Abstract
Background:
There has been a considerable development in the clinometric of stroke. But researchers are concerned that some scales are too generic, inherently and the insight may not be provided. The current study was conducted to determine which scale or scales should be used in stroke survivors.
Methods:
We selected 67 studies which were published between January 2010 and December 2018 from Up to date, CINAHL, ProQuest, Scopus, PubMed, Embase, Medline, Elsevier and Web of Science with MeSH terms. Inclusion criteria were: clinical trials, prospective studies, retrospective cohort studies, or cross-sectional studies; original research in adult human stroke survivors. We excluded the following articles: non-adult population; highly selected studies or treatment studies without incidence data; commentaries, single case reports, review article, editorials and non-English articles or articles without full text available.
Results:
Face Arm Speech Test and Cincinnati Pre-Hospital Stroke Scale scales because it was easy to learn and rapidly administer the recommended dose to use in pre-hospital, but there are not gold standard in stroke diagnosis in Pre-Hospital. National Institutes of Health Stroke Scale valuable in the acute stage for middle cerebral artery, not chronic or long term post stroke outcome. The Barthel Index scores for approximately three weeks could predict activities of daily living disabilities in 6 months.
Conclusion:
Every scale has an advantage and a disadvantage and we were not able to introduce the gold standard for each item, but some special scales were used more in the studies, preferred for comparing with other studies to match the research results.
Key Words: Stroke disability, Stroke scale, Quality of life
There has been a considerable development in the clinometric of stroke since the 1980s. No single scale is suitable for all clinical or research situations although there are many general and stroke-specific scales that have established reliability and validity (1). A large number of stroke scales are described. Despite a considerable interest research, it does not have a considerable impact that can be related to internal or external validity (quality of research and generalizability of results). Furthermore, too complex perception or too large required information are not routinely available. Researchers are concerned that some scales are too generic inherently and the insight may not be provided. Also, result showed that independent validation studies are lacking for many scales (2). This review aimed to assess the stroke scales that were used for the assessment, diagnosis, disability, handicap and quality of life. This review would be beneficial to healthcare providers and researchers in their clinical diagnosis and management of stroke. The review question was which scale should be used for stroke patients in assessment, diagnosis, disability, handicap and quality of life?
Method
Search strategy: We selected 67 studies which were published between January 2010 and December 2018. Relevant literature was identified as follows: pertinent articles in the following electronic databases: Up to date, CINAHL, ProQuest, Scopus, PubMed, Embase, Medline, Elsevier and Web of Science; We developed search strategies using keywords and MeSH terms including scale, stroke, cerebrovascular accident, disability, handicap, impairment and quality of life. The abstract of each article was carefully reviewed to detect appropriate publication; full-text articles were retrieved and read carefully, including all reference lists of all relevant articles to identify additional eligible publications; and references from previously retrieved articles and all eligible studies were also searched manually (table 1). Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidance were used (3). Table 1 indicates study search strategy with PICO model (P: Problem, Patient or Population, I: Intervention, C: Comparison, control or comparator and O: Outcome (s)).
Table 1.
Study search strategy with picos mdel
| PICOS | definition |
|---|---|
| P | (‘Stroke’ OR ‘Cerebral Stroke’ OR ‘Vascular Accident, Brain’ OR ‘CVA’ OR ‘Cerebrovascular accident’ OR ‘Cerebrovascular Accident, Acute‘ Cerebrovascular Stroke’ OR ‘Stroke, sub-acute’ OR ‘Stroke, Acute’ OR ‘Stroke, chronic’) |
| I | (‘Face Arm Speech Test’ OR ‘Cincinnati Prehospital Stroke Scale’ OR ‘stroke car’ OR ’Los Angeles Prehospital Stroke Screen’ OR ’Los Angeles Motor Scale ’OR’ Prehospital Acute Stroke Severity scale ’OR’ The Finnish Prehospital Stroke Scale’ OR’ Recognition of Stroke in the Emergency Room’ OR’ Guangzhou Stroke Scale’ OR’ Rapid Arterial Occlusion Evaluation scale’ OR’ National Institutes of Health Stroke Scale’ OR’ Pediatric National Institutes of Health Stroke Scale’ OR’ European Stroke Scale’ OR ’Canadian Neurologic Scale’ OR ’The Scandinavian Stroke Scale’ OR’ Barthel Index’ OR ’Functional Independence Measure’ OR ’Instrumental Activities of Daily Living’ OR ’Modified Rankin Scale ’OR ’Rankin Focused Assessment’ OR ’Sickness Impact Profile’ OR ’Short Form 36 ’OR ’European Quality of Life Score ’ OR ’Quality of Life after Stroke Scale’ OR ’Stroke Impact Scale’ OR ’Stroke-Specific Quality of Life Scale’) |
| C | (‘pre-hospital’ OR ‘emergency’ OR ‘rehabilitation unit’ OR ‘stroke care unit’ |
| O | (diagnose OR ‘impairment’ ‘handicap’ OR ‘disability’ OR ‘quality of life ) |
| S | (‘cohort analysis’ OR ‘intervention study’ OR ‘longitudinal study’ OR ‘cluster analysis’ OR ‘crossover trial’ OR ‘cluster analysis’ OR ‘randomized trial’ OR ‘major clinical study’)/de OR (longitudinal OR cohort OR crossover trial OR cluster analysis OR randomized trial OR clinical trial OR controlled trial) |
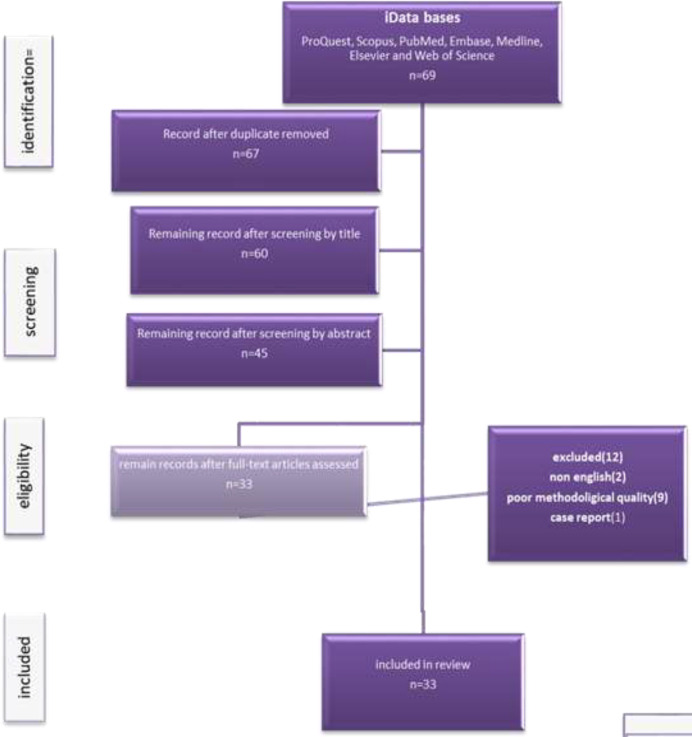
Inclusion: Definition of scale was according to the Drozdowska’s study (2). So, studies were included if they utilized one scale or compared different disability scales in stroke patients. Inclusion criteria were: clinical trials, prospective studies, retrospective cohort studies, or cross-sectional studies; original research in adult human stroke survivors; the eligibility of scale was reported in the study; the study population had episodes of total stroke, ischemic, or hemorrhagic stroke. The study selection process is depicted diagrammatically in fig. 1.
Figure 1.
Flow diagram of literature research and study selection process
Exclusion: We excluded the following articles: non adult population; highly selected studies or treatment studies without incidence data; commentaries, single case reports, review article, editorials and non-English articles or articles without full text available.
Data extraction and quality assessment: Descriptive data (first author and year of publication; place of study, study patients, scale and type of instrument, and result of study) extracted from each study. Then, two authors (Alijanpour and Mostafazadeh-Bora) confirmed the studies by reading each article carefully, extracting the data independently, and cross-checking the information. Any disagreement was discussed until a consensus was reached. A reviewer (Ahmadi Ahangar) was consulted if disagreement persisted.
Findings: in the section, we explain articles that assess stroke scale. All of stroke scale are listed in table 2. Also, studied articles are listed in table 3.
Table 2.
Category and sub category of stroke scale with different items
| Cut point | Grading | item | Authors | scale | Category |
|---|---|---|---|---|---|
| Facial drooping, Arm weakness, Speech difficulties and Time to call emergency services | Joseph Harbison et al. | FAST | DIAGNOSTIC SCALES | ||
| Normal: Both sides of face move equally. Abnormal: One side of face does not move as well as the other. |
Facial Droop | National Institutes of Health Stroke Scale | CPSS | ||
| Normal: Both arms move the same, or both arms do not move at all. Abnormal: One arm either does not move, or one arm drifts down compared to the other. | Arm Drift | ||||
| Normal: The patient says correct words with no slurring of words. Abnormal: The patient slurs words, says the wrong words, or is unable to speak |
Speech | ||||
| Positive answers to all 6 questions above: Contact hospital en-route Alert hospital of possible stroke patient Test Sensitivity: 93% Test Specificity: 97% |
Yes, No, unknown | Age over 45 years | Department of Health Services, County of Los Angeles | LAPSS | |
| Yes, No, unknown | History of seizures or epilepsy absent | ||||
| Yes, No, unknown | Symptom duration less than 24 hours | ||||
| Yes, No, unknown | At baseline, patientis not wheelchairbound or bedridden | ||||
| Yes, No | Blood glucose between 60 and 400 | ||||
| Facial droop, Grip weakness or absence, Arm weakness | Exam: Look for obvious asymmetry Based on exam | ||||
| A score ≥4 is highly predicted of large artery occlusion | Absent (0) Present (1) |
Facial Droop | Jeffrey Saber et al | LAMS | |
| Absent (0) Drifts down (1) Falls rapidly (2) |
Arm Drift | ||||
| Absent (0) Weak grip (1) No Grip (2) |
Grip Strength | ||||
| PASS ≥2 | Yes No |
level of consciousness (month/age), | Somerville et al | PASS | |
| Yes No |
gaze palsy/deviation | ||||
| Yes No |
arm weakness | ||||
| ≥5 predicts LVO | Facial droop (1) | Face | Ollikainen et al(10) | FPSS | |
| Weakness of 1 or more extremities (1) | Extremity | ||||
| Difficulty of understanding or producing speech, including slurring (1) |
Speech | ||||
| Field cut or blindness (1) | Vision | ||||
| Partial or fixed gaze or head deviation away from the paretic side (4) | Gaze | ||||
| If total score > 0 (1 to 6) a diagnosis of acute stroke is likely. If total scores 0, -1 or -2 stroke unlikely but is not excluded and patient should be discussed with the stroke team. DECT phone 21616 – Stroke Specialist Nurse 9-5. Medical SpR – Out of hours. |
Yea (-1), no (0) | LOC/syncope | Azlisham Mohd Nor | ROSIER | |
| Yea (-1), no (0) | Seizure activity | ||||
| Yea (+1), no (0) | Asymmetric facial weakness | ||||
| Yea (+1), no (0) | Asymmetric arm weakness | ||||
| Yea (+1), no (0) | Asymmetric leg weakness | ||||
| Yea (+1), no (0) | Speech disturbance | ||||
| Yea (+1), no (0) | Visual field defect | ||||
| Alert (or awakens easily and stays awake) (0) Drowsy (Responds to minor stim. but falls back asleep) (1) Obtunded (Responds only to deep pain or vigorous stim) (2) Comatose (No response) (3) |
Level of Consciousness (LOC) | Patrick D. Lyden | NIHSS | IMPAIRMENT | |
| Mild 1-5 Mild to moderate severe 5-14 Severe 15-24 Very severe ˃25 |
Both questions answered correctly (0) One question answered correctly (1) Neither question answered correctly (2) |
LOC- Questions Month? Age? | |||
| Both commands performed correctly (0) One command performed correctly (1) Neither command performed correctly (2) |
LOC– Commands Opens/closes eyes Opens/closes hands | ||||
| Normal (0) Mild gaze paralysis (can bring eyes only over to midline) (1) Complete gaze paralysis (deviated & unable to bring eyes over) (2) |
Eye Movements: Horizontal eye movements | ||||
| Normal (0) Partial hemianopia (upper OR lower quadrant) (1) Complete hemianopia (upper AND lower quadrants) (2) Bilateral hemianopia (total blindness) (3) |
Visual fields: Sees objects in Four quadrants | ||||
| Normal (0) Minor paralysis (flattening of nasolabial folds) (1) Partial paralysis (near or total paralysis lower face) (2) Complete paralysis (Of upper and lower face) (3) |
Facial: Facial movements | ||||
| Normal (No drift at all) (0) Drift (Drifts downward but NOT to bed before 10 sec.) (1) Drifts to bed within 10 sec (2) Movement, but not against gravity (3) Complete paralysis (No movement at all) (4) Amputation or joint fusion (N/A) |
Motor – Left Arm Hold arm straight out from chest | ||||
| Normal (No drift at all) (0) Drift (Drifts downward but NOT to bed before 10 sec.) (1) Drifts to bed within 10 sec (2) Movement, but not against gravity (3) Complete paralysis (No movement at all) (4) Amputation or joint fusion (N/A) |
Motor – Right Arm Hold arm straight out from chest | ||||
| Normal (No drift at all) (0) Drift (Drifts downward but NOT to bed before 10 sec.) (1) Drifts to bed within 10 sec (2) Movement, but not against gravity (3) Complete paralysis (No movement at all) (4) Amputation or joint fusion (N/A) |
Motor – Left leg Keep leg off bed | ||||
| Normal (No drift at all) (0) Drift (Drifts downward but NOT to bed before 10 sec.) (1) Drifts to bed within 10 sec (2) Movement, but not against gravity (3) Complete paralysis (No movement at all) (4) Amputation or joint fusion (N/A) |
Motor – Right leg Keep leg off bed | ||||
| Absent (no ataxia, OR pt cannot move arm/leg) (0) Presentinonelimb (1) Present in two or more limbs (2) (is absent if patient cannot understand or is too weak to do) |
Limb Ataxia Finger-Nose Heel-Knee-Shin | ||||
| Normal,nosensoryloss (0) Mildtomoderaeloss (1) Severe to total sensory loss (unaware of being touched) (2) |
Sensory Hemisensory loss: (Test on face, arm & thigh) | ||||
| Normal ability use words and follow commands (0) Mild to Moderate (Repeats / names with some difficulty) (1) Severe Aphasia (very few words correct or understood) (2) Mute (no ability to speak or understand at all (3) |
Language/Aphasia Repetition & Comprehension “Today is a bright sunny day” | ||||
| Normal (0) Mild to moderate slurred speech (some or most) (1) Severe (unintelligible - none understandable) (2) Intubated or other physical barrier (N/A) |
Dysarthria (slurred) Speech clarity (slurring | ||||
| No abnormality (0) Mild (either visual or tactile – partial neglect) (1) Profound (Visual and tactile – complete neglect) (2) |
Neglect Ignores touch or vision to one side | ||||
| 3 grade | Level of Consciousness | Ichord RN (16) | pedNIHSS | ||
| 3 grade | LOC Questions | ||||
| 3 grade | LOC Commands | ||||
| 3 grade | Best Gaze | ||||
| 4 grade | Visual | ||||
| 4 grade | Facial Palsy | ||||
| 6 grade | Motor Arm and Leg | ||||
| 3 grade | Limb Ataxia | ||||
| 3 grade | Sensory | ||||
| 4 grade | Best Language | ||||
| 6 grade | Level of consciousness | Hantson et al (30) | European Stroke Scale | ||
| 3 grade | Comprehension | ||||
| 5 grade | Speech | ||||
| 2 grade | visual field | ||||
| 4 grade | Gaze | ||||
| 3 grade | Facial movement | ||||
| 5 grade | Arm position, maintain | ||||
| 5 grade | Arm raising | ||||
| 5 grade | Wrist extension | ||||
| 3 grade | Finger strength | ||||
| 4 grade | Leg position, maintain | ||||
| 5 grade | Leg flexing | ||||
| 5 grade | Foot dorslflexion | ||||
| 6 grade | Gait | ||||
| Alert (3), Drowsy (1.5) | LEVEL CONSCIOUSNESS: | Cote et al | CNS | ||
| Oriented (1) Disoriented or Non Applicable (0) |
ORIENTATION | ||||
| Normal (1) Expressive Deficit (0.5) Receptive Deficit (0) |
SPEECH | ||||
| None (5) Present (0) |
FACE WEAKNESS | ||||
| None (1.5) Mild (1) Significant (5) Total (0) |
ARM:PROXIMAL WEAKNESS | ||||
| None (1.5) Mild (1) Significant (0.5) Total (0) |
ARM:DISTAL WEAKNESS | ||||
| None (1.5) Mild (1) Significant (0.5) Total (0) |
LEG WEAKNESS | ||||
| Symmetrical (5) Asymmetrical (0) |
FACE | ||||
| Equal (1.5) Unequal (0) |
ARM | ||||
| Equal (1.5) Unequal (0) |
LEG | ||||
| score 2–6 | consciousness | Askim et al (17) | Scandinavian Stroke Scale | ||
| score 0–4 | eye movement | ||||
| score 0–6 | arm motor power | ||||
| score 0–6 | hand motor power | ||||
| score 0–6 | leg motor power | ||||
| score 0–6 | orientation | ||||
| score 0–10 | speech | ||||
| score 0–2 | facial palsy | ||||
| score 0–12 | gait | ||||
| Unable to perform task (0) needs assistance (0) Fully independent (5) |
Personal hygiene | Mahoney et al (31) | BI | ||
| Unable to perform task (0) needs assistance (0) Fully independent (5) |
Bathing self | ||||
| Unable to perform task (0) needs assistance (5) Fully independent (10) |
Feeding | ||||
| Unable to perform task (0) needs assistance (5) Fully independent (10) |
Toilet | ||||
| Unable to perform task (0) needs assistance (5) Fully independent (10) |
Stair climbing | ||||
| Unable to perform task (0) needs assistance (5) Fully independent (10) |
Dressing | ||||
| Unable to perform task (0) needs assistance (5) Fully independent (10) |
Bowel control | ||||
| Unable to perform task (0) needs assistance (5) Fully independent (10) |
Bladder control | ||||
| Unable to perform task (0) needs assistance (5-10) Fully independent (15) |
Ambulation | ||||
| Unable to perform task (0) needs assistance (0) Fully independent (5) |
Wheelchair (when unable to walk.) | ||||
| unable to perform task (0) needs assistance (5-10) Fully independent (15) |
Chair/bed transfers | ||||
| 7-ordinal scale Total assistance (complete dependence) to complete independence |
Eating, grooming, bathing, upper body dressing, lower body dressing, toileting, bladder management, bowel management, bed to chair transfer, toilet transfer, shower transfer, locomotion (ambulatory or wheelchair level), stairs, cognitive comprehension, expersion, social interaction, problem solving, memory | Chumney et al (32) | FIM | ||
| a summary score from 0 (low functioning) to 8 (high functioning) | Operates telephone on own initiative; looks up and dials numbers, Dials a few well-known numbers, Answers telephone, but does not dial (1) Does not use telephone at all (0) |
Ability to Use Telephone | Lawton et al (33) | IADL | |
| Takes care of all shopping needs independently (1) Shops independently for small purchases, Needs to be accompanied on any shopping trip, Completely unable to shop (0) |
Shopping | ||||
| Plans, prepares, and serves adequate meals independently (1) Prepares adequate meals if supplied with ingredients, Heats and serves prepared meals or prepares meals but does not maintain adequate diet, Needs to have meals prepared and served (0) |
Food Preparation | ||||
| Maintains house alone with occasion assistance (heavy work) (1) Performs light daily tasks such as dishwashing, bed making (1) Performs light daily tasks, but cannot maintain acceptable level of cleanliness (1) Needs help with all home maintenance tasks (1) Does not participate in any housekeeping tasks (0) |
Housekeeping | ||||
| Does personal laundry completely (1) Launders small items, rinses socks, stockings, etc (1) All laundry must be done by others (0) |
Laundry | ||||
| Travels independently on public transportation or drives own car (1) Arranges own travel via taxi, but does not otherwise use public transportation (1) Travels on public transportation when assisted or accompanied by another (1) Travel limited to taxi or automobile with assistance of another (0) Does not travel at all (0) |
Mode of Transportation | ||||
| Is responsible for taking medication in correct dosages at correct time (1) Takes responsibility if medication is prepared in advance in separate dosages (0) Is not capable of dispensing own medication (0) |
Responsibility for Own Medications | ||||
| Manages financial matters independently (budgets, writes checks, pays rent and bills, goes to bank); collects and keeps track of income (1) Manages day-to-day purchases, but needs help with banking, major purchases, etc (1) Incapable of handling money (0) |
Ability to Handle Finances | ||||
| 0 | No symptoms at all | John van Swieten et al | mRS | HANDICAP | |
| 1 | No significant disability despite symptoms; able to carry out all usual duties and activities | ||||
| 2 | Slight disability; unable to carry out all previous activities, but able to look after own affairs without assistance | ||||
| 3 | Moderate disability; requiring some help, but able to walk without assistance | ||||
| 4 | Moderately severe disability; unable to walk without assistance and unable to attend to own bodily needs without assistance | ||||
| 5 | Severe disability; bedridden, incontinent and requiring constant nursing care and attention | ||||
| 6 | Dead | ||||
| Yes, no 5 |
Is the person bedridden? The patient is unable to walk even with another person’s assistance. May frequently be incontinent. May require constant care | Patel et al(20) | Rankin Focused Assessment | ||
| Yes, no 4 |
Is another person’s assistance essential for walking? | ||||
| Yes, no 3 |
Assistance to look after own affairs (5 question) | ||||
| Yes, no 2 |
USUAL DUTIES AND ACTIVITIES (4 questions) | ||||
| SPONTANEOUSLY REPORTED SYMPTOMS SYMPTOM CHECKLIST (8question) yes , no 1 |
SYMPTOMS AS A RESULT OF THESTROKE (2 category) | ||||
| 0 | Handicap None (life style none) | Perel et al (34) | Oxford Handicap Scale | ||
| 1 | Minor symptom ( no interference) | ||||
| 2 | Minor handicap (some restrictions but able to look after self) | ||||
| 3 | Moderate handicap (significant restrictions, unable to lead a totally independent existence ---require some assistance) | ||||
| 4 | Moderate to severe handicap handicap (unable to live independently but does not require constant attention) | ||||
| 5 | Severe handicap (totally dependent, require constant attention day and night | ||||
| Penson D.F and Wei J.T (35) | HRQOL | QUALITY OF LIFE | |||
| Yes or no | Body Care and Movement (23) | Bergner et al (36) | Sickness Impact Profile | ||
| Ambulation (12) | |||||
| Mobility (10) | |||||
| Social interaction (20) | |||||
| Sleep and rest (7) | |||||
| Work (9) | |||||
| Recreation and pastimes (8) | |||||
| Eating (9) | |||||
| Home Management (10) | |||||
| Emotional Behavior (9) | |||||
| Alterness Behavior (10) | |||||
| Communication (9) | |||||
| Vitality (4) | Jenkinson C (37) | SF36 | |||
| Physical functioning (10) | |||||
| Bodily pain (2) | |||||
| General health perceptions (5) | |||||
| Physical role functioning (4) | |||||
| Emotional role functioning (3) | |||||
| Social role functioning (2) | |||||
| Mental health | |||||
| 6 grade | Vision | Horsman J et al (38) | Health Utilities Index | ||
| 6 grade | Hearing | ||||
| 5 grade | Speech | ||||
| 6 grade | Ambulation | ||||
| 6 grade | Dexterity | ||||
| 5 grade | Emotion | ||||
| 6 grade | Cognition | ||||
| 5 grade | Pain | ||||
| mobility | Brooks R (39) | EuroQol | |||
| self-care | |||||
| usual activities | |||||
| pain/discomfort | |||||
| anxiety/depression | |||||
| A lot of strength (5) Quite a bit of strength (4) Some strength (3) A little strength (2) No strength at all (1) |
physical problems (4 questions) | Duncan PW (40) | SIS | ||
| Not difficult at all (5) A little difficult (4) Somewhat difficult (3) Very difficult (2) Extremely difficult (1) |
memory and thinking (7 questions) | ||||
| None of the time (5) A little of the time (4) Some of the time (3) Most of the time (2) All of the time (1) |
mood, and emotions (9 questions) | ||||
| Not difficult at all (5) A little difficult (4) Somewhat difficult (3) Very difficult (2) Extremely difficult (1) |
ability to communicate with other people, as well as your ability to understand what you read (7 questions) | ||||
| Not difficult at all (5) A little difficult (4) Somewhat difficult (3) Very difficult (2) Could not do at all (1) |
Activities (10 questions) | ||||
| Not difficult at all (5) A little difficult (4) Somewhat difficult (3) Very difficult (2) Could not do at all (1) |
ability to be mobile,at home and in the community (9 questions) | ||||
| Not difficult at all (5) A little difficult (4) Somewhat difficult (3) Very difficult (2) Could not do at all (1) |
ability to use your hand that was MOST AFFECTED by your stroke (5 questions) | ||||
| None of the time (5) A little of the time (4) Some of the time (3) Most of the time (2) All of the time (1) |
ability to participate in the activities that you usually do, things that are meaningful to you, and help you to find purpose in life (8 questions) | ||||
| Total help - Couldn't do it at all - Strongly agree (1) A lot of help - A lot of trouble - Moderately agree (2) Some help - Some trouble - Neither agree nor disagree (3) A little help - A little trouble - Moderately disagree (4) No help needed - No trouble at all - Strongly disagree (5) |
Energy(3) | SS-QoL | |||
| Family Roles (3) | |||||
| Language (5) | |||||
| Mobility (6) | |||||
| Mood (5) | |||||
| Personality (3) | |||||
| Self-Care (5) | |||||
| Social Roles (5) | |||||
| Thinking (3) | |||||
| Upper Extremity Function (5) | |||||
| Vision (3) | |||||
| Work/Productivity (3) |
*Abbreviations: FAST: Face Arm Speech Test, CPSS: Cincinnati Prehospital Stroke Scale, LAPSS: Los Angeles Prehospital Stroke Screen, LAMS: Los Angeles Motor Scale, PASS: Prehospital Acute Stroke
Severity scale, FPSS: The Finnish Prehospital Stroke Scale, ROSIER: Recognition of Stroke in the Emergency Room, SIS :Stroke Impact Scale and SS-QoL: Stroke-Specific Quality of Life Scale
**HRQOL, SF36, Health Utilities Index, EuroQol considered as general quality of life scale. SIS, Stroke-Specific Quality of Life Scale and Stroke-Specific Quality of Life Scale considered as specific Quality of Life Scale.
Table 3.
Different studies for determining validity of stroke scales
| Author, years | Contrary | Aim | Sampling | Studied scale | Sensitivity and Specificity |
|---|---|---|---|---|---|
| Hastrup et al, 2016 | Australia | the development and validation of PASS scale, for prediction of ELVO |
intravenous tPA clients in Denmark | PASS vs. other scale For emergent large vessel occlusion (ELVO) |
Derivation: Sensitivity 0.66 Specificity 0.83 Validation: Sensitivity 0.61 Specificity 0.83 |
| McArthur et al,2013 | UK | reliability of proxy-derived mRS | 97 stroke clients | proxy-derived mRS | Interobserver variability for standard mRS for stroke survivors: moderate k = 0·48, kw = 0·70; comparing paired raters scores, 67% matched. Reliability for proxy mRS: fair k = 0·37, kw = 0·62, 50% matched. |
| Noorian et al, 2018 | USA | validate the LAMS for LVO | 94 Acute cerebral ischemia patients | LAMS and NIHSS | LVO Among All Cerebral Ischemia: Sensitivity: 0.76 Specificity: 0.65 CSC Among All Suspected Stroke Transports: Sensitivity: 0.73 Specificity: 0.71 |
| Reznik et al, 2018 | USA | NIHSS scores and post-stroke functional outcome | 1183 ischemic stroke clients | Baseline NIHSS 24-h NIHSS Discharge NIHSS mRS at three months |
Baseline NIHSS scores are inferior to 24 h and discharge scores in predicting post-stroke functional outcomes, especially in patients receiving mechanical thrombectomy |
| Olivato et al, 2016 | Italy | the assessed the new version of NIHSS, the e-NIHSS | 22 patients with suspected vertebrobasilar stroke vs. 25 patients with anterior circulation stroke | NIHSS e-NIHSS |
Patients with POCI evaluated with e-NIHSS had an average score of 2 points higher than patients evaluated with classical NIHSS(significant) The e-NHISS could improve the sensibility of NIHSS on posterior circulation stroke and has an impact on clinical and therapeutic trials, as well as on outcomes of posterior strokes |
| Kerber et al, 2012 | Michigan | assess the validity of this scale in a biethnic ischemic stroke population | The study cohort comprised 45 patients with ischemic stroke, 56% female and 51% Mexican American |
The 12-item Stroke-Specific Quality of Life Scale (SSQOL) the original 49-item SSQOL |
The mean score for the 49-item scale: 3.33 ± 0.84, 3.31 ± 0.95 for the 12-item scale. Internal consistency of 49-item scale: 0.96 Internal consistency of 12-item scale: 0.88 The 2 scales were highly correlated (intraclass correlation coefficient, 0.98; R2 5 0.97). |
| Peters et al, 2015 | Ohio | Validity of the NIHSS vs. SIS | 147 Chronic Hemiparetic Stroke | NIHSS SIS |
There was no association between total NIHSS scores and SIS physical dimension scores, SIS overall perception of recovery scores, and SIS ADL/IADL scores. |
| Choi et al, 2017 | NIHSS and functional outcomes at 3 months after mild stroke | 2209 acute ischemic stroke patients with who presented within 4.5 hours of symptom onset and had baseline NIHSS scores less than or equal to 5. | NIHSS MRS |
Of the 15 items of the NIHSS, all except item 8 (sensory) and item 11(extinction) were significantly associated with unfavorable functional outcomes in bivariate analysis (P’s < .05). | |
| Mao et al, 2016 | China | to develop and validate a new stroke recognition instrument in an emergency setting | 416 suspected stroke patients | Guangzhou Stroke Scale (GZSS) ROSIER FAST LAPSS |
ROSIER: Sensitivity: 77.7 Specificity:70.7 Diagnostic accuracy: 76.68 FAST: Sensitivity: 76 Specificity:63.8 Diagnostic accuracy: 74.28 LAPSS: Sensitivity: 56.4 Specificity:87.9 Diagnostic accuracy: 60.82 GZSS: Sensitivity: 83.2 Specificity:74.1 Diagnostic accuracy: 81.97 |
| Kim et al, 2016 | Korea | To assess the validity of the LAMS | 1632 acute cerebrovascular disease patients | LAMS scores NIHSS scores |
the LAMS showed good to excellent convergent, divergent, and predictive validity |
| Askim et al, 2016 | Norway | identifying patients who are dead or dependent at 3-month follow-up by the SSS vs. NIHSS | 104 patients | NIHSS SSS (mRS) >2 |
SSS: Sensitivity: 69.5 Specificity: 82.2 NIHSS: Sensitivity: 64.4 Specificity: 80 |
| English et al, 2017 | Minnesota | to design an effective prehospital notification system | 130 patients | CPSS emergency medical services (EMS) impression NIHSS |
EMS impression: Sensitivity: 77.1 Specificity: 14.7 CPSS: ≥1: Sensitivity: 75 Specificity: 20.6 ≥2: Sensitivity: 58.3 Specificity: 55.9 3: Sensitivity: 32.3 Specificity: 94.1 EMS impression and CPSS: ≥1: Sensitivity: 85.1 Specificity: 17.2 ≥2: Sensitivity: 68.9 Specificity: 51.7 3: Sensitivity: 39.2 Specificity: 93.1 |
| Maddali et al, 2018 | India | to validate the CPSS in the prehospital setting by correlating with computed tomography scan findings. | 66 suspected stroke patients | CPSS | CPSS showed good sensitivity of 81% (confidence interval [CI] – 68.5%–97%) when combined and a positive predictive value (PPV) of 100% (CI: 91.9%–100%). Individually, they showed a sensitivity of 75.8%, 79%, and 74.1%, respectively, with a PPV of 100% and specificity of 95%–100%. |
| Ollikainen et al, 2018 | Finland | releasing the rest of the score items to assist in non- LVO stroke recognition. |
856 prehospital Code Stroke | the Finnish Prehospital Stroke Scale (FPSS) NIHSS-8 3I-SS C-STAT PASS FAST-ED |
FPSS: Sensitivity:54.3 Specificity: 91.2 NIHSS-8: Sensitivity: 62.6 Specificity: 88.7 3I-SS: Sensitivity: 41.8 Specificity: 92.7 C-STAT: Sensitivity: 54.0 Specificity: 90,5 PASS: Sensitivity: 68.5 Specificity: 85.4 FAST-ED: Sensitivity: 61.6 Specificity: 84.2 |
| MacIsaac et al, 2016 | United Kingdom | validated the SF-SIS | 5549 acute study patients | short form SIS original SIS |
SF-SIS demonstrated content, convergent, and discriminant validity |
| Nakao et al, 2010 | Japan | To clarify the threshold of acute BI for use in the prediction ADL | 78 patient out of 191 inpatient admitted with acute stroke | BI ADL |
patient with an early BI score ≥40: partially independent in their ADL at 6 months except for grooming, bathing, and stair climbing, implaying. two-theirds in patients with a BI score ≤40: a possibility of being partially independent in their ADL. |
| Kerber et al, 2012 | USA | to assess the validity 12-item SSQOL | Of the 45 ischemic stroke patients | 12-item SSQOL | Internal consistency was0.96 for the 49-item scale and 0.88 for the 12-item scale. The two scales were highly correlated (ICC= 0.98, R2 =0.97) |
| Post et al, 2011 | Netherlands | To assess short version of the SS-QoL | 97 patients with SAH and 105 patients with ischaemic stroke or intracerebral haemorrhage |
short version of the SS-QoL | Cronbach’s alpha 0.77e0.89 SS-Qol-12 scores predicted 88e95% of the variance of the original SS-QoL |
| Russell et al, 2011 | Ireland | to develop and test a QLASS | 92 stroke clients in immediately after discharge from hospital, 6 months and 12 months later | QLASS | The QLASS is proposed as a brief, valid HRQoL tool for use among people with stroke |
| Golicki et al, 2015 | Poland | To compare EQ-5D-5L (5L) validity vs. EQ-5D-3L (3L). | 408 patients with stroke | EQ-5D-5L (5L) EQ-5D-3L (3L) |
validity of the EQ-5D- 5L for health status in patients with acute stroke |
| Richardson et al, 2016 | Canada | to assess the psychometric properties of SIS | 164 patients with stroke | SIS Euroqol-5D (EQ-5D-5L) |
SIS for patient progress and tailor rehabilitation interventions in health intervention and assess them in various dimensions over time |
| Ayis et al, 2015 | UK | To assess the relationship between HRQoL at 3 months after stroke and survival up to 1 year across the 5 populations |
Patients with stroke, registered between 2004 and 2006 | EQ-5D SF-12 |
Strong associations between levels of the EQ-5D at 3 months and survival within the year a dose–response relationship |
1. Stroke Diagnostic Scales: It divided into pre-hospital and emergency department (table 2).
Pre-hospital scales: Several scales have been developed for paramedic.
1.1. Face Arm Speech Test (FAST): It has a good agreement for the detection of the acute stroke signs between emergency medical responders using the FAST system and stroke physicians. The scale is insensitive to isolated stroke-related visual or sensory impairments, vertigo, and gait disturbances (1).
1.2. Cincinnati Pre-hospital Stroke Scale (CPSS): It is effective for rapid diagnosis and can help to manage stroke in ambulance in short time with high specificity. This scale is a diagnostic screening tool, despite being easy to use; it cannot be the gold standard for stroke diagnosis (4). The result of other studies conducted on a combination of this scale with EMS impressions that indicate the combination both is sensitive, but does not have suitable specificity (5).
In fact, this scale has highly sensitive and moderate specifics.
1.3. Los Angeles Pre-hospital Stroke Screen (LAPSS): The LAPSS had a sensitivity of 91% (95% CI 76-98%) and specificity of 97% (95% CI 93-99%) (1).
1.4. Los Angeles Motor Scale (LAMS): In Noorian et al.’s study, sensitivity and specificity for LAMS in LVO among All Cerebral Ischemia was 0.76 and 0.65, respectively. The accuracy of LAMS was 0.72 (6). In Kim et al.’s study, indicated that the predictive validity of LAMS is excellent and has been used for evaluating stroke severity and researches (table 3) (7).
1.5. Pre-hospital Acute Stroke Severity scale (PASS): In the study of Hastrup et al., accuracy of scale for detecting large arterial occlusion was 0.76. This scale was simple and applicable for evaluating LVO in compromise with other scales(8). The patients with emergent large vessel occlusion (ELVO) who are the most likely to benefit from EVT (endovascular thrombectomy) can be identified by PASS with high specificity. The PASS scale included 3 clinical items and if there are 2 items. Although, this study suggests PASS scale is evaluated among general population (9).
1.6. The Finnish Pre-hospital Stroke Scale (FPSS): Ollikainen et al. combined conjugate eye deviation with common stroke signs for evaluating LVO and stroke. In this study, clients with 8 or higher NIHSS (National Institutes of Health Stroke Scale) score assessed computed tomography angiography. The sensitivity 54%, specificity 91%, positive predictive value 48%, negative predictive value 93%, and likelihood ratio was 6.2. this scale is easy for detecting stroke (10).
Emergency Department:
1.7. Recognition of Stroke in the Emergency Room (ROSIER): It facilitates rapid identification and triage by emergency department clinicians .The ROSIER scale incorporates the Glasgow Coma Scale and measurement of blood pressure and blood glucose along with the assessment of a seven-item stroke-recognition scale (1)
1.8. Guangzhou Stroke Scale (GZSS): In Mao et al.’s study, sensitivity and specificity of Guangzhou Stroke Scale among samples were 83.2 and 74.1, respectively. The diagnostic accuracy of Guangzhou Stroke Scale in this study was 81.97%. In fact, GZSS compromise with other scales is better for reorganization of suspected stroke (11).
1.9. Rapid Arterial Occlusion Evaluation (RACE): It is based on the items of NIHSS that had a high predictive value for large artery occlusion determined in the retrospective study. The RACE score ranges from a normal of 0 to a maximum of 9 points. For detecting large artery occlusion, score of 5 or higher score had sensitivity of 85% and specificity of 68% (12).
2. STROKE IMPAIRMENT SCALES
2.1. National Institutes of Health Stroke Scale (NIHSS): In the middle of cerebral artery territory size infarct, this score is valuable, but it cannot evaluate stroke related posterior circulation. Also, scoring for some symptoms and signs has not been considered.
On the other hand, the NIHSS can evaluate specific signs of posterior circulation stroke and severity of vertebra-basilar strokes undervalued (13). The baseline NIHSS score can be used to predict outcomes in these patients with mild stroke, but cutoff point is unclear (14). Also, the NIHSS is not effective for chronic stroke assessment. On one hand, distinguishing long-term post stroke outcomes has poor validity. This scale assesses the effect of stroke in acute stage (15).
2.2. Pediatric National Institutes of Health Stroke Scale (pedNIHSS): It was developed by modifying the adult NIHSS so examination items and testing materials are age-appropriate. In Ichord et al.’s study, in acute arterial ischemic stroke in children, the PedNIHSS showed good interrater reliability when employed by trained pediatric neurologists (16).
2.3. European Stroke Scale: It was designed to evaluate the territory of the MCA similar to the NIHSS which is reliable and partially validated (1).
2.4. Canadian Neurologic Scale (CNS): CNS is simpler and more rapidly performed than the NIHSS, but does not capture many stroke-related impairments. Like the NIHSS, the CNS has been validated for use retrospectively based on the information available in the medical record of clients with range of severities (1)
2.5. The Scandinavian Stroke Scale (SSS): The SSS has 82.2% of sensitivity and 71.4% of specificity. For identifying patients this was dependent on a 3-month follow-up good as NIHSS (17).
2.6. Barthel Index (BI): In Nakao et al’s. study, with a score of 40 or higher in 6 months except for bathing, grooming and stair climbing have been partially independent in their ADL. two-thirds in the patients with a score of 40 or higher had a possibility of being partially independent in their ADL and in approximately three weeks could predict activities of daily living disabilities in 6 months (18)
2.7. Functional Independence Measure (FIM): It assesses the patient disability in 13 aspects of motor function and five aspects of cognitive function. The FIM is widely used for monitoring functional improvement through the course of rehabilitation therapy. It can be assessed by telephone as well as in-person. A systematic review concluded that the FIM may have some utility for predicting outcome after stroke, though high-quality evidence was limited (1).
2.8. Instrumental Activities of Daily Living (IADL): It determines the ability of patients to live independently at home and assess a variety of activities (cooking, home management, recreation, etc). Several IADL scales are available, but the Frenchay Activities Index was specifically developed to use with stroke patients and is reliable (1).
3. HANDICAP SCALES
3.1. Modified Rankin Scale (mRS): It evaluates functional items in patients with stroke. Post stroke disorder due to stroke complication can effect on interview process. McArthur et al. evaluated proxy-derived modified Rankin Scale for solving this problem. but direct modified Rankin Scale interview is preferred (19).
3.2. Rankin Focused Assessment (RFA): In the study of Patel et al., was valuable and reliable instrument for global functional assessment. For all dichotomizations of the mRS, the inter-rater agreement was between 98-100% (20).
4. QUALITY OF LIFE SCALES
a. Health Related Quality of Life
4.1. Sickness Impact Profile (SIP): The sensitivity (64–84%), specificity (66–85%), positive predictive value (70–78%), and negative predictive value (76–87%) after six months after stroke were obtained (21).
4.2. Short Form 36: It is generic measure to assess HRQOL outcomes and may not be sensitive or specific enough to detect the psychological domains of mental health that are relevant to stroke (22).
4.4. European Quality of Life Score (EQ-5D-3L): In Golicki et al.’s study, it compromised EQ-5D-5L (5L) validity vs. EQ-5D-3L (3L) in stroke clients with acute phase. The results of study indicate that the EQ-5D-5L validate health status between patients with acute stroke (23). In the other study of Ayis et al. indicated the relations between HRQoL in three months with one year after stroke survival (24).
b. Stroke Specific Quality of Life Scale
4.5. Quality of Life after Stroke Scale (QLASS): It has 19 items in 3 category including emotional functioning, mastery and fatigue. These categories were correlated with valid measures of health status and activities of daily living. It is proposed as a brief, valid HRQoL tool for use among stroke patients (25).
4.6. Stroke Impact Scale (SIS): It has 60 items that can influence the use of scale for completion by the participants. For solving this problem 8-item SF-SIS was used that showed good agreement with original SIS and good correlation with our chosen functional and QOL measure (26). In another study of Richardson et al., they indicated that they can use the SIS for patient progress and tailor rehabilitation interventions in health intervention and assess them in various dimensions over time (27).
4.7. Stroke-Specific Quality of Life Scale ( SS-QoL ): Kerber et al.’s study, in 45 ischemic stroke patients, indicated that the 12-item scale is highly effective than the 49-item scale, with good internal consistency (Cronbach’s alpha 0.78- 0.89), short and valid for use in all subsets of stroke (8, 28).
We consider most common scales in current study with due the importance of stroke disease and relation with mortality (41-45) that was the strength of this study. The limitation of current study was we cannot be able to cover of too many instruments and scales in stroke.
In Conclusion the result of this study shows that for diagnostic stroke scales, study suggests fast and CPSS scale because they are easy to learn and rapidly administered, but there is no gold standard in stroke diagnosis in pre-hospital. For impairment stroke scales, NIHSS is valuable in MCA in acute stage not chronic or long term post stroke outcome. The BI scores at approximately three weeks could predict activities of daily living disabilities in 6 months. For handicap scales, Reliability of proxy mRS comprises mRS scores that was apparent and direct mRS interview is preferred. For quality of life, the stroke specific scales were suggested in comparison to HR-QOL scale. Finally, every scale has advantages and disadvantages and we were not able to introduce the gold standard for each item, but some special scales were used more in studies, preferred for comparability with other studies to match the research results.
Funding:
No
Disclosure:
This manuscript was presented in Third National Conference on neuromusculoskeletal Disorders in Babol, Iran, Nov 2018(29).
References
- 1.Goldstein LB, Kasner SE, Dashe JF. Use and utility of stroke scales and grading systems. UpToDate . 2017 Available at: https://zaya.io/z186d. [Google Scholar]
- 2.Drozdowska BA, Singh S, Quinn TJ. Thinking about the future-A review of prognostic scales used in acute stroke. Front Neurol. 2019;10:274. doi: 10.3389/fneur.2019.00274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–9. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 4.Maddali A, Razack FA, Cattamanchi S, Ramakrishnan TV. Validation of the cincinnati prehospital stroke scale. J Emerg Trauma Shock. 2018;11:111–4. doi: 10.4103/JETS.JETS_8_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.English SW, Rabinstein AA, Mandrekar J, Klaas JP. Rethinking prehospital stroke notification: assessing utility of emergency medical services impression and cincinnati prehospital stroke scale. J Stroke Cerebrovasc Dis. 2018;27:919–25. doi: 10.1016/j.jstrokecerebrovasdis.2017.10.036. [DOI] [PubMed] [Google Scholar]
- 6.Noorian AR, Sanossian N, Shkirkova K, et al. Los Angeles Motor Scale to identify large vessel occlusion: prehospital validation and comparison with other screens. Stroke. 2018;49:565–72. doi: 10.1161/STROKEAHA.117.019228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim JT, Chung PW, Starkman S, et al. Field validation of the Los Angeles Motor Scale as a tool for paramedic assessment of stroke severity. Clin Trial . 2017;48:298–306. doi: 10.1161/STROKEAHA.116.015247. [DOI] [PubMed] [Google Scholar]
- 8.Post MW, Boosman H, Van Zandvoort MM, et al. Development and validation of a short version of the Stroke Specific Quality of Life Scale. J Neurol Neurosurg Psychiatry. 2011;82:283–6. doi: 10.1136/jnnp.2009.196394. [DOI] [PubMed] [Google Scholar]
- 9.Hastrup S, Damgaard D, Johnsen SP, Andersen GJ. Prehospital acute stroke severity scale to predict large artery occlusion: design and comparison with other scales. Stroke. 2016;47:1772–6. doi: 10.1161/STROKEAHA.115.012482. [DOI] [PubMed] [Google Scholar]
- 10.Ollikainen JP, Janhunen HV, Tynkkynen JA, et al. The finnish prehospital stroke scale detects thrombectomy and thrombolysis candidates—a propensity score-matched study. J Stroke Cerebrovasc Dis. 2018;27:771–7. doi: 10.1016/j.jstrokecerebrovasdis.2017.10.015. [DOI] [PubMed] [Google Scholar]
- 11.Mao H, Lin P, Mo J, et al. Development of a new stroke scale in an emergency setting. BMC Neurol. 2016;16:168. doi: 10.1186/s12883-016-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pérez de la Ossa N, Carrera D, Gorchs M, et al. Design and validation of a prehospital stroke scale to predict large arterial occlusion: the rapid arterial occlusion evaluation scale. Stroke. 2014;45:87–91. doi: 10.1161/STROKEAHA.113.003071. [DOI] [PubMed] [Google Scholar]
- 13.Olivato S, Nizzoli S, Cavazzuti M, et al. e-NIHSS: an expanded National Institutes of Health Stroke Scale weighted for anterior and posterior circulation strokes. J Stroke Cerebrovasc Dis. 2016;25:2953–7. doi: 10.1016/j.jstrokecerebrovasdis.2016.08.011. [DOI] [PubMed] [Google Scholar]
- 14.Choi JC, Kim BJ, Han MK, et al. Utility of items of baseline national institutes of health stroke scale as predictors of functional outcomes at three months after mild ischemic stroke. J Stroke Cerebrovasc Dis. 2017;26:1306–13. doi: 10.1016/j.jstrokecerebrovasdis.2017.01.027. [DOI] [PubMed] [Google Scholar]
- 15.Peters HT, White SE, Page SJ. The national institutes of health stroke scale lacks validity in chronic hemiparetic stroke. J Stroke Cerebrovasc Dis. 2015;24:2207–12. doi: 10.1016/j.jstrokecerebrovasdis.2015.05.011. [DOI] [PubMed] [Google Scholar]
- 16.Ichord RN, Bastian R, Abraham L, et al. Interrater reliability of the Pediatric National Institutes of Health Stroke Scale (PedNIHSS) in a multicenter study. Stroke. 2011;42:613–7. doi: 10.1161/STROKEAHA.110.607192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Askim T, Bernhardt J, Churilov L, Indredavik B. The Scandinavian stroke scale is equally as good as The National Institutes of Health Stroke Scale in identifying 3-month outcome. J Rehabil Med. 2016;48:909–12. doi: 10.2340/16501977-2155. [DOI] [PubMed] [Google Scholar]
- 18.Nakao S, Takata S, Uemura H, et al. Relationship between Barthel Index scores during the acute phase of rehabilitation and subsequent ADL in stroke patients. J Med Invest. 2010;57:81–8. doi: 10.2152/jmi.57.81. [DOI] [PubMed] [Google Scholar]
- 19.McArthur K, Beagan ML, Degnan A, et al. Properties of proxy-derived modified Rankin Scale assessment. Int J Stroke. 2013;8:403–7. doi: 10.1111/j.1747-4949.2011.00759.x. [DOI] [PubMed] [Google Scholar]
- 20.Patel RD, Starkman S, Hamilton S, et al. The rankin focused assessment—ambulation: a method to score the modified rankin scale with emphasis on walking ability. J Stroke Cerebrovasc Dis. 2016;25:2172–6. doi: 10.1016/j.jstrokecerebrovasdis.2015.10.030. [DOI] [PubMed] [Google Scholar]
- 21.Stummer C, Verheyden G, Putman K, et al. Predicting sickness impact profile at six months after stroke: further results from the European multi-center CERISE study. Disabil Rehabil. 2015;37:942–50. doi: 10.3109/09638288.2014.948137. [DOI] [PubMed] [Google Scholar]
- 22.Winters C, Kwakkel G, van Wegen EE, et al. Moving stroke rehabilitation forward: The need to change research. NeuroRehabilitation. 2018;43:19–30. doi: 10.3233/NRE-172393. [DOI] [PubMed] [Google Scholar]
- 23.Golicki D, Niewada M, Buczek J, et al. Validity of EQ-5D-5L in stroke. Qual Life Res. 2015;24:845–50. doi: 10.1007/s11136-014-0834-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ayis S, Wellwood I, Rudd AG, et al. Variations in Health-Related Quality of Life (HRQoL) and survival 1 year after stroke: five European population-based registers. BMJ Open. 2015;5:e007101. doi: 10.1136/bmjopen-2014-007101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Russell M, Dempster M, Donnelly MJ. Measuring health-related quality of life after stroke: a brief tool. Queen Univ Belfast. 2011;6:41–51. [Google Scholar]
- 26.MacIsaac R, Ali M, Peters M, et al. Derivation and validation of a modified short form of the stroke impact scale. J Am Heart Assoc. 2016;5:e003108. doi: 10.1161/JAHA.115.003108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Richardson M, Campbell N, Allen L, Meyer M, Teasell R. The stroke impact scale: Performance as a quality of life measure in a community-based stroke rehabilitation setting. Disabil Rehabil. 2016;38:1425–30. doi: 10.3109/09638288.2015.1102337. [DOI] [PubMed] [Google Scholar]
- 28.Kerber KA, Brown DL, Skolarus LE, et al. Validation of the 12-item stroke-specific quality of life scale in a biethnic stroke population. Stroke Cerebrovasc Dis. 2013;22:1270–2. doi: 10.1016/j.jstrokecerebrovasdis.2012.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ahangar AA, Saadat P, Alijanpour S. Stroke and disability which scale should be use? Third National Conference on Neuromusculoskeletal Disorders; Babol, Iran: 2018. [Google Scholar]
- 30.Hantson L, De Weerdt W, De Keyser J, et al. The European stroke scale. Stroke. 1994;25:2215–9. doi: 10.1161/01.str.25.11.2215. [DOI] [PubMed] [Google Scholar]
- 31.Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index: a simple index of independence useful in scoring improvement in the rehabilitation of the chronically ill. Maryland State Med J. 1965;14:56–61. [PubMed] [Google Scholar]
- 32.Chumney D, Nollinger K, Shesko K, et al. Ability of Functional Independence Measure to accurately predict functional outcome of stroke-specific population: systematic review. J Rehabil Res Dev. 2010;47:17–29. doi: 10.1682/jrrd.2009.08.0140. [DOI] [PubMed] [Google Scholar]
- 33.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–86. [PubMed] [Google Scholar]
- 34.Perel P, Edwards P, Shakur H, Roberts I. Use of the Oxford Handicap Scale at hospital discharge to predict Glasgow Outcome Scale at 6 months in patients with traumatic brain injury. BMC Med Res Methodol. 2008;8:72. doi: 10.1186/1471-2288-8-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Litwin MS, McGuigan KA. Accuracy of recall in health-related quality-of-life assessment among men treated for prostate cancer. J Clin Oncol. 1999;17:2882–8. doi: 10.1200/JCO.1999.17.9.2882. [DOI] [PubMed] [Google Scholar]
- 36.Bergner M, Bobbitt RA, Carter WB, Gilson BS. The sickness impact profile: development and final revision of a health status measure. Med Care. 1981;19:787–805. doi: 10.1097/00005650-198108000-00001. [DOI] [PubMed] [Google Scholar]
- 37.Jenkinson C, Coulter A, Wright L. Short form 36 (SF36) health survey questionnaire: normative data for adults of working age. BMJ. 1993;306:1437–40. doi: 10.1136/bmj.306.6890.1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Horsman J, Furlong W, Feeny D, Torrance G. The Health Utilities Index (HUI): concepts, measurement properties and applications. BMJ. 2003;1:54. doi: 10.1186/1477-7525-1-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brooks R. EuroQol: the current state of play. Health Policy. 1996;37:53–72. doi: 10.1016/0168-8510(96)00822-6. [DOI] [PubMed] [Google Scholar]
- 40.Duncan PW, Bode RK, Min Lai S, et al. Rasch analysis of a new stroke-specific outcome scale: the stroke impact scale. Arch Phys Med Rehabil. 2003;84:950–63. doi: 10.1016/s0003-9993(03)00035-2. [DOI] [PubMed] [Google Scholar]
- 41.Ahmadi Ahangar A, Saadat P, Niroomand S, et al. Increased zinc serum level: new clues in babol stroke patients, Northern Iran. Stroke Res Treat. 2018;2018:7681682. doi: 10.1155/2018/7681682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ahangar AA, Saadat P, Heidari B, Taheri ST, Alijanpour S. Sex difference in types and distribution of risk factors in ischemic and hemorrhagic stroke. Int J Stroke. 2018;13:83–6. doi: 10.1177/1747493017724626. [DOI] [PubMed] [Google Scholar]
- 43.Ahmadi Ahangar A, Saadat P, Taheri Otaghsara ST, Alijanpour S. C-Reactive Protein Level in Admission and the Outcome of Stroke Survivors. J Babol Univ Med Sci. 2020;22:210–4. [Google Scholar]
- 44.Alijanpour S, Aslani Z, Alimohammadi N, Taleghani F. Empowerment of Nurses: A Key to Stroke Patients’ Satisfactions. Iran J Nurs Midwifery Res. 2020;25:237–41. doi: 10.4103/ijnmr.IJNMR_121_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Datobar H, Alijanpour H, Khafri S, Jahani MA, Naderi R. Patient’s Satisfaction of Emergency Department Affiliated Hospital of Babol University of Medical Sciences in 2013 -14. J Babol Univ Med Sci. 2016;18:56–62. [Google Scholar]