Abstract
Background:
Extrapulmonary tuberculosis accounts for only 15% of new cases of tuberculosis. In extrapulmonary tuberculosis, usually affected areas include bone, pleura, lymph nodes, genitourinary system, joints, peritoneum and meninges. Tuberculosis epididymo-orchitis is an uncommon type of extrapulmonary tuberculosis.
Case presentation:
We reported a case of tuberculosis epididymo-orchitis and involvement of the left testicle in a 37-year-old male patient. The left testicle had a heterogeneous parenchymal echo, and multiple hypo-echo and ill-defined areas were evident in the left testicle. In the color Doppler ultrasound, the left testicle with the epididymis on both sides was completely hyperemic. The findings were primarily in the favor of extrapulmonary tuberculosis. Therefore, after a 2-month first-stage treatment with four-drug therapy of anti-TB drugs such as rifampin 150 mg, isoniazid 75 mg, pyrazinamide 400 mg and ethambutol 275 mg, considering the weight of the patient (56 kg), 4 pills per day and the second phase with two-drug therapy, rifampin 150 mg and 75 mg of isoniazid, 4 pills per day for 4 months, extrapulmonary tuberculosis symptoms improved to a large extent.
Conclusion:
To prevent epididymectomy and the effects that the disease may have on fertility, it should be tried to quickly diagnose and treat the disease at the same early stage of the disease.
Key Words: Tuberculosis, Testis, Ultrasound, Treatment
Human tuberculosis caused by Mycobacterium tuberculosis appears in both pulmonary and extrapulmonary forms, the most common form of which is pulmonary tuberculosis, and extrapulmonary tuberculosis accounts for only 15% of new cases of tuberculosis (1, 2). In extrapulmonary tuberculosis, usually affected areas include bone, pleura, lymph nodes, genitourinary system, joints, peritoneum and meninges (3-5). In the meantime, genitourinary tuberculosis is considered as one of the major outcomes of extrapulmonary tuberculosis, with 15% of extrapulmonary tuberculosis. But genital tuberculosis independent from the urinary tract tuberculosis is not very common (2). The most common places affected by the disease in the genitourinary system are prostate, epididymis and seminal vesicles (6) and some cases of tuberculosis in the testicles, which are part of the reproductive system, are very rare and contain a total of 3% of genital tuberculosis (2). Most men aged 20 to 40 have testicular tuberculosis, which may also be accompanied swelling of the testicular sac, with or without discharging sinus and by pain or painless of the testicles. To confirm the diagnosis, ultrasound and fine needle aspiration cytology (FNAC) are used. In elderly people, because testicular malignancies are more common to testicular tuberculosis, it is very difficult to detect testicular tuberculosis in these people; therefore, for the differential diagnosis of testicular tuberculosis with testicular malignancies in the elderly,testicular biopsy is required.
For the treatment of pulmonary and extrapulmonary tuberculosis, the use of anti-TB drugs, such as rifampin, ethambutol, isoniazid, and pyrazinamide, are essential (7).
Case Presentation
The patient was a 37-year-old smoker, who had a six-month job in a hospital mattress and bedroom workshop, where he was exposed to glass wool. He also noted the history of drug addiction, such as crystal, heroin, and opium, which he abandoned them in the past two years. According to the patient's remarks, the patient in the addiction treatment camp contacted a person with tuberculosis, and after a while he suffered from blood-sucking, night sweats, and severe weight loss and did not refer to any health center. After a while, the patient goes to the hospital with complaints of swelling and severe pain in the left testicle as well as mild right testicular involvement. The person was diagnosed by an infectious disease specialist as an extrapulmonary tuberculosis. The patient denies the history of any sexually transmitted diseases and urology. The color Doppler ultrasound of the testicles revealed that the right testicle was 29*27*29 mm in diameter and the testicle on the left measured 23*30*42 mm. The testicle on the right side in terms of the size and parenchymal echo was normal. The left testicle had a heterogeneous parenchymal echo, and multiple hypo-echo and ill-defined areas were evident in the left testicle.
Both sides of the epididymis were larger than normal and the echo was completely heterozygous. In the Color Doppler Ultrasound, the left testicle with the epididymis on both sides was completely hyperemic. There was also a thick and edema scrotal wall (swollen). Image of the collection with approximately 32*23 mm size was observed in the scrotal wall, which was linked through the tract (duct) internal space scrotum. The findings were primarily in the favor of extrapulmonary tuberculosis and there was no evidence of torsion in the testicles. The patient was also negative in terms of hydrocele and varicocele and space mass (fig. 1).
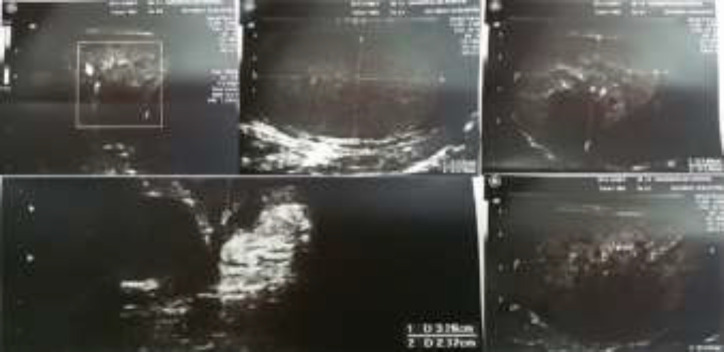
Figure (1).
Ultrasound of left testis showing a heterogeneous parenchymal echo and multiple hypo-echo and ill-defined areas
Also, PCR of the patient's urine was positive for tuberculosis, and in addition, it indicates that the patient is not resistant to anti-tuberculosis drugs. The patient did not have any history of TB treatment. Therefore, after a 2-month first-stage treatment with four-drug therapy of anti-TB drugs such as rifampin 150 mg((8-12)mg/kg), isoniazid 75 mg ((4-6)mg/kg), pyrazinamide 400 mg((20-30) mg/kg) and ethambutol 275 mg((15-20)mg/kg), considering the weight of the patient (56 kg), 4 pills per day and the second phase with two-drug therapy , rifampin 150 mg((8-12)mg/kg) and 75 mg((4-6)mg/kg) of isoniazid, 4 pills per day for 4 months, extrapulmonary tuberculosis symptoms improved to a large extent.
The testicular swelling also decreased with the perforation of the material on both sides and greatly improved. To find other tuberculosis lesions in other parts of the body, the culture, smeared sputum, PPD, and chest x-ray, were performed; the results are as follows: Chest x-ray showed turbidity and systematic changes on the peaks of both lungs with different sizes; these findings, along with changes in bronchiectasis, and the creation of numerous cavities suggested old tuberculosis. The lateral angles of the two sides were open and the size of the heart and mediastinum was normal and the pathologic point was not seen in the chest wall (fig. 2). Patient PPD was 20 mm, and smear three pluses (more than ten acid-fast bacillus in each microscopic field) and patient culture were also positive. Also, with the examination of the patient's relatives, the patient's father developed positive culture. Therefore, the patient had pulmonary TB in addition to extrapulmonary tuberculosis. Laboratory data revealed a white blood cell count of 8100 cells per µl with 60% neutrophil, 35% lymphocyte and 4% monocyte, hemoglobin concentration of 14.7 g/dl, aspartate aminotransferase (AST) 11 U/l, alanine aminotransferase) ALT) 10 U/l, alkaline phosphatase concentration 184.4 U/l, ESR 62 mm after one hour and fasting blood sugar 89 mg/dl. Retroviral screening and Venereal Disease Research Laboratory (VDRL) tests were non-reactive. The urinalysis revealed 4–6 erythrocytes per high-powered field, no seen bacteria and positive protein and glucose was negative.
Figure 2.

Chest x-ray showing turbidity and systematic changes on the peaks of both lungs with different sizes
Discussion
Tuberculosis is a disease caused by Mycobacterium tuberculosis bacillus. About one-third of the world's population has this basil in their body, and about three million patients die every year from this disease. It is considered one of the most important infectious diseases in the world. The emergence of AIDS has caused a significant increase in the disease in the world, especially in African countries (8). Tuberculosis appears in two forms of pulmonary and extrapulmonary (1); in extrapulmonary tuberculosis, one of the places involved in the genitourinary-urinary tract (4), and in genital tuberculosis, the involvement of testicular is rare (6). Testicular tuberculosis is commonly caused by diffuse tuberculosis from other parts of the body, especially the genital tract, and isolated cases of testicular tuberculosis are rare (7). In most cases, epidemic-orchitis is believed to result in the spread of tubercle bacilli in the urinary tract into the prostate, and from there into canalicular, then into seminal vesicles, its pores, and epididymis. Tuberculosis can also spread through the blood and lymph, which is the most common of testicular involvement due to the spread of tuberculosis in the epididymis or the return of the bacillus to the testicles; the cases that spread through the blood are very rare (9, 10).
The involvement of the testicle's wall in our patient indicates the spread of the disease out of the testicle. Genital tuberculosis generally indicate pain, one-sided swelling and discharging sinuses from the testicular sac (7). Ultrasound is very useful for the diagnosis of testicular tuberculosis. The epididymis and testicular involvement with tuberculosis, depending on ultrasound diagnosis, are divided into four types:
1. Extremely large, homogenously hypoechoic
2. Extremely large, heterogeneously hypoechoic
3. Miliary
4. Nodular magnitude, heterogeneously hypoechoic (11).
Lymphoma and seminoma are often homogeneous, but non-seminomal tumors are heterogeneous (12). The use of color Doppler in ultrasound is useful to detect testes tuberculosis from testes torsion. In the testes’ torsion, the blood flow does not reach or decrease in the testes, but in testicular tuberculosis, which can cause testicular inflammation, blood flow to the testes increases (13).
Urinary symptoms and the presence of pus in sterile urine indicate kidney involvement and kidney disease, and no evidence of such a patient has been found in our patient. Tuberculosis epididymo-orchitis can have a major effect on fertility. Mobility and the number of sperms may decrease due to secondary atrophy and duct obstruction (14).
The existence of the abnormal extrapulmonary tuberculosis was correlated with pulmonary tuberculosis in the genital tract of our patient. Also, bilateral involvement from the epididymis led to the dissemination and involvement of the left testicle. Therefore, in the differential diagnosis from scrotal inflation, apart from the acute infection, testicular tumor and inflammation of the orchitis, tuberculosis epididymo-orchitis should be considered (15).
In conclusion, to prevent epididymectomy and the effects that the disease may have on fertility, it should be tried to quickly diagnose and treat the disease at the same early stage of the disease. It is crucial for health centers to pay attention to people who referred to these centers. It also crucial to pay attention to drug addiction camps, glass fiber plants, dairy farms, and other places that can predispose a person to a diagnosis.
Acknowledgments
We would like to thank Ms. Dashtbani for helping us in collecting information.
Conflict of interest:
The authors declare that there is no conflict of interest with this project.
References
- 1.Azizi F, Janghorbani M, Hatami H. Epidemiology and control of common disorders in Iran. 3rd ed. Tehran: Khosravi Publisher ; pp. 2009–898. [in Persian] [Google Scholar]
- 2.Viveiros F, Tente D, Espiridião P, Carvalho A, Duarte R. Testicular tuberculosis: Case report. Revista Portuguesa de Pneumologia. 2009;15:1193–7. doi: 10.1016/s0873-2159(15)30201-4. [DOI] [PubMed] [Google Scholar]
- 3.Fitzgerald D, Sterling T, Haas D. Mycobacterium tuberculosis. In: Mandell G, Bennett J, Raphael D, editors. Principles and practice of infectious disease. 5th ed. London: Churchill Livingstone ; 2000. pp. 2575–607. [Google Scholar]
- 4.Özbay B, Uzun K. Extrapulmonary tuberculosis in high prevalence of tuberculosis and low prevalence of HIV. Clinics Chest Med. 2002;23:351–4. doi: 10.1016/s0272-5231(02)00002-3. [DOI] [PubMed] [Google Scholar]
- 5.Raviglone M, Obrein R. Tuberclusis. In: Kasper D, Harrison T, Braunwald E, et al., editors. Harison principeles of internal medicine. 16th ed. New York: McGraw-Hill ; 2005. pp. 953–86. [Google Scholar]
- 6.Das P, Ahuja A, Gupta SD. Incidence, etiopathogenesis and pathological aspects of genitourinary tuberculosis in India: A journey revisited. Indian J Urol. 2008;24:356–61. doi: 10.4103/0970-1591.42618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Das A, Batabyal S, Bhattacharjee S, Sengupta A. A rare case of isolated testicular tuberculosis and review of literature. J Fam Med Prim Care. 2016;5:468–70. doi: 10.4103/2249-4863.192334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kumar V, Abbas AK, Fausto N, Aster JC. Robbins and Cotran pathologic basis of disease. 8th ed. Philadelphia: WB Saunders Co; 2007. p. 1464. [Google Scholar]
- 9.Viswaroop B, Kekre N, Gopalakrishnan G. Isolated tuberculous epididymitis: A review of forty cases. J Postgrad Med. 2005;51:109–11. [PubMed] [Google Scholar]
- 10.Wise GJ, Shteynshlyuger A. An update on lower urinary tract tuberculosis. Curr Urol Rep. 2008;9:305–13. doi: 10.1007/s11934-008-0053-9. [DOI] [PubMed] [Google Scholar]
- 11.Muttarak M, Peh WC, Lojanapiwat B, Chaiwun B. Tuberculous epididymitis and epididymo-orchitis: sonographic appearances. Am J Roentgenol. 2001;176:1459–66. doi: 10.2214/ajr.176.6.1761459. [DOI] [PubMed] [Google Scholar]
- 12.Muttarak M, Peh WC. Case 91: tuberculous epididymo-orchitis. Radiology. 2006;238:748–51. doi: 10.1148/radiol.2382031851. [DOI] [PubMed] [Google Scholar]
- 13.Pavlica P, Barozzi L. Imaging of the acute scrotum. Eur Radiol. 2001;11:220–8. doi: 10.1007/s003300000604. [DOI] [PubMed] [Google Scholar]
- 14.Al-Ghazo MA, Bani-Hani KE, Amarin ZO. Tuberculous epididymitis and fertility in North Jordan. Saudi Med J. 2005;26:1212–5. [PubMed] [Google Scholar]
- 15.Kundu S, Sengupta A, Dey A, Thakur SB. Testicular tuberculosis mimicking testicular malignancy. J Indian Med Assoc. 2003;101:204–5. [PubMed] [Google Scholar]