Abstract
Pneumocephalus is commonly seen after skull and maxillofacial fractures. It can also occur following cerebrospinal fluid leak after skull base surgery and epidural catheter placement. We report a rare case report of a 20-year-old man who developed tension pneumocephalus following implant removal from the spine. He responded well to the conservative treatment without any neurological complications.
Keywords: orthopaedics, medical management
Background
Pneumocephalus describes the presence of gas within any of the intracranial compartments (subdural, subarachnoid, epidural, intraventricular or intraparenchymal spaces).1 The most frequent cause of pneumocephalus is head trauma (74%), followed by intracranial neoplasms, infections, neurosurgical procedures, paranasal sinus surgeries and lumbar puncture.2 3 Clinical presentations include headache, nausea and vomiting, restlessness, confusion, seizures, depressed neurological status and features of cerebellar ischaemia.4 The clinical features depend on whether it is non-tension or tension pneumocephalus and accordingly needs an aggressive treatment.4 The treatment includes bed rest, adequate hydration, supplemental oxygen, drilling of burr holes and closure of cerebrospinal fluid (CSF) fistula.1 2 5
Case presentation
Pneumocephalus as a complication of spine surgery is very rare.4 6–8 We present a case report of 20-year-old man who underwent spinal deformity correction with fusion at the age of 13 years. He was diagnosed to have congenital cervicothoracic scoliosis. He was followed up every year regularly after the surgery. There was no loss of correction of the deformity and had an excellent posterior bony fusion (figure 1).
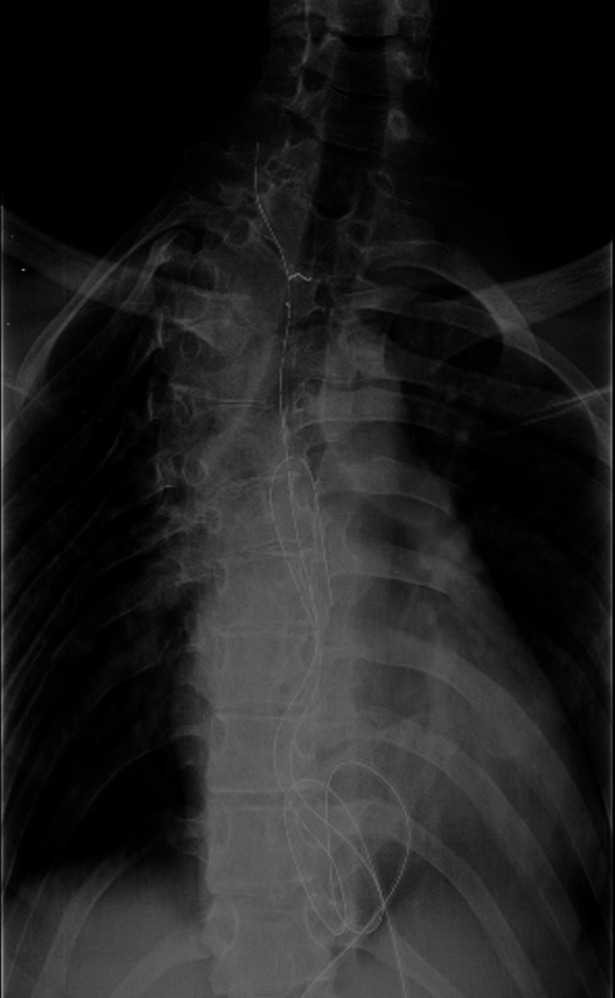
Figure 1.

Anteroposterior radiograph at final follow-up after scoliosis surgery.
The upper end of the implant was prominent with minimal pain and he wished to get it removed. He underwent spine implant removal surgery under general anaesthesia in prone position. Two pedicular hooks, three sublaminar wires, one transpedicular wire and a titanium connecting rod were removed. There was an excellent bony posterior fusion. After removing the upper sublaminar wire, a minimal CSF leak was noted at the level of third thoracic (T3) vertebra. As the site of leak was inaccessible and covered with thick bony fusion, no attempts were made to explore the dural tear. The site was packed the gel foam and local pressure was applied. The CSF leak stopped. The surgical wound was closed over an overflow (non-suction) drain superficial to the muscles layer. Postoperatively, the patient was on bed rest and broad-spectrum antibiotics (figure 2).
Figure 2.
Anteroposterior radiograph of the patient after the implant removal.
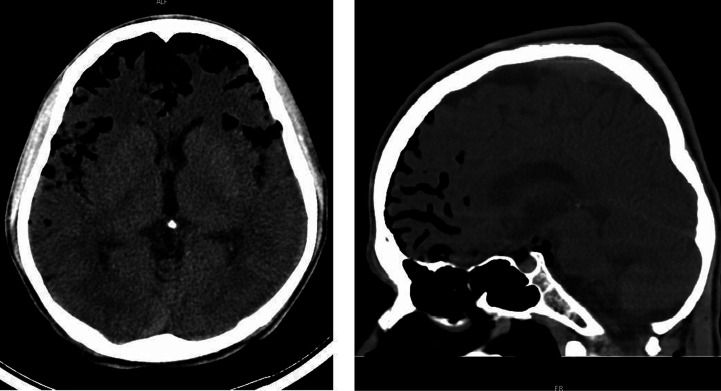
In the first and second postoperative day, he was asymptomatic except for pain at the surgical site. There was excess serosanguinous fluid (500 mL and 300 mL, respectively) in the overflow drain. However, his general condition was good. On the third postoperative day, he had sudden onset of intense frontal headache. Any attempts to move the head caused severe pain. A CT brain was done immediately after consulting a neurologist and the neurosurgeons. A CT brain showed multiple air pockets are in bilateral frontal and temporal subarachnoid spaces (figure 3).
Figure 3.
Day 3: multiple air pockets are in bilateral frontal and temporal subarachnoid spaces.
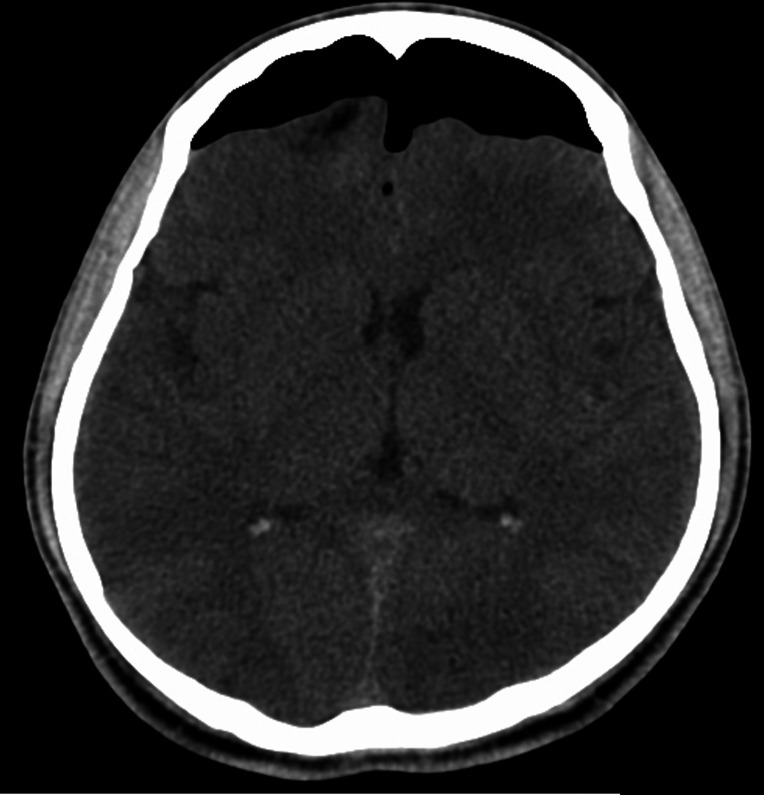
This condition was attributed to the CSF leak and the drains were removed with suturing of the stab wound through which drains were inserted. Prophylactic antiepileptic phenytoin sodium was started and continued for one month. He continued to have severe headache for six more days. As there was no deterioration in the neurological status, the patient was monitored in the Intensive Care Unit (ICU) in strict bed rest, oxygen therapy and adequate hydration. Paracetamol infusion was used for analgesia. The broad-spectrum antibiotics were continued. On eighth and ninth postoperative day, he had fever of 38°C associated with chills. His blood and urine microbiological cultures were sterile. The CT brain was repeated, which showed the classical Mount Fuji Sign indicating tension pneumocephalus5 (figure 4).
Figure 4.
Day 9: air pockets have coalesced to form a single pocket over the frontal area compressing both the frontal lobes (the Mount Fuji sign).
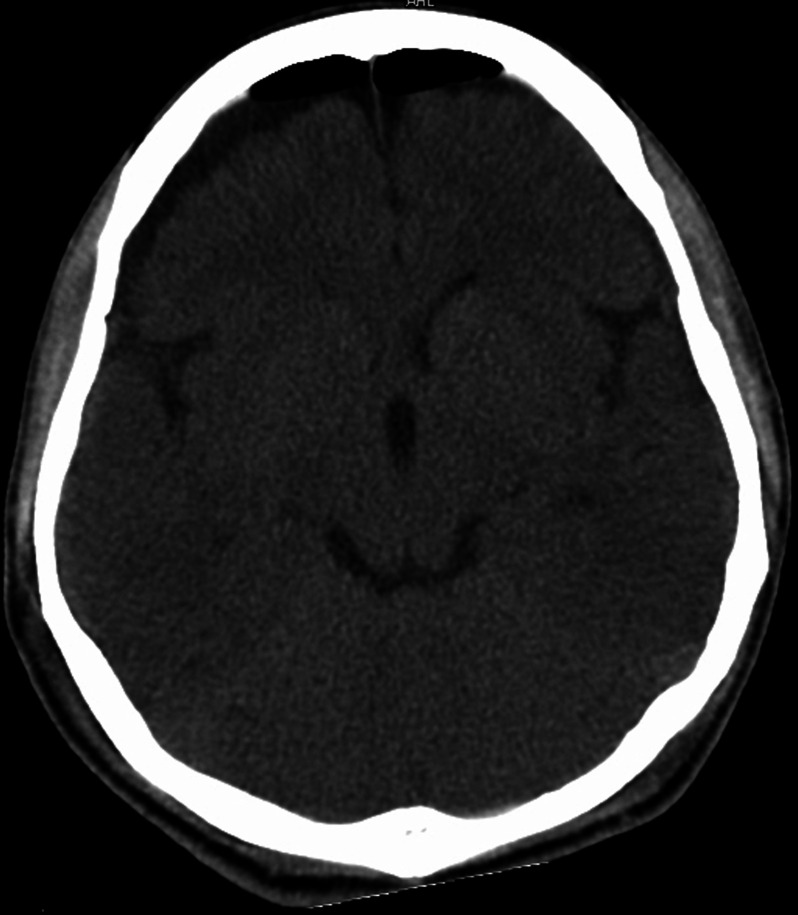
The fever subsided in 2 days. The headache also started reducing from the 10th postoperative day. On the 14th day, the CT brain was repeated to rule out any increase in the air volume (figure 5).
Figure 5.
Day 14: CT scan shows reduction in the volume of air.
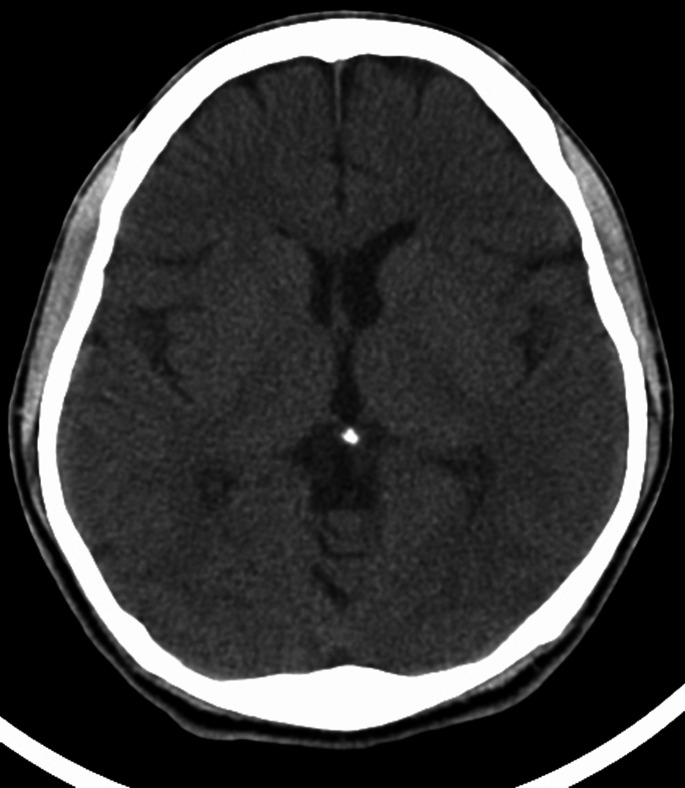
His headache gradually reduced over next 3 weeks. There were no wound-related complications. The CT scan was repeated at the end of 8 weeks, which showed complete resolution of the pneumocephalus (figure 6). His Glasgow Coma Score was 15 throughout the postoperative period.
Figure 6.
At 8 weeks, CT scan shows complete resolution of the pneumocephalus.
Differential diagnosis
Differential diagnosis includes non-tension pneumocephalus.
Outcome and follow-up
The patient was ambulated after complete resolution of the headache and discharged 5 weeks after surgery. He was further followed up regularly till the end of 1 year without any further complications.
Discussion
This is our first experience with such a serious complication which can occur after spinal surgery. The first description of pneumocephalus was made by Thomas in 1866.6 In the largest survey, Markham,2 studied 295 cases of pneumocephalus. The most common aetiology was traumatic (74%) and in 11 cases (3.7%) some kind of surgical intervention was found. Among them the leading cause of pneumocephalus is craniotomy.1 The other causes were, drainage of subdural haematomas, insertion of ventriculoperitoneal shunt and transsphenoidal or endoscopic sinus surgery. Spontaneous pneumocephalus was seen in neoplasms eroding the skull base, and in infection caused by gas producing organisms.9 This was also reported as a complication of invasive procedures like lumbar puncture,10 intracranial pressure monitoring11 and epidural catheter placement.3 Open thoracotomy for excision of bronchogenic carcinoma was later complicated by tension pneumothorax and hence pneumocephalus when the gas escaped through the CSF leak around the transected intercostals nerve.12
Many theories have been explained for the formation of pneumocephalus.13 (1) Once the air enters the subarachnoid space, it ascends cranially as air bubble rises in inverted pop bottle; (2) The ball valve mechanism allows the air to enter the subarachnoid space and prevents it from exiting and (3) The negative CSF pressure which increases after the CSF leak, drawing the air into the CSF compartment.
Pneumocephalus has also complicated many spine surgeries like lumbar disc surgery,14 lumbar spinal canal stenosis,14 anterior debridement for tuberculosis of dorsal spine,15 cervical myelopathy6 and pedicular fixation for correction of thoracolumbar scoliosis.8 16
In all these cases of spine surgery, CSF fistula was the common factor that occurred after dural tear in spite of dural repair. This was also the same cause of pneumocephalus after spine implant removal in our patient. As there was a dense bony fusion dorsal to the level of CSF leak, dural tear was not accessible. Hence, the fistula was packed with gel foam till it stopped leaking. Then drain was placed superficial to the muscle layer without negative suction. The drains were removed immediately when pneumocephalus was demonstrated and the wound were sealed. It was noted, while removing suction drain, that air was found escaping into the surgical wound around the tube orifice. We could not identify the cause of fever. It could have been due to chemical meningitis. However, broad-spectrum antibiotics were given prophylactically to prevent meningitis. Paracetamol infusion was effective in controlling the headache.
His initial CT showed multiple air pocket levels which later coalesced to form a single air bubble over the frontal lobe, compressing them to produce the Mount Fuji sign. This was a sign of tension pneumocephalus.5 The sign is not specific and it does not always warrant immediate surgical decompression.17 There are multiple case reports and series where tension pneumocephalus was managed non-operatively with a very close observation.17–20 As the patient neurological status was normal, and the only complaint of patient was frontal headache on moving the head, it was treated conservatively by adequate hydration, head end elevation, prophylactic antibiotics and antiepileptics as advised by the neurosurgeons. Prophylactic antibiotics and anticonvulsants are not necessarily evidence based and are largely driven by the local practice patterns.
Learning points.
Tension pneumocephalus is a rare but serious complication after spinal surgery.
It has resulted in fatal deaths and uncal herniation resulting in cerebellar infarcts, meningitis and cranial nerve palsies.
Knowledge about such entity and early detection and treatment of cerebrospinal fluid leak needs to be emphasised.
CT scan is a very useful investigation to detect and monitor pneumocephalus.
Footnotes
Twitter: @shyambhatn
Contributors: All authors made an individual contribution to the writing of the article. RSK, SNB and SPM: conception and design, acquisition of data or analysis and interpretation of data RSK and SNB: drafting the article or revising it critically for important intellectual content. RSK, SNB and SPM: final approval of the version published. All authors agreed to be accountable for the article and to ensure that all questions regarding the accuracy or integrity of the article are investigated and resolved.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Parental/guardian consent obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Schirmer CM, Heilman CB, Bhardwaj A. Pneumocephalus: case illustrations and review. Neurocrit Care 2010;13:152–8. 10.1007/s12028-010-9363-0 [DOI] [PubMed] [Google Scholar]
- 2.Markham JW. The clinical features of pneumocephalus based upon a survey of 284 cases with report of 11 additional cases. Acta Neurochir 1967;16:1–78. 10.1007/BF01401900 [DOI] [PubMed] [Google Scholar]
- 3.McMurtrie R, Jan R. Subarachnoid pneumocephalus: a rare complication of epidural catheter placement. J Clin Anesth 2002;14:539–42. 10.1016/S0952-8180(02)00426-9 [DOI] [PubMed] [Google Scholar]
- 4.Andrews RT, Koci TM. Cerebellar herniation and infarction as a complication of an occult postoperative lumbar dural defect. AJNR Am J Neuroradiol 1995;16:1312–7. [PMC free article] [PubMed] [Google Scholar]
- 5.Michel SJ. The Mount Fuji sign. Radiology 2004;232:449–50. 10.1148/radiol.2322021556 [DOI] [PubMed] [Google Scholar]
- 6.Sasaki K, Matsumoto T, Mizuno T, et al. Pneumocephalus associated with cerebrospinal fluid fistula as a complication of spinal surgery: a case report. Case Rep Med 2010;2010:1–4. 10.1155/2010/328103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Turgut M, Akyüz O. Symptomatic tension pneumocephalus: an unusual post-operative complication of posterior spinal surgery. J Clin Neurosci 2007;14:666–8. 10.1016/j.jocn.2006.02.021 [DOI] [PubMed] [Google Scholar]
- 8.Nowak R, Maliszewski M, Krawczyk L. Intracranial subdural hematoma and pneumocephalus after spinal instrumentation of myelodysplastic scoliosis. J Pediatr Orthop B 2011;20:41–5. 10.1097/BPB.0b013e32833f33d1 [DOI] [PubMed] [Google Scholar]
- 9.Jayaram S, Jadhav S, Rathod D, et al. Meningitis: an unusual cause of pneumocephalus. J Assoc Physicians India 2004;52:67–75. [PubMed] [Google Scholar]
- 10.Guarino AH, Wright NM. Pneumocephalus after a lumbar epidural steroid injection. Pain Physician 2005;8:239–80. [PubMed] [Google Scholar]
- 11.Vitali AM, le Roux AA. Tension pneumocephalus as a complication of intracranial pressure monitoring: a case report. Indian Journal of Neurotrauma 2007;04:115–8. 10.1016/S0973-0508(07)80025-6 [DOI] [Google Scholar]
- 12.D'Addario R, Greenberg J, O'Neill TJ, et al. Pneumocephalus: an unusual cause. J Neurol Neurosurg Psychiatry 1974;37:271–4. 10.1136/jnnp.37.3.271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Walker FO, Vern BA. The mechanism of pneumocephalus formation in patients with CSF fistulas. J Neurol Neurosurg Psychiatry 1986;49:203–5. 10.1136/jnnp.49.2.203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yun JH, Kim YJ, Yoo DS, et al. Diffuse pneumocephalus : a rare complication of spinal surgery. J Korean Neurosurg Soc 2010;48:288. 10.3340/jkns.2010.48.3.288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lin MB, Cheah FK, Ng SE, et al. Tension pneumocephalus and pneumorachis secondary to subarachnoid pleural fistula. Br J Radiol 2000;73:325–7. 10.1259/bjr.73.867.10817052 [DOI] [PubMed] [Google Scholar]
- 16.Ozturk E, Kantarci M, Karaman K, et al. Diffuse pneumocephalus associated with infratentorial and supratentorial hemorrhages as a complication of spinal surgery. Acta Radiol 2006;47:497–500. 10.1080/02841850600644766 [DOI] [PubMed] [Google Scholar]
- 17.Moscovici S, Halevy D, Mizrahi CJ, et al. Sensitivity of the Mount Fuji sign after evacuation of chronic subdural hematoma in nonagenarians. J Comput Assist Tomogr 2019;43:686–9. 10.1097/RCT.0000000000000897 [DOI] [PubMed] [Google Scholar]
- 18.Jakhere SG, Yadav DA, Jain DG, et al. Does the Mount Fuji Sign always signify ‘tension’ pneumocephalus? An exception and a reappraisal. European Journal of Radiology Extra 2011;78:e5–7. 10.1016/j.ejrex.2011.01.002 [DOI] [Google Scholar]
- 19.Himeno T, Takeshima S, Kubo S, et al. [Tension pneumocephalus complicated from bacterial meningitis - a report of case presenting "Mount Fuji sign" in brain CT]. Rinsho Shinkeigaku 2013;53:478–81. 10.5692/clinicalneurol.53.478 [DOI] [PubMed] [Google Scholar]
- 20.Ryan J, Shields G, Finegan E, et al. Post traumatic tension pneumocephalus: the Mount Fuji sign. Ir Med J 2017;110:550. [PubMed] [Google Scholar]