Abstract
Cerebral embolic protection (CEP) devices aim to reduce the risk of periprocedural cerebrovascular events during transcatheter aortic valve implantation (TAVI). Here, the authors describe the first-in-human experience with the ProtEmbo Cerebral Protection System (Protembis), a next-generation CEP device, during TAVI. This case is part of a larger European trial evaluating the safety and performance of this device. After deployment of the ProtEmbo in the aortic arch, a first transcatheter heart valve was implanted. Despite postdilatation, moderate to severe aortic regurgitation persisted. The operating team decided to perform a valve-in-valve procedure using a second transcatheter heart valve. The ProtEmbo demonstrated good coverage of all three head vessels and no interaction with TAVI catheters in the aortic arch throughout the entire procedure. No adverse events were observed during hospitalisation or follow-up, and there was a significant reduction in aortic regurgitation at follow-up echocardiography. Despite a challenging overall procedure with presumably high embolic burden, diffusion-weighted MRI at follow-up showed a low number (n=3) and volume (156 mm3) of new hyperintense lesions. The first-in-human use of the ProtEmbo was safe and feasible, despite a challenging TAVI valve-in-valve procedure.
Keywords: Aortic valve stenosis, embolic protection, transcatheter aortic valve implantation (TAVI), valve-in-valve
Cerebral embolic protection (CEP) devices are used to reduce the risk of periprocedural cerebrovascular events during transcatheter aortic valve implantation (TAVI).[1] Clinical cerebrovascular event rates as high as 10% have been reported at 30 days following TAVI.[2]
The next-generation ProtEmbo Cerebral Protection System (ProtEmbo; Protembis) is an aortic filter device that deflects emboli arising during TAVI away from the cerebral circulation (Figure 1). The ProtEmbo consists of an implantable filter with the smallest pore size available among CEP devices that is introduced via a 6 Fr left transradial sheath and prevents the migration of embolic particles through the three great branch vessels of the aortic arch into the brain. This new generation of the ProtEmbo has an improved frame shape and a dedicated ergonomic handle to facilitate push–pull and torque of the device during deployment in the aortic arch. The filter dimensions have increased in the new generation device from 29 mm × 68 mm to 38 mm × 70 mm (17.5% more surface).
Figure 1: ProtEmbo Cerebral Protection System.
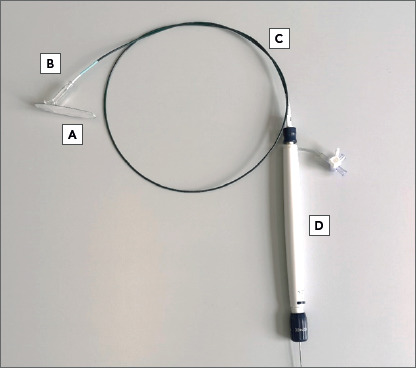
A: Deflection filter for placement in the aortic arch. B: Crimping tool to load the deflection filter (shaper). C: Delivery catheter (commercially available). D: Ergonomic handle for consistent deployment and retrieval.
The self-positioning ProtEmbo filter covers all three major cerebral arteries in the aortic arch, maintaining blood flow to the cerebral vessels through 60 µm pores. The filter membrane is heparin-coated to avoid clot formation.
The case with the ProtEmbo reported here was the very first-in-human case of a larger European trial evaluating the safety and performance of this device (NCT04618718).
Case Report
An 81-year-old woman (height 158 cm, weight 62 kg) was admitted with significant symptoms of heart failure (New York Heart Association Class III) and AF. The patient’s left ventricular ejection fraction was 60% prior to the procedure and her Society of Thoracic Surgeons score for mortality was 2.13%. A transthoracic echocardiogram revealed a severely calcified tricuspid aortic valve, with a maximum aortic valve gradient of 64 mmHg and mean aortic valve gradient of 40 mmHg.
The heart team approved transfemoral TAVI with a 23 mm SAPIEN 3 transcatheter heart valve (Edwards Lifesciences). Informed consent was obtained from the patient to implant the ProtEmbo for temporary cerebral embolic protection as part of the clinical study. To ensure the patient was a candidate for the trial, a multislice CT scan was analysed to exclude severe peripheral arterial disease or severely tortuous or atheromatous vasculature.
The ProtEmbo was easy to place using left radial access without experiencing any issues (Supplementary Material Videos 1–4). After deployment of the CEP device in the aortic arch, the native aortic valve was predilated prior to implantation of the transcatheter heart valve (THV). After implantation of the heart valve prosthesis, the patient exhibited moderate to severe aortic regurgitation. Despite postdilatation (23 mm balloon), moderate to severe aortic regurgitation persisted.
The operating team decided to perform a valve-in-valve procedure using a second 23 mm SAPIEN 3 THV. Postdilatation was performed with a good final result. The patient was extubated with no neurological deficits or vascular complications. No adverse events were observed during hospitalisation or follow-up, and there was a significant reduction in aortic regurgitation on follow-up echocardiography.
Despite multiple arch crossings with two THVs and additional devices, no interaction with the ProtEmbo was observed (Supplementary Material Videos 5–11). The ProtEmbo dwell time was 79 minutes and, after removal (Supplementary Material Video 12), the filter was devoid of embolic debris. The device demonstrated good coverage of all three head vessels during the entire procedure. An incremental amount of 15 ml contrast medium was used for the ProtEmbo. Despite the challenging overall procedure (predilatation, two THV implantations and two postdilatations) with presumably high embolic burden, fluoroscopy time was extended only marginally in this first-in-human use of the device (5 of 35 min in total) and diffusion-weighted MRI at follow-up showed a low number (n=3) and volume (156 mm[3]) of new hyperintense lesions compared with previous publications.[2–4]The patient was discharged home on day 5.
Discussion
This is a single-case report of the first-in-human use of the ProtEmbo as part of a larger study designed to evaluate the safety and performance of the device. Hence, this report does not provide any conclusive evidence of the benefits of embolic protection with the ProtEmbo; all results should be considered hypothesis generating and interpreted with caution.
Conclusion
In conclusion, the first-in-human use of the device was safe and feasible despite a challenging TAVI valve-in-valve procedure with presumably high embolic burden. The updated design of the ProtEmbo has significantly improved ease of use and has enhanced embolic protection features. The results of the ongoing European trial will determine the safety and performance of this new CEP device for preventing cerebral embolism during TAVI.
Impact on Daily Practice
Embolisation of a thrombus and other debris to the cerebral vasculature is a complication during TAVI. CEP devices may reduce the amount of migrating embolic material, potentially reducing the ischaemic burden in the brain and preserving neurocognitive function.
Box 1. List of Linked Supplementary Material Videos
Supplementary Material Video 1: Placement of the Sheath into the Aortic Arch for Delivery of the ProtEmbo
Supplementary Material Video 2: Advancing the ProtEmbo Through theSheath and Pushing Out the ProtEmbo Device Tip
Supplementary Material Video 3: Torquing of the ProtEmbo Device Tip for Correct Deployment
Supplementary Material Video 4: Deployment of the ProtEmbo in theAortic Arch Across All Three Side Branch Vessels
Supplementary Material Video 5: Crossing of First Transcatheter HeartValve System without Any Interaction with the ProtEmbo
Supplementary Material Video 6: Expansion of the First TranscatheterHeart Valve System
Supplementary Material Video 7: Removal of the Delivery System for theFirst Transcatheter Heart Valve System without Any Interaction with theProtEmbo
Supplementary Material Video 8: Crossing of the Second TranscatheterHeart Valve System without Any Interaction with the ProtEmbo
Supplementary Material Video 9: Expansion of the Second TranscatheterHeart Valve System
Supplementary Material Video 10: Removal of the Delivery System for the Second Transcatheter Heart Valve System without Any Interaction with the ProtEmbo
Supplementary Material Video 11: Removal of the Pigtail Catheter
Supplementary Material Video 12: Removal of the ProtEmbo from theAortic Arch
References
- 1.Giustino G, Sorrentino S, Mehran R et al. Cerebral embolic protection during TAVR: a clinical event meta-analysis. J Am Coll Cardiol. 2017;69:465–6. doi: 10.1016/j.jacc.2016.12.002. [DOI] [PubMed] [Google Scholar]
- 2.Kapadia SR, Kodali S, Makkar R et al. Protection against cerebral embolism during transcatheter aortic valve replacement. J Am Coll Cardiol. 2017;69:367–77. doi: 10.1016/j.jacc.2016.10.023. [DOI] [PubMed] [Google Scholar]
- 3.Haussig S, Mangner N, Dwyer MG et al. Effect of a cerebral protection device on brain lesions following transcatheter aortic valve implantation in patients with severe aortic stenosis: the CLEAN-TAVI randomized clinical trial. JAMA. 2016;316:592–601. doi: 10.1001/jama.2016.10302. [DOI] [PubMed] [Google Scholar]
- 4.Lansky AJ, Schofer J, Tchetche D et al. A prospective randomized evaluation of the TriGuard™ HDH embolic DEFLECTion device during transcatheter aortic valve implantation: results from the DEFLECT III trial. Eur Heart J. 2015;36:2070–8. doi: 10.1093/eurheartj/ehv191. [DOI] [PubMed] [Google Scholar]


