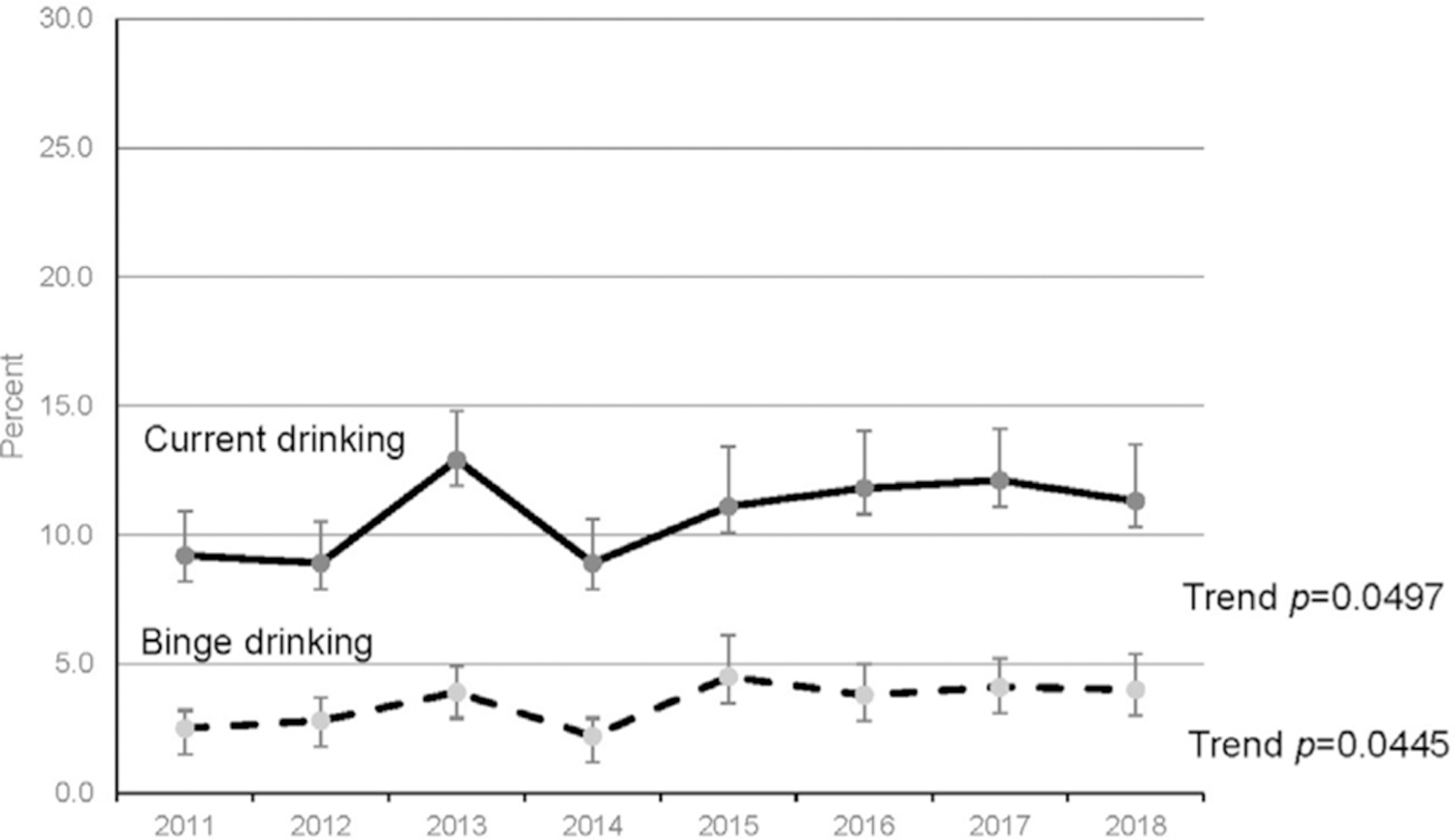
Trends in current drinking and binge drinking among pregnant women, standardized for age and race/ethnicity. Data from the Behavioral Risk Factor Surveillance System, 2011 to 2018. Age and race/ethnicity standardized point estimates and 95% CIs for current drinking (solid line) and binge drinking (dashed line) during pregnancy. Binge drinking estimates for 2014, 2015, and 2018 might be unstable because the relative SEs are 0.2–0.3.
DISCUSSION
During pregnancy, current drinking and binge drinking increased slightly from 2011 to 2018. Assuming 6,000,000 pregnancies in 2018,4 estimates indicate that roughly 678,000 (95% CI=546,000, 834,000) pregnant women drank alcohol, and 240,000 (95% CI=156,000, 372,000) binge drank, in the last 30 days. Binge drinking could increase while average quantity remained level if respondents interpreted average as usual and did not include binge episodes in their average quantity response.5 For example, if in the last 30 days a respondent drinks 1 drink a day for 20 days but has some additional binge drinking episodes on other days, she may only report her average number of drinks per occasion as 1 and exclude the binge drinking episodes. The results are based on self-report and likely underestimate alcohol consumption because of social desirability bias. Underestimation is also likely because some pregnancies were not recognized at the time of the interview, and prevalence of drinking alcohol is highest in the first trimester.6 Estimates may be affected by selection bias because BRFSS excludes institutionalized adults and adults without telephones, and response rates fell precipitously in the 1990s and then plateaued to around 50%.7 Despite clinical recommendations for alcohol screening during pregnancy,8 prevalence of alcohol use in pregnancy is not decreasing. Increased efforts by the public health community and healthcare providers may reduce alcohol consumption during pregnancy.
ACKNOWLEDGMENTS
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
No financial disclosures were reported by the authors of this paper.
REFERENCES
- 1.Stratton K, Howe C, Battaglia F, eds. Fetal Alcohol Syndrome: Diagnosis, Epidemiology, Prevention, and Treatment Washington, DC: National Academy Press, 1996. [Google Scholar]
- 2.May PA, Chambers CD, Kalberg WO, et al. Prevalence of fetal alcohol spectrum disorders in 4 U.S. communities. JAMA 2018;319(5):474–482. 10.1001/jama.2017.21896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.White A, Castle IJ, Chen CM, Shirley M, Roach D, Hingson R. Converging patterns of alcohol use and related outcomes among females and males in the United States, 2002 to 2012. Alcohol Clin Exp Res 2015;39(9):1712–1726. 10.1111/acer.12815. [DOI] [PubMed] [Google Scholar]
- 4.Curtin SC, Abma JC, Ventura SJ, Henshaw SK. Pregnancy rates for U.S. women continue to drop. NCHS Data Brief 2013(136):1–8. https://www.cdc.gov/nchs/products/databriefs/db136.htm. Accessed March 5, 2020. [PubMed] [Google Scholar]
- 5.Alanko T An overview of techniques and problems in the measurement of alcohol consumption. In: Smart RG, Cappell HD, Glaser FB, eds. Research Advances in Alcohol and Drug Problems, 8. Boston, MA: Springer, 1984:209–226. 10.1007/978-1-4613-2719-6_7. [DOI] [Google Scholar]
- 6.Ethen MK, Ramadhani TA, Scheuerle AE, et al. Alcohol consumption by women before and during pregnancy. Matern Child Health J 2009;13(2):274–285. 10.1007/s10995-008-0328-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fahimi M, Link M, Mokdad A, Schwartz DA, Levy P. Tracking chronic disease and risk behavior prevalence as survey participation declines: statistics from the Behavioral Risk Factor Surveillance System and other national surveys. Prev Chronic Dis 2008;5(3):A80. https://www.cdc.gov/pcd/issues/2008/jul/07_0097.htm. Accessed March 6, 2020. [PMC free article] [PubMed] [Google Scholar]
- 8.American College of Obstetricians and Gynecologists. Committee opinion no. 496: at-risk drinking and alcohol dependence: obstetric and gynecological implications. Obstet Gynecol 2011;118(2 Pt 1):383–388. 10.1097/AOG.0b013e31822c9906. [DOI] [PubMed] [Google Scholar]


