Abstract
“Foam Rolling” has been used in sports settings to increase range of motion and decrease muscle stiffness without decreasing muscle strength and athletic performance. However, there has been no study investigating the acute and prolonged effect of different durations of foam rolling intervention on muscle stiffness, and the minimum foam rolling intervention duration required to decrease muscle stiffness is unclear. Therefore, the purpose of this study was to investigate the acute and prolonged effect of different durations of foam rolling intervention on ROM, muscle stiffness, and muscle strength. The 45 participants were randomly allocated to 1 of 3 groups (30 s × 1 times group vs 30 s × 3 times group vs 30 s× 10 times group). The outcome measures were dorsiflexion range of motion, shear elastic modulus of medial gastrocnemius, and muscle strength before, 2 min and 30 min after foam rolling intervention. There were no significant differences before and 2 min after foam rolling intervention in 30 s×1 time group, whereas dorsiflexion range of motion was increased in both 30 s×3 times group (p = 0.042, d = 0.26) and 30 s× 10 times group (p < 0.01, d = 0.33). However, the increase in dorsiflexion range of motion was returned to baseline value after 30 minutes in both 30 s × 3 times group and 30 s × 10 times group. In addition, there were no significant changes in shear elastic modulus and muscle strength in all groups. This study suggested that foam rolling for more than 90 s or more of foam rolling was effective in order to increase the range of motion immediately without changing muscle stiffness and muscle strength.
Key points.
Dorsiflexion range of motion was increased after 90 s or 300 s foam rolling intervention, but not following 30 s foam rolling.
There were no significant changes in shear elastic modulus after 30s, 90s and 300s foam rolling.
The increase in range of motion after foam rolling could be contributed with change in stretch tolerance.
Key words: Shear elastic modulus, gastrocnemius muscle, dorsiflexion, isometric muscle strength
Introduction
Generally, it is believed that flexibility is an important component of sport performance and injury prevention. In particular, it has been reported that low range of motion (ROM) (Backman and Danielson, 2011; Witvrouw et al., 2001) lead to risk of sport injury. Therefore, an increase in ROM could be an effective approach for prevention of injury and recurrence. For that reason, in various situations, e.g., athletic and rehabilitation settings, stretching and some intervention are performed to increase ROM. However, concerning static stretching for ≥ 60 s per muscle tendon unit (especially without a comprehensive warm-up) caution should be taken, since detrimental effects on muscle performance were reported (Behm et al., 2016).
Recently, “foam rolling” has been used in sports settings to increase ROM and decrease muscle stiffness as a component of the warm-up routine. Yoshimura et al. (2019) reported that 180-second foam rolling intervention increased ROM but did not change the morphology (fascicle length and aponeurosis displacement during passive stretching) of muscle. In addition, MacDonald et al. (2013) reported that 120 s foam rolling intervention could increase ROM without decreasing muscle strength. Moreover, a recent meta-analysis by Wiewelhove et al. (2019) showed that foam rolling intervention resulted in a small improvement in sprint performance (+ 0.7%, effect size = 0.28) and flexibility (+ 4.0%, effect size = 0.34), whereas the effect on jump (-1.9%, effect size = 0.09) and strength performance (+ 1.8%, effect size = 0.12) was negligible. Furthermore, Wilke et al. (2020) in their meta-analysis showed that foam rolling intervention had a large magnitude in ROM but was not superior to stretching intervention. Interestingly, Morales-Artacho et al. (2017) investigated the effect of foam rolling on hamstring muscle stiffness by measured shear wave elastography (SWE), and showed a decrease in muscle stiffness after foam rolling intervention. To summarize these previous studies, it is assumed that foam rolling intervention could increase ROM and decrease muscle stiffness without decreasing muscle strength and athletic performance.
The previous studies showed that there was a dose-response relationship between static stretching duration and the effect on ROM or muscle stiffness. In fact, many studies have reported that longer duration static stretching resulted in a greater increase in ROM and decrease in passive stiffness (Boyce and Brosky, 2008; Nakamura et al., 2019; Nakamura et al., 2013). Similarly, it is possibility that there is a dose-response relationship between foam rolling duration and the effect on ROM. Phillips et al reported that 300 s foam rolling intervention was more effective in increasing ROM than 60 s foam rolling intervention (Phillips et al., 2018). In addition, Sullivan et al. (2013) investigated the effect of different durations of foam rolling interventions on sit and reach test, and showed that the sit and reach test was increased significantly after more than 5 second foam rolling intervention, and there was a trend for 10 second rolling duration to increase sit and reach test more than 5 second rolling duration. However, Bradbury-Squires et al. (2015) investigate the effects of 100 second and 300 second foam rolling interventions on knee flexion ROM, and showed that there was a trend for 300 second rolling duration to increase knee flexion ROM rather than 100 second rolling duration. Moreover, a systematic review by Hughes and Ramer (2019) investigated the dose-response relationship of foam rolling duration, and concluded that more than 90 s foam rolling could achieve a reduction in pain/soreness but the data were insufficient to draw a dose-response relationship between foam rolling duration and the effect on ROM. Therefore, revisiting the effect of different duration foam rolling intervention on ROM and muscle strength is warranted. Although e.g. Morales-Artacho et al. (2017) found a decrease in overall muscle stiffness, to best of our knowledge, there has been no study investigating the acute effect of especially different durations of foam rolling intervention on muscle stiffness, and the minimum foam rolling intervention duration required to decrease muscle stiffness is unclear. In addition, although the increase in ROM after stretching intervention might be involved an increase in passive torque (stretch tolerance) (Magnusson et al., 1996; Nakamura et al., 2018), as well as changes in the stiffness of muscle tendon unit (Kubo et al., 2001; Morse et al., 2008), the mechanism of increase in ROM after foam rolling intervention is also unclear. Moreover, while the prolonged effect of foam rolling intervention is important for athletes, coaches, and therapists, the prolonged effect of different durations of foam rolling intervention is unclear. Therefore, the purpose of this study was to investigate the acute and prolonged effect (after 30 minutes) of different durations of foam rolling intervention on ROM, muscle stiffness, and muscle strength. We have hypothesized that the longer duration of foam rolling intervention could have a greater and sustained effect of increasing ROM and decreasing muscle stiffness because there might be a dose-response relationship with the foam rolling effect.
Methods
Experimental Design
A randomized measured experimental design was used to investigate the acute and prolonged effects of different durations of foam rolling on ROM, shear elastic modulus of medial gastrocnemius (MG), and muscle strength in the dominant leg (the preferred leg for kicking a ball). Dorsiflexion (DF) ROM, passive torque, shear elastic modulus, and isometric muscle strength were measured before and after foam rolling for the plantar flexor muscle group. The participants were randomly allocated to 1 of 3 groups (30 s × 1 time group vs 30 s × 3 times group vs 30 s × 10 times group) in a 1:1 ratio using the alternation method (Nakamura et al., 2017). Based on a previous study (Kay and Blazevich, 2009), all measurements were taken prior to (PRE), 2 min after foam rolling (POST), and 30 minutes after foam rolling (30 min). In both 2 min and 30 min, participants remained resting in a sitting position on the isokinetic dynamometer (Biodex system 3.0; Biodex Medical Systems, NY, USA) after foam rolling intervention.
Participants
This study included 45 sedentary healthy adults volunteers (23 male: age 21.3 ± 1.9 years; height 1.73 ± 0.05 m; body mass 62.3 ± 7.9kg, 22 female: age 20.7 ± 0.5 years; height 1.58 ± 0.05 m; body mass 52.8 ± 6.7kg). Subjects with a history of neuromuscular disease or lower extremity musculoskeletal injury were excluded. Before this experiment, subjects did not performed regular resistance training and stretching of the lower limbs for more than 3 months. All subjects were fully informed of the procedures and purpose of the study, and all provided written informed consent. The study was approved by the ethics committee at the Niigata University of Health and Welfare, Niigata, Japan (Procedure 18304). Using G* power 3.1 software (Heinrich Heine University, Düsseldorf, Germany), the sample size required for a split-plot analysis of variance (ANOVA) (effect size = 0.40 (large), α error = 0.05, and power = 0.80) was calculated, and the required number of participants was more than 12 participants in each group.
Assessment of DF ROM
The subjects were secured in seated position in the chair of an isokinetic dynamometer with the knee angle at 0° (i.e., anatomical position). In addition, the trunk and the pelvis were fixed with the belt, and subjects were reclined (hip angle at 70°; 0° full extension) to prevent tension at the back of the knee. In this study, the footplate of the dynamometer was passively and isokinetically dorsiflexed at a speed of 5°/s from neutral anatomical position to the dorsiflexion angle just before the subjects started to feel discomfort or pain (Akagi and Takahashi, 2013; Nakamura et al., 2020; Sato et al., 2020). The subjects stopped the dynamometer by activating a safety trigger when they started to feel discomfort or pain, and the angle just before this point was defined as DF ROM. The measurement was done twice, and the average value was used for future analysis. We confirmed that there was no heel raise during DF ROM measurements. In addition, passive torque at DF ROM was defined as the stretch tolerance (Gajdosik et al., 2007; Mizuno et al., 2013; Weppler and Magnusson, 2010). Throughout the passive dorsiflexion test, participants were requested to relax completely and not offer any voluntary resistance. We confirmed that there was no voluntary contraction by watching the passive torque-angle curve during DF ROM measurements.
Assessment of shear elastic modulus of MG
In this study, we measured shear elastic modulus of MG by ultrasonic SWE (Aplio 500, Toshiba Medical Systems, Tochigi, Japan) with a 5-14 MHz linear probe at 10° dorsiflexion, similar to the positions during the DF ROM measurement. Shear elastic modulus of MG was measured at 30% of the lower leg length from the popliteal crease to the lateral malleolus near the point at which the maximal cross-sectional area in the lower leg is located (Akagi and Takahashi, 2013; Nakamura et al., 2014). Ultrasound image measurements were performed twice in the state of the long axis image of MG. The analysis of shear wave speed in ultrasound images was performed using image analysis software (MSI Analyzer version 5.0; Rehabilitation Science Research Institute, Japan). The measurement of shear wave speed (Vs) was set as the region of interest (ROI) in the area as large as possible in MG, and the average value of shear wave speed inside the ROI set was obtained. The shear elastic modulus was calculated as μ (kPa) = ρVs2, where ρ is muscle mass density (1000kg/m3). The average value of shear elastic modulus obtained from 2 ultrasound images was used for future analysis.
Assessment of Maximum Voluntary Isometric Contraction torque
The measurement of maximum voluntary isometric contraction (MVIC) torque was carried out using the dynamometer (Biodex System 3.0, Biodex Medical Systems, Inc., Shirley, NY, USA). The measurement position was similar to the DF ROM and shear elastic modulus assessment, and MVIC of the plantar flexors was measured with the ankle joint at the neutral position (0°). MVICs were performed for 5 s, and this was repeated two times with 60 s rest between each trial. The average value of two MVICs was used for analyses. Strong, verbal encouragement was provided to promote participants’ maximal effort during contractions.
Foam rolling intervention
Foam rolling was applied over gastrocnemius muscle using a foam roller (Gold’s Gym 18 Foam Roller, Logan, UT, USA) with a total diameter of 12.7 cm consisting of a 5-mm thick hollow plastic core covered with a 12-mm layer of dense foam(Richman et al., 2019). The subjects were instructed to perform 30-second foam rolling bouts. In the 30 s × 1 time group, the subjects performed only 1 set of foam rolling intervention. Moreover, in the 30 s × 3 times group and 30 s × 10 times group, the subjects performed 3 sets or 10 sets of foam rolling intervention with 30 s rest between each set. In this study, 1 cycle of foam rolling intervention was defined as one distal rolling plus 1 subsequent proximal rolling movement, and the frequency in this study was 30 cycles per 1 min using a metronome (Smart Metronome; Tomohiro Ihara, Japan). In detail, the subjects completed a total of 15 cycles for each set, in which adjusting the frequency seemed easy for them because everyone could do it. Foam rolling was performed unilaterally in a seated position with knees extended but relaxed. With the dominant lower leg laying on the foam roller, the non-dominant lower leg was put on the dominant lower leg and the participants used both hands on the floor to support their weight. Based on a previous studies (Kiyono et al., 2020; Krause et al., 2019), pressure was subjectively controlled with a target numerical rating scale rating of 7/10 (0 representing no discomfort and 10 representing maximal discomfort) during the intervention for both medial and lateral gastrocnemius muscle.
Statistical analysis
SPSS (version 24.0; SPSS Japan Inc., Tokyo, Japan) was used for statistical analysis. The distribution of the data was assessed using the Shapiro-Wilk test, and we confirmed that the data followed a normal distribution. Among groups differences in characteristics were assessed using one-way ANOVA. For DF ROM, passive torque at DF ROM, shear elastic modulus, muscle strength, a split-plot ANOVA using 2 factors (time [PRE vs POST vs 30 min] and group [30 s × 1 time group vs 30 s × 3 time group vs 30 s × 10 time group]) was used to determine the interaction and main effects. Furthermore, as a post hoc test, the significant differences among PRE, POST, and 30 min were determined using a paired t-test with Holm correction in each group. In addition, significant differences among each group were determined using an unpaired t-test with Holm correction in each time period. Spearman’s rank correlation coefficients (rs) were computed to quantify the linear relationship between the change in DF ROM and changes in passive torque at DF ROM (stretch tolerance) and the shear elastic modulus between PRE and POST in each group. Differences were considered statistically significant at an alpha of P < 0.05. Descriptive data are shown as mean ± standard deviation.
Results
The characteristics of study participants are reported in Table 1. There were no significant differences in age, height, or body mass between the 3 groups.
Table 1.
Characteristics of participants in 3 groups.
| 30s × 1 time group | 30s × 3 time group | 30s × 10 time group | P value | |
|---|---|---|---|---|
| Age (years) | 20.7 ± 0.8 | 20.9 ± 0.5 | 21.4 ± 2.3 | 0.461 |
| Height (m) | 1.66 ± 0.10 | 1.65 ± 0.09 | 1.66 ± 0.07 | 0.912 |
| Weight (kg) | 59.3 ± 10.0 | 59.0 ± 9.3 | 55.1 ± 6.3 | 0.366 |
| Male : Female | 8 : 7 | 7 : 8 | 8 : 7 |
Data presented as mean ± standard deviation.
All variables in all groups are presented in Table 2. The split-plot ANOVA indicated a significant interaction for the DF ROM (p < 0.01, F = 5.414, ηp 2 = 0.213). As a result of the post hoc test, there were no significant differences among times in 30 s×1 time group, whereas in both 30 s × 3 times group and 30 s × 10 times group, the DF ROM at POST values were higher than PRE and 30 min values (30 s × 3 times group: p = 0.042, d = 0.26, and p = 0.18, d = 0.20; 30 s × 10 times group: p < 0.01, d = 0.33, and p < 0.01, d = 0.37, respectively). However, there were no significant differences among each group in every time period.
Table 2.
Variables before and after 2 min or 30 min foam rolling intervention
| 30s × 1time group | 30s × 3 times group | 30s × 10 times group | |||||||
|---|---|---|---|---|---|---|---|---|---|
| PRE | POST | 30 min | PRE | POST | 30 min | PRE | POST | 30 min | |
| DF ROM (°) | 25.8 ±7.6 | 25.2± 6.7 | 25.2± 6.4 | 25.4± 7.7 | 27.2±6.4*# | 25.9±6.9 | 26.3±9.7 | 29.6±10.2*# | 26.1±8.6 |
| Passive torque at DF ROM (Nm) | 27.4±9.9 | 26.1±10.1 | 26.9±11.3 | 24.9±11.1 | 25.1±9.3 | 23.9±8.8 | 23.5±6.5 | 25.0±6.9 | 22.4±5.7 |
|
Shear elastic modulus of MG (kPa) |
24.9±10.9 | 25.1±10.7 | 25.3±11.7 | 15.5±9.0 | 14.7±9.0 | 17.5±9.3 | 19.9±8.1 | 20.4±9.6 | 20.2±8.3 |
| MVIC (Nm) | 139.1±38.5 | 137.0±40.8 | 140.3±41.1 | 131.4±30.6 | 127.1±29.4 | 128.8±32.6 | 122.5±26.4 | 123.4±24.5 | 122.9±29.7 |
* p < 0.05: significant difference between PRE and POST,
# p < 0.05: significant difference between POST and 30 min PRE, before foam rolling intervention; POST, 2 min after foam rolling intervention; 30 min, 30 min after foam rolling intervention; DF ROM: dorsiflexion range of motion; MG: medial gastrocnemius, MVIC, maximum voluntary isometric contraction. Data presented as mean ± standard deviation.
In addition, there were no significant interaction effects for passive torque at DF ROM, shear elastic modulus and muscle strength (passive torque at DF ROM: p = 0.072, F = 2.244, ηp2 = 0.101, shear elastic modulus: p = 0.953, F = 0.048, ηp2 = 0.001, muscle strength: p = 0.29, F = 1.266, ηp2 = 0.060, respectively). In addition, there were no significant main effects for time (passive torque at DF ROM: p = 0.136, F = 2.045, ηp2 = 0.049, shear elastic modulus: p = 0.808, F = 0.214, ηp2 = 0.005, muscle strength: p = 0.521, F = 0.657, ηp2 = 0.016, respectively).
The relationship between change in DF ROM and change in passive torque at DF ROM were shown in Figure 1. Although there was no significant correlation between change in DF ROM and change in passive torque at DF ROM in 30 s × 1 time group (rs = 0.468, p = 0.079), there was significant correlation between change in DF ROM and change in passive torque at DF ROM in both 30 s × 3 times group and 30 s × 10 times group (rs = 0.679, p < 0.01, rs = 0.704, p < 0.01, respectively). However, there was no significant correlation between change in DF ROM and change in shear elastic modulus (30 s × 1 time group: rs = -0.064, P = 0.82, 30 s × 3 time groups: rs = -0.168, p = 0.55, 30 s × 10 times group: rs = 0.004, p = 0.99, respectively).
Figure 1.
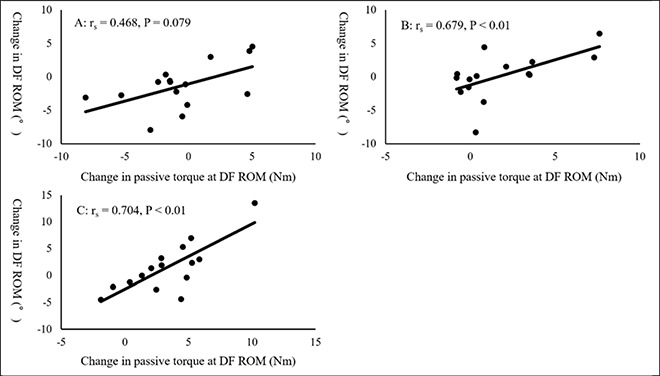
The relationship between change in DF ROM and change in passive torque at DF ROM.
Discussion
In this study, we investigated the acute and prolonged effect of different durations of foam rolling intervention (30 s×1time vs 30 s×3 times vs 30 s×10times) on DF ROM, shear elastic modulus of MG, and MVIC. Our results showed that there were significant increases in DF ROM in 30 s × 3 times group and 30 s × 10 times group, but the increase in DF ROM was returned to baseline following 30 min after foam rolling interventions. In addition, our results revealed that the increase in DF ROM was involved with changes in passive torque at DF ROM (i.e., stretch tolerance) in both 30 s × 3times group and 30 s × 10 times group (rs = 0.679, p < 0.01, rs = 0.704, p < 0.01, respectively). On the other hand, there were no significant changes for shear elastic modulus and MVIC in all foam rolling groups. To the best of our knowledge, this is the first paper to investigate the effect of different foam rolling durations in detail, and to clarify the minimum duration of foam rolling intervention required to increase ROM.
As mentioned above, our results showed that there was no significant change in DF ROM in 30 s× 1 time group (30 s), whereas there were significant increases in DF in 30 s × 3times group (90-second) and 30 s × 10 times group (300-second). Previous studies showed an increase in ROM after foam rolling intervention (MacDonald et al., 2013; Wiewelhove et al., 2019; Yoshimura et al., 2019), which is partially consistent with our results. However, there were no significant differences of DF ROM between PRE and 30 min in 30 s × 3times group and 30 s × 10 times group. Therefore, our results suggested that the increase in DF ROM after foam rolling intervention returned to baseline relatively rapidly. Mizuno et al investigated the prolonged effect of 300 s static stretching intervention on DF ROM and showed that DF ROM returned to baseline within 30 to 60 min (Gajdosik et al., 2007; Mizuno et al., 2013; Weppler and Magnusson, 2010). Since a meta-analysis review showed that there was no significant difference in ROM increase between foam rolling and stretching (Wilke et al., 2020), it was suggested that the prolonged effect of increasing ROM in foam rolling intervention was less than the effect of static stretching. Future studies are needed to clarify the mechanism of this difference between foam rolling and static stretching.
Interestingly, our results suggested that the increase in DF ROM could be involved with the change in passive torque at DF ROM, i.e., modification in stretch tolerance. In this study, we adopted the foam rolling intervention intensity of NRS = 7/10 (0 representing no discomfort and 10 representing maximal discomfort) based on a previous studies (Kiyono et al., 2020; Krause et al., 2019). Therefore, foam rolling intervention could change the pain threshold (stretch tolerance), and result in increased DF ROM. The previous studies suggested that change in ROM after stretching intervention is related to changes in tolerated passive torque, also known as stretch tolerance (Magnusson et al., 1996; 1997). In addition, Kay et al. (2015) reported that an increase in ROM after isometric contraction, static stretching, and contract-relax proprioceptive neuromuscular facilitation stretching could be involved with a change in stretch tolerance. The mechanism of change in stretch tolerance after foam rolling intervention is unknown, but our results extended the results of a previous study (Kay et al., 2015) on the effect of foam rolling intervention.
Interestingly, our results suggested that the minimum duration of foam rolling intervention required to increase DF ROM was 90 s. A previous study showed that 5-second foam rolling intervention significantly increases the sit and reach (Sullivan et al., 2013), which is inconsistent with our results. The discrepancy between the previous study and our results might be involved with differences in target muscle (hamstring muscle or plantar flexor) and/or the outcome measurement method (multiple joint ROM test or single-joint ROM test). Previous studies have reported that longer duration static stretching resulted in a greater increase in ROM and a decrease in passive stiffness (Boyce and Brosky, 2008; Nakamura et al., 2013; 2019). In addition, the systematic review by Hughes et al investigating the dose-response relationship of foam rolling duration concluded that more than 90 s foam rolling could achieve a reduction in pain/soreness (Hughes and Ramer, 2019). As described above, taken together with the fact that an increase in DF ROM was involved with the change in stretch tolerance, 90 s or more of foam rolling intervention could be necessary to change pain/soreness or stretch tolerance. These results should provide useful information for athletes, coaches, and therapists to perform, or prescribe foam rolling intervention. However, since the increase in DF ROM was dissipated within 30 min, foam rolling intervention could be insufficient for injury prevention.
Our results showed that there were no significant changes in shear elastic modulus in all foam rolling groups. These results were consistent with the results of a previous study showing that 180 s foam rolling intervention did not change morphology of muscle or muscle hardness (Yoshimura et al., 2019; 2020). By contrast, Morales-Artacho et al showed a decrease in shear elastic modulus of hamstring muscle after foam rolling intervention (Morales-Artacho et al., 2017). In addition, Baumgart et al. (2019) investigated the effect of foam rolling intervention on the anterior thigh and calf muscles using myomechanographic technique, and muscle stiffness of the rectus femoris was decreased after foam rolling intervention, whereas there was no significant change in muscle stiffness of MG. These results and our results suggested that muscle stiffness of thigh muscle could be decreased after foam rolling intervention, whereas muscle stiffness of calf muscle could not be changed after foam rolling intervention. Because of the difference in weight between the thigh and the lower leg, the discrepancy of changes in muscle stiffness between thigh muscle and plantar flexors might be involved with the differences in intervention intensities (Yoshimura et al., 2020). Further study is needed to clarify the possibility that the effect of foam rolling intervention on muscle stiffness differs depending on the muscle. In addition, higher muscle stiffness could lead to sport injury (Pickering Rodriguez et al., 2017; Watsford et al., 2010); foam rolling intervention for calf muscle could be insufficient for injury prevention.
Our results showed that there were no significant changes in MVIC in all foam rolling groups. A meta-analysis for foam rolling intervention showed that foam rolling resulted in a small improvement in sprint performance, whereas the effect on jump and strength performance was negligible (Wiewelhove et al., 2019), which was consistent with our results. Taken together with the change in DF ROM, because more than 90 s foam rolling intervention could increase DF ROM without decreasing muscle strength, incorporating more than 90-second foam rolling intervention into the warm-up routine is considered to be a good warm-up routine. Although the effect of more than 90 s foam rolling intervention on jump or sprint performance is still unclear, future study is needed to clarify this point.
There were some limitations in this study. Because the participants in this study were young healthy subjects, it is not clear whether similar changes occur in athletes. In addition, we investigated the effect of foam rolling on MG, and the possibility that the effect of foam rolling intervention on muscle stiffness differs depending on the muscle. Therefore, investigating foam rolling intervention on various muscles in athletes is needed. Moreover, this study investigated only the acute and prolonged effects of foam rolling intervention, but not the effect of incorporating foam rolling into the warm-up routine (i.e., prior aerobic activity or subsequent sport-specific activity; Behm et al., 2016). Therefore, the investigation of the effect of warm-up routine including the foam rolling intervention on ROM, muscle stiffness, and muscle strength is warranted.
Conclusion
In this study, we investigated the acute and prolonged effect of different durations of foam rolling intervention on DF ROM, shear elastic modulus, and muscle strength. This study suggested that foam rolling for more than 90 seconds (30 s × 3times) was effective in order to increase the DF ROM immediately, but the increase in DF ROM dissipated within 30 minutes. In addition, our results showed that an increase in DF ROM was not involved with any change in shear elastic modulus (muscle stiffness) of MG, but with passive torque at DF ROM (stretch tolerance). As an application in the sports field, from the standpoint of performance, it was suggested that foam rolling intervention for more than 90 seconds could be a useful technique before exercise because it increases ROM while not changing maximum torque. However, from the viewpoint of injury prevention, since it was shown that foam rolling intervention did not reduce shear elastic modulus, foam rolling intervention might be not an effective warm-up method for injury prevention.
Acknowledgements
This study was supported by a grant (Project P 32078-B) from the Austrian Science Fund FWF. The experiments comply with the current laws of the country in which they were performed. The authors have no conflict of interest to declare.
Biographies

Masatoshi NAKAMURA
Employment
Lecturer, Institute for Human Movement and Medical Sciences, Niigata Univ. of Health and Welfare, Niigata, Niigata, Japan
Degree
PhD
Research interests
Physical therapy, stretching, exercise physiology, flexibility
E-mail: masatoshi-nakamura@nuhw.ac.jp

Remi ONUMA
Employment
Department of Physical Therapy, Niigata University of Health and Welfare, Niigata, Niigata, Japan
Degree
BSc student
Research interests
Physical therapy, foam rolling, flexibility
E-mail: hpa17024@nuhw.ac.jp

Ryosuke KIYONO
Employment
Institute for Human Movement and Medical Sciences, Niigata Univ. of Health and Welfare, Niigata, Niigata, Japan
Degree
BSc, MSc student
Research interests
Physical therapy, foam rolling, flexibility, exercise physiology
E-mail: hpm19005@nuhw.ac.jp

Koki YASAKA
Employment
Department of Physical Therapy, Niigata University of Health and Welfare, Niigata, Niigata, Japan
Degree
BSc student
Research interests
Physical therapy, foam rolling, flexibility, delayed onset muscle soreness
E-mail: hpa17114@nuhw.ac.jp
Shigeru SATO
Employment
Institute for Human Movement and Medical Sciences, Niigata Univ. of Health and Welfare, Niigata, Niigata, Japan
Degree
BSc, MSc student
Research interests
Physical therapy, stretching, flexibility, resistance training
E-mail: hpm19006@nuhw.ac.jp

Kaoru YAHATA
Employment
Institute for Human Movement and Medical Sciences, Niigata Univ. of Health and Welfare, Niigata, Niigata, Japan
Degree
BSc, MSc student
Research interests
Physical therapy, stretching, flexibility, delayed onset muscle soreness
E-mail: hpm20011@nuhw.ac.jp

Taizan FUKAYA
Employment
PhD student, Institute for Human Movement and Medical Sciences, Niigata University of Health and Welfare, Niigata, Niigata, Japan
Degree
MSc, BSc
Research interests
Physical therapy, stretching, flexibility, exercise physiology
E-mail: fukaya.taizan@gmail.com

Andreas KONRAD
Employment
Institute of Human Movement Science, Sport and Health, University of Graz
Degree
PhD, MSc
Research interests
Biomechanics, muscle performance, training science, muscle-tendon-unit, soccer science
E-mail: andreas.konrad@uni-graz.at
References
- Akagi R., Takahashi H. (2013) Acute effect of static stretching on hardness of the gastrocnemius muscle. Medicine and Science in Sports and Exercise 45, 1348-54. [DOI] [PubMed] [Google Scholar]
- Backman L.J., Danielson P. (2011) Low range of ankle dorsiflexion predisposes for patellar tendinopathy in junior elite basketball players: a 1-year prospective study. American Journal of Sports Medicine 39, 2626-33. [DOI] [PubMed] [Google Scholar]
- Baumgart C., Freiwald J., Kühnemann M., Hotfiel T., Hüttel M., Hoppe M.W. (2019) Foam Rolling of the Calf and Anterior Thigh: Biomechanical Loads and Acute Effects on Vertical Jump Height and Muscle Stiffness. Sports (Basel) 7(1), 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behm D. G., Blazevich A. J., Kay A. D., McHugh M. (2016) Acute effects of muscle stretching on physical performance, range of motion, and injury incidence in healthy active individuals: a systematic review. Applied Physiology, Nutrition, and Metabolism 41(1), 1-11. [DOI] [PubMed] [Google Scholar]
- Boyce D., Brosky J.A., Jr. (2008) Determining the minimal number of cyclic passive stretch repetitions recommended for an acute increase in an indirect measure of hamstring length. Physiotherapy: Theory and Practice 24, 113-120. [DOI] [PubMed] [Google Scholar]
- Bradbury-Squires D. J., Noftall J. C., Sullivan K. M., Behm D. G., Power K. E., Button D. C. (2015) Roller-massager application to the quadriceps and knee-joint range of motion and neuromuscular efficiency during a lunge. Journal of Athletic Training, 50(2), 133-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gajdosik R.L., Allred J.D., Gabbert H.L., Sonsteng B.A. (2007) A stretching program increases the dynamic passive length and passive resistive properties of the calf muscle-tendon unit of unconditioned younger women. European Journal of Applied Physiology 99, 449-454. [DOI] [PubMed] [Google Scholar]
- Hughes G.A., Ramer L.M. (2019) Duration of myofascial rolling for optimal recovery, range of motion, and performance: a systematic review of the literature. International Journal of Sports Physical Therapy 14, 845-859. [PMC free article] [PubMed] [Google Scholar]
- Kay A.D., Blazevich A.J. (2009) Moderate-duration static stretch reduces active and passive plantar flexor moment but not Achilles tendon stiffness or active muscle length. Journal of Applied Physiology 106, 1249-1256. [DOI] [PubMed] [Google Scholar]
- Kay A.D., Husbands-Beasley J., Blazevich A.J. (2015) Effects of Contract-Relax, Static Stretching, and Isometric Contractions on Muscle-Tendon Mechanics. Medicine and Science in Sports and Exercise 47, 2181-2190. [DOI] [PubMed] [Google Scholar]
- Kiyono R., Onuma R., Yasaka K., Sato S., Yahata K., Nakamura M. (2020) Effects of 5-Week Foam Rolling Intervention on Range of Motion and Muscle Stiffness. The Journal of Strength and Conditioning Research. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Krause F., Wilke J., Niederer D., Vogt L., Banzer W. (2019) Acute effects of foam rolling on passive stiffness, stretch sensation and fascial sliding: A randomized controlled trial. Human Movement Science 67, 102514. [DOI] [PubMed] [Google Scholar]
- Kubo K., Kanehisa H., Kawakami Y., Fukunaga T. (2001) Influence of static stretching on viscoelastic properties of human tendon structures in vivo. Journal of Applied Physiology 90, 520-527. [DOI] [PubMed] [Google Scholar]
- MacDonald G.Z., Penney M.D., Mullaley M.E., Cuconato A.L., Drake C.D., Behm D.G., Button D.C. (2013) An acute bout of self-myofascial release increases range of motion without a subsequent decrease in muscle activation or force. The Journal of Strength and Conditioning Research 27, 812-821. [DOI] [PubMed] [Google Scholar]
- Magnusson S.P., Simonsen E.B., Aagaard P., Boesen J., Johannsen F., Kjaer M. (1997) Determinants of musculoskeletal flexibility: viscoelastic properties, cross-sectional area, EMG and stretch tolerance. Scandinavian Journal of Medicine & Science in Sports 7, 195-202. [DOI] [PubMed] [Google Scholar]
- Magnusson S.P., Simonsen E.B., Aagaard P., Sørensen H., Kjaer M. (1996) A mechanism for altered flexibility in human skeletal muscle. The Journal of Physiology 497 (Pt 1), 291-298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mizuno T., Matsumoto M., Umemura Y. (2013) Viscoelasticity of the muscle-tendon unit is returned more rapidly than range of motion after stretching. Scandinavian Journal of Medicine & Science in Sports 23, 23-30. [DOI] [PubMed] [Google Scholar]
- Morales-Artacho A.J., Lacourpaille L., Guilhem G. (2017) Effects of warm-up on hamstring muscles stiffness: Cycling vs foam rolling. Scandinavian Journal of Medicine & Science in Sports 27, 1959-1969. [DOI] [PubMed] [Google Scholar]
- Morse C.I., Degens H., Seynnes O.R., Maganaris C.N., Jones D.A. (2008) The acute effect of stretching on the passive stiffness of the human gastrocnemius muscle tendon unit. The Journal of Physiology 586, 97-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakamura M., Hirabayashi R., Ohya S., Aoki T., Suzuki D., Shimamoto M., Kikumoto T., Ito W., Nakamura E., Takabayashi T., Edama M. (2018) Effect of Static Stretching with Superficial Cooling on Muscle Stiffness. Sports Medicine International Open 2, E142-e147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakamura M., Ikezoe T., Kobayashi T., Umegaki H., Takeno Y., Nishishita S., Ichihashi N. (2014) Acute effects of static stretching on muscle hardness of the medial gastrocnemius muscle belly in humans: an ultrasonic shear-wave elastography study. Ultrasound in Medicine and Biology 40, 1991-7. [DOI] [PubMed] [Google Scholar]
- Nakamura M., Ikezoe T., Nishishita S., Tanaka H., Umehara J., Ichihashi N. (2019) Static stretching duration needed to decrease passive stiffness of hamstring muscle-tendon unit. The Journal of Physical Fitness and Sports Medicine 8, 113-116. [Google Scholar]
- Nakamura M., Ikezoe T., Takeno Y., Ichihashi N. (2013) Time course of changes in passive properties of the gastrocnemius muscle-tendon unit during 5 min of static stretching. Manual Therapy 18, 211-215. [DOI] [PubMed] [Google Scholar]
- Nakamura M., Ikezoe T., Umegaki H., Kobayashi T., Nishishita S., Ichihashi N. (2017) Changes in Passive Properties of the Gastrocnemius Muscle-Tendon Unit During a 4-Week Routine Static-Stretching Program. Journal of Sport Rehabilitation 26, 263-268. [DOI] [PubMed] [Google Scholar]
- Nakamura M., Sato S., Hiraizumi K., Kiyono R., Fukaya T., Nishishita S. (2020) Effects of static stretching programs performed at different volume-equated weekly frequencies on passive properties of muscle-tendon unit. Journal of Biomechanics. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Phillips J., Diggin D., King D.L., Sforzo G.A. (2018) Effect of Varying Self-myofascial Release Duration on Subsequent Athletic Performance. The Journal of Strength and Conditioning Research. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Pickering Rodriguez E.C., Watsford M.L., Bower R.G., Murphy A.J. (2017) The relationship between lower body stiffness and injury incidence in female netballers. Sports Biomechanics 16, 361-373. [DOI] [PubMed] [Google Scholar]
- Richman E.D., Tyo B.M., Nicks C.R. (2019) Combined Effects of Self-Myofascial Release and Dynamic Stretching on Range of Motion, Jump, Sprint, and Agility Performance. The Journal of Strength and Conditioning Research 33, 1795-1803. [DOI] [PubMed] [Google Scholar]
- Sato S., Kiyono R., Takahashi N., Yoshida T., Takeuchi K., Nakamura M. (2020) The acute and prolonged effects of 20-s static stretching on muscle strength and shear elastic modulus. Plos One 15, e0228583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan K.M., Silvey D.B., Button D.C., Behm D.G. (2013) Roller-massager application to the hamstrings increases sit-and-reach range of motion within five to ten seconds without performance impairments. International Journal of Sports Physical Therapy 8, 228-236. [PMC free article] [PubMed] [Google Scholar]
- Watsford M.L., Murphy A.J., McLachlan K.A., Bryant A.L., Cameron M.L., Crossley K.M., Makdissi M. (2010) A prospective study of the relationship between lower body stiffness and hamstring injury in professional Australian rules footballers. American Journal of Sports Medicine 38, 2058-2064. [DOI] [PubMed] [Google Scholar]
- Weppler C.H., Magnusson S.P. (2010) Increasing muscle extensibility: a matter of increasing length or modifying sensation? Physical Therapy 90, 438-449. [DOI] [PubMed] [Google Scholar]
- Wiewelhove T., Döweling A., Schneider C., Hottenrott L., Meyer T., Kellmann M., Pfeiffer M., Ferrauti A. (2019) A Meta-Analysis of the Effects of Foam Rolling on Performance and Recovery. Frontiers in Physiology 10, 376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilke J., Müller A.L., Giesche F., Power G., Ahmedi H., Behm D.G. (2020) Acute Effects of Foam Rolling on Range of Motion in Healthy Adults: A Systematic Review with Multilevel Meta-analysis. Sports Medicine 50, 387-402. [DOI] [PubMed] [Google Scholar]
- Witvrouw E., Bellemans J., Lysens R., Danneels L., Cambier D. (2001) Intrinsic risk factors for the development of patellar tendinitis in an athletic population. A two-year prospective study. American Journal of Sports Medicine 29, 190-195. [DOI] [PubMed] [Google Scholar]
- Yoshimura A., Inami T., Schleip R., Mineta S., Shudo K., Hirose N. (2019) Effects of Self-myofascial Release Using a Foam Roller on Range of Motion and Morphological Changes in Muscle: A Crossover Study. The Journal of Strength and Conditioning Research. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Yoshimura A., Schleip R., Hirose N. (2020) Effects of Self-Massage Using a Foam Roller on Ankle Range of Motion and Gastrocnemius Fascicle Length and Muscle Hardness: A Pilot Study. Journal of Sport Rehabilitation 28(8), 1171-1178. [DOI] [PubMed] [Google Scholar]


